Abstract
Background
Cognitive impairment was a common sequela among stroke survivors, and exercise intervention was a promising non-pharmacological treatment modality for it.
Purpose
To explore the effects of exercise intervention programs on cognitive and motor function in patients with cognitive impairment after stroke.
Study design
Systematic review and meta-analysis.
Methods
Seven online databases (PubMed, Embase, Cochrane Library, Web of Science, Scopus, PsycInfo, and SPORTDiscus) were searched from their inception to 10 February 2022. Randomised controlled trials (RCTs) comparing the effects of exercise with non-exercise rehabilitation, using the Montreal Cognitive Assessment, Addenbrooke’s Cognitive Examination, Mini-Mental State Examination, Trial Making Test, Upper and Lower Extremity Fugl-Meyer Assessment, Berg Balance Scale, and Barthel Index, were selected. Calculations for each assessment were performed for the overall effect and the therapy of interest, taking into account the effect of stroke severity or stimulus parameters.
Results
Twelve RCTs involving 975 participants and investigating nine different types of exercise interventions were included. The results were not affected by participant characteristics or reactive balance outcomes. Our results emphasise the importance of lightweight and operable aerobic exercises. Exercise itself had a high potential to improve cognitive impairment and motor function after stroke.
Conclusions
Exercise had significant positive effects on alleviating cognitive and motor impairments after stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Post-stroke cognitive impairment (PSCI) refers to different types and degrees of cognitive impairment caused by acute cerebrovascular disease [1] and emphasises cognitive impairment that occurs or worsens after stroke events [2]. PSCI is one of the most common complications of stroke. More than 20% of patients with stroke develop cognitive impairment within the first 3 months after stroke onset [3]; of these, approximately 1/3 will develop dementia within 5 years [4]. Because cognitive impairment interferes with patients’ perception and adaptability to the external environment, patients are prone to life maladjustment, social adaptability disorders, and emotional disorders, such as anxiety and depression. At the same time, the risk of falls increases, which could induce secondary stroke and even threaten life. Cognitive impairment seriously restricts the overall rehabilitation process in patients with stroke. Therefore, early intervention is particularly important in patients with PSCI. The European Stroke Organisation and European Academy of Neurology joint guidelines on PSCI [5] pointed out that hypertension treatment was an important aspect of PSCI prevention and that controlling hyperlipidaemia might be beneficial to PSCI prevention. Exercise is a very effective treatment for both hypertension and hyperlipidaemia.
However, because the long-term efficacy of drug intervention is not clear and may produce adverse reactions, an increasing number of researchers have tended to use aerobic exercise, cognitive, and dietary interventions [6]. However, the optimal clinical prevention and treatment plan for PSCI remains controversial. PSCI-related content has rarely been mentioned in national and international stroke treatment guidelines. With the development of a large number of large-scale cohort studies and other studies, the correlation between clinical and evidence gradually changed, which would help to better understand and manage [7]. Although many studies have used exercise to improve PSCI, relatively unified opinions are lacking, and few meta-analyses have been conducted on the impact of exercise in patients with PSCI.
In this meta-analysis, the efficacy of different types of exercise interventions on cognitive function was compared with the results of previous RCTs to determine the best exercise therapy that will protect cognitive function in PSCI. The European Stroke Organisation and European Academy of Neurology joint guidelines on PSCI [5] suggest that studies related to PSCI should consider the similarities and differences between post-stroke dementia and other dementia subtypes or brain injuries. In this study, the health and living conditions of patients were regarded as two parts of interaction, and the impact of exercise on cognitive and motor functions and quality of life of patients with PSCI was analyzed comprehensively and innovatively..
Method
The protocol was prospectively registered in the PROSPERO database (CRD42022315163) and conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension statement for meta-analyses [8].
Search strategy
An information specialist developed the search strategy and searched seven electronic databases: PubMed, Embase, Cochrane Central Register of Controlled Trials (CENTRAL), Web of Science, Scopus, PsycINFO (EBSCO), and SPORTDiscus with Full Text (EBSCO), from the inception date to 10 February 2022. In addition, one trial registry, ClinicalTrials.Gov, was searched from its inception date to February 2022 to identify registered trials and relevant reports. No restrictions were applied on the date, language, or publication status.
