Abstract
The emergence of carbapenemase-producing Gram-negative bacilli is a worldwide problem. To date, no study has evaluated the prevalence of faecal carriage of carbapenemase-producing and carbapenem-resistant Gram-negative bacilli (CR GNB) in France. From 1 February to 30 April 2012, we conducted a prospective, multicentre study in three University Hospitals and four General Hospitals in the south of France. The carriage of carbapenemase-producing Enterobacteriaceae (CPE) and other CR GNB was screened by both cultivation on chromID® CARBA and chromID® OXA-48 media (bioMérieux) and molecular tools [multiplex polymerase chain reaction (PCR) and NucliSENS EasyQ® KPC (bioMérieux)]. The genetic relationship between isolates was assessed by rep-PCR (DiversiLab, bioMérieux) or multilocus sequence typing (MLST). The prevalences of CR GNB and carbapenemase-producing bacteria were 2.4 % (27/1,135) and 0.4 % (n = 5), respectively. Two strains corresponded to OXA-23-producing Acinetobacter baumannii and belonged to the widespread sequence type (ST) 2/international clone II, whereas one strain was an ST15 OXA-48-producing Klebsiella pneumoniae. Two OXA-48-producers were detected exclusively by PCR. This first French study revealed the very low dissemination of carbapenemase-producing bacteria in patients attending hospitals in southern France during a non-outbreak situation. However, the increasing description of epidemic cases in this area must reinforce the use of hygiene procedures to prevent diffusion of these multidrug-resistant microorganisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Carbapenem-resistant Gram-negative bacilli (CR GNB) isolates have been increasingly reported throughout the world [1]. The main bacteria harbouring this resistance are Pseudomonas aeruginosa, Acinetobacter spp. and members of the family Enterobacteriaceae. Different mechanisms are involved in carbapenem resistance: (i) selective impermeability or efflux, especially in P. aeruginosa, (ii) reduced outer membrane permeability in combination with production of extended-spectrum β-lactamase (ESBL) or overproduction of AmpC β-lactamase, especially in Enterobacteriaceae, and (iii) production of carbapenemase, e.g. OXA-48-, KPC- or NDM-producers in Enterobacteriaceae and OXA-23-, IMP-, VIM- or GES-producers in non-fermenters. The emergence of carbapenemase-producing Enterobacteriaceae (CPE) has become a major public health concern, notably in Mediterranean countries [2]. To limit the propagation of these multidrug-resistant bacteria, French national recommendations suggest the screening of all patients who came from a foreign country and were hospitalised in this country (http://www.hcsp.fr/explore.cgi/avisrapportsdomaine?clefr=372).
If different publications allow to map the countries where CPE have emerged, very few data on the faecal carriage of these isolates are available [3–6]. The aim of the present study was to determine the prevalence of faecal carriage of CR GNB in patients hospitalised or consulting in the south of France during a non-outbreak period.
Materials and methods
Data collection and bacterial isolates
A bioMérieux collection of 202 strains [33 OXA-48-producing Enterobacteriaceae, four OXA-181-producing Enterobacteriaceae, 35 carbapenemase-producing Enterobacteriaceae, 36 ESBL-producing Enterobacteriaceae, 14 carbapenem-resistant Enterobacteriaceae by impermeability, 10 non-fermentative Gram-negative bacilli, 14 vancomycin-resistant enterococci and 56 wild-type strains (12 Enterobacteriaceae, eight Candida spp., four Staphylococcus aureus, three Enterococcus spp., 11 A. baumannii, 11 P. aeruginosa, seven Stenotrophomonas maltophilia)] was used to validate the screening media [7].
