Abstract
Endovascular Thrombectomy (EVT) as first-line treatment of patients with large core ischemic infarct is a subject of debate. A systematic literature search was conducted in four electronic databases for randomized control trials (RCTs) comparing EVT to best medical treatment (BMT) for large core infarcts (ASPECTS ≤ 5). Relevant studies were added after screening for titles, abstracts, and complete text. Meta-analysis was performed. The continuous outcomes were analyzed using the standardized mean difference (SMD) and 95% CI, while the binary outcomes were analyzed using the risk ratio (RR) and 95% confidence interval (CI). A funnel plot was used to visually evaluate publication bias, and if feasible, Egger's test was used to validate. We included 1918 patients from six RCTs that compared EVT plus BMT and BMT alone in patients with large core infarct due to large vessel occlusion in the anterior circulation. There were 946 patients in the EVT group and 972 patients in the BMT group. The one-year outcomes are available for 314 patients in the EVT group and 292 patents in the BMT group from two RCTs. EVT group had statistically significant higher rate of 90-day mRS 0–1 (RR = 3.1, P-value < 0.0001), mRS 0–2 (RR = 2.64, P-value < 0.0001), mRS 0–3 (RR = 1.80, P-value < 0.0001), lower 90-day mean mRS score (SMD = -0.29, P-value < 0.0001), lower 90-day mortality rate (RR = 0.85, P-value = 0.015), and greater early neurological improvement (RR = 2.16, P-value < 0.00001) compared to the BMT group. However, the rates of symptomatic intracerebral hemorrhage (sICH) (RR = 1.76, P-value = 0.01) and any ICH (RR = 2.18, P-value < 0.00001) were higher in EVT group. Our finding showed that EVT plus BMT led to in an absolute improvement of 5%, 12%, and 16% in 90-day mRS 0–1, 0–2, and 0–3, respectively. In addition, patients in EVT plus BMT group had a 3% increased probability of experiencing sICH and were 32% more susceptible to any ICH. Moreover, the one-year mRS 0–2 (RR = 2.16, P-value < 0.00001) and mRS 0–3 (RR = 1.80, P-value < 0.0001) was significantly favor the EVT plus BMT over BMT alone. Although, the one-year mortality rate was not significantly differed between two groups (RR = 0.91, P-value = 0.31). There was no statistically significant difference observed between the EVT plus BMT group and the BMT group concerning new stroke, decompressive craniectomy, and serious adverse events. Combined data from six RCTs shows that EVT plus BMT provides significantly better short- and long-term functional outcomes with minimal increase in symptomatic hemorrhage over BMT in patient with large core infarcts.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Endovascular thrombectomy (EVT) plus best medical treatment (BMT) has been considered as a therapeutic option in individuals with acute ischemic stroke (AIS) with large vessel occlusion and is associated with more favorable outcomes compared to BMT alone [1, 2]. EVT is indicated in patient presentation within six hours of stroke onset and a National Institutes of Health Stroke Scale score (NIHSS) and an Alberta Stroke Program Early CT Score (ASPECTS) of ≥ 6 [2,3,4]. Therefore, the mentioned criteria indicate that EVT should only performed in small to medium-sized infarcts [4].
Nevertheless, previous exclusion criteria for EVT are actively being challenged with the expansion of indications. First, the time window was expanded from 6 to 24 h for patients fulfilling advanced imaging criteria [3]. Several ongoing RCTs are evaluating the potential of EVT for patients with distal occlusions (DISTALS: NCT06034847) and low NIHSS (MOSTE: NCT03796468 and ENDO-LOW: NCT04167525). The next boundary is the interventional treatment of patients with large infarcts (ASPECTS of < 6). Application of EVT is generally avoided in the setting of large-core infarcts due to concern of symptomatic intracranial hemorrhage (sICH) will minimally benefit. According to the presence of limited data in the literature, the feasibility and efficacy of EVT in these patients remains unclear [1, 4]. Several recent randomized control trials (RCTs) have investigated the feasibility and safety of EVT plus BMT in large-core ischemic infarcts [4,5,6,7,8]. These studies demonstrated that EVT plus BMT was associated with favorable outcomes and was superior to BMT alone in the management of patients presenting with large-core ischemic infarcts [4,5,6,7,8].
Due to this underrepresented application of EVT in the management of large-core ischemic infarcts and questions of generalizability, we performed a systematic review and meta-analysis of high-quality RCTs to assess the effectiveness and practicability of EVT plus BMT versus BMT alone in patients with large-core ischemic infarcts.
