Abstract
The association between cerebral hemodynamics and cognitive impairment has been reported in neurodegenerative and cerebrovascular disorders (CVD). However, it is still unclear whether changes occur in the acute phase of CVD. Here we investigated cognitive and hemodynamic parameters and their association in patients with CVD during the acute and subacute phases. Seventy-three patients with mild stroke, not undergoing endovascular treatment, were recruited. All subjects were devoid of intracranial or external carotid stenosis, significant chronic cerebrovascular pathology, dementia or non-compensated cardiovascular diseases. Patients were evaluated within 7 days from symptoms onset (T1) and after 3 months (T2). Clinical and demographic data were collected. NIHSS, MoCA, FAB, and Word-Color Stroop test (WCST) were used to evaluate disease severity and cognitive functions. Basal hemodynamic parameters in the middle cerebral artery were measured with transcranial Doppler. Differences between T2 and T1, correlations between cognitive and hemodynamic variables at T1 and T2, as well as correlations between the T2-T1 variation in cognitive and hemodynamic parameters were assessed. At T1, cognitive performance of MoCA, FAB, and WCST was lower compared with T2; and pulsatility index, a parameter reflecting distal vascular resistance, was higher. However, no correlations between the changes in cognitive and hemodynamic variables were found; therefore, the two seems to be independent phenomena. In the acute phase, the linear association between cerebral blood flow and cognitive performances was lost, probably due to a differential effect of microenvironment changes and vascular-specific phenomena on cognition and cerebral hemodynamics. This relationship was partially restored in the subacute phase.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
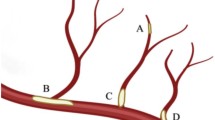
The main mechanisms modulating cerebral hemodynamics, with the aim of adapting cerebral blood flow (CBF) to the metabolic demand of the brain, are cerebral autoregulation, cerebral vasoreactivity (CVR), and neurovascular coupling [1]. These have been incorporated recently into the concept of neurovascular unit, a complex of cellular and extra-cellular structures adapting perfusion to increased metabolic demand in response to local changes in neural activity [2]. Several nuclear medicine and neuroimaging techniques are currently available to measure hemodynamic parameters [3]. Among them, transcranial Doppler sonography (TCD) allows reliable, non-invasive, and inexpensive evaluation of CBF parameters at the level of the main intracranial arteries [4, 5].
Cognitive impairment after an acute cerebrovascular disease (CVD) is rather common, prevalence ranging from 20 to 80% of cases, and may contribute to morbidity and mortality [6]. CVD-related cognitive impairment more frequently involves frontal executive functions, such as attention and working memory [7,8,9,10]. Pathogenesis of CVD-related cognitive alterations is quite complex, due to the interactions between acute ischemic event, pre-existing risk factors, and brain alterations related to age, pathology, and comorbidities [9].
Alterations in CVR and hemodynamics have been described in patients with neurodegenerative and vascular cognitive impairment, and the severity of these alterations seems to correlate with CVR derailment. Furthermore, an increased risk of worsening of cognitive impairment has been associated with alterations in CVR parameters and hemodynamics [11]. Despite the potential interest of the connection between cognitive impairment and altered cerebrovascular hemodynamics, few studies examined such association in patients with acute cerebral ischemia [12,13,14]. Understanding this complex interplay is, however, critical for developing prevention, intervention, and rehabilitation strategies following acute cerebral ischemia.
Given these premises, the aim of the present study was to evaluate executive functions and hemodynamic parameters and their possible association during the acute and subacute phase of acute CVD. We hypothesized transient impairments of cognitive and hemodynamic parameters, undergoing improvement in the subacute stage.
Materials and methods
This was a longitudinal, pilot study aimed at assessing cognitive and hemodynamic parameters in patients with acute CVD in acute and subacute phase, and at evaluating the association between these two factors.
Ethics
The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments. Approval was granted by the Local Ethical Committee of Sapienza University of Rome (Ref. CE 6584_2021). Data collection and processing followed the current European regulation for data protection. All participants provided written informed consent before the beginning of the procedures.
