Abstract
Background
Epidemiological studies on predisposing conditions and outcomes of progressive multifocal leukoencephalopathy (PML) cases have been carried out exclusively in high-income countries. We aim to report and compare the main characteristics and outcomes of patients with PML and several underlying diseases in a referral center in a middle-income country.
Methods
We performed a retrospective cohort study of PML cases admitted to a tertiary care hospital in São Paulo, Brazil during 2000–2022. Demographic and PML-specific variables were recorded. One-year case-fatality rate and factors associated with death were identified using a multivariate Cox proportional hazards regression model.
Results
Ninety-nine patients with PML were included. HIV infection (84.8%) and malignancy (14.1%) were the most prevalent underlying conditions. Other predisposing diseases were autoimmune/inflammatory diseases (5.1%) and solid organ transplantation (1.0%). One (1.0%) patient had liver cirrhosis and another (1.0%) patient was previously healthy. Focal motor deficits (64.2%) and gait instability (55.1%) were the most common signs. The one-year case-fatality rate was 52.5% (95% CI 42.2–62.7). The one-year case-fatality rate (95% CI) in patients with or without malignancy (85.7%, 95% CI 57.2–98.2% and 47.1%, 95% CI 36.1–58.2%, respectively) were statistically different (P = 0.009). Crude and adjusted Cox regression models identified malignancy as independently associated with death (adjusted HR = 3.92, 95% CI 1.76–8.73, P = 0.001).
Conclusions
HIV/AIDS was the predisposing condition in 84.8% of PML cases. The one-year case-fatality rate was 52.5% and having a malignancy was independently associated with death. This study reports emerging data on the epidemiology and outcome of PML in a middle-income country.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Progressive multifocal leukoencephalopathy (PML) is a severe demyelinating disease of the central nervous system (CNS) caused by the JC virus (JCV) [1]. Despite JCV infection being common in the adult population worldwide, PML remains a rare disease occurring almost exclusively in immunosuppressed individuals [2]. Furthermore, few PML cohorts, most of which are restricted to people living with HIV/AIDS (PLWHA), have been described in low- and middle-income countries [3]. In these settings, there are no published cohorts on PML in non-HIV-infected individuals.
The predominant risk factor underlying PML has changed over time since the first cases of the disease were described in 1958 [4], with four “epochs” describing the history of PML to the present: (i) predominance of individuals with hematological malignancies, particularly B cell disorders, before the AIDS pandemic; (ii) predominance of individuals with advanced HIV disease in the pre-combined antiretroviral therapy (cART) era; (iii) predominance of individuals with advanced HIV disease in the post-combined antiretroviral therapy (cART) era with a dramatic reduction in the incidence of PML; and (iv) predominance of individuals with advanced HIV disease combined with the appearance of PML in individuals receiving natalizumab or other immunomodulatory therapies [2, 5].
This history is based on data from the US and Western Europe, whereas little information on PML has been reported from low- and middle-income countries where the AIDS epidemic remains a public health problem, including in Latin America. Some reasons for the purported low incidence of PML in low- and middle-income income countries (LMICs) include underdiagnosis [i.e., low autopsy rates, unavailability of or limited access to neuroimaging, particularly magnetic resonance imaging (MRI), and to molecular diagnostics from cerebrospinal fluid (CSF)], underreporting, and higher morbidity and mortality related to other common infections (i.e., tuberculosis, bacterial infections, cerebral toxoplasmosis). In addition, biological variables as differences in viral strains (i.e. high prevalence of HIV Clade C in India and Africa), HIV and JCV interactions, variability in host susceptibility, and variable pathogenic potential of some JCV strains were postulated as potential causes of low PML incidence in low-income countries [6, 7]. Nowadays, available evidence does not suggest the presence of biological factors that justify the concept of low incidence or non-existence of PML in some settings [7,8,9]. For example, a study from India, where HIV clade C is predominant, showed that PML cases presented no significant differences in clinical, radiological, and pathological features when compared to patients in the US and Western Europe where HIV clade B is most common. Probably the main reason for the low incidence of PML in low- and middle-income countries is the lack of diagnostic tools. In this line, studies carried out over last decade in some tertiary centers in Africa [7], Asia [9] and Latin America [10] using molecular diagnostics in CSF and/or MRI suggest that HIV-related PML is not as uncommon as previously reported. Despite this, there is a paucity of information from large series of PML in PLWHA in LMICs and reports of PML in hosts with other underlying immunosuppressive conditions (rheumatological diseases, hematological malignancies, chronic inflammatory diseases, solid organ transplantation, and primary immunodeficiency) [11] are even rarer.
