Abstract
Background
About 15% to one third of migraineurs experience aura symptoms. Aura is a reversible focal neurological phenomenon involving visual, sensory, speech, and motor symptoms that usually precede migraine pain. Monoclonal antibodies against calcitonin-related peptide (anti- CGRP mAbs) are effective in preventing chronic and episodic migraine, but little is known about their effectiveness on specifically preventing migraine with aura.
Methods
This is a pilot prospective observational cohort study, aiming at evaluating the effectiveness and safety of Erenumab, Fremanezumab or Galcanezumab for the treatment of migraine aura. We enrolled 14 patients at the Headache Centre of University Federico II of Naples. Duration of follow-up was 12 months. We assessed mean monthly days with aura symptoms, with or without subsequent headache, as well as mean monthly days with headache and mean monthly MIDAS score, by reviewing standardized paper patient headache diaries every three months.
Results
A significant decrease in mean monthly aura days was observed throughout the observation period (median baseline: 13, interquartile range: 4–16; after 12 months: 1, interquartile range: 0–3, p < 0.001). We observed a statistically significant decrease in mean monthly headache days as well (median baseline 21, interquartile range: 16–30; after 12 months: 5, interquartile range: 4–7, p < 0.001). During the 12-month treatment period, none of the 14 patients reported mild or serious adverse events.
Conclusion
Our findings suggest that anti-CGRP mAbs are highly effective in migraine with aura, both in reducing mean monthly aura days and mean monthly days with headache.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Migraine affects a substantial portion of the global population, with an estimated prevalence of 14.7% worldwide [1]. Migraine can manifest with or without aura, and aura symptoms are experienced by approximately 15% to 33% of individuals with migraine [2, 3]. Aura refers to a transient, reversible focal neurological phenomenon that typically precedes the onset of migraine pain. It involves a range of symptoms, including visual disturbances, sensory alterations, speech impairments, and motor abnormalities [4].
While the pathophysiology of migraine with aura remains incompletely understood, it is believed to involve complex neurovascular interactions and cortical spreading depression (CSD) [5, 6]. CSD is a wave of neuronal depolarization that propagates across the cerebral cortex, leading to changes in blood flow and neurochemical activity, possibly contributing to the development of migraine symptoms [7]. The critical event in the initiation and transmission of CSD is characterized by a significant reduction in the resistance of neuronal membranes, accompanied by substantial elevations in extracellular potassium (K +) levels and concurrent elevations in intracellular sodium (Na +) and calcium (Ca2 +) levels [8, 9]. In addition to the changes in the flow of ions, CSD is linked to modifications in the release and dispersion of various substances within the interstitial space, including excitatory neurotransmitters, serotonin, calcitonin gene-related peptide (CGRP), and brain-derived neurotrophic factor [10, 11].
In recent years, monoclonal antibodies targeting calcitonin gene-related peptide (CGRP) and its receptor have emerged as a novel treatment option for migraine prevention. CGRP is a potent vasodilator and a key mediator of neurogenic inflammation. It is released during migraine attacks and is implicated in the pathophysiology of migraines, including those with aura [12].
CGRP has been found to enhance the susceptibility of brain tissue to CSD, potentially making it more likely to occur and propagate [13,14,15]. Additionally, the inhibition in CGRP activity causes inhibition of CSD-mediated vasodilation in various species such as rats, cats, or rabbits [11]. It is speculated that CGRP promotes neurovascular coupling and vasodilation, leading to increased blood flow and facilitating the propagation of CSD across the cortical surface. The interaction between CGRP and the neurovascular system may create a positive feedback loop, exacerbating the occurrence of migraine aura [16].
Anti-CGRP monoclonal antibodies (anti-CGRP mAbs) have demonstrated efficacy in reducing the frequency and severity of both chronic and episodic migraine [17,18,19,20,21]. However, limited research has focused specifically on their effectiveness in preventing migraine aura.
We hypothesize that anti-CGRP mAbs are effective in reducing the occurrence and severity of migraine attacks accompanied by aura symptoms. Therefore, the objective of this study is to evaluate the effectiveness and safety of anti-CGRP mAbs in the prevention of migraine aura.