Methods
Methodology and inclusion criteria
We performed a PRISMA guided literature search up to February 2024. A comprehensive search of all peer-reviewed articles and abstracts was conducted using PubMed/Medline, Google Scholar, Web of Science, and Scopus for RCTs comparing EVT and BMT in patients with large core ischemic infarct (low ASPECTS). The MeSH phrases "Large core", "Acute Ischemic Stroke", "Cerebrovascular Accident", "Endovascular Thrombectomy", and "Randomized Controlled Trial" were used in conjunction.
Two investigators (AM and BHK) separately evaluated the title and abstracts of articles and one investigator (AA) assessed the full-text of articles that were considered to be eligible. One investigator (BHK) performed manual collection of the required data. The extraction of variables was focused on presenting symptoms and patient characteristics (age, gender proportion, and past medical history), and outcomes (90-day Mortality, Functional Outcome, sICH, Any ICH, Decompressive Craniectomy, Serious Adverse Event, and New Stroke).
Statistical analysis
We performed a meta-analysis of EVT compared to BMT. Binary outcomes were analyzed and reported through the risk ratio (RR) and 95% confidence interval (CI). The heterogeneity of results among the included studies was examined using Cochrane’s Q-test and the I2 statistic. The common-effects (fixed-effect) model was used for outcomes without significant heterogeneity, while the random-effects model was used for outcomes with significant heterogeneity. Heterogeneity was assessed through visual inspection of the forest plots and measured using the I2 and chi-square (χ2) tests. The χ2 test was employed to determine the presence of significant heterogeneity, while the I2 test was utilized to quantify the magnitude of heterogeneity, if present. The interpretation of the I2 test followed the recommendations provided by the Cochrane Handbook (Part 2, Chapter 9). For testing statistical heterogeneity, a significance level (α) below 0.1 was considered indicative of significant heterogeneity, as recommended by the Cochrane Handbook. Publication bias was visually assessed with a funnel plot and confirmed by Egger’s test if possible. All p-values were two-sided, and a p-value < 0.05 was considered statistically significant. Also, statistical significance was assessed in alliance with confidence interval range. The analysis was conducted using RevMan Software.
Results
Literature review the and risk of bias assessment
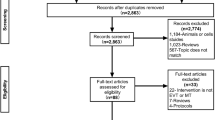
182 studies were found in our systematic search; duplicates were eliminated, leaving 98 studies. Six studies qualified for full-text screening after passing the title and abstract screening. Six papers were included in final examination and qualified for quantitative synthesis following a thorough evaluation. Additionally, no additional publications were included after a manual check of the listed studies' referenced sources. The research selection process flowchart is displayed in PRISMA flow diagram in Fig. 1 (Table 1).
Study characteristics
We included 1918 patients from 6 RCTs that compared EVT plus BMT and BMT alone among patients with large core ischemic infarct. There were 946 patients in EVT group and 972 patients in BMT group. The summary of demographic and clinical characteristics of included patients are shown in (Table 2). The middle cerebral artery was the most prevalent artery in both groups. A majority of patients in EVT group underwent local anesthesia. Successful revascularization was achieved in 82% (519/633) of patients and stent retriever was the most common technique employed in the EVT group. The rate of procedure-related vascular injury was 11.2% (57/509). Distal embolization occurred in 7.6% (27/355) and 15.6% (20/128) of patients in the EVT group and BMT group, respectively. The incidence of arterial access-site complications was 2.8% (5/178). Some data on demographic for LASTE and TESLA were missed as these were abstract presentations only.
Short-term functional outcomes
90-day mRS 0–1
The proportion of patients with mRS 0–1 at three months was statistically significant higher in the EVT group versus the BMT group [7.6% (59/776) vs 2.4% (19/771), (RR = 3.1, 95% CI (1.86—5.13), P-value < 0.0001)], Fig. 2A. No statistically significant heterogeneity was found so the Fixed effect model was implicated (I2 = 0%, P-value = 0.87). The funnel plot of the outcome is attached on Supplementary Fig. 2A.