Participants
Patients were consecutively recruited at the Neurology ward and the Stroke Unit of the Sant’Andrea University Hospital, Rome, between April and October 2022. Inclusion criteria were (i) diagnosis of acute mild ischemic stroke with National Institute of Health Stroke Scale (NIHSS) score ≤ 10 and (ii) ability to understand and sign informed consent. Exclusion criteria were (i) stenosis > 50% of the middle cerebral arteries, vertebrobasilar arteries, or intracranial or external carotid arteries defined by MRI or CT scan angiography. Carotid and vertebrobasilar artery stenoses were also assessed by color flow B-mode Doppler ultrasound according to standardized criteria [15]; (ii) severe leukoaraiosis, defined as a Fazekas scale > 2 at brain MRI [16]; (iii) major disability resulting from CVD as defined by a modified Rankin Scale (mRankin) > 4; (iv) other conditions affecting evaluation (e.g., altered mental state, auditory or visual disturbances, etc.); (v) severe respiratory or cardiovascular disease; (vi) uncompensated psychiatric disorder; (vii) preexisting dementia; (viii) aphasia or dysarthria with a score > 1 on NIHSS scoring; and (ix) endovascular treatment of cerebral ischemia (intravenous thrombolysis was not an exclusion criteria).
Study design
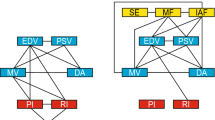
Figure 1 shows the flowchart of the participants throughout the study. Participants were evaluated at baseline, within 7 days from onset of symptoms (T1), and 3 months after the ischemic event (T2). At baseline, demographic and clinical data including age, gender, years of education, smoke habits, alcohol consumption, hypertension, diabetes, dyslipidaemia, arrhythmias, coronary heart disease, previous CVD, and side and location of lesion, were collected for all participants. The stroke severity was evaluated by means of the National Institute of Health Stroke Scale (NIHSS) [17]. The modified Rankin Scale (mRS) [18] was used to assess the functional status and disability of patients before ischemic event. A brain MRI with angiographic sequences was obtained for all participants, and the Fazekas score was calculated. General cognitive functions were assessed using the Montreal Cognitive Assessment (MoCA) [19]. Executive functions were evaluated through the Frontal Assessment Battery (FAB) [20] and the Word-Color Stroop Test (WCST) [21, 22]. All patients underwent TCD with evaluation of cerebral hemodynamics parameters. We used the transtemporal acoustic window to evaluate the blood flow velocity of the middle cerebral artery (MCA). Two dual 2-MHz transducers fitted on a headband were used, granting bilateral continuous measurement of flow velocity in the MCA (Multidop X2 DWL GmbH Compumedics, Germany). Depth of insonation ranged from 48 to 52 mm. Maximum, minimum, and mean MCA blood flow velocity (Vmax, Vmin and Vmean, respectively) and pulsatility index (PI) were recorded in all participants. The average of right and left side was calculated for all TCD-based variables. Cognitive and TCD evaluations were performed both at T1 and T2.
Statistical analysis
Statistical analyses were performed using JASP v0.16.3 (JASP Team, University of Amsterdam), R v4.0.3, and RStudio v2022.07.1 + 554 for Windows (R Foundation for Statistical Computing, Vienna, Austria). Descriptive statistics were calculated for the examined variables. Spearman’s rho correlation coefficient was used to test correlation between clinical and hemodynamic measures at T1 and T2 and to assess the correlation between the T2-T1 variation in cognitive and hemodynamic parameters. To assess the difference between T2 and T1 for the investigated measures, and to compare hemodynamic parameters between the side affected and unaffected by ischemic lesion at T1 and T2, the Wilcoxon test was used. To control error from multiple tests, Bonferroni’s correction of p values was performed. The significance threshold was set at α < 0.05. All data were reported as mean ± SD or median (Q1-Q3) for numerical data and N (%) for categorical variables. For comparisons between T2 and T1, mean difference ± standard error (MD ± SE) were reported.
