Abstract
Objective
This study aimed to develop a Japanese version of the New Freezing of Gait Questionnaire (NFOG-Q) and investigate its validity and reliability.
Methods
After translating the NFOG-Q according to a standardised protocol, 56 patients with Parkinson’s disease (PD) were administered it. Additionally, the MDS-UPDRS parts II and III, Hoehn and Yahr (H&Y) stage, and number of falls over 1 month were evaluated. Spearman’s correlation coefficients (rho) were used to determine construct validity, and Cronbach’s alpha (α) was used to examine reliability.
Results
The interquartile range of the NFOG-Q scores was 10.0–25.3 (range 0–29). The NFOG-Q scores were strongly correlated with the MDS-UPDRS part II, items 2.12 (walking and balance), 2.13 (freezing), 3.11 (freezing of gait), and 3.12 (postural stability) and the postural instability and gait difficulty score (rho = 0.515–0.669), but only moderately related to the MDS-UPDRS item 3.10 (gait), number of falls, disease duration, H&Y stage, and time of the Timed Up-and-Go test (rho = 0.319–0.434). No significant correlations were observed between age and the time of the 10-m walk test. The internal consistency was excellent (α = 0.96).
Conclusions
The Japanese version of the NFOG-Q is a valid and reliable tool for assessing the severity of freezing in patients with PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Freezing of gait (FOG) is one of the most disturbing motor symptoms in Parkinson’s disease (PD) [1], affecting 60%–80% of patients with PD [2]. This increases the risk of falls [3] and reduces the quality of life [4]. Despite its common and disabling features in everyday circumstances, it is challenging to assess the severity of FOG in daily clinical practice because of its episodic nature [5].
The New Freezing of Gait Questionnaire (NFOG-Q) has been widely used to subjectively quantify the occurrence and severity of FOG [6, 7]. The NFOG-Q is the only recommended instrument for assessing FOG severity [8, 9], as it has adequate clinimetric properties and the benefits of being short and easy to administer [7, 8].
The NFOG-Q consists of nine items organised into three parts: “Part I – Distinction (freezer or non-freezer)”, “Part II – Freezing severity”, and “Part III – Freezing impact on daily life”, which together assess FOG severity and its impact on daily life. Another feature of the NFOG-Q is a video demonstration of the FOG for participants to view different freezing episodes before completing the questionnaire, which allows them to accurately perceive the FOG. This leads to more reliable outcomes of the questionnaire-based methodology [7].
To date, the original version of the NFOG-Q has been translated into several languages, including Swedish [10], Italian [11], Turkish [12], Spanish [13], Brazilian Portuguese [14], Czech [15], German [16], Chinese [17], and Thai [18] (in order of publication year).
Despite their advantages and global use in assessing FOG severity, a Japanese translation is not currently available. Therefore, the aim of the current study was to develop a Japanese version of the NFOG-Q and investigate its validity and reliability.
Furthermore, the pathophysiological mechanism of FOG has been implicated in executive dysfunction as a series of functional neuroimaging studies have highlighted that frontostriatal projections and the basal ganglia hyperdirect pathway may contribute to FOG [19,20,21]. Thus, we further investigated the relationship between the NFOG-Q and executive function as well as global cognition.
Methods
Participants
Sixty-one patients with PD from two different medical centres (N = 32, Osaka University Hospital, Japan; N = 29, Hyogo Prefectural Rehabilitation Hospital at Nishi-Harima, Japan) participated in the study. The inclusion criteria were as follows: (1) diagnosis of idiopathic PD based on the Movement Disorder Society (MDS) clinical diagnostic criteria [22] and (2) Hoehn and Yahr (H&Y) stage < 5. The exclusion criteria were as follows: (1) probable dementia (Mini-Mental State Examination (MMSE) score < 24) [23] and (2) problems other than PD that might affect gait.
Development of the Japanese version of the NFOG-Q
After obtaining permission from the developers of the original version [6, 7], the Japanese version of the NFOG-Q was developed in accordance with a standardised protocol [24] (see Supplementary Information).