Forest plot for short-term functional outcomes. A Forest plot for 90-day mRS 0–1. B Forest plot for one-year mRS 0–2. C Forest plot for independent ambulation at 90 days. D Forest Plot for Mean mRS score at three months E Forest plot for early neurological improvement. F Forest plot for 90-day mortality
90-day mRS 0–2
The incidence of patients with mRS 0–2 at three months was statistically significant greater in the EVT group versus the BMT group [19.3% (180/931) vs 7.3% (68/922), (RR = 2.64, 95% CI (2.03–3.43), P-value < 0.0001)], Fig. 2B. No statistically significant heterogeneity was found so the Fixed effect model was implicated (I2 = 0.1%, P-value = 0.41). The funnel plot of the outcome is attached on Supplementary Fig. 2B.
90-day mRS 0–3
The proportion of patients with 90-day mRS 0–3 was significantly higher in the EVT group versus the BMT group [36.4% (343/942) vs 20% (188/935), (RR = 1.80, 95% CI (1.55–2.1), P-value < 0.0001)], Fig. 2C. No statistically significant heterogeneity was found so the Fixed effect model was implicated (I2 = 35%, P-value = 0.19). The funnel plot of the outcome is attached on Supplementary Fig. 2C.
Mean mRS score at three months
The mean mRS score at three months was significantly higher in the EVT group compared to the BMT group [4.3 (2.2) vs 5.3 (1.4), (SMD = −0.29, 95% CI (−0.4—−0.17), P-value < 0.0001)], Fig. 2D. No statistically significant heterogeneity was found so the Fixed effect model was implicated (I2 = 33%, P-value = 0.22).
Early neurological improvement
Early neurological improvement was defined as a reduction of ≥ 4 points in the NIHSS score from baseline to 24 h after presentation. The incidence was significantly higher in EVT group compared to the BMT group [21.4% (90/420) vs 10% (41/414), (RR = 2.16, 95% CI (1.54–3.04), P-value < 0.00001)], Fig. 2E. No statistically significant heterogeneity was found so the Fixed effect model was implicated (I2 = 32%, P-value = 0.23). The funnel plot of the outcome is attached on Supplementary Fig. 2D.
90-day mortality
The 90-day mortality was statistically significantly lower in EVT group versus BMT group [31% (295/938) vs 37% (343/933), (RR = 0.85, 95% CI (0.81–1.07), P-value = 0.015)], Fig. 2F. No statistically significant heterogeneity was found so the Fixed effect model was implicated (I2 = 44.6%, P-value = 0.1). The funnel plot of the outcome is attached on Supplementary Fig. 2E.
Long-term functional outcomes
One-year mRS 0–2
The proportion of patients with mRS 0–2 was significantly higher in the EVT group versus the BMT group [22.9% (72/314) vs 5.8% (17/292), (RR = 3.94, 95% CI (1.55—2.8), P-value < 0.0001)]. No statistically significant heterogeneity was found so the Fixed effect model was implicated (I2 = 0%, P-value = 0.85).
One-year mRS 0–3
The rate of patients with mRS 0–3 was significantly higher in the EVT group versus the BMT group [35.7% (112/314) vs 17.1% (50/292), (RR = 2.1, 95% CI (1.55—2.8), P-value < 0.0001)]. No statistically significant heterogeneity was found so the Fixed effect model was implicated (I2 = 0%, P-value = 0.85).
One-year mortality rate
The mortality rate was non-significantly lower in the EVT group versus the BMT group [44.9% (141/314) vs 49% (143/292), (RR = 0.91, 95% CI (0.77 – 21.08), P-value = 0.31)]. No statistically significant heterogeneity was found so the Fixed effect model was implicated (I2 = 0%, P-value = 0.47).
Complications and safety outcomes
Symptomatic intracerebral hemorrhage
The prevalence of sICH was statistically significantly higher in the EVT group versus the BMT group [5.6% (52/932) vs 3.2% (30/940), (RR = 1.76, 95% CI (1.14—2.7), P-value = 0.01)], Supplementary Fig. 1A. No statistically significant heterogeneity was found so the Fixed effect model was utilized (I2 = 0%, P-value = 0.8). The funnel plot of the outcome is attached on Supplementary Fig. 2F.
Any intracerebral hemorrhage
The proportion of patients had any ICH within 48 h was statistically significantly in the EVT group compared with the BMT group [53.6% (171/319) vs 21.9% (71/324), (RR = 2.18, 95% CI (1.85–2.57), P-value < 0.00001)], Supplementary Fig. 1B. No statistically significant heterogeneity was found so the Fixed effect model was implicated (I2 = 38%, P-value = 0.19). The funnel plot of the outcome is attached on Supplementary Fig. 2G.