Results
A total of 102 patients were screened for enrolment; 73 patients fulfilled the inclusion and exclusion criteria and underwent cognitive evaluation at baseline. In 15 patients, no TCD evaluation was performed due to the absence of a proper temporal acoustic window. Of the 73 enrolled patients, nine did not undergo evaluation at T2. Details about population throughout the study are shown in Table 1.
Mean age was 69.5 ± 12.1 years; 40 participants (55%) were males. Median NIHSS score for patients with stroke was 2 (1–4) and median mRS before ischemic event was 0 (0–1). Median Fazekas score was 1 (1–2). As to cerebrovascular risk factors, 53 (73%) participants had hypertension, 40 (55%) had dyslipidaemia, 31 (43%) were smoker, 15 (21%) had a diagnosis of diabetes, and 10 (14%) suffered from atrial fibrillation. In 32 (44%) patients, lesion was on the right-side and in 41 (56%) on the left side. Lesion was localized at cortical level in 17 (19%) patients, at subcortical level in 41 (46%) patients, and at brainstem level in 31 (35%) patients.
Changes between T1 and T2 in the overall population
Wilcoxon test showed a significant reduction at T2 compared to T1 for WCST time (Z = 4.314; P < 0.001; MD ± SE = − 8.1 ± 3.2) and PI (Z = 2.624; P = 0.009; MD ± SE = − 0.07 ± 0.03), together with significant increases in MoCA (Z = − 5.685; P < 0.001; MD ± SE = 2.6 ± 0.3) and FAB (Z = − 3.8321; P < 0.001; MD ± SE = 0.8 ± 0.2) scores (Table 2, Fig. 2).
Cognitive and hemodynamic variables that showed significant changes between T1 and T2. Variables are shown through boxplots, raincloud plots, and violin plots. Thick line in the boxes indicates median; lower and upper box limits indicate first (Q1) and third quartile (Q3), respectively; black vertical lines indicate lower and upper outliers boundaries calculated Q1-(1.5*IQR) and Q3 + (1.5*IQR), respectively. Each green point of the raincloud plot represents a participants at T1 with the respective, connected value in orange at T2. Violin plot shows the kernel density of variables. Panel A Montreal Cognitive Assessment (MoCA). Panel B Frontal Assessment Battery (FAB). Panel C Word-Color Stroop Test time in seconds (WCST). Panel D pulsatility index (PI). IQR, interquartile range
Correlation between cognitive functions and hemodynamics
At T1, Spearman’s test showed no correlations between cognitive and hemodynamic variables. At T2, a weak negative correlation between WCST time and Vmin (ρ = − 0.354; P = 0.015) was found. No correlations between the T2-T1 changes in cognitive and hemodynamic variables were found (Fig. 3). A significant positive correlation between NIHSS score and PI was found both at T1 and T2 (ρ = − 0.322; P = 0.014 and ρ = − 0.464; P < 0.001, respectively).
Differences between affected and unaffected hemisphere in stroke patients
Wilcoxon test showed no significant differences in hemodynamic parameters between affected and unaffected side (Table 3).
Discussion
This was a longitudinal pilot study aimed at assessing cognitive and hemodynamic parameters in patients with acute mild stroke in the acute and subacute phase and at evaluating the possible relationships between these two factors.
Our data suggest that (i) cognitive functions and hemodynamics are transiently impaired during the acute phase of mild stroke, and undergo improvement in the subacute phase; (ii) there is no correlation in the changes in hemodynamic and cognitive parameters between acute and subacute phases. In the subacute phase, a linear association between CBF velocity and cognitive functions was found while this relationship is lost in the acute phase; and (iii) there are no differences in hemodynamic parameters between affected and unaffected hemisphere in stroke patients. These results are discussed in detail in the following.