We aimed to report the main features and outcomes of patients with PML and several underlying conditions in a tertiary care hospital in São Paulo, Brazil, over a 20-year period.
Methods
This study was designed and reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Study design, setting and data collection
This was a retrospective cohort study of all patients with PML admitted to the Instituto Central of the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (HCFMUSP) in São Paulo, Brazil between January 2000 and December 2022. The Instituto Central has 900 beds and is the main public tertiary referral center in the State of São Paulo. Patients were identified from: (i) the database of the Virology Laboratory of Instituto de Medicina Tropical de São Paulo (IMT), where JCV PCR in CSF samples were assayed; and (ii) the database of autopsies carried out in HCFMUSP. The IMT was the only laboratory to carry out the molecular diagnostic testing for JCV during the study period. Electronic and physical medical records were reviewed, including clinical, neuroradiologic and laboratory data, to classify patients according to the American Academy of Neurology diagnostic criteria for PML [12].
Clinical characteristics
Variables of interest included sex, date of birth, date of hospital admission, date of discharge to home, date of death, date of PML-related symptom onset, date of PML diagnosis, clinical outcome, presenting symptoms, HIV infection status, malignancy status, transplantation status, autoimmune disease status, immunosuppressive medications, CSF profile, neuroimaging, and treatment history. We define oncohematological disease as the presence of malignancy (hematological or solid tumor), in order to increase the number of cases of this variable, and considering that these two groups of diseases have similar outcomes previously reported [11]. For patients who were HIV infected, lymphocytes T-CD4 + count and HIV viral load at the time of PML diagnosis, and after 3, 6, and 12 months of hospital admission were included. Neuroimaging description were documented according to the reports made by neuroimaging specialists or annotations in medical charts.
Statistical analyses
There was no formal sample size calculation, otherwise a convenience sampling of consecutive cases of PML. Median (interquartile range -IQR-) and frequencies were used when appropriate. Quantitative variables were compared using t-Student’s test with or without correction for homogeneous variance and categorical variables using the Chi-square (χ2) test or Fisher’s exact test when appropriate. Log-rank test and Cox proportional hazards model were used for survival analysis. The one-year all-cause mortality rate was defined as the number of deaths occurring within 12 months following the date of hospital admission. To estimate the case-fatality rate at 3, 6 and 12 months, we considered the worst case scenario, as lost-to-follow-up equal to death cases. Ninety-five percent confidence intervals (95% CI) were calculated for each variable. A parsimonious multivariate model was created with one-year mortality as the outcome and sex (male/female), age (years), diagnosis of HIV/AIDS (yes/no) and diagnosis of malignancy (yes/no) as the predictors, according to a prior study [13]. A sensitivity analysis excluding three patients with possible PML was performed. All assumptions of normality, homogeneity of variances, and proportionality of hazards were evaluated. The Chi-squared goodness-of-fit tests for the proportional hazards regression model, as well as Schoenfeld residuals, were used for this purpose. Survival curves (for the total population and for defined subgroups) at one-year were displayed using Kaplan–Meier plots of cumulative survival probabilities following hospital admission. All tests used were two-tailed and the significance level was P < 0.05. All statistical analysis were performed with the software SPSS 24.0 (IBM Corp., Armonk, NY, EUA).
Ethical approval
This study was approved by the Clinical Research Ethics Committee of HCFMUSP (approval code: 76445323.8.0000.0068).
Data availability
Data will be made available upon reasonable request by qualified investigators and subject to ethics board approvals.