From 1st February to 30th April 2012, faecal samples from patients hospitalised or consulting in seven hospitals in southern France (University Hospitals of Montpellier, Nîmes and Toulouse; General Hospitals of Aix-en-Provence, Alès, Aubagne and Perpignan) were prospectively and consecutively collected. Sampling was carried out among stools submitted for the detection of enteropathogens or rectal swab performed to screen multidrug-resistant enteric bacteria on the first day of hospitalisation and without antibiotic treatment. Redundant samples were excluded. The following clinical data were collected prospectively: demographic data, clinical ward, previous hospitalisation in the last 12 months and length of the current stay. Specimens were conserved at −20 °C and sent to Nîmes University Hospital at the end of inclusion.
Screening methods
To validate the selective chromogenic media [chromID® CARBA and chromID® OXA-48 (bioMérieux, La Balme-les-Grottes, France)], we inoculated by streaking per plate a low inoculum (103 CFU) for OXA-48-producing Enterobacteriaceae and a high inoculum (106 CFU) for all the other strains. Plates were incubated at 37 °C under aerobic conditions and assessed after 24 and 48 h of incubation. The colour and intensity of the colonies were recorded according to the colour chart provided by the manufacturer.
To screen for CR GNB, samples were placed in 1 mL sterile 0.9 % NaCl solution and then vortexed. From this suspension, 100 μL were plated on two selective chromogenic culture media performed to identify CPE, chromID® CARBA and chromID® OXA-48 [8]. Plates were incubated at 37 °C under aerobic conditions and assessed after 18, 24 and 48 h of incubation. The colour and intensity of the colonies were recorded according to the colour chart provided by the manufacturer.
In parallel, we used molecular biology tools to screen stools. Plasmid and chromosomal DNA was extracted from the clinical specimens using the NucliSENS® easyMAG system (bioMérieux) with onboard lysis. For bla KPC screening, the NucliSENS EasyQ® KPC assay (bioMérieux) was performed according to the manufacturer’s instructions. For Enterobacteriaceae and P. aeruginosa, the genotypic characterisation was determined by multiplex polymerase chain reaction (PCR) assays targeting bla OXA-48-like, bla NDM-like, bla IMP-like and bla VIM-like genes on sample extracts [9]. For A. baumannii, fragments of bla OXA alleles were amplified using a specific multiplex PCR assay [10]. All PCR products were identified by sequencing [9, 10].
Strain identification and antimicrobial susceptibility testing
The Vitek 2 automated system (bioMérieux) was used for the biochemical identification of all isolates growing on the two commercial media. Antimicrobial susceptibility was determined by the disc diffusion method according to recommendations of the Antibiogram Committee of the French Society for Microbiology (http://www.sfm-microbiologie.org). The Etest method (bioMérieux) was used to determine the susceptibility to the four carbapenems (ertapenem, imipenem, meropenem and doripenem).
Characterisation of carbapenemase-encoding genes in bacterial isolates
Plasmid and chromosomal DNA was extracted from the isolates of screening media using the EZ1 DNA Tissue Kit on the BioRobot EZ1 extraction platform (Qiagen, Courtaboeuf, France). The same multiplex PCRs used for screening and sequencing were performed [9, 10].
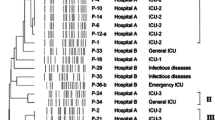
Clonality analysis
For OXA-23-producing A. baumannii isolates, the genetic relationship was studied using the DiversiLab system (bioMérieux), a semi-automated fingerprinting tool based on repetitive sequence-based PCR (rep-PCR), by following the manufacturer’s instructions. Isolates with identical strain patterns were considered to be clonally related when the similarity percentage was ≥95 %. Multilocus sequence typing (MLST) was carried out for the CPE isolates according to the Institut Pasteur’s MLST scheme (http://www.pasteur.fr/mlst).
Results
Validation of screening chromogenic media
All strains tested were detected at 18 h of incubation on the chromID® OXA-48 medium. The sensitivity of this medium is 99 %, despite the low inoculum. The specificity of detection of OXA-48-producing Enterobacteriaceae with chromID® OXA-48 is 92 % at 18 h; 98 % of the non-OXA-48-producing Enterobacteriaceae strains tested are negative. The two false-positive strains growing on the medium were IMP-producing Serratia marcescens and a vancomycin-resistant Enterococcus faecium.