Changes between T1 and T2
The present results show the improvement of executive functions in the subacute phase (T2) as compared to baseline (T1) in subjects suffering from acute mild stroke. The alteration of cognitive functions after stroke is extremely common and very impactful on disability and quality of life of patients [6, 9]. Previous studies are in line with our results, indicating that, although the cognitive dysfunction in stroke is broad and involves different domains, frontal executive functions, such as working memory and attention, are particularly prone to derangement [8, 10, 23].
Similarly, hemodynamic parameters were altered in the acute phase and returned toward normality in the subacute phase in patients with stroke. Acute ischemic stroke has been shown to induce several processes aimed at facilitating the restoration of adequate blood flow in the infarct zone. The first response after an ischemic insult is the activation of collateral circulation with a redistribution of blood toward ischemic areas. Subsequently, release of chemical factors supporting angiogenesis and vascular remodelling occurs. This latter phenomenon represents one of the long-term responses to ischemia and reperfusion [24].
In the early phase of acute ischemic event, we detected the increased of PI suggesting an increased vascular resistance. These results are in line with previous studies reporting increased PI [13, 25] in the acute phase of ischemic event. Indeed, the increased PI measured proximally to the blood vessels is thought to reflect increased distal vascular resistance and the consequent reduction of diastolic flow, which may depend on alterations of microcirculation [26]. Moreover, in our study, PI increased with increasing NIHSS score, further supporting the presence of an altered vascular mechanism related to stroke severity. After 3 months (T2), these alterations appear reduced, probably because of vascular remodelling and adaptation in the subacute ischemic phase. Previous reports suggested that altered cerebral autoregulation and neurovascular coupling could play a key role to facilitate cerebral tissue perfusion recovery in the first week after acute stroke, but returned to control levels within 3 months [27]. Our results are in line with this hypothesis of dynamic changes of vascular response in the weeks following an acute ischemic event.
Correlation between cognitive functions and hemodynamics
The finding that, in our patients, both cognitive and hemodynamic parameters are altered in the acute phase (T1) and tend to revert toward normality at T2 supports the idea of a possible association between the two phenomena. However, we could not find any significant correlation between the changes in hemodynamic and cognitive parameters at either T1 or T2. In addition, we found a linear association between CBF and executive cognitive functions at T2 but not at T1. These findings are in contrast with a recent study from Altmann and colleagues [13], who reported the association between PI and both global and executive cognitive functions in the acute phase in patients with a lacunar stroke. Since PI is believed to reflect the resistance in the arteries deep in the brain [26], authors concluded that this parameter may be an indicator of small vessel disease, thus explaining the association with cognitive performance. Indeed, in previous studies, PI was significantly higher in patients with vascular dementia compared to patients with Alzheimer’s disease [28]. However, in the study from Altmann and colleagues, no longitudinal evaluation was performed to assess the potential changes in the correlation between hemodynamic parameters and cognitive performance over time. Moreover, this association was found only for patients with lacunar stroke. Conversely, Suministado and collaborators [25] showed no association between cognitive decline and longitudinal changes in hemodynamic parameters between acute and subacute phase. Our results are in line with this latter finding, supporting the idea that both cognitive functions and hemodynamic parameters are dynamically altered in the following months after an acute ischemic event, but the two phenomena seem to be independent.
As to the association between executive performance and CBF, this has been reported before [29, 30]. Frontal and prefrontal cortices, in particular, are brain areas with high oxygen and metabolic demand [31, 32], therefore requiring high blood perfusion. This observation may explain the relationship between CBF and cognitive performance. To our best knowledge, this is the first study investigating this aspect in both the acute (T1) and subacute (T2) phase of stroke. One possible explanation to our results could involve the altered microenvironment and cellular function [33] and the altered neurovascular coupling [27]. Indeed, recent studies showing a negative effect of neurovascular dysfunction on cognitive performance in animal models, suggested that that the disruption of the homeostasis of neuronal proteins and the interference with the delivery of neurotrophic factors needed to maintain a healthy cognition could be crucial in these processes [34]. Impaired perivascular clearance due to altered neurovascular function has also been suggested to play a role in the pathophysiology of cognitive impairment in the context of neurodegenerative disorders [35, 36]. An altered neurovascular unit function is described in CVD [37, 38]; therefore, we could hypothesize that these microenvironmental changes could affect cognitive functions, particularly in the acute phase, while more vascular-specific phenomena including altered cerebral autoregulation and impaired cerebral vasoreactivity [11, 39] could play a more prominent role in the cerebral hemodynamic modifications hereby observed. This could explain why, although both cognitive and hemodynamic parameters are altered in the acute phase of CVD, they showed no association.
