Abstract
Background
The ratio of triglycerides (TG) to high-density lipoprotein cholesterol (HDL-C) bears a relation with poor outcomes of acute ischemic stroke (AIS), but the impact of serum TG/HDL-C level on post-stroke cognitive impairment (PSCI) remains unknown. We conducted this prospective study to explore the association between TG/HDL-C and PSCI.
Methods
Consecutive AIS patients from the Stroke Units of our hospital were prospectively enrolled between July 1, 2020, and June 30, 2021. Blood samples were collected within 24 h after admission. Cognition function was evaluated by the Montreal Cognitive Assessment (MoCA) at 3 months after stroke. We used logistic regression analyses to explore the relationship between TG/HDL-C and PSCI, and then used a receiver operating characteristic (ROC) analysis to assess the ability of acute TG/HDL-C for predicting PSCI.
Results
A total of 227 AIS patients were recruited. Compared with patients without PSCI, those with PSCI had a higher level of TG/HDL-C at admission (P < 0.01). The multivariate logistic regression analyses showed that TG/HDL-C level was independently associated with PSCI (P < 0.01). The area under the curve of the ROC for TG/HDL-C as predictor of PSCI was 0.701 (95%CI 0.635–0.768). The optimal cutoff value of TG/HDL-C to indicate PSCI was 1.564, which gave a sensitivity of 55.2% and specificity of 80.6%.
Conclusions
Our study demonstrated that a higher level of TG/HDL-C at the acute phase of ischemic stroke predicted the presence of PSCI at 3 months after stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ischemic stroke is a leading cause of death and disability in China [1]. Previous studies and interventions have generally focused on physical disability after stroke, but neglected from consideration post-stroke cognitive impairment (PSCI) [2], which affects about two-thirds of stroke survivors [3]. PSCI not only affects quality of life, but also leads to poorer prognosis and increased mortality in AIS patients [4]. Consequently, there is an important clinical need for neurologists to identify diagnostic biomarkers and related risk factors of PSCI, which might support timely interventions. In recent years, an increasing number of studies have indicated that certain biomarkers of inflammation and oxidative damage might be associated with PSCI [5,6,7]. Besides, plasma lipid levels have also been reported to be associated with ischemic stroke and subsequent cognitive impairment [8,9,10]. However, no clear consensus has yet emerged on these issues.
The TG/HDL-C ratio was first reported to be significantly correlated with insulin resistance [11], and subsequently was widely acknowledged as a major risk factor of cardiovascular events [12]. More recently, a population-based study in Japan has shown that an elevated TG/HDL-C ratio can predict chronic kidney disease [13]. Besides, recent research has found the level of TG/HDL-C to be independently associated with mortality, poor outcome, and hemorrhagic transformation after AIS [14, 15]. However, the possible relationship between TG/HDL-C and PSCI is not well-established.
Therefore, in the current study, we explored the relationship between TG/HDL-C level at admission and PSCI, with an aim to establish a predictive value of TG/HDL-C for PSCI.
Methods
Patients’ recruitment
The present study was approved by the Medical Ethics Committee of the First People’s Hospital of Yancheng and complied with the Declaration of Helsinki. All participants or their relatives provided written informed consent. This study was conducted between July 1, 2020, and June 30, 2021. All the study subjects were recruited from the Stroke Unit of the First People’s Hospital of Yancheng, consecutively. All eligible patients were included in the present analysis.
For inclusion, subjects must meet all following criteria: (1) ≥ 18 years of age, (2) admission within 72 h of onset, (3) first stroke, (4) subjects were willing and able to provide their disease history and informed consents. The exclusion criteria included the following: (1) severe aphasia or dysarthria or hearing impairment that might influence cognitive examination; (2) any history of stroke; (3) Alzheimer’s disease (AD), depression, dementia with Lewy bodies (DLB), frontotemporal dementia (FTD), or dementia caused by other diseases such as malignant tumors, intracranial infection, neurodegenerative diseases, and craniocerebral trauma; (4) history of mental diseases or behavior disorders; and (5) use of nootropics, antipsychotic, antilipemic drugs within 3 months.