Concerning the chromID® CARBA medium, the sensitivity and specificity are 68 and 95.5 %, respectively. The sensitivity is 97 % if we exclude the OXA-48-producing strains as recommended by the manufacturer.
The combination of chromID® OXA-48 and chromID® CARBA allows 99 % detection of CPE with 95 % specificity at 18 h. The false-positive results are mainly due to the growth of vancomycin-resistant E. faecium and strains resistant to carbapenem by impermeability on chromID® CARBA.
Main characteristics of the patients
A total of 1,135 specimens (1,074 stools and 61 rectal swabs) were collected during the 3-month study period. The repartition of the study population was 57 % males and the median age was 48 years (range 0–94). Of the 1,135 patients, 420 (37 %) had a previous hospitalisation or lived in a nursing home or a healthcare centre in the last year. The studied population belonged to the following wards: paediatrics (33 %, n = 375), internal medicine (27 %, n = 306), geriatrics (20 %, n = 227), surgical units (7 %, n = 79), intensive care units (7 %, n = 80), emergency (3 %, n = 34) and recovery units (3 %, n = 34).
Prevalence and identification of CR GNB
Of the 1,135 patients, 27 (2.4 %) harboured CR GNB isolates (Fig. 1). Species identified were P. aeruginosa (1.5 %, n = 17), Enterobacteriaceae (0.7 %, n = 8) and A. baumannii (0.2 %, n = 2). The prevalence of carbapenemase-producing bacteria was 0.4 % (n = 5). Two strains corresponded to OXA-23-producing A. baumannii (0.2 %) and one strain to OXA-48-producing Klebsiella pneumoniae (0.1 %) (Table 1). Based on the molecular screening, we detected two other bla OXA-48-positive samples. Repeated cultures of these positive PCR stools on the two chromogenic media and a Drigalski agar with ertapenem disc failed to identify the corresponding bla OXA-48-producing bacterium. Finally, we also found Enterobacter spp. and Escherichia coli with reduced outer membrane permeability in combination with overproduction of AmpC β-lactamase (0.3 %, n = 3).
Despite the low prevalence of digestive carriage of CPE in our population, the two media showed excellent specificities: 98.7 % for chromID® OXA-48 and 95.5 % for chromID® CARBA.
MLST and characteristics of patients colonised by CPE or carbapenemase-producing A. baumannii
The OXA-48-producing K. pneumoniae strain isolated during this study belonged to sequence type (ST) 15 (Table 1). It was detected in stools from a man hospitalised at Nîmes University Hospital and with a history of hospitalisation in Morocco. The two bla OXA-48PCR-positive samples were obtained from children hospitalised in the same paediatric unit at Toulouse University Hospital. They had no history of hospitalisation in the year before the screening and no contact with a foreign country. Concerning the A. baumannii isolates, the two OXA-23-producing strains isolated at Nîmes Hospital appeared to be genetically very close by rep-PCR typing (≥95 % similarity). They belonged to ST2. They were isolated from male patients with a long-term hospitalisation in geriatric and rehabilitation wards, respectively. In the five cases, no isolation precautions and contact screening have been prescribed while the diagnostic was after the hospitalisation. However, no other case was observed. Moreover, no clinical signs could be noted in the five carriers during the hospital stay.