The putative differential effect of microenvironment and vascular dysfunction on cognitive and hemodynamic parameters, could also explain why we observed a loss of linear relationship between executive functions and CBF at T1. In the following months, the gradual adaptation and remodelling phenomena (e.g., return toward homeostasis, collateral flow stimulation, neo-angiogenesis, and restoration of cerebral autoregulation) could have led to a new balance and to the re-emergence of this relationship at T2.
According to this hypothesis, the early interval following acute CVDs may represent a period at risk for excessive stimulation of prefrontal cortical areas mediating executive functions such as attention, set shifting, and complex working memory paradigms. This should be taken into account when planning early neurorehabilitation strategies in subjects affected by acute CVD.
Differences between affected and unaffected hemisphere
We did not find any significant difference in hemodynamic parameters between affected and unaffected hemisphere in stroke patients. Regional differences in hemodynamic parameters between affected and unaffected hemisphere have been reported before [27, 40,41,42]. However, regarding hemodynamic parameters measured at the level of MCA, the results are conflicting. Some studies reported no differences in CBF between affected and unaffected hemisphere in stroke patients [43, 44]. Another recent study, on the other hand, found a significant difference of CBF between the affected and unaffected side [45]. However, the difference was significant only in moderate (NIHSS 5–15) and severe stroke (NIHSS > 15). In our study, we included only patients with mild stroke and a NIHSS score ≤ 10 with median score of 2 (1–4); therefore, this could explain the discrepancy with previous data.
Limitations
We acknowledge that our study suffers from limitations due to the non-controlled design and the relative low severity of symptoms of our cohort. Moreover, the lack of a control group and the features of enrolled patients could limit the generalizability of our data due to the relatively good status, differences being potentially found in subjects with more severe stroke symptoms and size. Further studies, including patients with a higher NIHSS, could help addressing this issue. Finally, as a pilot study, the small cohort of patients enrolled prevented performing more advanced analysis, including cerebrovascular risk factors. Considering the complex interplay and the dynamic relationship between cognition, hemodynamic parameters, and CVDs, future studies will be useful to elucidate this aspect.
Conclusions
In conclusion, cognitive functions and hemodynamic parameters are impaired in the acute phase of stroke with an improvement in the subacute phase. However, the two phenomena appear independent. In the acute phase, the linear association between CBF and cognitive functions is lost while this relationship seems restored, at least, partially, in the subacute phase. These results could suggest different underlying phenomena between cognitive and hemodynamic dysfunction following acute CVD. Altered perivascular microenvironment, neurovascular dysfunction, and disrupted homeostasis could play a major role in cognitive dysfunction, while more vascular-specific phenomena, such as altered cerebral autoregulation and impaired cerebral vasoreactivity could be more relevant for cerebral hemodynamic modifications. In subacute phase, the return toward homeostasis as well as vascular remodeling could explain the re-emergence of linear relationship between CBF and cognitive functions. There is no difference between affected and unaffected hemisphere. The results from this study could help better understand the complex network of physiological and pathological phenomena occurring after cerebral ischemic events, design future studies focusing on hemodynamics and cognitive alterations, and guide effective assessment and treatment strategies in mild stroke patients.