Results
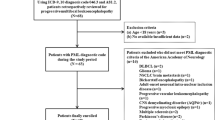
We identified 113 potentially eligible cases. Ninety-eight (86.7%) cases had an initial report of a positive CSF JCV PCR, but 17 (15.0%) were excluded due to insufficient clinical and neuroradiological information (n = 7); inability to locate medical records (n = 6); and presence of BK virus instead of JCV (n = 4). Fifteen (13.2%) cases, all of whom were included, had a histopathological diagnosis of PML. Three (2.7%) patients with advanced HIV disease and clinical and neuroimaging findings typical of PML were inadvertently included (protocol deviation). Thus, 99 patients were included.
Patients characteristics
Most patients were male (69.7%) and the median age at the time of hospital admission was 41 years (range 12 – 89) (Table 1). Patients with HIV/AIDS were slightly younger than patients without HIV/AIDS, but this difference was not statistically significant (median ages of 41 and 47.5 years, respectively, P = 0.224). Classification of PML by diagnosis category showed 82 (82.8%) patients with definite PML, 14 (14.1) with probable PML and 3 (3.0%) with possible PML. The majority of patients were white (78.8%) (Table 1). Almost half of PML diagnoses (44%) were made between 2010–2014 (Fig. 1).
Underlying conditions
Eighty-five percent of patients (85.8%) had HIV/AIDS (Table 2). Among PLWHA, 43.7% (31/71) reported cART use (regular or irregular) at hospital admission and only 11 (11.1%) patients had an undetectable HIV viral load at admission. The median (IQR) of lymphocytes T-CD4 + count (n = 81) at the time of PML diagnosis was 58 cells/µl (23.0–155.0) (Table 2). Of those, 33 (40.7%) patients had lymphocytes T-CD4 + count < 50 cell/µl, 38 (46.9%) patients had lymphocytes T-CD4 + count between 50–200 cells/µl and 10 (12.3%) patients had lymphocytes T-CD4 + count > 200 cells/µl. In 33 (39.8%) of 83 PLWHA, PML was the AIDS-defining disease. Eight (9.4%) PLWHA had an underlying malignancy: Kaposi’s sarcoma (n = 4), non-Hodgkin’s lymphoma (n = 3), and seminoma (n = 1).
Fourteen (14.1%) patients did not have HIV/AIDS (Table 2) and 6 (42.9%) of them had an underlying oncohematological disease: acute myeloid leukemia (n = 2), non-Hodgkin’s lymphoma (n = 2) and multiple myeloma (n = 2). Two patients with underlying oncohematological diseases underwent allogenic stem cell transplantation prior to the diagnosis of PML. Eight (57.1%) patients had other underlying diseases or conditions.
Two patients had systemic erythematosus lupus, which one patient was treated with azathioprine plus prednisone and the other with hydroxychloroquine and prednisone. Three patients had inflammatory diseases, one of whom had Devic's disease treated with methylprednisolone, cyclophosphamide and plasmapheresis. One patient had cerebral amyloid angiopathy related inflammation (CAA-RI) and underwent treatment with prednisone, pulse methylprednisolone and cyclophosphamide. The last patient with inflammatory disease had an unspecified demyelinating disease of the CNS, and received methylprednisolone, azathioprine and prednisone. The other 3 patients did not have oncohematological or autoimmune / inflammatory disease. One patient underwent a kidney transplantation 16 months prior to the diagnosis of PML and received tacrolimus, everolimus and prednisone. One patient had liver cirrhosis, secondary to hepatitis C, and received two doses of interferon-alpha. Finally, one patient with PML did not have any comorbidity identified or immunosuppression condition.
Clinical, laboratory and neuroradiological manifestations
The median (IQR) time between symptom onset and hospital admission was similar in patients with (30, 9–60 days] or without HIV/AIDS (30, 1–60 days) (P = 0.910).
The median (IQR) time of hospitalization was 51 (43–59) days. Focal motor deficits (64.2%), gait instability (55.1%), and psychomotor slowing (50.0%) were the most common clinical manifestations (Table 3). These and other abnormalities (i.e., limb incoordination, speech deficits, seizures) were more common in PLWHA, but none of the differences were statistically significant. Headache, paresthesias, and visual deficits were more common in non-HIV/AIDS patients, but none of the differences were statistically significant.