Methods
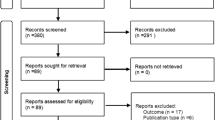
This is a pilot observational cohort study evaluating the effectiveness and safety profiles of Galcanezumab, Fremanezumab, and Erenumab for the treatment of migraine with aura meeting the International Classification of Headache Disorders, 3rd edition (ICHD-3) criteria for migraine with aura [22]. The study was approved by our local ethics committee and all patients gave written informed consent before any procedure linked to the study. The patient's identity was known only to the treating physician and privacy was guaranteed by assigning a pseudonym to each patient. We enrolled 14 patients with migraine with aura at the Headache Centre of the University Federico II of Naples, who were offered for the first time a mAbs prescription between February 2021 and March 2022. A total of 3 patients were excluded from the study because of contraindications to the use of mAbs (severe arterial hypertension, history of cardiovascular or cerebrovascular disease). Inclusion criteria were: diagnosis of migraine with aura fulfilling the ICHD-3 criteria, at least two aura episodes per month in the last 12 months, age greater than or equal to 18 years, and a history of ≥ 3 failed treatments with validated migraine preventatives at a standard dose for at least 2 months. Alternatively, preventive treatments had to be contraindicated. The duration of follow-up was 12 months. Demographics, detailed medical history, and the presence of comorbidities were recorded at baseline. During a 1-month run-in period and for the study duration, patients were asked to complete a paper and pencil headache diary. For this task they recorded daily presence of aura, aura presentation (typical forms such as visual, sensory, speech, motor; or atypical forms), headache, headache duration, headache-related symptoms (photophobia, phonophobia, aura, nausea, vomiting, motion sensitivity), pain intensity using a 0–10 analogue scale (0 no pain, 1–3 mild, 4–7 moderate, 8–10 severe pain), and the use of acute medication to treat headache. Diaries were collected at each treatment prescription and in the absence of a filled-in diary, a prescription was not handed to the patient. For this reason, we did not have missing diaries at any time point, but it is still possible that patients did not fill them in while having a migraine attack.
Erenumab (monthly dose 140 mg), Fremanezumab (monthly dose 225 mg), or Galcanezumab (at initial dose of 240 mg and subsequent monthly doses of 120 mg) were administered according to manufacturers’ recommendations. Patients were allowed to take their current preventive therapies if the dose had been stable for at least 3 months before starting anti-CGRP mAb treatment. Migraine-related clinical burden was assessed with the Migraine Disability Assessment (MIDAS) at baseline and every 3 months for 12 months. Mean monthly days with aura, with or without subsequent headache, occurring during the run-in period, as well as during anti-CGRP mAb treatment, were evaluated by reviewing standardized paper patient headache diaries at baseline and every 3 months during follow-up visits. The same was done with mean monthly days with headache. Migraine monthly days and MIDAS score have both proved to be reliable in clinical studies [23].
The primary outcome of this study was the reduction of mean monthly days with migraine aura after 12 months of continuous treatment with mAbs. The secondary outcomes were the reduction of mean monthly days with headache, MIDAS score, and the use of acute medications to treat headache.
Statistical analysis
Quantitative variables are reported as median and interquartile range given the sample size. Variables normal distribution was checked with the Shapiro–Wilk test. Qualitative variables are given as relative frequencies and percentages. Given the specific structure of the data (longitudinal data), a mixed model approach was used. Given that the outcome was a count variable (number of days), multinomial mixed model with log link function was applied, where patients were used as random effect. Covariance structure for marginal model was unstructured. The linearity of both models was confirmed by a post-hoc analysis. Migraine days, aura days, and MIDAS was needed for the acute phase were used as dependent variables. Statistical significance was set at 0.01 after Bonferroni correction. Statistical analyses were performed using Stata18 (StataCorp., College Station, TX, USA).