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Claassen JAHR, Thijssen DHJ, Panerai RB, Faraci FM (2021) Regulation of cerebral blood flow in humans: physiology and clinical implications of autoregulation. Physiol Rev 101:1487–1559. https://doi.org/10.1152/physrev.00022.2020
Kugler EC, Greenwood J, MacDonald RB (2021) The “Neuro-Glial-Vascular” Unit: the role of glia in neurovascular unit formation and dysfunction. Front Cell Dev Biol 9:732820. https://doi.org/10.3389/fcell.2021.732820
Herzig R, Hlustík P, Skoloudík D et al (2008) Assessment of the cerebral vasomotor reactivity in internal carotid artery occlusion using a transcranial Doppler sonography and functional MRI. J Neuroimaging 18:38–45. https://doi.org/10.1111/j.1552-6569.2007.00168.x
Valdueza JM, Balzer JO, Villringer A et al (1997) Changes in blood flow velocity and diameter of the middle cerebral artery during hyperventilation: assessment with MR and transcranial Doppler sonography. AJNR Am J Neuroradiol 18:1929–1934
Herrera CRC, Beltramini GC, Avelar WM et al (2016) Cerebral vasomotor reactivity assessment using transcranial Doppler and MRI with apnea test. Braz J Med Biol Res 49:e5437. https://doi.org/10.1590/1414-431X20165437
Sun J-H, Tan L, Yu J-T (2014) Post-stroke cognitive impairment: epidemiology, mechanisms and management. Ann Transl Med 2:80. https://doi.org/10.3978/j.issn.2305-5839.2014.08.05
van Rooij FG, Kessels RPC, Richard E et al (2016) Cognitive impairment in transient ischemic attack patients: a systematic review. Cerebrovasc Dis 42:1–9. https://doi.org/10.1159/000444282
Riepe MW, Riss S, Bittner D, Huber R (2004) Screening for cognitive impairment in patients with acute stroke. Dement Geriatr Cogn Disord 17:49–53. https://doi.org/10.1159/000074082
Rost NS, Brodtmann A, Pase MP et al (2022) Post-stroke cognitive impairment and dementia. Circ Res 130:1252–1271. https://doi.org/10.1161/CIRCRESAHA.122.319951
Leśniak M, Bak T, Czepiel W et al (2008) Frequency and prognostic value of cognitive disorders in stroke patients. Dement Geriatr Cogn Disord 26:356–363. https://doi.org/10.1159/000162262
Sforza M, Bianchini E, Alivernini D et al (2022) The impact of cerebral vasomotor reactivity on cerebrovascular diseases and cognitive impairment. J Neural Transm (Vienna) 129:1321–1330. https://doi.org/10.1007/s00702-022-02546-w
Sivakumar L, Riaz P, Kate M et al (2017) White matter hyperintensity volume predicts persistent cognitive impairment in transient ischemic attack and minor stroke. Int J Stroke 12:264–272. https://doi.org/10.1177/1747493016676612
Altmann M, Thommessen B, Rønning OM et al (2016) Middle cerebral artery pulsatility index is associated with cognitive impairment in lacunar stroke. J Neuroimaging 26:431–435. https://doi.org/10.1111/jon.12335
Viticchi G, Falsetti L, Potente E et al (2021) Impact of carotid stenosis on cerebral hemodynamic failure and cognitive impairment progression: a narrative review. Ann Transl Med 9:1209. https://doi.org/10.21037/atm-20-7226
von Reutern G-M, Goertler M-W, Bornstein NM et al (2012) Grading carotid stenosis using ultrasonic methods. Stroke 43:916–921. https://doi.org/10.1161/STROKEAHA.111.636084
Fazekas F, Chawluk JB, Alavi A et al (1987) MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol 149:351–356. https://doi.org/10.2214/ajr.149.2.351
