Abstract
Since 2002, the Belgian Antibiotic Policy Coordination Committee (BAPCOC) has supported the development of antibiotic management teams (AMTs) in Belgian hospitals with policy guidance and federal funding for antibiotic managers. We report on the analysis of the activity reports for the year 2011 and compare the results with those for 2007. A structured questionnaire survey was performed on the composition, organisation and service activities of the AMT in all acute care and larger chronic care hospitals in the country in 2011. Descriptive statistics were stratified by duration of AMT funding. Completed questionnaires were provided by 105 of 109 hospitals (response rate 96.3 %). The AMTs have further formalised their working method over the previous years. Significantly higher implementation rates were achieved in 2011 for concurrent review for antibiotic therapies (92.0 % in 2011 vs. 64.2 % in 2007), for the de-escalation of therapy after a few days (93.0 % in 2011 vs. 63.9 % in 2007) and for sequential i.v.-oral therapy for antibiotics with equivalent bioavailability (86.0 % in 2011 vs. 78.7 % in 2007). The AMTs who first joined the project were able to maintain their activities at a high level, while those who last joined the national project in 2007 made considerable progress 4 years later. This has also resulted in significantly higher implementation rates for the totality of the acute care hospitals. The presence of AMTs in all hospitals also proves to be a great boon when setting up projects, surveys and studies on a(n) (inter)national level.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antimicrobial resistance has increased dramatically in healthcare settings and in the community, and is considered to be an extremely serious issue by the World Health Organization (WHO) [1–3]. The European Centre for Disease Prevention and Control (ECDC) reported that 25,000 people die each year from antibiotic-resistant bacteria in EU Member States and that multidrug-resistant organisms (MDROs) result in extra healthcare costs and productivity losses of at least 1.5 billion Euros each year in Europe [4]. The major driving force for the development of resistance is the misuse and overuse of antibiotics in human and non-human medicine. Antibiotic management teams (AMTs) have been advocated as an excellent approach to optimise the use of antimicrobial drugs in hospitals. They strive to support clinical practitioners to avoid the inappropriate use of antibiotics and optimise their choice, dosing, route and duration of administration, with the aim of improving patient outcomes, promoting cost-effective therapy, avoiding adverse effects and reducing levels of resistance [5–12].
In 2010, we reported on the nationwide implementation of AMTs in all acute care hospitals and a few of the larger chronic care hospitals by the Belgian Antibiotic Policy Coordination Committee (BAPCOC) [9]. These AMTs are positioned as a subgroup within the Drugs and Therapeutics Committee of their institution. Their composition, mandate and tasks have been consolidated in the legislation on hospitals and an annual budget of 3.6 million Euros is divided among these hospitals according to the number of beds. The BAPCOC and the Belgian Scientific Institute of Public Health (known as WIV-ISP) lend support and guidance to the AMTs in the form of an advanced training course on antibiotic policy, national study days on related topics, feedback reports based on the analysis of the activity reports of the AMTs and a web-based national surveillance of hospital antibiotic consumption. Analysis of the activity reports for the year 2007 led us to conclude that the AMTs were well developed and provided a broad range of services, such as the development of an antibiotic formulary and therapeutic and prophylactic guidelines, and the analysis of local data on antibiotic consumption and microbial resistance [9].
This time, we report on the analysis of the activity reports of the acute care hospitals for the year 2011 and compared the results with previous years.
Materials and methods
The AMTs must provide yearly activity reports by the use of a standardised questionnaire, so that the BAPCOC can monitor their organisation, local objectives and delivery of services [9]. The questionnaire included inter alia questions on the following topics: members of the AMT; strategic plan; and implementation of antibiotic stewardship initiatives, such as the antibiotic formulary and clinical practice guidelines, prescription guidance and support tools, and the analysis of antibiotic consumption and microbial resistance.
In January 2011, 109 hospitals were entitled to financial support for their AMT. The BAPCOC received activity reports from 105 of these hospitals (response rate, 96.3 %): 100/103 acute care hospitals and 5/6 chronic care hospitals with at least 150 beds. Table 1 shows the distribution of the acute care hospitals in 2011, according to the number of beds and the time at which they first received financial support for their AMT.
Results
The mean number of members of the AMTs in acute care hospitals was 11.5 (10 in 2007). The AMTs have further formalised their working method over the previous years: the majority of the AMTs defined their activities and goals for the upcoming year (94.0 % in 2011 vs. 83.0 % in 2007) and for a longer period (78.0 vs. 58.9 %), and almost all AMTs evaluated their initiatives and outcomes of the previous year (94.0 vs. 71.4 %).