A combination of the following keywords was employed for the database search: “Stroke*” OR “Apoplexy” OR “cerebrovascular accident” OR “brain vascular accident” AND “Cognitive Dysfunction*” OR “Cognitive Impairment” OR “neurocognitive disorder” OR “cognitive decline” AND “Exercise*” OR “physical activit*” OR “isometric*” OR “aerobic*” AND “randomized controlled trial” OR “randomized” OR “placebo”.
Considering the various sport types, the researchers conducted additional searches in the seven databases according to the specific classification of sports. The interventions searched were as follows: “Stretch*” OR “Strengthen*” OR “walk*” OR “jog*” OR “run*” OR “cycl*” OR “pilates” OR “yoga” OR “tai chi” OR “ai chi” OR “swim*” OR “dance”. Although a larger dataset would offer further insight, no other relevant literature could be included.
Eligibility criteria
Studies were included if they met the following criteria: (1) adults (> 18 years) diagnosed with cognitive impairment after stroke were enrolled; (2) the treatment group received an exercise intervention, defined by the American College of Sports Medicine as any activity using large muscle groups maintained continuously and typically performed for extended periods on devices or ergometers (American College of Sports Medicine 2009) including progressive resistance programmes, and a detailed description of the exercise intervention, including intensity, duration, and frequency, was provided; (3) the control group was given routine non-drug intervention, including balanced diet, health education, routine rehabilitation training, etc.; (4) cognitive function and motor function were included as one of the outcome measures (primary or secondary); and (5) randomised controlled trials.
The exclusion criteria were as follows: (1) studies that focussed on patients with Parkinson’s or Huntington’s disease, epilepsy, multiple sclerosis, diabetes, cognitive impairment, or mental illness such as schizophrenia (in addition to being directly related to cognitive dysfunction disease, these diseases are often associated with different pathological changes and may interfere with the effects of exercise on cognitive function) and (2) studies that examined the effects of acute exercise. If multiple articles were from the same study and reported the same or overlapping results, only the most recently published articles were included.
Study selection
The search results were managed using Endnote software. After exporting the references and removing duplicates and/or language other than English, one author screened the titles and abstracts of all identified references. A second reviewer independently screened the titles and abstracts identified from the primary source of RCTs (CENTRAL), comprising more than half of the search results. The main screener missed none of the studies eventually included in the review, indicating a low likelihood that trials were missed in other sources. The full texts of all potentially relevant trials were subsequently retrieved and reviewed to confirm the final eligible trials. Any disagreements were resolved via consensus, and when any disagreement was elusive, a third reviewer acted as an arbiter.
Data extraction
Data were extracted independently by two researchers, using a self-designed statistical form based on the Cochrane handbook [9]. The form included study characteristics (first author’s name, publication year, title, study design, and setting), participant characteristics (type of cognitive impairment, sample size, average age, and sex ratio), interventions (type, frequency, intensity, duration per session, length of intervention, and comparator information), and outcomes (relevant statistics at the endpoint of the intervention for estimating effect sizes, such as mean, standard deviation, and outcome indicators). Where relevant statistics were incompletely reported, the mean and standard deviation based on the sample size, median, range, and p-value were estimated according to the Cochrane handbook [9].
During data extraction, the Chinese guidelines [10] for the diagnosis and treatment of dementia and cognitive impairment were referred to for the classification of cognitive function, and the Physical Activity Guidelines for Americans [11] and previous systematic reviews were referred to for the classification of exercise interventions [12].
Risk-of-bias assessment
Risk of bias was assessed by two authors using the Cochrane Collaboration’s risk-of-bias tool [9]. Considering the characteristics of exercise intervention, it was impossible to blind participants in the included studies. Thus, only six categories of risk of bias were assessed: random sequence generation, allocation concealment, outcome assessor blinding, incomplete data, selective reporting, and other sources of bias. Disagreements were resolved by the corresponding authors.
Data synthesis and analyses
The data were analysed using RevMan 5.4.1. Continuous data were analysed using mean differences (MD). First, the chi-square test was used to determine whether there was heterogeneity among the studies. If P > 0.1 and I2 < 50%, heterogeneity was considered to be absent among the studies, and the fixed effects model was used for analysis; if P < 0.1 and I2 ≥ 50%, heterogeneity was considered to be high among the studies, and the random effects model was used for analysis. There were five different scales for the outcome indicators of cognitive function, and exercise intervention types could be roughly divided into aerobic and anaerobic. Therefore, subgroup analysis was used to determine the impact of exercise on cognitive function from different perspectives.