Brott T, Adams HP, Olinger CP et al (1989) Measurements of acute cerebral infarction: a clinical examination scale. Stroke 20:864–870. https://doi.org/10.1161/01.str.20.7.864
Saver JL, Chaisinanunkul N, Campbell BCV et al (2021) Standardized nomenclature for modified Rankin Scale global disability outcomes: consensus recommendations from Stroke Therapy Academic Industry Roundtable XI. Stroke 52:3054–3062. https://doi.org/10.1161/STROKEAHA.121.034480
Nasreddine ZS, Phillips NA, Bédirian V et al (2005) The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53:695–699. https://doi.org/10.1111/j.1532-5415.2005.53221.x
Dubois B, Slachevsky A, Litvan I, Pillon B (2000) The FAB: a Frontal Assessment Battery at bedside. Neurology 55:1621–1626. https://doi.org/10.1212/wnl.55.11.1621
Stroop JR (1935) Studies of interference in serial verbal reactions. J Exp Psychol 18:643–662. https://doi.org/10.1037/h0054651
Scarpina F, Tagini S (2017) The Stroop Color and Word Test. Front Psychol 8:557. https://doi.org/10.3389/fpsyg.2017.00557
Edwards JD, Jacova C, Sepehry AA et al (2013) A quantitative systematic review of domain-specific cognitive impairment in lacunar stroke. Neurology 80:315–322. https://doi.org/10.1212/WNL.0b013e31827deb85
Lapi D, Colantuoni A (2015) Remodeling of cerebral microcirculation after ischemia-reperfusion. J Vasc Res 52:22–31. https://doi.org/10.1159/000381096
Suministrado MSP, Shuang EWY, Xu J et al (2017) Poststroke cognitive decline is independent of longitudinal changes in cerebral hemodynamics parameters. J Neuroimaging 27:326–332. https://doi.org/10.1111/jon.12395
Kidwell CS, el-Saden S, Livshits Z et al (2001) Transcranial Doppler pulsatility indices as a measure of diffuse small-vessel disease. J Neuroimaging 11:229–235. https://doi.org/10.1111/j.1552-6569.2001.tb00039.x
Salinet ASM, Panerai RB, Robinson TG (2014) The longitudinal evolution of cerebral blood flow regulation after acute ischaemic stroke. Cerebrovasc Dis Extra 4:186–197. https://doi.org/10.1159/000366017
Sabayan B, Jansen S, Oleksik AM et al (2012) Cerebrovascular hemodynamics in Alzheimer’s disease and vascular dementia: a meta-analysis of transcranial Doppler studies. Ageing Res Rev 11:271–277. https://doi.org/10.1016/j.arr.2011.12.009
Ogoh S (2017) Relationship between cognitive function and regulation of cerebral blood flow. J Physiol Sci 67:345–351. https://doi.org/10.1007/s12576-017-0525-0
Leeuwis AE, Smith LA, Melbourne A et al (2018) Cerebral blood flow and cognitive functioning in a community-based, multi-ethnic cohort: the Sabre study. Front Aging Neurosci 10:279. https://doi.org/10.3389/fnagi.2018.00279
Uzuner N, Özdemir Ö, Tekgöl Uzuner G (2013) Relationship between pulsatility index and clinical course of acute ischemic stroke after thrombolytic treatment. Biomed Res Int 2013:265171. https://doi.org/10.1155/2013/265171
Chi N-F, Hu H-H, Chan L et al (2020) Impaired cerebral autoregulation is associated with poststroke cognitive impairment. Ann Clin Transl Neurol 7:1092–1102. https://doi.org/10.1002/acn3.51075
Freitas-Andrade M, Raman-Nair J, Lacoste B (2020) Structural and functional remodeling of the brain vasculature following stroke. Front Physiol 11:948. https://doi.org/10.3389/fphys.2020.00948
Iadecola C, Smith EE, Anrather J et al (2023) The neurovasculome: key roles in brain health and cognitive impairment: a scientific statement from the American Heart Association/American Stroke Association. Stroke 54:e251–e271. https://doi.org/10.1161/STR.0000000000000431
van Veluw SJ, Hou SS, Calvo-Rodriguez M et al (2020) Vasomotion as a driving force for paravascular clearance in the awake mouse brain. Neuron 105:549-561.e5. https://doi.org/10.1016/j.neuron.2019.10.033