Basic cerebrospinal (CSF) characteristics (leukocyte count, glucose, and protein) were available for 86 (86.9%) patients. Median (IQR) leukocytes count, protein, and glucose were 3.5 cells/mm3 (1.0–15.5), 55 mg/dL (31.0–98.0), and 52 mg/dL (IQR 46.0–60.5), respectively. No CSF parameter showed statistically significantly differences between patients with or without HIV/AIDS. On MRI, areas of increased signal on T2-weighted and fluid attenuated inversion recovery (FLAIR) sequences were described in 71 (82.8%) of 82 patients. The 17 (17.2%) patients without MRI findings had histopathological confirmation of PML.
Outcomes
In hospital case-fatality ratio following hospital admission was 39.4% (95% CI 29.7–49.7) for the whole cohort. In hospital case-fatality ratio (95% CI) in HIV/AIDS patients (41.2%, 30.6–52.4) and in non-HIV/AIDS patients (28.6%, 8.4–58.1), were not statistically different (P = 0.556). In hospital case-fatality ratio (95% CI) in oncohematological patients (64.3%, 35.1–87.2) and in nononcohematological patients (5.3%, 25.2–46.4) were not statistically different (P = 0.073). Neurological sequelae at discharge was reported in 72.2% (39/54) and rates in HIV/AIDS patients and non-HIV/AIDS were 72.7% (32/44) and 70.0% (7/10), respectively (P = 0.501). Nosocomial pneumonia was the most frequent cause of in hospital death (16/40, 40%). These 16 deaths occurred in HIV/AIDS patients and none in patients without this condition (P = 0.432).
Twelve (20%) out of the 60 patients who were discharged from the hospital, lost to follow-up within the first year after PML diagnosis. During a mean follow-up of 9.3 (95% CI 7.9–10.6) months and 21,393 person-day, we found an incidence of 3.1 (95% CI 2.4–3.9) deaths per 1,000 person-day. One-year case-fatality ratio (95% CI) following hospital admission was 52.5% (42.2–62.7) for the whole cohort. In patients with HIV/AIDS, (17,643 person-days), we found an incidence of 3.7 (95% CI 2.9–4.8) deaths per 1,000 person-day. In patients without HIV/AIDS (3,750 person-days), we found an incidence of 17.6 (95% CI 13.6–22.4) deaths per 1,000 person-days.
One-year case-fatality ratio (95% CI) in HIV/AIDS patients (54.1%, 42.9–65.0) and in non-HIV/AIDS patients (42.9%, 17.7–71.1), were not statistically different (P = 0.556). One year case-fatality ratio (95% CI) in oncohematological patients (85.7%, 57.2–98.2%) and in non-oncohematological patients (47.1%, 36.1–58.2%) were statistically different (P = 0.009). Case-fatality ratios of the patients of this study by follow-up period is showed in Fig. 2.
Kaplan–Meier survival curves for the entire study population and for the two subgroups of underlying diseases are presented in Fig. 3. Crude and adjusted Cox regression models identified oncohematological diseases as independently associated with death (adjusted HR = 3.92, 95% CI 1.76–8.73. P = 0.001) (Table 4). The sensitivity analysis that excluded the 3 cases with possible PML showed similar results to the main analysis (adjusted HR = 3.82, 95% CI 1.71–8.51, P = 0.001).
Survival curves at one year following progressive multifocal leukoencephalopathy in individuals admitted at Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo, 2000–2022. A Survival curve for the entire study population (n = 99). B Survival curve of subgroups of patients with or without HIV/AIDS. C Survival curve of subgroups of patients with or without onco-hematological diseases
Discussion
This study showed that PML occurs in a broad spectrum of predisposing conditions in Brazil, but HIV/AIDS is the most important of them. Clinical outcomes of our PML cases were similar to those described in high-income countries. To the best of our knowledge, the present study is the first carried out in low- and middle-income countries to report the spectrum of predisposing conditions of PML.