New stroke
Recurrence of (New) cerebral infarction was non-significantly lower in EVT group versus BMT group [6.2% (25/403) and 7.4% (30/404), (RR = 0.85, 95% CI (0.51–1.40), P-value = 0.52)], Supplementary Fig. 1C. No statistically significant heterogeneity was found so the Fixed effect model was implicated (I2 = 0%, P-value = 0.95). The funnel plot of the outcome is attached on Supplementary Fig. 2H.
Serious adverse event
The rate of at least one serious adverse event non-significantly higher in EVT group and BMT group, [45.4% (207/456) and 43.5% (198/455), (RR = 1.06, 95% CI (0.83–1.35), P-value = 0.63), Supplementary Fig. 1D. Statistically significant heterogeneity was found so the Random effect model was implicated (I2 = 80%, P-value = 0.002). Sensitivity analysis was conducted to resolve the significant heterogeneity; however, it was not successful, so the random-effect model was implemented. The funnel plot of the outcome is attached on Supplementary Fig. 2I.
Decompressive craniectomy
The number of patients underwent the decompressive craniectomy did not significantly differ between the EVT group and the BMT group [8.1% (36/444) vs 6.9% (31/452), (RR = 1.18, 95% CI (0.75–1.88), P-value = 0.47)], Supplementary Fig. 1E. No statistically significant heterogeneity was found so the Fixed effect model was implicated (I2 = 29%, P-value = 0.25). The funnel plot of the outcome is attached on Supplementary Fig. 2J.
Quality assessment
The quality of included studies was assessed using the Cochrane a revised tool for assessing the risk of bias in randomized trials (RoB2). The risk of bias was low among all RCTs included in the study. However, because of the TESLA and LASTE is not officially published we cannot evaluate the risk of bias of this trial. A detailed summary of risk of bias assessment is available in Supplementary Appendix 2.
Discussion
The current systematic review and meta-analysis included 6 RCTs encompassing approximately 1594 patients investigating the impact of EVT with BMT versus BMT alone in patients who presented with large core infarct due to large vessel occlusion (LVO). The findings demonstrated that the EVT group had statistically significant higher rate of better functional outcome (mRS 0–1, mRS 0–2, and mRS 0–3) at three months, lower 90-day mean mRS score, lower 90-day mortality rate, and greater early neurological improvement. Though the rate of sICH and any ICH were significantly higher in EVT group, there was only an increase of approximately 2% in symptomatic hemorrhage. The one-year functional outcome (mRS 0–2 and mRS 0–3) at one year were significantly higher in EVT group compared with BMT group. There were no statistically significant differences observed between the EVT group and the BMT group concerning one-year mortality rate, new stroke, decompressive craniectomy, and serious adverse events. Trends favored the EVT across several of these endpoints.
Our findings support the results of previous meta-analyses demonstrating that EVT is safe and superior for improving functional outcomes in patients with large infarcts [9,10,11]. The majority of these meta-analyses included observational studies with high data heterogeneity (especially in imaging modality), due predominance of single-arm and single-center studies and thus considerable risk of bias. Furthermore, some of the studies included patients with an ASPECT score of 5 or a low ASPECT score (0–4), which potentially weakens reported results. Moreover, our study included the TENSION [8] and LASTE [12] trials and long-terms outcomes, which initially demonstrated a significant benefit in survival with EVT. The current study provides the largest sample size (six RCTs) and importantly more detailed functional and safety outcomes than two recent meta-analyses [1, 2].
Quantification of infarct core volume for patient selection in the majority of RCTs is based either on MRI (diffusion-weighted sequence) [4] or CT perfusion imaging and a specialized post-processing software [4,5,6,7]. The TENSION [8] and TESLA [5] trials employed visual assessment of infarct size on unenhanced CT augmented with CTA to demonstrate the location of vascular occlusion, which is the most commonly used imaging technique globally for stroke management [13, 14].