Discussion
The emergence and global spread of CPE and carbapenem-resistant A. baumannii are of great concern to healthcare facilities worldwide [1]. The Mediterranean region is of interest due to a great diversity and population mixing. In this area, the prevalence of carbapenemases is particularly high, with this area constituting one of the most important reservoirs [1]. In France, episodes involving CPE remained uncommon until 2010 [11]. The identification of CPE now seems to be more and more frequent, with a notable increase in the number of cases, especially those involving K. pneumoniae, during the last two years [12]. Moreover, we could note a change in the epidemiology with the increase of CPE from patients without a history of travelling in foreign countries. In the Mediterranean area, only a few studies have investigated the prevalence of digestive carriage and were mainly conducted during outbreak periods [3, 6]. To our knowledge, our study is the first that investigates the rate of CR GNB and CPE faecal carriage in three French regions (Midi-Pyrénées, Languedoc-Roussillon, Provence-Alpes-Côte d’Azur) bordering the Mediterranean Sea.
At the time of this survey, the occurrence of CPE was very uncommon in the population hospitalised or consulting in the south of France (0.3 %), lower than that reported in Spain (1.1 %), Morocco (11 %) and Pakistan (18.3 %) [3, 5, 6]. The unique strain recovered in our study was the most widespread CPE in France and in our region: the OXA-48-producing K. pneumoniae [12, 13]. As with half of the patients colonised/infected by OXA-48-producers in France [11], the carrier had been hospitalised in Morocco in the year preceding the isolation of the strain (Casablanca University Hospital). This enzyme is widespread in this country since its first identification in 2010 [14], and has generated several outbreaks in many European countries [12, 15]. The strain belonged to ST15, an international clone predominantly associated with the spread of different ESBLs in China, central Europe and recently described as carrying the bla OXA-48 gene in Finland [15–19]. The strains detected by PCR were considered to belong to K. pneumoniae due to the prevalence of this bacteria in our region [13]. However, we could not exclude the carriage of a non-pathogenic commensal carrying the bla OXA-48 gene (e.g. Shewanella spp.). Concerning A. baumannii, the occurrence of OXA-23-producers is very low (<0.1 %). As previously described in European countries, the OXA-58- and OXA-24-producers have been replaced by OXA-23-producers [20]. In the Languedoc-Roussillon region, almost all OXA-23-producing A. baumannii strains belonged to the widespread ST2/international clone II [13], and were mainly associated with hospitalisations in long-stay units, as observed in our population. Finally, no patient carried carbapenemase-producing P. aeruginosa, bacteria very uncommon in our region.
Our study validated that the chromID® OXA-48 medium is both sensitive and highly specific for CPE detection. Moreover, the combined use of chromID® OXA-48 and chromID® CARBA should allow accurate detection of all clinically relevant carbapenemases. These results are in accordance with previous data [8, 21, 22]. Girlich et al. showed that the chromID® OXA-48 medium has the highest specificity, 100 %, as compared to 53 and 68 % for the SUPERCARBA and chromID® CARBA media, respectively for detecting those OXA-48-producers [8]. The sensitivity of chromID® CARBA was evaluated to be 96.5 and 96.9 % in two clinical studies, respectively [21, 22]. The specificity was 91.2 % at the reading level and 100.0 % after Gram staining [21]. Vrioni et al. found a greater specificity (96.9 %) [22]. All these results suggest that we used a rapid and accurate culture screening method for our study and allow to validate our low carriage prevalence. Moreover, the NucliSENS EasyQ® KPC PCR assay had also demonstrated a high sensitivity and specificity (93.3 and 99.0 %, respectively) [23].
Conclusion
The low prevalence of carbapenemase-producing Enterobacteriaceae (CPE) in this study represents a useful baseline. Despite this low level of carriage prevalence, the emergence of OXA-48-producers in other situations, including epidemic cases, is described in the south of France. This underlines the importance to maintain vigilance and control strategies including strict hand hygiene and screening of patients who may be at risk of CPE carriage (notably patients previously hospitalised in foreign countries) to prevent/limit the spread of these multidrug-resistant microorganisms.
