Abstract
Objective
Insomnia disorder with objective short sleep duration (ISS) has been considered as a biologically severe subtype. The aim of this meta-analysis was to reveal the association of the ISS phenotype and cognitive performance.
Methods
We searched PubMed, EMBASE, and the Cochrane Library for studies that observed an association of cognitive performance and insomnia with objective short sleep duration (ISS) phenotype. The “metafor” and “MAd” packages in R software (version 4.2.0) were used to calculate the unbiased standardized mean difference (Hedge’s g), which was adjusted so that a negative value indicated worse cognitive performance.
Results
The pooled analysis with 1339 participants revealed that the ISS phenotype was associated with overall cognitive impairments (Hedges’ g = − 0.56 [− 0.89, − 0.23]), as well as specific cognitive domains including attention (Hedges’ g = − 0.86 [− 1.25, − 0.47]), memory (Hedges’ g = − 0.47 [− 0.82, − 0.12]), and executive function (Hedges’ g = − 0.39 [− 0.76, − 0.02]). However, cognitive performance was not significantly different between insomnia disorder with objective normal sleep duration (INS) and good sleepers (p > .05).
Conclusion
Insomnia disorder with the ISS phenotype, but not the INS phenotype, was associated with cognitive impairments, suggesting the possible utility of treating the ISS phenotype to improve cognitive performance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Insomnia disorder is defined as difficulty initiating sleep, maintaining sleep, or early-morning awakening, and the predominant complaints at least 3 nights per week for at least 3 months with associated daytime impairment [1, 2]. Approximately, 30% of the general population experience insomnia symptoms, and 10% experience chronic disorder [3]. Sleep is inherently a multidimensional biobehavioral process. To understand insomnia disorder using a multidimensional clinical approach, the insomnia with objective short sleep duration (ISS) phenotype is developed by relying on both self-reported and objectively measured domains [4]. A proposed hallmark of the ISS phenotype is physiologic hyperarousal, reflecting 24-h activation of the stress system, and has been considered as a biologically severe subtype of insomnia disorder [5].
Although a causal link of the ISS phenotype with physical health has been suggested, a potential causal link with the cognitive impairment remains elusive [6]. Mild cognitive impairment (MCI) is considered a precursor of Alzheimer’s disease (AD). Increasing evidences suggest that insomnia disorder makes individuals be vulnerable to developing MCI and progress into AD [7]. In this case, if we can confirm a causal link of the ISS phenotype with cognitive impairment, an opportunity of early intervention for insomnia disorder may be provided to prevent the progression to AD.
Therefore, we performed a meta-analysis to identify the association between insomnia disorder with the ISS phenotype and cognitive performance.
Methods
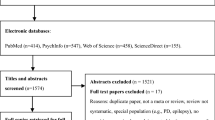
This meta-analysis was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) protocol [8].
We searched PubMed, EMBASE, and the Cochrane Library for studies that observed an association of cognitive performance and insomnia with objective short sleep duration (ISS) phenotype through Aug. 31, 2022 by using combination of “insomnia” AND “cognitive” or “cognition” or “neuropsychology.”
Inclusion and exclusion criteria
The PICOS principle were following (1) patients with insomnia disorder diagnosed with DSM (Diagnostic and Statistical Manual of Mental Disorders) or ICD (International Classification of Diseases) criteria, excluding comorbidity insomnia and obstructive sleep apnea; (2) the ISS phenotype defined as less than 6 h of total sleep using polysomnography (PSG); (3) comparisons with good sleepers or insomnia with objective normal sleep duration (INS) phenotype (more than 6h total sleep); and (4) available cognitive performance measures, including a battery of standardized neuropsychological tests commonly used in clinical practice to assess a wide range of cognitive domains before the sleep recording. The classification of cognitive domains used the previous definition [9].
Data extraction and quality assessment
Two independent raters (D.R. and Z.G.) abstracted data using a standardized form, and discrepancies were resolved by discussion. To facilitate comparison and continuity, cognitive domains were classified according to the previous criteria [9, 10].
The included studies were assessed using the Newcastle-Ottawa Scale (NOS) for non-randomized studies. A study is judged by the NOS on three broad perspectives: the selection of the study groups, the comparability of the groups, and the ascertainment of either the exposure or outcome of interest for case-control studies [8].
Statistical analysis
The “metafor” and “MAd” packages in R software (version 4.2.0) were used to calculate the unbiased standardized mean difference (Hedge’s g), which was adjusted so that a negative value indicated worse cognitive performance.