Results
Study selection
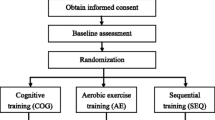
A total of 506 records were retrieved from electronic databases, and seven additional records were obtained from other sources; of these, 413 studies remained after removing duplicates and screening titles and abstracts. Following elimination due to duplication and/or language other than English, single-case reports, irrelevant titles or abstracts, and expert opinions, 97 studies were fully screened. Finally, 12 eligible trials published between 2005 and 2022 were included, with sample sizes ranging from seven to 595. The studies were classified according to seven different indicator types: the cognitive tests were performed in Montreal Cognitive Assessment (MoCA) (n = 4), Addenbrooke’s Cognitive Examination (ACE) (n = 2), Trial Making Test (TMT) (n = 4), and Mini-Mental State Examination (MMSE) (n = 1); motor function was estimated in Fugl-Meyer Assessment (FMA) (n = 2); balance function was supervised in Berg Balance Scale (BBS) (n = 5); and Barthel Index used for assessment of activities of daily living (n = 2). The pooled sample size was 971.
The MoCA is mainly used to assess mild cognitive disorders and has a reliability of 0.736 Cronbach’s alpha in patients with stroke with cognitive impairment. The TMT test requires maintaining two types of parallel thinking abilities: alteration of cognitive function such as set shifting ability and backward inhibition. The ACE test has high sensitivity in screening mild cognitive impairment and dementia.
There was excellent reviewer agreement regarding study selection. The absolute inter-rater agreement for the screening procedures was 96%. The identification process is illustrated in Fig. 1.
Risk of bias
A summary of the risk of bias assessment across all the included studies is presented in Fig. 2. The percentages of studies with low, unclear, and high risks of bias for the individual items were as follows: random sequence generation (75.0%, 25.0%, and 0%, respectively); allocation concealment (58.3%, 33.3%, and 8.3%, respectively); blinding of participants and personnel (41.7%, 50.0%, and 8.3%, respectively); blinding of outcome assessors (66.6%, 33.3%, and 0%, respectively); incomplete outcome (83.3%, 8.3%, and 8.3%, respectively), and selective outcome reporting (66.6%, 33.3%, and 0%, respectively). Detailed information regarding the risk of bias for the included studies is shown in Fig. 3.
Details of the interventions
The main features of the 12 included studies are summarised in Table 1. Among the eligible trials, 10 employed an aerobic intervention programme [13,14,15,16,17,18,19,20,21,22], one focussed on resistance exercise of the more-affected lower limb [23], and one examined the effect of strength (major muscle groups of the upper and lower extremities using elastic bands and body weight), balance, and endurance (using an exercise bicycle) [24].
Of the 10 trials that implemented an aerobic programme, two combined it with patients’ daily routines [20, 22], including out-of-bed activities (without any extra time and equipment) such as sitting, standing, and walking. Two studies used professional physical activity programmes with multiple choices of equipment types [13, 15]. Four studies focussed on one exercise with related facilities, including handgrip and treadmill-based weight loading training [16], walk training on a treadmill with BWS [17], aerobic exercise on a bicycle ergometer [19], and golf training [21]. Two studies conducted the Baduanjin exercise programme [14, 18].
Studies differed in length and number of sessions per week; three studies lasted for 6 months [14, 15, 18], eight lasted between 6 and 119 weeks [13, 16, 17, 19,20,21, 23], and one applied flexible duration according to the practical situation of participants, lasting 14 days or until discharge from the acute stroke unit [22]. Eight studies scheduled their training sessions twice or three times a week [14, 16, 18,19,20,21, 23, 24], one held weekly sessions [15], and three conducted five to seven sessions per week [13, 17, 22].
Table 2 presents the main characteristics of the participants of these studies. In addition to the indicators presented in Table 2, two RCTs considered the education level of patients. Considering that the education level did not have a significant impact on each experiment included in the study, it is not included in Table 2.