Most studies about PML have evaluated specific populations of patients at risk, mainly HIV/AIDS infection or use of monoclonal antibodies. Population-based studies of PML epidemiology remain scarce, since PML is considered to be rare in the general population [14]. However, studies with several designs have analysed the spectrum of PML predisposing conditions from a local to a national scale. Table 5 shows selected studies, carried out since 2000, that simultaneously included several hosts with PML. Four were carried-out in the U.S [15,16,17,18], three in Scandinavia [13, 19,20,21], two in Asia [22, 23], and two in western Europe [11, 24]. All these studies were performed in high-income countries. Our results suggest that HIV/AIDS is the most common underlying condition in cases of PML in Brazil and probably in other epidemiologically similar settings. As expected, the vast majority of PML cases occurred in PLWHA with advanced HIV disease, confirming the opportunistic nature of this disease. In contrast, HIV-related PML has been rarely observed in the last decade in some high-income countries, while in the same period an increase in chronic inflammatory diseases-related PML, particularly when monoclonal antibodies are used [21].
Globally, HIV/AIDS is the main underlying condition of PML in most [11, 15, 18, 23, 24] but not in all studies [19, 21, 22]. When HIV/AIDS was the most common predisposing condition for PML, this proportion varied between 44 and 84.1% [11, 15]. Some arguments may explain the ongoing importance of HIV/AIDS as the main risk factor for PML in our setting. First, despite important advances in prevention and treatment, the HIV epidemic continues to be a major public health issue in Brazil when compared with other epidemiological scenarios [20,21,22]. Second, the proportion of individuals with advanced HIV disease at the time of HIV diagnosis or re-engagement in care continues to be high in Brazil [25]. Third, HIV-related PML is a well-known opportunistic disease in tertiary care centers in Brazil for which laboratory confirmation is readily available [3, 10]. Fourth, PML is probably more underdiagnosed and underreported in patients with predisposing conditions other than HIV. Nowadays, the availability of diagnostic tools to confirm PML continues to be very restricted in most health services in Brazil. Finally, PML has been an emerging concern in patients using some monoclonal antibody therapies, mainly natalizumab, but these medications were introduced late and are less used in Brazil when compared with high-income countries.
Well-established risk factors for PML in HIV-negative patients include.
hematological malignancies, organ transplantation, immunomodulatory therapy, autoimmune disorders, and primary immunodeficiency disorders [1, 2, 26]. Classically, the second most significant risk factor for the development of PML has been hematologic malignancies, but the proportion of PML cases attributed to this condition is varied able (4.5—61.3%) [11, 13, 15,16,17,18,19, 21, 23]. In fact, hematological malignancies were more frequent than HIV/AIDS in some studies [19, 22].
Other risk factors for PML as autoimmune diseases, inflammatory diseases, and organ solid transplantation were less common in the present study, similarly to previously described [11, 13, 17,18,19, 23, 24, 27].
Some studies described non-hematological malignancies as the underlying condition for PML range in frequency from 2.8 to 23.4% [11, 13, 15, 17,18,19, 22, 23]. As expected, the use of chemotherapy is common in this scenario, which appears to have a synergistic effect on the development of PML. Thus, concomitant risk factors for PML usually coexist and a similar rational can be speculated in patients with underlying conditions who required transplantation or in patients with HIV/AIDS with Kaposi’s sarcoma and use of chemotherapy [11, 13, 19, 23].
The risk for PML is not equal among immunosuppressive agents and the presence of confounding factors are common. Three classes of drug that vary by PML risk, latency to infection, and underlying illness had been stratified with natalizumab as the prototype of Class 1 that unequivocally increases the risk of PML in individuals without known disorders that predispose to PML [28]. Unlike other studies [11, 16, 22] we did not report any case with multiple sclerosis and the use of natalizumab [29]. The recent incorporation of this medication into the Brazilian public health system may explain, at least partially, the limited number of patients who received natalizumab in our hospital. In contrast, some patients of the present study received azathioprine, cyclophosphamide, and/or methotrexate before the development of PML. These medications belong to Class 3 and depend on the underlying disorder and treatment with other immunosuppressive agents to cause PML [28].
Although very rare, individuals with minimal or no immunosuppression may develop PML [30]. In this study we reported one patient with hepatic cirrhosis and a previously healthy patient with no known predisposing conditions.
The clinical, CSF, and neuroimaging features of patients included in this study are in accordance with the consolidated knowledge of PML [31,32,33] and were similar between patients with or without HIV/AIDS. Natalizumab-associated PML has some particular clinical and neuroradiological features [34], but we did not have any patients with this predisposing condition.