Given that multiple measures within the same cognitive domain were often used, we firstly implemented the “BHHR” method in the “MAd” package to aggregate dependent effect sizes into only a single effect size [11, 12]. The aggregation of dependent effect sizes contributed only one effect size for each cognitive domain from each independent sample. Secondly, we further aggregated effect sizes across cognitive domains, so that each independent sample only contributed one effect size. Lastly, we conducted an omnibus meta-analysis to examine the overall effect of the ISS phenotype on cognitive performance across all cognitive domains and studies.
Results
We identified five studies [13,14,15,16,17] to make omnibus meta-analysis (Fig. 1) with 1339 participants, including 241 patients with the ISS phenotype, 235 patients with the INS phenotype, and 863 good sleepers (Table 1). The quality scores of the single included studies ranged from five to eight stars, with a mean quality score of 7.2 and a standard deviation of 0.84.
Compared to patients with the INS phenotype, the overall cognitive performance was significantly impaired in patients with the ISS phenotype (Hedges’ g = − 0.56, 95% CI [− 0.89, − 0.23]), as well as in cognitive domains of attention (Hedges’ g = − 0.86, 95% CI [− 1.25, − 0.47]), memory (Hedges’ g = − 0.47, 95% CI [− 0.82, − 0.12]), and executive function (Hedges’ g = − 0.39, 95% CI [− 0.76, − 0.02]) (Fig. 2). The heterogeneity statistic was not significant in omnibus meta-analyses with standardized mean difference (SMD) as effect size (Fig. S1 and S2).
Forest plot of the omnibus meta-analyses. Compared to insomnia with objective normal sleep duration (INS) phenotype, insomnia with objective short sleep duration (ISS) phenotype significantly impairs overall cognitive performance (Hedges’ g = -0.56, p < 0.001), as well as specific cognitive domains including attention (Hedges’ g = -0.86, p<0.001), memory (Hedges’ g = -0.47, p = 0.02), and executive function (Hedges’ g = -0.39, p = 0.04). Compared to good sleepers, impaired cognitive performance is not significantly different (p > 0.05) in the insomnia with objective normal sleep duration (INS) phenotype
The cognitive performance was not significantly different between patients with the INS phenotype and good sleepers, in terms of overall cognitive performance, general cognitive function, attention, memory, and executive function (Fig. 2). The heterogeneity statistic was not significant in most omnibus meta-analyses with standardized mean difference (SMD) as effect size (Fig. S1 and S2).
Publication bias with funnel plot analysis indicated that there was no significant asymmetry (p = .24). We did not conduct a meta-regression analysis to reveal potential moderating effects of age, gender, body mass index (BMI), or education in the omnibus meta-analysis because of limited original data.
Discussion
The current meta-analysis indicated that insomnia with objective short sleep duration (ISS) phenotype significantly impaired overall cognitive performance, as well as specific cognitive domains including attention, memory, and executive function. However, insomnia with objective normal sleep duration (INS) phenotype did not show a significant effect on poorer cognitive performance.
It is very meaningful to reveal the relationship of insomnia with poorer cognitive performance due to the negative effects of cognitive impairment, such as lower quality of life, increased costs of care, increased accidents, and morbidity [18,19,20]. A better understanding of the relationship between insomnia and cognitive performance may inform potential interventions to improve cost-effectiveness of impaired cognition on health. Previous meta-analysis studies have found that insomnia is associated with deficits in objective and subjective cognitive performance, highlighting the utility of treating insomnia disorder to potentially improve cognitive outcomes [9, 10, 21].
However, insomnia disorder is multidimensional; specific phenotype may have specific etiology, pathophysiology, clinical features, natural course, downstream consequences, and intervention procedures [22, 23]. Insomnia with objective short sleep duration (ISS) phenotype as a disorder of physiologic hyperarousal emphasizes the clinical importance of considering the quality and duration of sleep, as well as its perceived and objective aspects [4]. Different from previous meta-analysis studies on the association of insomnia disorder with cognitive performance, we divided insomnia disorder into the ISS subtype and the INS subtype. Our findings indicated that cognitive impairments were associated with the ISS phenotype, but the INS phenotype did not impair cognitive performance. This result is also proved by a previous study that the risk of cognitive disorder is significantly elevated when the nocturnal sleep duration is shortened [21].