Procedure
Demographics and disease profiles, including the H&Y stage (“on,” or best state), MDS-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) parts II and III, medication (Levodopa Equivalent Daily Dose [LEDD]), number of falls over the previous 1 month, and cognitions (Mini-Mental State Examination [MMSE], and the Frontal Assessment Battery [FAB]) were evaluated. Additionally, participants underwent a clinical evaluation using the 10-m walk test (10MWT) and the Timed Up-and-Go test (TUG).
After participants watched the demonstration video, they were administered the NFOG-Q. The questionnaire’s nine items have ratings of up to 3 or 4, with a total score ranging from 0 to 29 points, with a higher score indicating more severe FOG.
Construct validity was examined by determining the associations between the NFOG-Q scores and functional measures (scores on the MDS-UPDRS, number of falls, and objective gait measures). Score reliability and ceiling and floor effects were also evaluated based on previous validation studies [6, 11]. Participants were classified as “faller” if they had at least one fall, or “non-faller” if they had no history of fall within the last 1 month. Moreover, participants were categorized as the “freezers” if they had a score of > 0, or “non-freezers” if they had a score of = 0 on the NFOG-Q, and we investigated the relationship between the NFOG-Q and global cognition (measured by the MMSE) and executive function (measured by the FAB) in whole group as well as the freezers. The questionnaires and other assessments were completed during the participants’ ‘‘on’’ or best state. This study was conducted after pre-registration with the UMIN Clinical Trials Registry (UMIN000049889). All participants provided informed consent as required under the Declaration of Helsinki. The study protocol was approved by the Ethics Committee of Osaka University Hospital (No. 20563) and the Hyogo Prefectural Rehabilitation Hospital at Nishi-Harima (No. 2209). Data collection procedures were harmonized and standardized across centres.
Statistical analysis
Construct validity of the NFOG-Q was determined based on correlations between the NFOG-Q scores and existing functional scales: the MDS-UPDRS items 2.12 (Walking and balance), 2.13 (Freezing), 3.10 (Gait), 3.11 (Freezing of gait), 3.12 (Postural Stability); the MDS-UPDRS part II total; MDS-UPDRS part III total; postural instability and gait difficulty (PIGD) score, which is the sum of sub-items 2.12, 2.13, 3.10, 3.11, 3.12 [25]; TUG time, fast gait time; and number of falls. Spearman’s correlation coefficients (rho) were considered moderate for values of 0.30–0.39 and strong for values of 0.40–0.69 [26].
To determine reliability, the internal consistency was examined using Cronbach’s alpha (α) for which a value > 0.90 was considered excellent internal consistency [27].
To evaluate the possible ceiling or floor effects, the proportion of participants obtaining the minimum and maximum scores was set at a threshold of 15% [28]. Additionally, a receiver operating characteristic (ROC) curve analysis was conducted to examine the optimal NFOG-Q cutoff value for distinguishing fallers from non-fallers.
Statistical analyses were performed using SPSS (version 29.0). The false discovery rate (FDR)-corrected P values < 0.05 were considered statistically significant.
Results
Patient characteristics and NFOG-Q score distributions
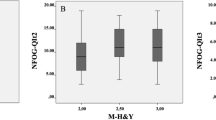
Fifty-six patients were included in this study after excluding five patients. The median age was 71.0 years (interquartile range [IQR] 65.5–76.0), with a median disease duration of 11 years (IQR 6.8–14.0); a median UPDRS-III score of 30.5 (IQR 19.75–42.25); and H&Y stage II (n = 11), III (= 35), and IV (n = 10). The median total NFOG-Q score was 21.0 (IQR 10.0–25.3) with a range of 0–29, and 48 patients were classified as freezers and 8 patients as non-freezers. The floor and ceiling effects were both < 15%. Twenty-two participants (39.3%) had experienced at least one fall during the previous 1 month. Further characteristics of the participants are presented in Table 1.
