Abstract
A 37-year-old migrainous woman was referred several hours after a sudden dysarthria lasting less than 1 min. Brain MRI undertaken a few hours later showed no acute cerebral infarction on the diffusion-weighted imaging (DWI) sequence. However, an intraluminal thrombus within a distal branch of the middle cerebral artery (MCA) was seen on the T2*-weighted gradient echo images as well as hyperintense vessels related to slow flow beyond the occlusion’s site. Control MRI 24 h later confirmed the presence of a small infarct affecting the distal portion of the MCA territory but the thrombus was no longer visible. A comprehensive etiologic workup revealed the presence of a patent foramen ovale, as the underlying cause of the patient’s stroke. Though the sensitivity of DWI sequence for acute ischemia is high, false negative exist particularly in cases of transient ischemic attack, brainstem or lacunar strokes. A careful brain MRI examination or the use of perfusion weighted imaging sequences are useful to avoid misdiagnosis particularly in young patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A 37-year-old migrainous woman was referred for dysarthria during a conversation. Dysarthria was with sudden onset, lasted less than 1 min and was accompanied by a migraine headache identical to the patient’s usual ones.
She was admitted many hours after the symptom’s resolution. General and neurological examinations were unremakable.
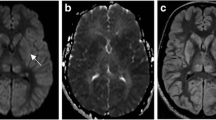
Brain MRI undertaken a few hours later showed no acute cerebral infarction on the diffusion-weighted imaging (DWI) sequence. However an intraluminal thrombus within a distal branch of the middle cerebral artery (MCA) was seen on the T2*-weighted gradient echo images as well as hyperintense vessel related to slow flow beyond the occlusion’s site. Intravenous thrombolysis was not indicated because the patient was asymptomatic and out the therapeutic time window. Control MRI 24 h later confirmed the presence of a small infarct affecting the distal portion of the MCA territory but the thrombus was no longer visible (Fig. 1).
Initial DWI sequence showed no acute cerebral infarct (A). T2*-weighted gradient echo image disclosed a distal MCA occlusion located within the M4 segment (B) as well as hyperintense vessels beyond the site of occlusion (C). On the 24-h control MRI, axial DWI sequence demonstrated a small hyperintense lesion affecting the distal part of the MCA territory (D) associated with severe apparent diffusion coefficient decrease (not shown) corresponding to an acute brain infarction. The corresponding thrombus of the affected artery was no longer seen (not shown)
No arterial dissection was seen on cervical MRI. After a complete etiologic workup, no identifiable cause other than a patent foramen ovale with large interatrial shunt was found. Thus, she benefited from a transcatheter closure without stroke recurrence during the follow-up.
Though the sensitivity of DWI sequence for acute ischemia is high, false negative can occur particularly in cases of transient ischemic attack, brainstem strokes or lacunar syndromes [1]. According to some studies, up to one third of patients with nondisabling stroke do not have an acute lesion on DWI sequence [2]. Several explanations have been suggested. Concerning brainstem or lacunar strokes, technical concerns such as artifacts and slice gap thickness may be an explanation. In other cases, DWI negativity could be attributable to DWI reversal due to early recanalization, for example after thrombolytic treatment [3]. A small proportion of patients could also have reduced perfusion not severe enough to produce DWI abnormality at the time of MRI [1, 2]. Hyperintense vessels on FLAIR imaging are often observed distal to arterial occlusion, more frequently when the occlusion is proximal. They represent slow retrograde flow through collaterals distal to the occlusion’s site, as in our patient [4].
Despite a negative DWI sequence, stroke diagnosis is easy to suspect in the setting of persistent neurological symptoms in a patient with vascular risk factors especially when a proximal arterial occlusion is seen on MR angiogram. Conversely our patient was younger, without vascular risk factors and with a very transient deficit. Moreover the intraluminal thrombus and hyperintense vessels were difficult to see because of their very distal location. Only the realization of a follow-up MRI led to the diagnosis of stroke.
To conclude, physicians should not hesitate to perform an early control MRI when the diagnosis of cerebral infarction is suspected despite a normal initial DWI sequence even in a young patient.
References
Sylaja PN, Coutts SB, Krol A, Hill MD, Demchuk AM; VISION Study Group (2008) When to expect negative diffusion-weighted images in stroke and transient ischemic attack. Stroke 39:1898–900
Makin SD, Doubal FN, Dennis MS, Wardlaw JM (2015) Clinically confirmed stroke with negative diffusion-weighted imaging magnetic resonance imaging: longitudinal study of clinical outcomes, stroke recurrence, and systematic review. Stroke 46:3142–3148
Kidwell CS, Saver JL, Mattiello J, Starkman S, Vinuela F, Duckwiler G, Gobin YP, Jahan R, Vespa P, Kalafut M, Alger JR (2000) Thrombolytic reversal of acute human cerebral ischemic injury shown by diffusion/perfusion magnetic resonance imaging. Ann Neurol 47:462–469
Lee KY, Latour LL, Luby M, Hsia AW, Merino JG, Warach S (2009) Distal hyperintense vessels on FLAIR: an MRI marker for collateral circulation in acute stroke? Neurology 72(13):1134–1139
Funding
No funding was reported.
Author information
Authors and Affiliations
Contributions
Dr Benjamin Hebant, MD: Study concept and design.
Dr Linda Zourdani, MD: Critical revision of the manuscript for important intellectual content.
Dr Camille Dagba, MD: Critical revision of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hebant, B., Zourdani, L. & Dagba, C. Stroke in a young adult: looking beyond the diffusion-weighted imaging sequence. Neurol Sci 45, 1315–1317 (2024). https://doi.org/10.1007/s10072-023-07237-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-07237-2