Specifically, we found that the ISS phenotype was associated with large (Hedges’ g = − 0.86) deficits in attention. Attention is traditionally measured using reaction time, which is a sensitive measure of cognitive performance. Wang et al. found that reaction time was significantly increased after sleep deprivation, and the increased reaction time was correlated with altered anterior insula-superior frontal gyrus functional connectivity [24]. They suggested that functional connectivity abnormalities in the anterior insular subregions represented a neuroimaging biomarker of sleep deprivation-associated cognitive impairment. As a form of chronic sleep deprivation, the ISS phenotype is more likely to damage functional connectivity by complex phenotype-genotype associations based on the genetic underpinnings of sleep deprivation-induced impairments in human cognition [25].
The small to moderate deficits in memory and executive function were in alignment with results from the 2019 meta-analysis conducted by Wardle-Pinkston et al. [10]. In their study, the smaller effect size might be related to the mixing of the ISS and the INS phenotypes. Impaired memory and executive function emphasize the detrimental impact of the ISS phenotype on daytime performance. Memory involves an individual’s ability to retain and manage information in the short-term memory, or the learning of new material and recalling them after a delay. The ISS phenotype increases hypothalamic pituitary adrenal axis and sympathetic nervous system activations, which has been proved to be positively correlated with memory deficits [26]. The executive function appears to be more complex and more impacted by the negative effects of the ISS phenotype.
Recent studies have attempted to link the ISS phenotype with altered neurocognitive function and potential increased risk of cognitive impairments, indicating lower gamma-aminobutyric acid (GABA) levels in the anterior cingulate cortex, greater waking connectivity between the retrosplenial cortex/hippocampus and various nodes of the default mode network (DMN), and decreased glutamate metabolites and brain-derived neurotrophic factor [27,28,29]. These results indicated that managing ISS phenotype might serve as a promising target for cognitive impairment prevention.
There were some limitations in the current meta-analysis. First, despite that the Failsafe-N analysis and publication bias results indicated our findings were relatively robust, the sample size was small. Second, the included studies were cross-sectional and no causal relationship could be drawn. Third, cognitive measures varied greatly between the enrolled studies. Therefore, there is a need for large, multicenter, longitudinal studies using objective cognitive and sleep measures, as well as developing standardized battery of cognitive performance to facilitate comparison and replication of results.
In conclusion, this meta-analysis revealed that insomnia disorder with ISS phenotype is associated with cognitive impairments, including overall cognitive performance and specific cognitive domains. While cognitive performance is not significantly different between patients with INS phenotype and good sleepers, that suggests the possible utility of treating ISS phenotype, but not INS phenotype, to improve cognitive performance. In the future, multicenter, longitudinal studies with standardized battery of cognitive measures are needed to draw a potential causal relationship.
References
Association AP (2013) Diagnostic and Statistical Manual of Mental Disorders, 5th edn. American Psychiatric Association, Arlington
Medicine AAoS (2014) International Classification of Sleep Disorders (ICSD): Diagnostic and Coding Manual, 3rd edn. American Academy of Sleep Medicine, Westchester
Ohayon MM (2002) Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev 6:97–111
Vgontzas AN, Fernandez-Mendoza J, Liao D, Bixler EO (2013) Insomnia with objective short sleep duration: the most biologically severe phenotype of the disorder. Sleep Med Rev 17:241–54
Fernandez-Mendoza J (2017) The insomnia with short sleep duration phenotype: an update on it’s importance for health and prevention. Curr Opin Psychiatry 30:56–63
Johnson KA, Gordon CJ, Chapman JL, Hoyos CM, Marshall NS, Miller CB et al (2021) The association of insomnia disorder characterised by objective short sleep duration with hypertension, diabetes and body mass index: a systematic review and meta-analysis. Sleep Med Rev 59:101456
Benedict C, Byberg L, Cedernaes J, Hogenkamp PS, Giedratis V, Kilander L et al (2015) Self-reported sleep disturbance is associated with Alzheimer’s disease risk in men. Alzheimers Dement 11:1090–7
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Fortier-Brochu E, Beaulieu-Bonneau S, Ivers H, Morin CM (2012) Insomnia and daytime cognitive performance: a meta-analysis. Sleep Med Rev 16:83–94