Validity and reliability
Construct validity
Correlation analysis showed that the NFOG-Q score was significantly positively related to the MDS-UPDRS items 2.12 (walking and balance), 2.13 (freezing), 3.11 (freezing of gait), and 3.12 (postural Stability), PIGD score, and total scores in the MDS-UPDRS parts II and III and positively correlated with disease duration, H&Y stage, TUG time, and number of falls. However, there was no significant association between the NFOG-Q score and age or fast gait time during the 10MWT. Additional information is presented in Table 2.
Predictive validity
ROC analysis of the NFOG-Q score indicated an optimal cut-off value of 20.5 points for distinguishing fallers from non-fallers over 1 month, with sensitivity of 81.8% and specificity of 61.8%, and the area under the ROC curve (AUC) was 0.72.
Reliability
Internal consistency as measured by Cronbach α was 0.96, suggesting adequate reliability.
Association between scores in the NFOG-Q and cognitive performances
There were no significant correlations between scores in the NFOG-Q and cognitive tests in any freezer group (with the MMSE [rho = -0.112, p = 0.689], and with the FAB [rho = 0.059, p = 0.689]), or whole PD group (with the MMSE [rho = -0.092, p = 0.497], and with the FAB [rho = 0.266, p = 0.096]).
Discussion
A Japanese version of the NFOG-Q was developed and its validity and reliability were evaluated. The construct validity of the NFOG-Q was demonstrated by a good correlation with freezing- and gait-related measures and negligible floor and ceiling effects. The Japanese version of the NFOG-Q also showed high internal consistency (α = 0.96), which was similar to the results of original English version (0.96) [6] and other validation studies (0.81–0.95) [10, 11, 13,14,15, 17].
Correlation analysis showed that the NFOG-Q score was related to the TUG test time; however, it was not related to fast gait time during the 10MWT. This could be explained by the higher complexity of the TUG test (incorporating chair transfer, walking, and turning) compared with the straight-path walking in the 10MWT [29], and there is a consensus that turning is one of the strongest provocative triggers of FOG [30,31,32,33].
Consistent with previous translated versions [6, 10, 14, 15, 17], the current results demonstrate the relationship between the NFOG-Q score and the number of falls over one month. Unsurprisingly, 61% of falls in PD are related to FOG (12.6% syncope, 26.3% imbalance) [3]. The current study showed that the NFOG-Q scores had a stronger relationship with freezing items than with gait items: item 2.13 (freezing) vs item 2.12 (walking and balance), rho = 0.669 vs 0.599; item 3.11 (freezing of gait) vs item 3.10 (gait), rho = 0.515 vs 0.374, respectively.
Moreover, our findings indicated that subjectively reported items (i.e., MDS-UPDRS part II total and items 2.12 and 2.13) were more strongly related to NFOG-Q scores than objectively measured items of the MDS-UPDRS (i.e., MDS-UPDRS part III total and items 3.10 and 3.11), similar to previous translations [10, 11, 15, 17, 18]. To explain these results, the effect of different types of measurements (subjective or objective) on the freezing phenomenon should be considered. Importantly, it is recognised that gait can improve and freezing of gait can disappear while an examiner observes [5, 34], since patients shift from an automatic motor control to a more goal-directed one [35], which is also described as the "white coat effect" [34]. In particular, the current study enrolled only inpatients and outpatients who were assessed in a hospital setting, which may have resulted in a better performance in hospitals than in daily life settings.
Moreover, we found that the NFOG-Q score was related to disease duration and H&Y stage but not to age, consistent with other validation studies [10, 11, 14, 18]; however, one validation study showed that the NFOG-Q was associated with increased age [15]. This discrepancy may be ascribed to the differences in the study populations, given that the four studies reporting no correlation with age enrolled a relatively large number of participants compared with that reporting a correlation [10, 11, 14, 18]. In addition, a large-cohort survey (6,620 patients) further supported this interpretation, showing that freezing episodes were significantly related to a longer disease duration and a more advanced stage of PD but had no relationship with age [36].