Results
Fourteen patients were included in the study (median 38 years, IQR. 31–53). The median duration of the disease was 19 years (IQR: 6–30). Six patients were treated with Fremanezumab, five patients with Galcanezumab and three with Erenumab. All patients had typical aura. Eleven patients had chronic migraine. Demographic and baseline clinical characteristics of patients are fully reported in Table 1.
Overall, a significant decrease in mean monthly days with aura was observed throughout the observation period (median baseline: 13, IQR: 4–16; after 3 months: 3, IQR: 1–4, p < 0.001; after 6 months: 1; IQR: 0–4, p < 0.001; after 9 months: 0, IQR: 0–4, p < 0.001; after 12 months: 1, IQR: 0–3, p < 0.001) (Fig. 1). There was no statistically significant difference in mean monthly days with aura between patients with different monoclonal antibodies (p = 0.613).
There was a statistically significant decrease in mean monthly headache days after three months (median baseline 21, IQR: 16–30; three months: 7, IQR: 6–8, p < 0.001), which remained statistically low compared to baseline over the entire observation period (6 months: 7, IQR: 6–8, p < 0.001; 9 months: 6, IQR: 4–7, p < 0.001; 12 months: 5, IQR: 4–7, p < 0.001) (Fig. 2). Mean monthly days with headache was not statistically different between the three monoclonal antibodies (interaction term p = 0.884).
Overall, MIDAS showed a statistically significant reduction from baseline (median: 55, IQR: 43–81) throughout the observation period (after 3 months: 19, IQR: 16–22, p < 0.001; after 6 months: 19, IQR: 16–22, p < 0.001; after 9 months: 16, IQR: 11–22, p < 0.001; after 12 months: 14, IQR: 11–19, p < 0.001) (Fig. 3). There were no differences in MIDAS compared to the monoclonal antibodies (p = 0.913).
During the 12-month treatment period, none of the 14 patients reported mild or serious adverse events.
Discussion
The results of our study provide valuable clinical evidence supporting the role of CGRP in the pathophysiology of migraine with aura. We observed a significant reduction in the mean monthly days with migraine aura in patients receiving anti-CGRP monoclonal antibodies. This finding suggests that targeting CGRP can effectively mitigate the occurrence and severity of migraine aura, further supporting the hypothesis that CGRP is implicated in the initiation and propagation of CSD.
CGRP has emerged as a key player in the pathophysiology of migraine, and its involvement in the activation of cortical spreading depression has been investigated in recent years. CSD is a phenomenon characterized by a wave of neuronal hyperactivity followed by a period of depression, and it is strongly associated with migraine aura [6].
CGRP has been shown to increase neuronal excitability, which can trigger CSD by promoting sustained depolarization and facilitating the spread of neuronal activity across the cortex [24]. The excitatory effects of CGRP may be mediated through its direct action on ion channels and receptors, leading to enhanced neuronal firing and synaptic transmission. Additionally, CGRP can stimulate the release of other neurotransmitters, such as glutamate, which is known to play a pivotal role in the initiation and propagation of CSD [25]. Interestingly, CSD itself stimulates the release of CGRP, suggesting a bidirectional and reciprocal interaction [14, 16].
A recent study by Tozzi et al. demonstrated inhibition of CSD by blocking the CGRP receptor in an in vitro model, reinforcing the hypothesis of a CGRP contribution in the pathogenesis of CSD [14]. In another study by Jiang et al. it was found that transient receptor potential ankyrin A1 (TRPA1), whose activation is known to stimulate CGRP release in the trigeminal ganglion, plays a pivotal role in CSD propagation, and it has been suggested that the activation of TRPA1 and production of CGRP by reactive oxygen species (ROS) initiate a feedback loop that regulates cortical susceptibility to CSD, so that CGRP may enhance the propagation of CSD [13, 26, 27].