PML is usually progressive and fatal but varies according to the underlying condition and treatment. In this study we identified a one-year case-fatality ratio of 52.5% for the whole cohort. Interestingly, the case-fatality ratios at 6 and 12 months was similar, indicating that virtually no additional deaths occur between 6 and 12 months after PML diagnosis. This result suggests that if the patient survives at least 6 months after being diagnosed with PML, they will most likely be able to survive longer while receiving cART. The 11 studies presented in Table 5 reported case fatality rates between 21 to 71%, but only 2 [18, 19] had higher values than ours. This finding suggests a greater lethality in our patients, probably associated with structural problems such as inequity and barriers accessing the health system when compared to other epidemiological scenarios. Interestingly, we identified a one-year case-fatality rate of 54% in patients with HIV/AIDS, similarly with prior reports from high-income countries [14, 16]. However, recent studies showed that mortality rate in HIV-related PML patients has improved to 21% to 40.4% [11, 21, 23, 24]. In the present study, all deaths from nosocomial pneumonia occurred in patients with HIV/AIDS, suggesting a worse neurological status or the presence of concomitant opportunistic diseases, frequently described in our setting [10]. In our study, the one-year case-fatality ratio in HIV/AIDS (54.0%) was higher than in non-HIV/AIDS (42.9%), but one-year case-fatality ratio in oncohematological diseases (including patients with and without HIV/AIDS) was 85.7%. This result is in line with other studies that demonstrate a worse outcome in PML cases with hematological and solid organ neoplasm [11, 23, 24]. In contrast, some studies have reported one-year all-cause mortality < 20% in PML cases with chronic inflammatory diseases, particularly in natalizumab use [11, 35].
Our study has several limitations. First, it was carried out in a high complexity tertiary urban center from a middle-income country. Thus, caution is required before extrapolating results to other LMICs. Second, we used two reliable sources for case selection of hospitalized patients, but did not have access to PML individuals diagnosed through brain biopsy or on an outpatient basis. For these reasons, in particular, our frequency of severe cases must be underestimated. However, this is the first approach in the southern hemisphere to analyse PML in individuals with diverse underlying conditions and similar studies are needed. Third, we included 3 cases of possible PML (protocol deviation). However, they were HIV/AIDS patients with typical manifestations of PML and sensitivity analysis were compatible with the main analysis. Finally, due to the relatively low number of events, we decided to use a more comprehensive definition to evaluate the outcome of individuals with malignancy. Interestingly, this variable was the single independently associated with death but future studies are necessary to evaluate this association.
In conclusion, HIV/AIDS was the underlying condition in 84.8% of cases. One-year case-fatality ratio was 52.5% and oncohematological diseases was independently associated with death. This study reports emerging data on the epidemiology and outcome of PML in a middle-income country.
References
Ferenczy MW, Marshall LJ, Nelson CD et al (2012) Molecular biology, epidemiology, and pathogenesis of progressive multifocal leukoencephalopathy, the JC virus-induced demyelinating disease of the human brain. Clin Microbiol Rev 25:471–506. https://doi.org/10.1128/CMR.05031-11
Rocchi A, Sariyer IK, Berger JR (2023) Revisiting JC virus and progressive multifocal leukoencephalopathy. J Neurovirol 29:524–537. https://doi.org/10.1007/s13365-023-01164-w
Lima MA, Silva MTT, Afonso LA, Vaz BJP (2017) Post-cART progressive multifocal leukoencephalopathy era in a Brazilian center. J Neurol Sci 381:321–324. https://doi.org/10.1016/j.jns.2017.09.002
Astrom KE, Mancall EL, Richardson EP Jr (1958) Progressive multifocal leukoencephalopathy; a hitherto unrecognized complication of chronic lymphatic leukaemia and Hodgkin’s disease. Brain 81:93–111. https://doi.org/10.1093/brain/81.1.93
Berger JR, Hartung HP (2023) Commentary: Progressive multifocal leukoencephalopathy genetic risk variants for pharmacovigilance of immunosuppressant therapies. Front Neurol 14:1146027. https://doi.org/10.3389/fneur.2023.1146027