Wardle-Pinkston S, Slavish DC, Taylor DJ (2019) Insomnia and cognitive performance: a systematic review and meta-analysis. Sleep Med Rev 48:101205
Borenstein M, Hedges L, Higgins JPT, Rothstein HR (2009) Introduction to meta-analysis. John Wiley and Sons, Ltd, West Sussex
Hoyt WT, Del Re AC (2018) Effect size calculation in meta-analyses of psychotherapy outcome research. Psychother Res 28:379–388
Fernandez-Mendoza J, He F, Puzino K, Amatrudo G, Calhoun S, Liao D et al (2021) Insomnia with objective short sleep duration is associated with cognitive impairment: a first look at cardiometabolic contributors to brain health. Sleep 44:zsaa150
Fernandez-Mendoza J, Calhoun S, Bixler EO, Pejovic S, Karataraki M, Liao D et al (2010) Insomnia with objective short sleep duration is associated with deficits in neuropsychological performance: a general population study. Sleep 33:459–65
Fan TT, Chen WH, Shi L, Lin X, Tabarak S, Chen SJ et al (2019) Objective sleep duration is associated with cognitive deficits in primary insomnia: BDNF may play a role. Sleep 42:zsy192
Khassawneh BY, Bathgate CJ, Tsai SC, Edinger JD (2018) Neurocognitive performance in insomnia disorder: the impact of hyperarousal and short sleep duration. J Sleep Res 27:e12747
Miller CB, Bartlett DJ, Mullins AE, Dodds KL, Gordon CJ, Kyle SD et al (2016) Clusters of insomnia disorder: an exploratory cluster analysis of objective sleep parameters reveals differences in neurocognitive functioning, quantitative EEG, and heart rate variability. Sleep 39:1993–2004
Wadsworth EJ, Simpson SA, Moss SC, Smith AP (2003) The Bristol Stress and Health Study: accidents, minor injuries and cognitive failures at work. Occup Med (Lond) 53:392–7
Claesson L, Linden T, Skoog I, Blomstrand C (2005) Cognitive impairment after stroke - impact on activities of daily living and costs of care for elderly people. The Goteborg 70+ Stroke Study. Cerebrovasc Dis 19:102–9
Aasvik J, Stiles TC, Woodhouse A, Borchgrevink P, Inge Landro N (2018) The effect of insomnia on neuropsychological functioning in patients with comorbid symptoms of pain, fatigue, and mood disorders. Arch Clin Neuropsychol 33:14–23
Xu W, Tan CC, Zou JJ, Cao XP, Tan L (2020) Sleep problems and risk of all-cause cognitive decline or dementia: an updated systematic review and meta-analysis. J Neurol Neurosurg Psychiatry 91:236–244
Edinger JD, Means MK, Krystal AD (2013) Does physiological hyperarousal enhance error rates among insomnia sufferers? Sleep 36:1179–86
Biddle DJ, Naismith SL, Griffiths KM, Christensen H, Hickie IB, Glozier NS (2017) Associations of objective and subjective sleep disturbance with cognitive function in older men with comorbid depression and insomnia. Sleep Health 3:178–183
Wang Y, Yang X, Xiao L, Li W, Huo X, Wang C et al (2022) Altered anterior insula-superior frontal gyrus functional connectivity is correlated with cognitive impairment following total sleep deprivation. Biochem Biophys Res Commun 624:47–52
Satterfield BC, Stucky B, Landolt HP, Van Dongen HPA (2019) Unraveling the genetic underpinnings of sleep deprivation-induced impairments in human cognition. Prog Brain Res 246:127–158
Yoo SS, Hu PT, Gujar N, Jolesz FA, Walker MP (2007) A deficit in the ability to form new human memories without sleep. Nat Neurosci 10:385–92
Miller CB, Rae CD, Green MA, Yee BJ, Gordon CJ, D’Rozario AL et al (2017) An objective short sleep insomnia disorder subtype is associated with reduced brain metabolite concentrations in vivo: a preliminary magnetic resonance spectroscopy assessment. Sleep 40:zsx148
Spiegelhalder K, Regen W, Nissen C, Feige B, Baglioni C, Riemann D et al (2016) Magnetic resonance spectroscopy in patients with insomnia: a repeated measurement study. PLoS One 11:e0156771
Regen W, Kyle SD, Nissen C, Feige B, Baglioni C, Hennig J et al (2016) Objective sleep disturbances are associated with greater waking resting-state connectivity between the retrosplenial cortex/ hippocampus and various nodes of the default mode network. J Psychiatry Neurosci 41:295–303
Funding
This work was supported by the Sichuan Science and Technology Program (2021JDRC0038).
Author information
Authors and Affiliations
Contributions
Study conception and design: BJ and DR; acquisition of data: DR and ZG; analysis and interpretation of the data and writing of this paper: BJ, DR, and ZG. All of the authors approved the submission of the final version of this paper.
Corresponding author
Ethics declarations
Ethical approval
None.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ren, D., Jiang, B. & Guo, Z. Insomnia disorder with objective short sleep duration (ISS) phenotype and cognitive performance: a systematic review and meta-analysis. Neurol Sci 44, 2363–2368 (2023). https://doi.org/10.1007/s10072-023-06692-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-06692-1