Over the last years, there has been a report by Matteo et al. pointing out the effectiveness of Erenumab in reducing aura frequency [28], and a small case-series of 2 patients by Albanese and Mercuri in which Galcanezumab and Erenumab were effective in treating and reducing aura frequency, duration and intensity [29], providing an initial clinical evidence regarding anti-CGRP mAbs effectiveness in migraine aura. In a very recent study on migraine with aura patients it was demonstrated that, following intravenous CGRP infusion, 38% of the patients developed aura symptoms, further underscoring the involvement of CGRP in aura mechanisms [30].
By blocking the action of CGRP, anti-CGRP mAbs can modulate the excitability of neurons, inhibit the release of other neurotransmitters involved in CSD, and attenuate the susceptibility of brain tissue to CSD. This multifaceted mechanism of action may contribute to the observed reduction in mean monthly days with migraine aura in our study.
In addition to the impact on migraine aura, anti-CGRP mAbs have also demonstrated efficacy in reducing the frequency and severity of migraine attacks in general. Previous studies have shown that these medications can effectively prevent both episodic and chronic migraines, as well as other rarer subtypes of migraine such as vestibular migraine [21, 31]. The broader clinical benefits observed with anti-CGRP mAbs further support their potential as a comprehensive treatment option for migraineurs, addressing both the aura symptoms and the headache phase.
It is important to note that while our study provides promising results regarding the reduction of mean monthly days with migraine with aura following treatment with anti-CGRP mAbs, further research is warranted to elucidate the underlying mechanisms and confirm the generalizability of these findings. A recent study using animal models of migraine aura found that Fremanezumab was able to slow the propagation of CSD but didn’t prevent its initiation [32], suggesting that other mechanisms are involved in CSD initiation, and future studies should explore the specific effects of anti-CGRP mAbs on initiation of CSD and CSD parameters, such as propagation velocity and duration, to provide a more comprehensive understanding of their impact on the pathophysiology of migraine with aura. Finally, beyond CSD other mechanisms may also play a role in the pathogenesis of migraine with aura, necessitating further investigation into potential therapeutic interventions.
This work has some limitations, mainly due to the nature of a pilot study and thus the small sample size, which prevents a generalisation of our findings. Future research should be conducted with a larger sample to confirm these preliminary results.
Conclusion
Our findings support the hypothesis that CGRP may play a crucial role in CSD and development of migraine aura. These results provide valuable insights into the therapeutic potential of anti-CGRP mAbs as a targeted treatment for migraineurs with aura. Further investigations are needed to elucidate the precise mechanisms by which CGRP influences CSD and aura symptoms and to optimize the clinical management of migraine with aura.
References
Steiner TJ, Stovner LJ, Birbeck GL (2013) Migraine: the seventh disabler. J Headache Pain 14(1):1. https://doi.org/10.1186/1129-2377-14-1
Rasmussen BK, Olesen J (1992) Migraine with aura and migraine without aura: an epidemiological study. Cephalalgia 12(4):221–186. https://doi.org/10.1046/j.1468-2982.1992.1204221.x
Lucas C (2021) Migraine with aura. Rev Neurol 177(7):779–784. https://doi.org/10.1016/j.neurol.2021.07.010
Goadsby PJ, Holland PR, Martins-Oliveira M, Hoffmann J, Schankin C, Akerman S (2017) Pathophysiology of migraine: a disorder of sensory processing. Physiol Rev 97(2):553–622. https://doi.org/10.1152/physrev.00034.2015