Shankar SK, Satishchandra P, Mahadevan A et al (2003) Low prevalence of progressive multifocal leukoencephalopathy in India and Africa: is there a biological explanation? J Neurovirol 9(Suppl 1):59–67. https://doi.org/10.1080/13550280390195397
Mubanga E, Patel A, Siddiqi OK et al (2019) Progressive multifocal leukoencephalopathy in Zambia is caused by JC virus with prototype regulatory region. J Neurovirol 25(4):475–9. https://doi.org/10.1007/s13365-019-00746-x
Fink MC, de Oliveira AC, Romano CM et al (2010) Molecular characterization of human polyomavirus JC in Brazilian AIDS patients with and without progressive multifocal leukoencephalopathy. J Clin Virol. 48(1):6–10. https://doi.org/10.1016/j.jcv.2010.02.020
Netravathi M, Mahadevan A, Satishchandra P et al (2013) Progressive multifocal leukoencephalopathy (PML) associated with HIV Clade C–is not uncommon. J Neurovirol. 19(3):198–208. https://doi.org/10.1007/s13365-013-0168-8
Telles JP, Fernandes R, Barros TD et al (2021) Neurological manifestations in people living with HIV/AIDS in the late cART era: a prospective observational study at a tertiary healthcare center in São Paulo, Brazil. HIV Res Clin Pract 22:87–95
Joly M, Conte C, Cazanave C et al (2023) Progressive multifocal leukoencephalopathy: epidemiology and spectrum of predisposing conditions. Brain. 146(1):349–58. https://doi.org/10.1093/brain/awac237
Berger JR, Aksamit AJ, Clifford DB et al (2013) PML diagnostic criteria: consensus statement from the AAN Neuroinfectious Disease Section. Neurology 80:1430–1438. https://doi.org/10.1212/WNL.0b013e31828c2fa1
Iacobaeus E, Burkill S, Bahmanyar S et al (2018) The national incidence of PML in Sweden, 1988–2013. Neurology 90:e498–e506. https://doi.org/10.1212/WNL.0000000000004926
Engsig FN, Hansen AB, Omland LH et al (2009) Incidence, clinical presentation, and outcome of progressive multifocal leukoencephalopathy in HIV-infected patients during the highly active antiretroviral therapy era: a nationwide cohort study. J Infect Dis 199:77–83. https://doi.org/10.1086/595299
Eng PM, Turnbull BR, Cook SF et al (2006) Characteristics and antecedents of progressive multifocal leukoencephalopathy in an insured population. Neurology 67:884–886. https://doi.org/10.1212/01.wnl.0000233918.21986.9c
Marzocchetti A, Tompkins T, Clifford DB et al (2009) Determinants of survival in progressive multifocal leukoencephalopathy. Neurology 73:1551–1558. https://doi.org/10.1212/WNL.0b013e3181c0d4a1
Molloy ES, Calabrese LH (2009) Progressive multifocal leukoencephalopathy: a national estimate of frequency in systemic lupus erythematosus and other rheumatic diseases. Arthritis Rheum 60:3761–3765. https://doi.org/10.1002/art.24966
Anand P, Hotan GC, Vogel A et al (2019) Progressive multifocal leukoencephalopathy: A 25-year retrospective cohort study. Neurol Neuroimmunol Neuroinflamm 6:e618. https://doi.org/10.1212/NXI.0000000000000618
Kartau M, Verkkoniemi-Ahola A, Paetau A et al (2019) The incidence and predisposing factors of john cunningham virus-induced progressive multifocal leukoencephalopathy in Southern Finland: a population-based study. Open Forum Infect Dis 6:ofz024. https://doi.org/10.1093/ofid/ofz024
Kartau M, Sipilä JO, Auvinen E et al (2019) Progressive multifocal leukoencephalopathy: current insights. Degener Neurol Neuromuscul Dis 9:109–121. https://doi.org/10.2147/DNND.S203405
Sipilä JOT, Soilu-Hänninen M, Rautava P et al (2019) Progressive multifocal leukoencephalopathy in Finland: a cross-sectional registry study. J Neurol 266:515–521. https://doi.org/10.1007/s00415-018-09167-y
Nakamichi K, Miura Y, Shimokawa T et al (2023) Nationwide laboratory surveillance of progressive multifocal leukoencephalopathy in Japan: fiscal years 2011–2020. Viruses 15:968. https://doi.org/10.3390/v15040968
Kim J, Kim C, Lee JA et al (2023) Long-term prognosis and overall mortality in patients with progressive multifocal leukoencephalopathy. Sci Rep 13:14291. https://doi.org/10.1038/s41598-023-41147-9
Graf LM, Rosenkranz SC, Hölzemer A et al (2021) Clinical Presentation and Disease Course of 37 Consecutive Cases of Progressive Multifocal Leukoencephalopathy (PML) at a German tertiary-care hospital: a retrospective observational study. Front Neurol 12:632535. https://doi.org/10.3389/fneur.2021.632535
Ministério da Saúde do Brasil. Secretaria de Vigilância em Saúde Departamento de Doenças de Condições Crônicas e Infecções Sexualmente Transmissíveis. Relatório de Monitoramento Clínico do HIV 2022. Available at: https://www.gov.br/aids/pt-br/central-de-conteudo/publicacoes/2022/relatoriode-monitoramento-clinico-do-hiv-setembro-2022.pdf/view. Accessed in May 20, 2024.