Our finding indicated that EVT plus BMT led to in an absolute improvement of 5%, 12%, and 16% in excellent functional outcome, independent functional outcomes, and ability to walk independently at 90 days, respectively. Moreover, one-year functional outcomes was significantly higher in the EVT group compared with the BMT group [5, 15]. Although the 90-day mortality rate was lower in the EVT group in all except two RCTs (21.7 and 35.3% in EVT versus 20% and 33.3% in BMT) [7, 8], EVT showed an absolute pooled decrease of 6% in mortality at 90 days. Furthermore, one-year mortality rate showed pooled decreased of 5%. In the LASTE trial [12], incidence of patients with critically large core infarct (56%, ASPECTS 0–2) was about 4 to 13 times more than other RCTs, nevertheless, they showed significant benefit of EVT over BMT in mortality rate (36% vs. 55%) and independent functional outcome at three months (13% vs. 5%).
The current study shows that EVT was associated with a substantial revascularization rate of 82% (mTICI 2b/3), which fits within the typical range of revascularization rates reported in neuroendovascular literature [4,5,6,7,8]. Nevertheless, there are still lingering concerns over EVT potentially exacerbating the risk of ICH. Our findings revealed that patients who received EVT had a 3% increased probability of experiencing sICH and were 32% more susceptible to any ICH. It is unclear if this increase is clinically meaningful. Concerning recurrence or new cerebral infarction within 90 days, there is no statistically significant difference between two group (6% vs. 7%). We observed no significant difference in rate of 90-day decompressive craniotomy between EVT and BMT. Contrary to TENSION (9% vs. 7%) and ANGEL-ASPECT (7% vs. 34%), RESCUE-Japan LIMIT (10% vs. 14%) showed a lower rate of 90-day decompressive craniotomy in the EVT group than the BMT group.
Although ANGEL-ASPECT revealed a similar occurrence of serious adverse events between the two groups, TENSION reported that 7% of patients in the EVT group experienced at least one procedure-related adverse event without any procedure-related mortality. They also showed a statistically significantly lower rate of at least one serious adverse event in the EVT group (56% vs. 70%). On the other hand, RESCUE-Japan LIMIT showed significantly higher rate of serious events in the EVT group compared to the BMT group (44% vs. 24%). We showed a comparable non-significant rate of at least one serious adverse event between the two groups.
SELECT2 and TENSION demonstrated that patients in the EVT group had statistically significantly better three-month quality of life scores than the BMT group [6, 8]. In a trial, one out of ten patients in the EVT group were discharged to a home, which was approximately twice the number of patients in the BMT group. Additionally, the EVT group exhibited a smaller proportion of patients discharged into hospice (6% vs. 11%) and a lower in-hospital death rate (24% vs. 25%) compared to the BMT group [6].
To the best of our knowledge, the current study is the largest systematic review and meta-analysis that exclusively assessed all available RCTs. The present study had few study-specific limitations that need to be acknowledged. First, trials enrolled a limited number of participants and were stopped prematurely. Additionally, our findings indicated that patients in the BMT group received approximately a similar quantity of IV tPA compared to the EVT group, which can affect the overall outcomes of the BMT group. Second, international enrollment of patients was performed only in two trials, and three other trials were conducted in Japan, China, and the United States. Although this difference can lead to some concerns about the applicability of reported results, our research revealed neglectable rate of heterogeneity in the analysis. Third, there is some heterogeneity in the criteria for selecting or excluding patients in the trials. The homogenous criteria definition is crucial for upcoming trials to enhance the generalizability of findings. Last but not least, short-term and one-year results of TESLA, and LASTE has not yet been formally published, and data collection of this study is based on reported results in the abstract presented at the European Stroke Organization Conference 2023 and International Stroke Conference 2024.
Conclusion
EVT could be beneficial in patients presenting with large infarct core. However, there are some safety concerns which can be resolve with progressive development of thrombectomy devices and techniques.
Data availability
N/A.