Charles A (2013) Migraine: a brain state. Curr Opin Neurol 26(3):235–239. https://doi.org/10.1097/WCO.0b013e32836085f4
Lauritzen M, Dreier JP, Fabricius M, Hartings JA, Graf R, Strong AJ (2011) Clinical relevance of cortical spreading depression in neurological disorders: migraine, malignant stroke, subarachnoid and intracranial hemorrhage, and traumatic brain injury. J Cereb Blood Flow Metab 31(1):17–35. https://doi.org/10.1038/jcbfm.2010.191
Charles A (2018) The pathophysiology of migraine: implications for clinical management. The Lancet Neurology 17(2):174–182. https://doi.org/10.1016/S1474-4422(17)30435-0
Akerman S, Goadsby PJ (2005) Topiramate inhibits cortical spreading depression in rat and cat: impact in migraine aura. NeuroReport 16(12):1383–1387. https://doi.org/10.1097/01.wnr.0000175250.33159.a9
Somjen GG (2001) Mechanisms of spreading depression and hypoxic spreading depression-like depolarization. Physiol Rev 81(3):1065–1096. https://doi.org/10.1152/physrev.2001.81.3.1065
Cozzolino O, Marchese M, Trovato F, Pracucci E, Ratto GM, Buzzi MG, Sicca F, Santorelli FM (2018) Understanding spreading depression from headache to sudden unexpected death. Front Neurol 9:19. https://doi.org/10.3389/fneur.2018.00019
Mathew AA, Panonnummal R (2022) Cortical spreading depression: culprits and mechanisms. Exp Brain Res 240(3):733–749. https://doi.org/10.1007/s00221-022-06307-9
Edvinsson L (2019) Role of CGRP in migraine. Handb Exp Pharmacol 255:121–130. https://doi.org/10.1007/164_2018_201
Jiang L, Wang Y, Xu Y, Ma D, Wang M (2018) The transient receptor potential ankyrin type 1 plays a critical role in cortical spreading depression. Neuroscience 382:23–34. https://doi.org/10.1016/j.neuroscience.2018.04.025
Tozzi A, de Iure A, Di Filippo M, Costa C, Caproni S, Pisani A, Bonsi P, Picconi B, Cupini LM, Materazzi S, Geppetti P, Sarchielli P, Calabresi P (2012) Critical role of calcitonin gene-related peptide receptors in cortical spreading depression. Proc Natl Acad Sci USA 109(46):18985–18990. https://doi.org/10.1073/pnas.1215435109
Filiz A, Tepe N, Eftekhari S, Boran HE, Dilekoz E, Edvinsson L, Bolay H (2019) CGRP receptor antagonist MK-8825 attenuates cortical spreading depression induced pain behavior. Cephalalgia 39(3):354–365. https://doi.org/10.1177/0333102417735845
Close LN, Eftekhari S, Wang M, Charles AC, Russo AF (2019) Cortical spreading depression as a site of origin for migraine: role of CGRP. Cephalalgia 39(3):428–434. https://doi.org/10.1177/0333102418774299
Drellia K, Kokoti L, Deligianni CI, Papadopoulos D, Mitsikostas DD (2021) Anti-CGRP monoclonal antibodies for migraine prevention: a systematic review and likelihood to help or harm analysis. Cephalalgia 41(7):851–864. https://doi.org/10.1177/0333102421989601
Vernieri F, Altamura C, Brunelli N, Costa CM, Aurilia C, Egeo G, Fofi L, Favoni V, Pierangeli G, Lovati C, Aguggia M, d'Onofrio F, Doretti A, Di Fiore P, Finocchi C, Rao R, Bono F, Ranieri A, Albanese M, Cevoli S, Barbanti P, GARLIT Study Group (2021) Galcanezumab for the prevention of high frequency episodic and chronic migraine in real life in Italy: a multicenter prospective cohort study (the GARLIT study). J Headache Pain 22(1):35. https://doi.org/10.1186/s10194-021-01247-1
Driessen MT, Cohen JM, Thompson SF, Patterson-Lomba O, Seminerio MJ, Carr K, Totev TI, Sun R, Yim E, Mu F, Ayyagari R (2022) Real-world effectiveness after initiating fremanezumab treatment in US patients with episodic and chronic migraine or difficult-to-treat migraine. J Headache Pain 23(1):56. https://doi.org/10.1186/s10194-022-01415-x
Cullum CK, Do TP, Ashina M, Bendtsen L, Hugger SS, Iljazi A, Gusatovic J, Snellman J, Lopez-Lopez C, Ashina H, Amin FM (2022) Real-world long-term efficacy and safety of erenumab in adults with chronic migraine: a 52-week, single-center, prospective, observational study. J Headache Pain 23(1):61. https://doi.org/10.1186/s10194-022-01433-9