Outcomes of meta-analysis
The primary cognitive tests commonly performed in the eligible studies were the MoCA, ACE, and TMT. The secondary outcome indicators were motor function, balance function, and ability of daily living. The evaluation tools used were the FMA and BBS. Activities of daily living (ADL) were assessed using the modified BI, a widely used standard scale for assessing functional disability in basic ADL [25].
Effects of exercise on cognitive function in patients with PSCI
Eight studies evaluated the effects of exercise on cognitive function in patients with PSCI. Four of them reported MoCA scores, two reported ACE scores, and four reported TMT scores. In addition, only one study reported MMSE scores [15], showing that aerobic exercise had a positive influence on cognitive function in patients with PSCI.
Effects of aerobic exercise on MoCA scores
Four studies reported the effect of aerobic exercise on the MoCA scores of patients with PSCI. The intervention duration of one study [14] was significantly longer than that of the other three (24 weeks). Therefore, three studies were included in the meta-analysis. Heterogeneity was observed among the three studies (I2 = 43%, P = 0.62), which was analysed using a random-effects model. The meta-analysis showed that there was no significant difference in cognitive function between the experimental and control groups after exercise training [MD = − 0.39, 95% confidence interval (CI) = − 1.93 to 1.16]. A forest plot representing the effect sizes of the studies included in this meta-analysis is shown in Fig. 4.
Effects of aerobic exercise on ACE scores
Two studies reported the effect of aerobic exercise on the ACE scores of patients with PSCI. There was heterogeneity between the two studies (I2 = 0%, P < 0.01), which was analysed using a random-effects model. The results showed that the ACE score of the exercise group was higher than that of the control group (MD = 3.91, 95% CI = 1.31 to 6.51). A forest plot representing the effect sizes of the studies included in this meta-analysis is shown in Fig. 5.
Effects of exercise on TMT scores
Four RCTs, which used the TMT-A and TMT-B as indicators, were included in the present study. One used resistance exercise as an intervention and showed that the TMT-A and TMT-B scores of the exercise group were higher than those of the control group [23]. The other three focussed on aerobic exercise. Among these three studies, the intervention frequency of one trial [15] was once per week, which was lower than that of the other two. Therefore, two studies were meta-analysed using a randomised effect model. Results showed that there was no significant difference in cognitive function between the experimental and control groups after exercise training (TMT-A: [95% CI = − 80.64 to 62.4), P = 0.001]; TMT-B: [95%CI = − 111.74 to 61.89), P = 0.009]). Figure 6 illustrates the forest plot representing the effect sizes of the studies included in this meta-analysis.
Effects of exercise on motor function of PSCI patients
Two studies reported the effect of aerobic exercise on FMA scores in patients with PSCI. The results showed that the FMA score of the exercise group was higher than that of the control group (MD = 6.39, 95% CI = 1.46 to 11.33). A forest plot representing the effect sizes of the studies included in this meta-analysis is shown in Fig. 7.
Effects of exercise on balance function in patients with PSCI
Five studies reported the effect of exercise on the BBS scores of patients with PSCI. Among these studies, one focussed on resistance exercise, showing that the BBS score of the exercise group was higher than that of the control group [23]. The other four studies focussing on aerobic exercise were analysed using standardised mean difference. There was heterogeneity among the four studies (I2 = 84%, P < 0.01), which was analysed using a random-effects model. After clinical heterogeneity was discussed, it was analysed in subgroups. The intervention was divided into two groups according to the number of weeks of intervention duration: ≤ 12 and > 12 weeks of intervention. The results showed that the BBS score of the exercise group was higher than that of the control group (MD = 7.04, 95% CI = 1.90 to 12.18). Figure 8 illustrates the forest plot representing the effect sizes of the studies included in this meta-analysis.
Effects of exercise on ADL in patients with PSCI
Two studies reported the effects of exercise on ADL using the BI in patients with PSCI. One study applied Baduanjin training as an intervention [14], while the other focussed on strength, balance, and endurance exercise [24]. Both studies concluded that exercise improved the ADL of the participants.
Discussion
Methodological quality of included studies
Among the 12 RCTs included in this analysis, blinding of patients and interveners in post-stroke rehabilitation training was difficult; therefore, the evaluator was single blinded. Nine (75%) of the 12 articles described the specific random method and process, seven (58.3%) reported the method of hiding the allocation scheme, and eight (66.6%) used the result evaluator blind method. Ten (83.3%) articles reported loss of cases and explained the reasons for withdrawal. The loss rate was 0–33.5%. Eight (66.6%) articles used intention analysis. All studies compared the baseline data of patients’ age, sex, pathological grade and stage, treatment plan, and so on. The results showed that the baseline values of patients in the experimental and control groups were comparable (P > 0.05).