References
Nordmann P, Naas T, Poirel L (2011) Global spread of carbapenemase-producing Enterobacteriaceae. Emerg Infect Dis 17:1791–1798
Patel G, Bonomo RA (2013) “Stormy waters ahead”: global emergence of carbapenemases. Front Microbiol 4:48
Girlich D, Bouihat N, Poirel L, Benouda A, Nordmann P (2014) High rate of faecal carriage of extended-spectrum beta-lactamase and OXA-48 carbapenemase-producing Enterobacteriaceae at a University hospital in Morocco. Clin Microbiol Infect 20:350–354
Boutet-Dubois A, Pantel A, Prère MF, Bellon O, Brieu-Roche N, Lecaillon E, Le Coustumier A, Davin-Regli A, Villeneuve L, Bouziges N, Gleize E, Lamarca R, Dunyach-Remy C, Sotto A, Lavigne JP (2013) Faecal carriage of oxyiminocephalosporin-resistant Enterobacteriaceae among paediatric units in different hospitals in the south of France. Eur J Clin Microbiol Infect Dis 32:1063–1068
Day KM, Ali S, Mirza IA, Sidjabat HE, Silvey A, Lanyon CV, Cummings SP, Abbasi SA, Raza MW, Paterson DL, Perry JD (2013) Prevalence and molecular characterization of Enterobacteriaceae producing NDM-1 carbapenemase at a military hospital in Pakistan and evaluation of two chromogenic media. Diagn Microbiol Infect Dis 75:187–191
Gijón D, Curiao T, Baquero F, Coque TM, Cantón R (2012) Fecal carriage of carbapenemase-producing Enterobacteriaceae: a hidden reservoir in hospitalized and nonhospitalized patients. J Clin Microbiol 50:1558–1563
Dévigne L, Pantel A, Bourguignon MP, Cellier M, Courbière E, Ghirardi S, Vignon V, Zambardi G, Lavigne JP (2013) First evaluation of chromID® OXA-48, a new chromogenic medium for detection of Enterobacteriaceae producing OXA-48 carbapenemase. In: Proceedings of the 23rd European Congress of Clinical Microbiology and Infectious Diseases (ECCMID), Berlin, Germany, April 2013. Available online at: https://molecularhub.org/resources/207/download/eP683-1.pdf. Accessed 10 October 2014
Girlich D, Anglade C, Zambardi G, Nordmann P (2013) Comparative evaluation of a novel chromogenic medium (chromID OXA-48) for detection of OXA-48 producing Enterobacteriaceae. Diagn Microbiol Infect Dis 77:296–300
Poirel L, Walsh TR, Cuvillier V, Nordmann P (2011) Multiplex PCR for detection of acquired carbapenemase genes. Diagn Microbiol Infect Dis 70:119–123
Woodford N, Ellington MJ, Coelho JM, Turton JF, Ward ME, Brown S, Amyes SG, Livermore DM (2006) Multiplex PCR for genes encoding prevalent OXA carbapenemases in Acinetobacter spp. Int J Antimicrob Agents 27:351–353
Vaux S, Carbonne A, Thiolet JM, Jarlier V, Coignard B; RAISIN and Expert Laboratories Groups (2011) Emergence of carbapenemase-producing Enterobacteriaceae in France, 2004 to 2011. Euro Surveill 16. pii: 19880
Robert J, Pantel A, Mérens A, Lavigne JP, Nicolas-Chanoine MH; ONERBA’s Carbapenem Resistance Study Group (2014) Incidence rates of carbapenemase-producing Enterobacteriaceae clinical isolates in France: a prospective nationwide study in 2011–12. J Antimicrob Chemother 69:2706–2712
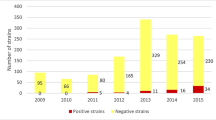
Pantel A, Boutet-Dubois A, Jean-Pierre H, Marchandin H, Sotto A, Lavigne JP; CARB-LR group (2014) French regional surveillance program of carbapenemase-producing Gram-negative bacilli: results from a 2-year period. Eur J Clin Microbiol Infect Dis 33:2285–2292. doi:10.1007/s10096-014-2189-5