Furthermore, the fall rate in this study was similar to that of the Chinese validation study (39.3% vs. 32.4%) [17] and the results of the ROC analysis indicated good predictive validity. The cut-off value for the NFOG-Q was 20.5 points for distinguishing fallers from non-fallers over 1 month, while a previous study showed a cut-off of 5.5 points over a 12-month period [37]. Thus, a follow-up study is required to examine prospective fall histories over long intervals.
We did not find any significant associations between the scores in the cognitive functions and the NFOG-Q. They are in keeping with a recent novel study including a large cohort of PD, which showed that the NFOG-Q scores was not associated to global cognition or executive function [38]. However, more in depth assessment of more specific executive function (such as the behavioral assessment of the dysexecutive syndrome battery [39]) may be needed to rule out the dependency of the cognitive functions.
One limitation of the current study was that non-motor symptoms (e.g., anxiety, stress, depression), which could also affect FOG [40] were not adequately assessed, as only the MMSE and the FAB considered cognitive impairments in this study. However, further studies are required to clarify this.
In conclusion, the current study developed a Japanese version of the NFOG-Q and reported its validity and reliability in assessing FOG in patients with PD.
Data availability
The datasets generated and analysed during the current study are not publicly available because of ethical restrictions but are available from the corresponding author on reasonable request.
References
Giladi N, Treves TA, Simon ES, Shabtai H, Orlov Y, Kandinov B, Paleacu D, Korczyn AD (2001) Freezing of gait in patients with advanced parkinson’s disease. J Neural Transm (Vienna) 108:53–61
Bertoli M, Croce UD, Cereatti A, Mancini M (2019) Objective measures to investigate turning impairments and freezing of gait in people with parkinson’s disease. Gait Posture 74:187–193
Pelicioni PHS, Menant JC, Latt MD, Lord SR (2019) Falls in parkinson’s disease subtypes: risk factors, locations and circumstances. Int J Environ Res Public Health 16:2216
Walton CC, Shine JM, Hall JM, O’Callaghan C, Mowszowski L, Gilat M, Szeto JY, Naismith SL, Lewis SJ (2015) The major impact of freezing of gait on quality of life in parkinson’s disease. J Neurol 262:108–115
Mancini M, Bloem BR, Horak FB, Lewis SJG, Nieuwboer A, Nonnekes J (2019) Clinical and methodological challenges for assessing freezing of gait: future perspectives. Mov Disord 34:783–790
Giladi N, Shabtai H, Simon ES, Biran S, Tal J, Korczyn AD (2000) Construction of freezing of gait questionnaire for patients with parkinsonism. Parkinsonism Relat Disord 6:165–170
Nieuwboer A, Rochester L, Herman T, Vandenberghe W, Emil GE, Thomaes T, Giladi N (2009) Reliability of the new freezing of gait questionnaire: agreement between patients with parkinson’s disease and their carers. Gait Posture 30:459–463
Bloem BR, Marinus J, Almeida Q, Dibble L, Nieuwboer A, Post B, Ruzicka E, Goetz C, Stebbins G, Martinez-Martin P, Schrag A, ftMDSRS Committee (2016) Measurement instruments to assess posture, gait, and balance in Parkinson’s disease: Critique and recommendations. Mov Disord. 31:1342–1355
Keus S, Munneke M, Graziano M, Paltamaa J, Pelosin E, Domingos J, Brühlmann S, Ramaswamy B, Prins J, Struiksma C, Rochester L, Nieuwboer A, Bloem B (2014) European physiotherapy guideline for parkinson's disease. KNGF/ParkinsonNet. https://www.parkinsonnet.nl/app/uploads/sites/3/2019/11/eu_guideline_parkinson_guideline_for_pt_s1.pdf. Accessed 19 Feb 2024
Nilsson MH, Hagell P (2009) Freezing of gait questionnaire: validity and reliability of the swedish version. Acta Neurol Scand 120:331–334