Most of the included studies had medium methodological quality. Because the rehabilitation training methods used in most studies were similar, the outcome evaluation indices varied greatly. Even for the same outcome index, the evaluation methods were the same; therefore, meta-analysis could not be performed.
Methods of exercise training
According to a comprehensive literature review, the exercise patterns suitable for patients with PSCI include two categories: low-intensity aerobic exercise and low-intensity impedance exercise in line with the participants’ own ability.
Regardless of the type of the exercise pattern, early initiation was advocated under the guidance of professionals, and safety should be guaranteed to prevent adverse reactions. Exercise training should last between 3 months and 2 years. The following could be strengthened step by step and adjusted in a timely manner according to individual fitness.
In the included studies, few experiments using anaerobic exercise as an intervention measure were performed. By analysing these experiments separately, we found that anaerobic exercise was as effective for PSCI as aerobic exercise. However, the specific duration and frequency of interventions require further analysis in future research.
Exercise improves cognitive function in patients with PSCI
After stroke, due to damage to a brain region or neural network, the overall cognitive function of most patients is in a state of decline [26]. Cognitive impairment is mainly manifested in impaired functions such as attention, memory, language ability, visuospatial ability, and executive ability [27]. A recent study has shown that after intervention with moderate-intensity aerobic exercise, the amplitude of event-related potential in patients with PSCI increased and latency shortened. Moderate-intensity aerobic exercise improves overall cognitive ability and control of attention [28]. The 2019 Canadian Stroke Best Practice Guide [29] recommended that exercise be considered as an adjuvant therapy for cognitive impairment, including attention, memory, and execution. A meta-analysis showed that starting low- to medium-intensity exercise early after stroke could improve patients’ cognitive functions in learning ability, memory, and attention, while improving patients’ balance and coordinating limb movement [30]. The results of this meta-analysis showed that the ACE score of the exercise group was significantly higher than that of the control group (P < 0.05). According to the meta-analysis of the MoCA score, one study [13] did not present positive result. Through the analysis of the specific content, the negative result was achieved irrespective of variability in duration of exercise programmes, which suggests the need for engagement of patients in extra activities during their hospital stay and the longer term in the community. Although the results of this meta-analysis of the TMT score were not completely positive, considering that the intervention duration of the included studies was not long enough, we could separately take the results of these three studies into consideration, which all reported that exercise improved cognitive function in patients with PSCI. It was also consistent with the results of Ravichandran et al. [31].
Exercise has been recognised and confirmed as a clinical method for the treatment of PSCI in many studies. Exercise improves PSCI in several ways. First, exercise reportedly reduces the risk of progression from mild cognitive impairment to dementia [32]. Second, exercise interventions have significant therapeutic advantages in the community. Regular exercise plays an extremely important role in delaying decline in cognitive function and in improving symptoms of chronic diseases. It has the advantages of low cost, high efficiency, simplicity, ease of use, safety, and no adverse reactions and can be well integrated with health education. It has broad application prospects in the field of health management. It is a dynamic and effective way for the elderly to undergo important interventions in the process of continuous health management [32]. From the point of view of biological mechanisms, exercise could improve cognition in patients with mild PSCI by improving cardiorespiratory function, reducing the volume of cerebral atrophy, increasing cerebral blood flow, promoting the establishment of brain neural networks, improving the metabolism of brain tissue, and stimulating the central nervous system [33]. Moreover, exercise also reduces stroke risk factors, such as coronary atherosclerotic heart disease and type 2 diabetes mellitus. The occurrence of common diseases like hypertension may delay its occurrence [34]. The 2017 practice guide of the American Academy of Neurology on mild cognitive impairment indicated that exercise twice a week was beneficial for the recovery of cognitive function in patients with cognitive impairment [35].