Greenberg SM, Bacskai BJ, Hernandez-Guillamon M et al (2020) Cerebral amyloid angiopathy and Alzheimer disease - one peptide, two pathways. Nat Rev Neurol 16:30–42. https://doi.org/10.1038/s41582-019-0281-2
Forró T, Bajkó Z, Bălașa A, Bălașa R (2021) Dysfunction of the neurovascular unit in ischemic stroke: highlights on microRNAs and exosomes as potential biomarkers and therapy. Int J Mol Sci 22:5621. https://doi.org/10.3390/ijms22115621
Wang L, Xiong X, Zhang L, Shen J (2021) Neurovascular unit: a critical role in ischemic stroke. CNS Neurosci Ther 27:7–16. https://doi.org/10.1111/cns.13561
Jordan JD, Powers WJ (2012) Cerebral autoregulation and acute ischemic stroke. Am J Hypertens 25:946–950. https://doi.org/10.1038/ajh.2012.53
Wang C, Miao P, Liu J et al (2019) Cerebral blood flow features in chronic subcortical stroke: Lesion location-dependent study. Brain Res 1706:177–183. https://doi.org/10.1016/j.brainres.2018.11.009
Toyoda K, Minematsu K, Yamaguchi T (1994) Long-term changes in cerebral blood flow according to different types of ischemic stroke. J Neurol Sci 121:222–228. https://doi.org/10.1016/0022-510x(94)90356-5
Salinet ASM, Robinson TG (1985) Panerai RB (2015) Effects of cerebral ischemia on human neurovascular coupling, CO2 reactivity, and dynamic cerebral autoregulation. J Appl Physiol 118:170–177. https://doi.org/10.1152/japplphysiol.00620.2014
Aries MJ, Elting JW, Stewart R et al (2013) Cerebral blood flow velocity changes during upright positioning in bed after acute stroke: an observational study. BMJ Open 3:e002960. https://doi.org/10.1136/bmjopen-2013-002960
Venkatakrishnan S, Khanna M, Gupta A (2022) Transcranial color coded duplex sonography findings in stroke patients undergoing rehabilitation: an observational study. J Neurosci Rural Pract 13:129–133. https://doi.org/10.1055/s-0041-1742158
Salinet AS, Silva NC, Caldas J et al (2019) Impaired cerebral autoregulation and neurovascular coupling in middle cerebral artery stroke: influence of severity? J Cereb Blood Flow Metab 39:2277–2285. https://doi.org/10.1177/0271678X18794835
Author information
Authors and Affiliations
Contributions
Conceptualization, Michela Sforza, Edoardo Bianchini and Giuliano Sette; methodology, Michela Sforza and Giuliano Sette; formal analysis, Edoardo Bianchini.; participants recruitment, Michela Sforza, Edoardo Bianchini and Diletta Alivernini; investigation, Michela Sforza, Diletta Alivernini, Alessandra Spalloni, Valentina Teresi, Irene Madonia, and Giuliano Sette; data curation, Michela Sforza and Edoardo Bianchini; writing—original draft preparation, Michela Sforza and Edoardo Bianchini; writing—review and editing, Diletta Alivernini, Alessandra Spalloni, Valentina Teresi, Irene Madonia, Marco Salvetti, Francesco E. Pontieri, and Giuliano Sette; supervision, Francesco E. Pontieri and Giuliano Sette. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was granted by the Local Ethical Committee of Sapienza University of Rome (Ref. CE 6584_2021). The study was conducted in accordance with the Declaration of Helsinki and its later amendments. Data collection and processing followed the current European regulation for data protection.
Consent to participate
Written informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Michela Sforza and Edoardo Bianchini contributed equally to the work and share co-first authorship.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sforza, M., Bianchini, E., Alivernini, D. et al. Cerebral hemodynamics and cognitive functions in the acute and subacute stage of mild ischemic stroke: a longitudinal pilot study. Neurol Sci 45, 2097–2105 (2024). https://doi.org/10.1007/s10072-023-07260-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-07260-3