Hays C, Benouda A, Poirel L, Elouennass M, Nordmann P (2012) Nosocomial occurrence of OXA-48-producing enterobacterial isolates in a Moroccan hospital. Int J Antimicrob Agents 39:545–547
Cantón R, Akóva M, Carmeli Y, Giske CG, Glupczynski Y, Gniadkowski M, Livermore DM, Miriagou V, Naas T, Rossolini GM, Samuelsen Ø, Seifert H, Woodford N, Nordmann P; European Network on Carbapenemases (2012) Rapid evolution and spread of carbapenemases among Enterobacteriaceae in Europe. Clin Microbiol Infect 18:413–431
Damjanova I, Tóth A, Pászti J, Hajbel-Vékony G, Jakab M, Berta J, Milch H, Füzi M (2008) Expansion and countrywide dissemination of ST11, ST15 and ST147 ciprofloxacin-resistant CTX-M-15-typebeta-lactamase-producing Klebsiella pneumoniae epidemic clones in Hungary in 2005—the new ‘MRSAs’? J Antimicrob Chemother 62:978–985
Wang Q, Li B, Tsang AK, Yi Y, Woo PC, Liu CH (2013) Genotypic analysis of Klebsiella pneumoniae isolates in a Beijing hospital reveals high genetic diversity and clonal population structure of drug-resistant isolates. PLoS One 8:e57091
Sánchez-Romero I, Asensio A, Oteo J, Muñoz-Algarra M, Isidoro B, Vindel A, Alvarez-Avello J, Balandín-Moreno B, Cuevas O, Fernández-Romero S, Azañedo L, Sáez D, Campos J (2012) Nosocomial outbreak of VIM-1-producing Klebsiella pneumoniae isolates of multilocus sequence type 15: molecular basis, clinical risk factors, and outcome. Antimicrob Agents Chemother 56:420–427
Österblad M, Kirveskari J, Hakanen AJ, Tissari P, Vaara M, Jalava J (2012) Carbapenemase-producing Enterobacteriaceae in Finland: the first years (2008–11). J Antimicrob Chemother 67:2860–2864
Minandri F, D’Arezzo S, Antunes LC, Pourcel C, Principe L, Petrosillo N, Visca P (2012) Evidence of diversity among epidemiologically related carbapenemase-producing Acinetobacter baumannii strains belonging to international clonal lineage II. J Clin Microbiol 50:590–597
Papadimitriou-Olivgeris M, Bartzavali C, Christofidou M, Bereksi N, Hey J, Zambardi G, Spiliopoulou I (2014) Performance of chromID® CARBA medium for carbapenemases-producing Enterobacteriaceae detection during rectal screening. Eur J Clin Microbiol Infect Dis 33:35–40
Vrioni G, Daniil I, Voulgari E, Ranellou K, Koumaki V, Ghirardi S, Kimouli M, Zambardi G, Tsakris A (2012) Comparative evaluation of a prototype chromogenic medium (ChromID CARBA) for detecting carbapenemase-producing Enterobacteriaceae in surveillance rectal swabs. J Clin Microbiol 50:1841–1846
McEwan AS, Derome A, Meunier D, Burns PJ, Woodford N, Dodgson AR (2013) Evaluation of the NucliSENS EasyQ KPC assay for detection of Klebsiella pneumoniae carbapenemase-producing Enterobacteriaceae. J Clin Microbiol 51:1948–1950
Acknowledgements
This work was supported by University Montpellier 1 and the French National Institute of Health and Medical Research (INSERM).
We thank bioMérieux for providing us the different screening media and the NucliSENS EasyQ® KPC kits.
Conflict of interest
The authors report no conflicting interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pantel, A., Marchandin, H., Prère, MF. et al. Faecal carriage of carbapenemase-producing Gram-negative bacilli in hospital settings in southern France. Eur J Clin Microbiol Infect Dis 34, 899–904 (2015). https://doi.org/10.1007/s10096-014-2298-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-014-2298-1