Tambasco N, Simoni S, Eusebi P, Ripandelli F, Brahimi E, Sacchini E, Nigro P, Marsili E, Calabresi P (2015) The validation of an Italian version of the freezing of gait questionnaire. Neurol Sci 36:759–764
Candan SA, ÇAtiker A, ÖZcan TŞ (2019) Psychometric properties of the Turkish version of the freezing of gait questionnaire for patients with Parkinson’s disease. Neurol Sci Neurophysiol 36:44–50
Cervantes-Arriaga A, Rodríguez-Violante M (2011) Validation of the spanish version of the questionnarie freezing of gait (FOG-Q) in parkinson’s disease. Arch Neurocien. 16(4):173–178
Baggio JA, Curtarelli MB, Rodrigues GR, Tumas V (2012) Validity of the Brazilian version of the freezing of gait questionnaire. Arq Neuropsiquiatr 70:599–603
Gal O, Polakova K, Brozova H, Bezdicek O, Hoskovcova M, Jech R, Ruzicka E (2020) Validation of the freezing of gait questionnaire in patients with parkinson’s disease treated with deep brain stimulation. Neurol Sci 41:1133–1138
Seuthe J, Kuball K, Hoffmann AK, Weisser B, Deuschl G, Schlenstedt C (2021) Validation of the German version of the new freezing of gait questionnaire for people with parkinson’s disease. Parkinsons Dis 2021:8841679
Tao P, Shao X, Zhuang J, Wang Z, Dong Y, Shen X, Guo Y, Shu X, Wang H, Xu Y, Li Z, Adams R, Han J (2021) Translation, cultural adaptation, and reliability and validity testing of a chinese version of the freezing of gait questionnaire (FOGQ-CH). Front Neurol 12:760398
Taweekitikul A, Tanvijit P, Tantisuvanitchkul P, Srivanitchapoom P, Pitakpatapee Y, Khobkhun F, Akkathep P (2023) Validity and reliability of the thai version of the freezing of gait questionnaire in individuals with parkinson’s disease. Ann Rehabil Med 47:45–51
Snijders AH, Leunissen I, Bakker M, Overeem S, Helmich RC, Bloem BR, Toni I (2010) Gait-related cerebral alterations in patients with parkinson’s disease with freezing of gait. Brain 134:59–72
Shine JM, Matar E, Ward PB, Frank MJ, Moustafa AA, Pearson M, Naismith SL, Lewis SJ (2013) Freezing of gait in parkinson’s disease is associated with functional decoupling between the cognitive control network and the basal ganglia. Brain 136:3671–3681
Gilat M, Bell PT, Ehgoetz Martens KA, Georgiades MJ, Hall JM, Walton CC, Lewis SJG, Shine JM (2017) Dopamine depletion impairs gait automaticity by altering cortico-striatal and cerebellar processing in Parkinson’s disease. Neuroimage 152:207–220
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, Obeso J, Marek K, Litvan I, Lang AE, Halliday G, Goetz CG, Gasser T, Dubois B, Chan P, Bloem BR, Adler CH, Deuschl G (2015) MDS clinical diagnostic criteria for parkinson’s disease. Mov Disord 30:1591–1601
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Beaton D, Bombardier C, Guillemin F, Ferraz MB (2002) Recommendations for the cross-cultural adaptation of health status measures. N Y Am Acad Orthop Surg 12:1–9
Stebbins GT, Goetz CG, Burn DJ, Jankovic J, Khoo TK, Tilley BC (2013) How to identify tremor dominant and postural instability/gait difficulty groups with the movement disorder society unified parkinson’s disease rating scale: comparison with the unified parkinson’s disease rating scale. Mov Disord 28:668–670
Dancey CP, Reidy J (2004) Statistics without maths for psychology: using SPSS for windows. Prentice Hall, New Jersey
Lance CE, Butts MM, Michels LC (2006) The sources of four commonly reported cutoff criteria: what did they really say? Organ Res Methods 9:202–220
McHorney CA, Tarlov AR (1995) Individual-patient monitoring in clinical practice: are available health status surveys adequate? Qual Life Res 4:293–307
Morris S, Morris ME, Iansek R (2001) Reliability of measurements obtained with the timed “up & go” test in people with parkinson disease. Phys Ther 81:810–818