However, MMSE and MoCA are cognitive screening scales with low sensitivity to attention and memory. The mechanism of the effect of exercise on attention and memory is still in the research stage. At present, some scholars have put forward their own views to elaborate this problem. Through research, it is found that visuospatial working memory is highly correlated with other cognitive fields, especially attention and executive function. Working memory and attention often involve overlapping frontoparietal brain regions [36]. In general, patients with memory impairment often suffer from subcortical areas (such as hippocampus) outside the prefrontal or medial temporal lobe structures [37, 38]. The study found that, when aerobic exercise is included in the intervention measures, the level of the serum brain-derived neurotrophic factor can be increased to enhance the synaptic plasticity of neurons in the hippocampus, thus avoiding the reduction of the volume of the hippocampus, thus improving the memory function related to the function of the hippocampus, etc. [39], It can also increase cerebral perfusion, improve neurotransmitter conduction function, and increase the thickness of the cortex layer in the frontotemporal area and the volume of hippocampus [40].
Exercise improves motor function and balance ability in patients with PSCI
The FMA score of the exercise group was higher than that of the control group (P < 0.05), proving that exercise improves motor function in patients with PSCI. This might be because the patients had mastered the correct exercise skills again through repeated and regular coordination training during exercise. By inputting the repeated and strengthened normal movement mode into the brain for stimulation, the movement of the motor area of the cerebral cortex was “shaped”, and the limb movements of the patients were coordinated and random to the greatest extent, which promoted recovery of the motor ability of the affected limbs, improved the self-care ability of the patients, and effectively reduced the incidence of disuse and misuse atrophy and deformation of the hemiplegic limbs [35]. The process of exercise intervention focuses on cultivating the brain’s ability to dominate and regulate limbs and muscles, promoting flexibility and coordination in the training process, and improving body function. At the same time, it can adjust the patients’ subjective initiative, establish rehabilitation confidence, and relieve the body and mind to improve muscle tension and the overall coordination ability of the body.
The BBS score of the exercise group was higher than that of the control group (P < 0.05), proving that exercise can improve balance ability in patients with PSCI. A study on the effect of Baduanjin on balance function in patients with PSCI reported that multiple movements in Baduanjin require bending knees and squatting and movements at the centre of gravity, which could increase the weight-bearing capacity of the lower limbs and enhance the strength of muscles in the lower limbs. Each movement was symmetrical (left and right), the joints of the upper and lower limbs were fully extended, and the up, down, left, and right movement of the trunk improved the patient’s ability to control their centre of gravity [41]. In addition, balance training improves proprioception and coordination and sensitivity of the limbs and promotes the recovery of balance function [42]. Aerobic exercises twice a week for 6 months improve balance and physical function in patients with mild cognitive impairment [43]. Aerobic exercise training is related to the moderate improvement of attention and processing speed, executive function, and memory, although the effect of exercise on working memory is not consistent. Strict randomised controlled trials are needed, with larger sample size, appropriate control group, and longer follow-up time [44].
Exercise improves the ability of patients with PSCI to conduct ADL
The results of the meta-analysis showed that the BI score of the exercise group was higher than that of the control group (P < 0.05), proving that exercise could improve the ability of patients with PSCI to conduct ADL. In general, the improvement in motor function and balance ability had a positive relationship with the improvement in the ability of patients with PSCI to conduct ADL, which could further positively influence patients’ cognitive function [45].
Conclusions
Exercise, particularly light and operable aerobic exercise, is generally effective in improving cognitive function in patients’ post-stroke. However, methodological limitations existed in the current clinical trial, such as insufficient sample size, lack of control design and consensus on the best outcome indicators, insufficient treatment dose, deficiency in the consideration of socio-demographic characteristics and the phase of stroke of the participant (in particular, the education level), and absence of long-term follow-up, all of which need to be improved in future research. Further trials with high methodological quality, low-bias risk, and larger sample size are needed to construct a comprehensive literature base, which would facilitate a more thorough exercise rehabilitation for patients with PSCI.
Data availability
The original contributions presented in the study are included in the article/supplementary material, and further enquiries can be directed to the corresponding author.