Yousry TA, Major EO, Ryschkewitsch C et al (2006) Evaluation of patients treated with natalizumab for progressive multifocal leukoencephalopathy. N Engl J Med 354:924–933. https://doi.org/10.1056/NEJMoa054693
Mateen FJ, Muralidharan R, Carone M et al (2011) Progressive multifocal leukoencephalopathy in transplant recipients. Ann Neurol 70:305–322. https://doi.org/10.1002/ana.22408
Chahin S, Berger JR (2015) A risk classification for immunosuppressive treatment associated progressive multifocal leukoencephalopathy. J Neurovirol 21:623–631. https://doi.org/10.1007/s13365-014-0303-1
Anton R, Haas M, Arlett P et al (2017) Drug-induced progressive multifocal leukoencephalopathy in multiple sclerosis: European regulators’ perspective. Clin Pharmacol Ther 102:283–289. https://doi.org/10.1002/cpt.604
Tan IL, Koralnik IJ, Rumbaugh JA et al (2011) Progressive multifocal leukoencephalopathy in a patient without immunodeficiency. Neurology 77:297–299. https://doi.org/10.1212/WNL.0b013e318225ab3f
Williamson EML, Berger JR (2017) Diagnosis and treatment of progressive multifocal leukoencephalopathy associated with multiple sclerosis therapies. Neurotherapeutics 14:961–973. https://doi.org/10.1007/s13311-017-0570-7
Berger JR (2014) Progressive multifocal leukoencephalopathy. Handb Clin Neurol 123:357–376. https://doi.org/10.1016/B978-0-444-53488-0.00017-1
Berger JR (2011) The clinical features of PML. Cleve Clin J Med. 78(Suppl 2):8–12. https://doi.org/10.3949/ccjm.78.s2.03
Harrer A, Tumani H, Niendorf S et al (2013) Cerebrospinal fluid parameters of B cell-related activity in patients with active disease during natalizumab therapy. Mult Scler 19:1209–1212. https://doi.org/10.1177/1352458512463483
Dahlhaus S, Hoepner R, Chan A et al (2013) Disease course and outcome of 15 monocentrically treated natalizumab-associated progressive multifocal leukoencephalopathy patients. J Neurol Neurosurg Psychiatry 84:1068–1074. https://doi.org/10.1136/jnnp-2013-304897
Acknowledgements
In Memoriam. We would like to thank Maria Cristina Domingues da Silva Fink for her pioneering spirit, scientific contribution and inspiration, which made this study possible.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was conducted according to the principles of the Declaration of Helsinki.
Informed consent
Informed consent was waived by the institutional Ethics Committee.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mari, J.F., de Miranda, É.J.F.P., Mendes-Correa, M.C. et al. Progressive multifocal leukoencephalopathy and spectrum of predisposing conditions: a 20-year retrospective cohort study in a tertiary center in São Paulo, Brazil. Neurol Sci (2024). https://doi.org/10.1007/s10072-024-07669-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10072-024-07669-4