Schaafsma JD, Balash Y, Gurevich T, Bartels AL, Hausdorff JM, Giladi N (2003) Characterization of freezing of gait subtypes and the response of each to levodopa in parkinson’s disease. Eur J Neurol 10:391–398
Spildooren J, Vercruysse S, Desloovere K, Vandenberghe W, Kerckhofs E, Nieuwboer A (2010) Freezing of gait in parkinson’s disease: the impact of dual-tasking and turning. Mov Disord 25:2563–2570
Snijders AH, Haaxma CA, Hagen YJ, Munneke M, Bloem BR (2012) Freezer or non-freezer: clinical assessment of freezing of gait. Parkinsonism Relat Disord 18:149–154
Matar E, Shine JM, Gilat M, Ehgoetz Martens KA, Ward PB, Frank MJ, Moustafa AA, Naismith SL, Lewis SJG (2019) Identifying the neural correlates of doorway freezing in parkinson’s disease. Hum Brain Mapp 40:2055–2064
Shah VV, McNames J, Mancini M, Carlson-Kuhta P, Spain RI, Nutt JG, El-Gohary M, Curtze C, Horak FB (2020) Laboratory versus daily life gait characteristics in patients with multiple sclerosis, parkinson’s disease, and matched controls. J Neuroeng Rehabil 17:159
Redgrave P, Rodriguez M, Smith Y, Rodriguez-Oroz MC, Lehericy S, Bergman H, Agid Y, DeLong MR, Obeso JA (2010) Goal-directed and habitual control in the basal ganglia: implications for parkinson’s disease. Nat Rev Neurosci 11:760–772
Macht M, Kaussner Y, Möller JC, Stiasny-Kolster K, Eggert KM, Krüger HP, Ellgring H (2007) Predictors of freezing in parkinson’s disease: a survey of 6,620 patients. Mov Disord 22:953–956
Araújo HAGO, Smaili SM, Morris R, Graham L, Das J, McDonald C, Walker R, Stuart S, Vitório R (2023) Combination of Clinical and gait measures to classify fallers and non-fallers in Parkinson’s Disease. Sensors (Basel) 23(10):4651
Morris R, Smulders K, Peterson DS, Mancini M, Carlson-Kuhta P, Nutt JG, Horak FB (2020) Cognitive function in people with and without freezing of gait in Parkinson’s disease. NPJ Park Dis 6:9
Teramoto H, Morita A, Ninomiya S, Shiota H, Kamei S (2014) Relation between freezing of gait and frontal function in parkinson’s disease. Parkinsonism Relat Disord 20:1046–1049
Gao C, Liu J, Tan Y, Chen S (2020) Freezing of gait in parkinson’s disease: pathophysiology, risk factors and treatments. Transl Neurodegener 9:12
Acknowledgements
We would like to thank all the participants and partners in this study, and Dr. Alice Nieuwboer and Dr. Nir Giladi for giving permission to translate the NFOG-Q.
Funding
Open Access funding provided by Osaka University. This work was partially supported by JSPS KAKENHI Grant Number JP21K17524, and JP23KJ1539.
Author information
Authors and Affiliations
Contributions
ST, KI, HM contributed to the study conception and design. YK, GR contributed to the translation and back-translation processes. ST, KM, TO, CS, ES, MI, HY, RK, EM, RT, YK contributed to the participants recruitment and data collection. ST performed data analysis and wrote the first draft of the manuscript. All authors commented on previous versions of the manuscript, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical statement
The study protocol was approved by the Ethics Committee of Osaka University Hospital (No. 20563) and the Hyogo Prefectural Rehabilitation Hospital at Nishi-Harima (No. 2209). Written informed consent was obtained from all participants.
Conflict of interest
The authors declare they have no financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 80668 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Taniguchi, S., Marumoto, K., Kajiyama, Y. et al. The validation of a Japanese version of the New Freezing of Gait Questionnaire (NFOG-Q). Neurol Sci 45, 3147–3152 (2024). https://doi.org/10.1007/s10072-024-07405-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-024-07405-y