Table 2 presents an overview of the implementation of antibiotic stewardship initiatives in the acute care hospitals in 2011, according to the time at which they first received financial support for their AMT and the number of beds.
The evolution of the degree of implementation of antibiotic stewardship initiatives in the acute care hospitals from 2007 to 2011 is presented in Table 3. In 2010, only a summary analysis has been done and, therefore, these results are not mentioned.
In almost all acute care hospitals, an antibiotic formulary and clinical practice guidelines for antibiotic therapy and prophylaxis were already available in 2007 (96.3, 91.6 and 96.3 %, respectively), and that was still the case in 2011 (97.0, 91.0 and 93.0 %, respectively). Likewise, almost all AMTs were already analysing their antibiotic consumption and microbial resistance in 2007 (96.2 and 89.8 %, respectively), and they continued doing so in 2011 (97.0 and 96.0 %, respectively).
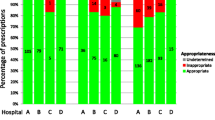
The number of hospitals that have defined a list of ‘restricted’ antimicrobial agents which require justification for their use and either prior approval or post hoc review by a member of the AMT for delivery by the hospital pharmacy had not changed much between 2007 (75.9 %) and 2011 (79 %). However, when we look at the hospitals who first received financial support for an AMT in 2007 (group C), we notice a significant improvement (58.3 % in 2007 vs. 72.7 % in 2011 (see Table 4).
When we compare the situation in 2011 with that in 2007, significantly higher implementation rates were achieved in 2011 for prospective audit, whereby antibiotic therapies for certain indications or for patients on certain units are checked daily by a member of the AMT, with immediate feedback to the prescriber in the case of inappropriate therapy (92.0 % in 2011 vs. 64.2 % in 2007), for the promotion of de-escalation of therapy after a few days on the basis of clinical evolution and microbiological results for certain indications or for patients on certain units (93.0 vs. 63.9 %), and for the promotion of rapid parenteral to oral conversion for antibiotics with equivalent bioavailability (86.0 vs. 78.7 %). These improvements are largely the result of the efforts over the previous years of the hospitals in group C; from 42.5 % in 2007 to 84.1 % in 2011 for prospective audit, from 50.0 to 88.6 % for the promotion of de-escalation of therapy and from 66.7 to 79.5 % for the promotion of rapid parenteral to oral conversion (see Table 4).
Antimicrobial order forms (47.0 % in 2011 vs. 36.1 % in 2007) and automatic stop of delivery of the antibiotic after a defined number of days (52.0 % vs. 43.5 %) are on the rise, but still only half the hospitals use them. Again, these changes are largely due to increases in group C hospitals; from 22.9 % in 2007 to 40.9 % in 2011 for antimicrobial order forms and from 25.0 to 40.9 % for automatic stop orders.
Discussion
Based on the analysis of the activity reports, we concluded in our previous publication that the AMTs were already well developed in 2007 and were able to provide a broad range of services [9]. This was the year in which a considerable group of hospitals had joined the project and for this group C, the situation in 2007 can, thus, be regarded as the baseline. It is no surprise then that these hospitals scored lower for the implementation of several antimicrobial stewardship initiatives compared with the other hospitals who had joined previously.
Four years later, we notice that the hospitals that joined the project in 2007 have made considerable progress. Significant improvements are noted for the requirement of justification and/or authorisation for specific antibiotics (58.3 % in 2007 vs. 72.7 % in 2011), prospective audit with intervention and feedback (42.5 vs. 84.1 %), promotion of de-escalation of therapy (50.0 vs. 88.6 %) and promotion of rapid parenteral to oral conversion (66.7 vs. 79.5 %). For the last three items, this has also resulted in significantly higher implementation rates for the totality of the acute care hospitals.
Based on these excellent results of the annual reports of all acute care hospitals, the Hospital Medicine Working Group of the BAPCOC decided to implement a brief annual report, focusing more on audits and the training of healthcare professionals. For this reason, no recent data are available from all acute care hospitals since 2011. Some experiences with antimicrobial stewardship in other European countries have been published over the last few years. A cross-sectional survey of the profile and activities of AMTs in Irish hospitals shows that around half of the responding hospitals (43 %) do not have an AMT in place but most of them have an antimicrobial management prescribing policy (88 %). Four in five of these hospitals monitor antibiotic consumption; almost half of them conduct audits to measure appropriate prescribing of all antibiotics (47 %) and of restricted antibiotics (43 %) [13].