Saccà F, Braca S, Sansone M, Miele A, Stornaiuolo A, De Simone R, Russo CV (2023) A head-to-head observational cohort study on the efficacy and safety of monoclonal antibodies against calcitonin gene-related peptide for chronic and episodic migraine. Headache 63(6):788–794. https://doi.org/10.1111/head.14528
Headache Classification Committee of the International Headache Society (IHS) (2018) The international classification of headache disorders, 3rd edition. Cephalalgia 38(1):1–211. https://doi.org/10.1177/0333102417738202
Stewart WF, Lipton RB, Dowson AJ, Sawyer J (2001) Development and testing of the Migraine Disability Assessment (MIDAS) Questionnaire to assess headache-related disability. Neurology 56(6 Suppl 1):S20–S28. https://doi.org/10.1212/wnl.56.suppl_1.s20
Charles AC, Baca SM (2013) Cortical spreading depression and migraine. Nat Rev Neurol 9(11):637–644. https://doi.org/10.1038/nrneurol.2013.192
Ayata C, Lauritzen M (2015) Spreading depression, spreading depolarizations, and the cerebral vasculature. Physiol Rev 95(3):953–993. https://doi.org/10.1152/physrev.00027.2014
Shatillo A, Koroleva K, Giniatullina R, Naumenko N, Slastnikova AA, Aliev RR, Bart G, Atalay M, Gu C, Khazipov R, Davletov B, Grohn O, Giniatullin R (2013) Cortical spreading depression induces oxidative stress in the trigeminal nociceptive system. Neuroscience 253:341–349. https://doi.org/10.1016/j.neuroscience.2013.09.002
Jiang L, Ma D, Grubb BD, Wang M (2019) ROS/TRPA1/CGRP signaling mediates cortical spreading depression. J Headache Pain 20(1):25. https://doi.org/10.1186/s10194-019-0978-z
Matteo E, Pensato U, Favoni V, Giannini G, Pierangeli G, Cevoli S (2021) Do anti-CGRP drugs have a role in migraine aura therapy? J Neurol 268(6):2273–2274. https://doi.org/10.1007/s00415-021-10546-1
Albanese M, Mercuri NB (2022) Could the new anti-CGRP monoclonal antibodies be effective in migraine aura? Case reports and literature review. J Clin Med 11(5):1228. https://doi.org/10.3390/jcm11051228
Al-Khazali HM, Ashina H, Wiggers A, Rose K, Iljazi A, Christensen RH, Schytz HW, Amin FM, Ashina M (2023) Calcitonin gene-related peptide causes migraine aura. J Headache Pain 24(1):124. https://doi.org/10.1186/s10194-023-01656-4
Russo CV, Saccà F, Braca S, Sansone M, Miele A, Stornaiuolo A, De Simone R (2023) Anti-calcitonin gene-related peptide monoclonal antibodies for the treatment of vestibular migraine: A prospective observational cohort study. Cephalalgia 43(4):3331024231161809. https://doi.org/10.1177/03331024231161809
Melo-Carrillo A, Schain AJ, Stratton J, Strassman AM, Burstein R (2020) Fremanezumab and its isotype slow propagation rate and shorten cortical recovery period but do not prevent occurrence of cortical spreading depression in rats with compromised blood-brain barrier. Pain 161(5):1037–1043. https://doi.org/10.1097/j.pain.0000000000001791
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethic approval and patient consent
The study was approved at our local ethics committee and all patients gave written informed consent before any procedure linked to the study. The study conforms with World Medical Association Declaration of Helsinki.
Conflicting interests
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: CVR received personal compensation from Sanofi Genzyme, Eli Lilly and Merck Serono. SB and RDS received personal compensation from Lilly for oral presentations. AM, AS and GC declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Braca, S., Miele, A., Stornaiuolo, A. et al. Are anti-calcitonin gene-related peptide monoclonal antibodies effective in treating migraine aura? A pilot prospective observational cohort study. Neurol Sci 45, 1655–1660 (2024). https://doi.org/10.1007/s10072-023-07241-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-07241-6