Change history
21 February 2023
A Correction to this paper has been published: https://doi.org/10.1007/s10072-023-06691-2
References
Bejot Y et al (2011) Prevalence of early dementia after first-ever stroke: a 24-year population-based study. Stroke 42(3):607–612
Mok VCT et al (2017) Early-onset and delayed-onset poststroke dementia — revisiting the mechanisms. Nat Rev Neurol 13(3):148–159
Lo Coco D, Lopez G, Corrao S (2016) Cognitive impairment and stroke in elderly patients. Vasc Health Risk Manag 12:105–16
Pendlebury ST et al (2015) Methodological factors in determining risk of dementia after transient ischemic attack and stroke: (II) effect of attrition on follow-up. Stroke 46(6):1494–1500
Quinn TJ et al (2021) European stroke organisation and European academy of neurology joint guidelines on post-stroke cognitive impairment. Eur J Neurol 28(12):3883–3920
Bechard LE et al (2020) Physical activity perceptions, experiences, and beliefs of older adults with mild cognitive impairment or Alzheimer’s disease and their care partners. Appl Physiol Nutr Metab 45(11):1216–1224
Wardlaw JM et al (2021) Rates, risks and routes to reduce vascular dementia (R4vad), a UK-wide multicentre prospective observational cohort study of cognition after stroke: Protocol. Eur Stroke J 6(1):89–101
Hutton B et al (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 162(11):777–784
Higgins JP, Altman DG, Gotzsche PC et al (2011) Te Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Jia JP, Wang YH, Zhang CD (2011) Chinese guidelines for diagnosis and management of cognitive impairment and dementia (I): dementia diagnostic procedures. Zhonghua Yi Xue Za Zhi 91(9):577–581
Piercy KL et al (2018) The physical activity guidelines for Americans. JAMA 320(19):2020–2028
Zou L et al (2019) The beneficial effects of mind-body exercises for people with mild cognitive impairment: a systematic review with meta-analysis. Arch Phys Med Rehabil 100(8):1556–1573
Khan F et al (2016) An enriched environmental programme during inpatient neuro-rehabilitation: a randomized controlled trial. J Rehabil Med 48(5):417–425
Zheng G et al (2020) Effect of Baduanjin exercise on cognitive function in patients with post-stroke cognitive impairment: a randomized controlled trial. Clin Rehabil 34(8):1028–1039
Ihle-Hansen H et al (2019) A physical activity intervention to prevent cognitive decline after stroke: secondary results from the Life After STroke study, an 18-month randomized controlled trial. J Rehabil Med 51(9):646–651
Kim J, Yim J (2017) Effects of an exercise protocol for improving handgrip strength and walking speed on cognitive function in patients with chronic stroke. Med Sci Monit 23:5402–5409
Nilsson L et al (2001) Walking training of patients with hemiparesis at an early stage after stroke: a comparison of walking training on a treadmill with body weight support and walking training on the ground. Clin Rehabil 15(5):515–527
Ye M et al (2022) Baduanjin exercise ameliorates motor function in patients with post-stroke cognitive impairment: a randomized controlled trial. Complement Ther Clin Pract 46:101506
El-Tamawy MS et al (2014) Aerobic exercises enhance cognitive functions and brain derived neurotrophic factor in ischemic stroke patients. NeuroRehabilitation 34(1):209–213
Moore SA et al (2015) Effects of community exercise therapy on metabolic, brain, physical, and cognitive function following stroke: a randomized controlled pilot trial. Neurorehabil Neural Repair 29(7):623–635
Schachten T, Jansen P (2015) The effects of golf training in patients with stroke: a pilot study. Int Psychogeriatr 27(5):865–873
Cumming TB et al (2018) Early mobilization after stroke is not associated with cognitive outcome findings from AVERT. Stroke 49(9):2147–2154
Fernandez-Gonzalo R et al (2016) Muscle, functional and cognitive adaptations after flywheel resistance training in stroke patients: a pilot randomized controlled trial. J Neuroeng Rehabil 13:37
Studenski S et al (2005) Daily functioning and quality of life in a randomized controlled trial of therapeutic exercise for subacute stroke survivors. Stroke 36(8):1764–1770
Duffy L et al (2013) Reliability (inter-rater agreement) of the Barthel index for assessment of stroke survivors. Stroke 44(2):462–468
Li W et al (2013) Transient focal cerebral ischemia induces long-term cognitive function deficit in an experimental ischemic stroke model. Neurobiol Dis 59:18–25
Pantoni L, Salvadori E (2021) Location of infarcts and post-stroke cognitive impairment. Lancet Neurol 20(6):413–414
Swatridge K et al (2017) The acute effects of aerobic exercise on cognitive control among people with chronic stroke. J Stroke Cerebrovasc Dis 26(12):2742–2748