Change history
20 July 2024
A Correction to this paper has been published: https://doi.org/10.1007/s10072-024-07692-5
References
Kobeissi H, Adusumilli G, Ghozy S, Kadirvel R, Brinjikji W, Albers GW et al (2023) Endovascular thrombectomy for ischemic stroke with large core volume: an updated, post-TESLA systematic review and meta-analysis of the randomized trials. Interv Neuroradiol 28:15910199231185738
Palaiodimou L, Sarraj A, Safouris A, Magoufis G, Lemmens R, Sandset EC et al (2023) Endovascular treatment for large-core ischaemic stroke: a meta-analysis of randomised controlled clinical trials. J Neurol Neurosurg Psychiatry 94(10):781–785
Turc G, Bhogal P, Fischer U, Khatri P, Lobotesis K, Mazighi M et al (2019) European Stroke Organisation (ESO) – European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischaemic StrokeEndorsed by Stroke Alliance for Europe (SAFE). Eur Stroke J 4(1):6–12
Yoshimura S, Sakai N, Yamagami H, Uchida K, Beppu M, Toyoda K et al (2022) Endovascular therapy for acute stroke with a large ischemic region. N Engl J Med 386(14):1303–1313
Zaidat OO, Kasab SA, Sheth S, Ortega-Gutierrez S, Rai AT, Given CA et al (2023) TESLA trial: rationale, protocol, and design. SVIN 3(4):e000787
Sarraj A, Hassan AE, Abraham MG, Ortega-Gutierrez S, Kasner SE, Hussain MS et al (2023) Trial of endovascular thrombectomy for large ischemic strokes. N Engl J Med 388(14):1259–1271
Huo X, Ma G, Tong X, Zhang X, Pan Y, Nguyen TN et al (2023) Trial of endovascular therapy for acute ischemic stroke with large infarct. N Engl J Med 388(14):1272–1283
Bendszus M, Fiehler J, Subtil F, Bonekamp S, Aamodt AH, Fuentes B et al (2023) Endovascular thrombectomy for acute ischaemic stroke with established large infarct: multicentre, open-label, randomised trial. Lancet 402(10414):1753–1763
Cagnazzo F, Derraz I, Dargazanli C, Lefevre PH, Gascou G, Riquelme C et al (2020) Mechanical thrombectomy in patients with acute ischemic stroke and ASPECTS ≤6: a meta-analysis. J Neurointerv Surg 2(4):350–5
Li Q, Abdalkader M, Siegler JE, Yaghi S, Sarraj A, Campbell BCV et al (2023) Mechanical thrombectomy for large ischemic stroke: a systematic review and meta-analysis. Neurology 101(9):e922–32
Sarraj A, Grotta JC, Pujara DK, Shaker F, Tsivgoulis G (2020) Triage imaging and outcome measures for large core stroke thrombectomy - a systematic review and meta-analysis. J Neurointerv Surg 12(12):1172–9
Costalat V, Lapergue B, Albucher J, Labreuche J, Henon H, Gory B et al (2024) Evaluation of acute mechanical revascularization in large stroke (ASPECTS ⩽5) and large vessel occlusion within 7 h of last-seen-well: the LASTE multicenter, randomized, clinical trial protocol. Int J Stroke 19(1):114–119
Kim Y, Lee S, Abdelkhaleq R, Lopez-Rivera V, Navi B, Kamel H et al (2021) Utilization and availability of advanced imaging in patients with acute ischemic stroke. Circ Cardiovasc Qual Outcomes 14(4):e006989
Nogueira RG, Haussen DC, Liebeskind D, Jovin TG, Gupta R, Jadhav A et al (2021) Stroke imaging selection modality and endovascular therapy outcomes in the early and extended time windows. Stroke 52(2):491–497
Sarraj A, Abraham MG, Hassan AE, Blackburn S, Kasner SE, Ortega-Gutierrez S et al (2024) Endovascular thrombectomy plus medical care versus medical care alone for large ischaemic stroke: 1-year outcomes of the SELECT2 trial. Lancet 403(10428):731–740
Funding
There is no funding source with authors to declare.
Author information
Authors and Affiliations
Contributions
AM contributed to the study conception and design, performed search. AM and MMM edited the manuscript. AM, ZH, OE, BHK, and AYA analyzed the data and wrote the first draft of the manuscript. AM, MAA, and BHK collected data and evaluated the quality assessment. RR, AM and AAD contributed to the study design, revised the manuscript, analyzed data, and drew figures. All authors commented on previous versions of the manuscript and revised it. All authors read and approved the final manuscript.”
Corresponding author
Ethics declarations
Ethical approval
NA.
Consent to participate
N/A.
Consent to publish
N/A.
Conflict of interest
The authors received no financial or material support for the research, authorship, and/or publication of this article.
Informed consent
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The original article contains an error. Figures and Supplementary figure citations has been modified in the body text for clarity.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1
(DOCX 140 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mortezaei, A., Morsy, M.M., Hajikarimloo, B. et al. Endovascular thrombectomy for ischemic stroke with large infarct, short- and long-term outcomes: a meta-analysis of 6 randomised control trials. Neurol Sci (2024). https://doi.org/10.1007/s10072-024-07662-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10072-024-07662-x