The Scottish Antimicrobial Prescribing group (SAPG) was established by the Scottish Government in 2008 to lead the first national initiative to actively address antimicrobial stewardship [14]. The SAPG developed national prescribing indicators based on compliance with local antibiotic policies to support the reduction of Clostridium difficile infections (CDI). Surgical prophylaxis and management of sepsis are their next national priorities for improvement in hospital care settings [14, 15].
French hospitals are required to implement antibiotic stewardship programmes (ABS) to improve antibiotic use. In 2008, at least 98 % of hospitals had implemented formularies, antibiotic committees, surgical prophylaxis guidelines and monitored antibiotic use; antibiotic advisors were appointed in 85 % of hospitals but audits remained under-used [16].
The creation of the AMTs also offers organisational benefits on a national level. Indeed, it proves much easier for the BAPCOC to set up nationwide studies and projects. This is clearly illustrated by the high rate of participation of Belgian hospitals (52.5 %) in the European point prevalence survey on healthcare-associated infections and antibiotic use in 2011. The BAPCOC invited all Belgian acute care hospitals to participate in the survey, organised an information session and provided additional funding (80,000 Euros) for participating hospitals. Another recent example is the organisation by the BAPCOC of a nationwide clinical audit on perioperative antibiotic prophylaxis (PAP) in October–November 2013, in which the AMTs had a leading role. Seventy-eight acute care hospitals (74.3 %) voluntarily performed this internal audit and sent their data to the BAPCOC. The results were presented and discussed during a workshop on PAP in January 2014.
The Hospital Medicine Working Group of the BAPCOC is in the process of defining new objectives for the next 5 years. Based on the recent experience with the clinical audit on perioperative antibiotic prophylaxis, AMTs in acute care hospitals will be obliged to participate in national audits on topics related to antibiotic policy. Each audit on a specific topic will be performed on two separate occasions (baseline and after intervention) so as to be an integral part of a plan–do–study–act (PDSA) cycle in the hospital. When appropriate, specific targets will be set by the Working Group.
The Hospital Medicine Working Group also encourages the AMTs to participate in international studies. At the end of October 2014, the AMTs were invited to participate at the Global Point Prevalence Survey of Antimicrobial Consumption and Resistance (Global PPS) that will take place in spring 2015.
Furthermore, the analyses of the reports and the clinical audit on perioperative antibiotic prophylaxis shows that there is a need to develop a national antibiotic guide for hospitals; this is also one of our priorities the next several years.
As of 2009, the BAPCOC and the Scientific Institute of Public Health (WIV-ISP) implemented a web-based national surveillance programme for hospital antibiotic consumption, providing the hospitals with standardised feedback data [expressed as defined daily doses (DDDs) per 1,000 bed-days and DDDs per 1,000 admissions]. In the new strategic approach, we wish to further expand the functionality of this surveillance and realise cross-institutional benchmarking. In conclusion, while the AMTs of groups A and B were able to maintain their activities at a high level, those of group C have made considerable progress since 2007, the year in which they joined the national project.