Lanctôt KL et al (2020) Canadian stroke best practice recommendations: mood, cognition and fatigue following stroke, 6th edition update 2019. Int J Stroke 15(6):668–688
Hasan SM et al (2016) Defining optimal aerobic exercise parameters to affect complex motor and cognitive outcomes after stroke: a systematic review and synthesis. Neural Plast 2016:2961573
Ravichandran H et al (2020) Effects of trunk exercise with physioball to improve trunk balance among subjects with stroke: a systematic review and meta-analysis. J Exerc Rehabil 16(4):313–324
Grande G et al (2014) Physical activity reduces the risk of dementia in mild cognitive impairment subjects: a cohort study. J Alzheimers Dis 39(4):833–839
Szulc-Lerch KU et al (2018) Repairing the brain with physical exercise: cortical thickness and brain volume increases in long-term pediatric brain tumor survivors in response to a structured exercise intervention. Neuroimage Clin 18:972–985
Callisaya M, Nosaka K (2017) Effects of exercise on type 2 diabetes mellitus-related cognitive impairment and dementia. J Alzheimers Dis 59:503–513
Petersen RC et al (2018) Practice guideline update summary: mild cognitive impairment: report of the guideline development, dissemination, and implementation subcommittee of the American Academy of Neurology. Neurology 90(3):126–135
Kiyonaga A et al (2021) Hemisphere-specific parietal contributions to the interplay between working memory and attention. J Cogn Neurosci 33(8):1428–1441
Fischer M, Moscovitch M, Alain C (2021) A systematic review and meta-analysis of memory-guided attention: frontal and parietal activation suggests involvement of fronto-parietal networks. Wiley Interdiscip Rev Cogn Sci 12(1):e1546
Kol A et al (2020) Astrocytes contribute to remote memory formation by modulating hippocampal-cortical communication during learning. Nat Neurosci 23(10):1229–1239
von Bohlen und Halbach O, von Bohlen und Halbach V (2018) BDNF effects on dendritic spine morphology and hippocampal function. Cell Tissue Res 373(3):729–741
Zimmerli L et al (2012) Validation of a mechanism to balance exercise difficulty in robot-assisted upper-extremity rehabilitation after stroke. J Neuroeng Rehabil 9:6
Zou L et al (2018) A review study on the beneficial effects of Baduanjin. J Altern Complement Med 24(4):324–335
Nagamatsu LS et al (2012) Resistance training promotes cognitive and functional brain plasticity in seniors with probable mild cognitive impairment. Arch Intern Med 172(8):666–668
Shiraishi N et al (2017) Effects of a self-exercise program on activities of daily living in patients after acute stroke: a propensity score analysis based on the Japan Association of Rehabilitation Database. Arch Phys Med Rehabil 98(3):434–441
Barha CK et al (2022) Reshaping the path of mild cognitive impairment by refining exercise prescription: a study protocol of a randomized controlled trial to understand the “what,” “for whom,” and “how” of exercise to promote cognitive function. Trials 23(1):766
Richard G et al (2020) Brain age prediction in stroke patients: highly reliable but limited sensitivity to cognitive performance and response to cognitive training. Neuroimage Clin 25:102159
Funding
This work was supported by the budget project of Shanghai University of Traditional Chinese Medicine-Natural Science, Project No. 2021LK014.
Author information
Authors and Affiliations
Contributions
Wenxuan Li: investigation, data curation, formal analysis, and writing of the original draft; Ziyan Luo: investigation, data curation, and formal analysis; Jieting Jiang: formal analysis and data curation; Kunpeng Li: conceptualisation, methodology, data curation, writing, review, and editing; Caiqin Wu: conceptualisation, methodology, data curation, writing, review, editing, and supervision. All the authors agree to be accountable for all aspects of this work.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
There are no human subjects in this article.
Informed consent
Not applicable.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The article was originally published with error. The old version of figures 4, 6 and 8 were used during processing and the level of some headings was not correctly identified.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, W., Luo, Z., Jiang, J. et al. The effects of exercise intervention on cognition and motor function in stroke survivors: a systematic review and meta-analysis. Neurol Sci 44, 1891–1903 (2023). https://doi.org/10.1007/s10072-023-06636-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-06636-9