References
Carlet J, Jarlier V, Harbarth S, Voss A, Goossens H, Pittet D (2012) Ready for a world without antibiotics? The Pensières Antibiotic Resistance Call to Action. Antimicrob Resist Infect Control 1:11
Carlet J, Pittet D (2013) Access to antibiotics: a safety and equity challenge for the next decade. Antimicrob Resist Infect Control 2:1
World Health Organization (WHO) (2012) The evolving threat of antimicrobial resistance—options for actions. WHO, Geneva. Available online at: http://whqlibdoc.who.int/publications/2012/9789241503181_eng.pdf. Accessed 14 December 2012
European Centre for Disease Prevention and Control (ECDC), European Medicines Agency (EMEA) (2009) ECDC/EMEA Joint Technical Report: The bacterial challenge: time to react. EMEA/576176/2009. Available online at: http://www.ema.europa.eu/docs/en_GB/document_library/Report/2009/11/WC500008770.pdf
Owens RC Jr (2008) Antimicrobial stewardship: concepts and strategies in the 21st century. Diagn Microbiol Infect Dis 61:110–128
Dellit TH, Owens RC, McGowan JE Jr, Gerding DN, Weinstein RA, Burke JP, Huskins WC, Paterson DL, Fishman NO, Carpenter CF, Brennan PJ, Billeter M, Hooton TM; Infectious Diseases Society of America; Society for Healthcare Epidemiology of America (2007) Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis 44:159–177
MacDougall C, Polk RE (2005) Antimicrobial stewardship programs in health care systems. Clin Microbiol Rev 18:638–656
Lesprit P, Brun-Buisson C (2008) Hospital antibiotic stewardship. Curr Opin Infect Dis 21:344–349
Van Gastel E, Costers M, Peetermans WE, Struelens MJ (2010) Nationwide implementation of antibiotic management teams in Belgian hospitals: a self-reporting survey. J Antimicrob Chemother 65:576–580
Fridkin S, Baggs J, Fagan R, Magill S, Pollack LA, Malpiedi P, Slayton R, Khader K, Rubin MA, Jones M, Samore MH, Dumyati G, Dodds-Ashley E, Meek J, Yousey-Hindes K, Jernigan J, Shehab N, Herrera R, McDonald CL, Schneider A, Srinivasan A; Centers for Disease Control and Prevention (CDC) (2014) Vital signs: improving antibiotic use among hospitalized patients. MMWR Morb Mortal Wkly Rep 63(9):194–200
Pogue JM, Mynatt RP, Marchaim D, Zhao JJ, Barr VO, Moshos J, Sunkara B, Chopra T, Chidurala S, Kaye KS (2014) Automated alerts coupled with antimicrobial stewardship intervention lead to decreases in length of stay in patients with gram-negative bacteremia. Infect Control Hosp Epidemiol 35(2):132–138
Avdic E, Cushinotto LA, Hughes AH, Hansen AR, Efird LE, Bartlett JG, Cosgrove SE (2012) Impact of an antimicrobial stewardship intervention on shortening the duration of therapy for community-acquired pneumonia. Clin Infect Dis 54(11):1581–1587
Fleming A, Tonna A, O’Connor S, Byrne S, Stewart D (2014) A cross-sectional survey of the profile and activities of Antimicrobial Management Teams in Irish Hospitals. Int J Clin Pharm 36(2):377–383
Nathwani D, Sneddon J, Malcolm W, Wiuff C, Patton A, Hurding S, Eastaway A, Seaton RA, Watson E, Gillies E, Davey P, Bennie M; Scottish Antimicrobial Prescribing Group (2011) Scottish Antimicrobial Prescribing Group (SAPG): development and impact of the Scottish National Antimicrobial Stewardship Programme. Int J Antimicrob Agents 38(1):16–26
Nathwani D, Sneddon J, Patton A, Malcolm W (2012) Antimicrobial stewardship in Scotland: impact of a national programme. Antimicrob Resist Infect Control 1:7
Dumartin C, Rogues A-M, Amadeo B, Pefau M, Venier A-G, Parneix P, Maurain C (2011) Antibiotic stewardship programmes: legal framework and structure and process indicator in Southwestern French hospitals, 2005–2008. J Hosp Infect 77(2):123–128
Acknowledgements
We thank the other members of the Hospital Medicine Working Group of the Belgian Antibiotic Policy Coordination Committee: Jan Verhaegen; Steven Callens; Stefaan Vande Casteele; Franky Buyle; Patrick Lacor; Mark DeJongh; Benedicte Delaere; Yves Van Laethem; Danielle Govaerts; Baudouin Byl; Christine Ernes; Anne Ingenbleek; Dirk Vogelaers; Hector Rodriguez; Willy Peetermans; Youri Gluczynski; Boudewijn Catry; Camelia Rossi; Christelle Verchevalle; Frédéric Frippiat; Hilde Jansens; Olivier Denis.
Funding
The data have been generated as part of the routine work of the Hospital Medicine Working Group of the Belgian Antibiotic Policy Coordination Committee. No specific funding has been received to perform the survey or the analysis of the data.
Conflict of interest
E.V.G.: none to declare.
E.B.: none to declare.
M.C.: none to declare.
K.M.: none to declare.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Van Gastel, E., Balligand, E., Costers, M. et al. Antibiotic management teams in Belgian hospitals: continued improvement in the period from 2007 to 2011. Eur J Clin Microbiol Infect Dis 34, 673–677 (2015). https://doi.org/10.1007/s10096-014-2279-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-014-2279-4