Clinical and laboratory assessments
The baseline characteristics collected on admission included demographic data (gender, age, body mass index (BMI), years of education), past medical history (hypertension, diabetes mellitus, heart diseases, atrial fibrillation, smoking habit, and alcohol use), clinical assessment (baseline National Institutes of Health Stroke Score (NIHSS), cerebral infarct volume, infarction location, carotid plaque, artery stenosis, Fazekas score, stroke etiology), and blood laboratory data (homocysteine (Hcy), uric acid (UA), glycosylated hemoglobin A1 (HbA1c), total cholesterol (TC), triglyceride (TG), low-density lipoprotein (LDL), high-density lipoprotein (HDL)). MRI was performed on patients within 72 h after admission. An infarction impinging upon any part of the cerebral cortex was defined as a cortical infarction. The infarct volume was evaluated using the initial DWI lesion volume and calculated as the sum of the infarction area of every slice multiplied by the slice thickness. The degree of cerebral vascular damage was assessed on MRI by applying the Fazekas score. The Fazekas score is a validated diagnostic tool for assessing the severity of white matter hyper-intensities in periventricular regions and deep white matter, with a possible score from 0 to 6. All patients underwent carotid ultrasound or carotid artery CTA to assess plaque and stenosis. Stroke etiology was categorized according to Trial of Org 10,172 in Acute Stroke Treatment (TOAST) criteria.
Blood samples were collected after at least 8 h of fasting within 24 h of hospital admission and the plasma was separated and frozen at − 80 °C before being assayed. A laboratory technician blinded to all clinical data processed all the samples. The levels of serum lipids including TG, TC, HDL-C, and LDL-C were measured in the clinical laboratory of the hospital with an automated biochemical analyzer. The levels of Hcy, UA, and HbA1c were also analyzed and recorded by staff who were blinded to the clinical data of the patients.
Definition of PSCI
The cognitive dysfunction was assessed by trained neurologists at 3 months after stroke onset through the Chinese version of the Montreal Cognitive Assessment (MoCA). MoCA is a well-known questionnaire to assess the severity of cognitive impairment. PSCI was defined by a MoCA score < 26. We add one point to scores of those with education less than 12 years [16, 17].
Statistical analysis
Statistical analyses were performed by SPSS version 23.0 (IBM SPSS Inc.). Continuous variables, which followed normal or skewed distributions, were respectively presented as the mean ± standard deviation or the median (25% and 75% interquartile). Categorical variables were presented as frequency (percentages). Differences in baseline characteristics among TG/HDL-C quartiles were conducted using analysis of variance or the Kruskal–Wallis test for continuous variables, and chi-square test for categorical variables. Differences in baseline characteristics among PSCI and non-PSCI groups were conducted using analysis of one-way ANOVA or the Mann–Whitney test for continuous variables, and chi-square test for categorical variables. Univariable logistic regression analysis was applied to screen risk factors. All variables with a significant relationship at P < 0.15 in univariate analysis entered multivariable analysis. Multivariate logistic regression analysis was then applied to evaluate the independent impact of TG/HDL-C on the occurrence of PSCI, and the corresponding odds ratios (ORs) and 95%CIs were calculated. Furthermore, we conducted receiver operating characteristic (ROC) analysis to evaluate the predictive ability of TG/HDL-C to PSCI, and then calculated the area under the curve (AUC) of the ROC and best cutoff point. A value of P < 0.05 was considered to be statistically significant.
Results
Baseline characteristics among TG/HDL-C quartiles
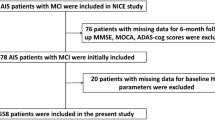
In this study, a total of 452 consecutively admitted patients with AIS were screened. A total of 177 AIS patients were excluded for various reasons, including aphasia (24, 13.6%). Among the 275 patients who met entry criteria, 48 patients had dropped out of the study during follow-up. Ultimately, 227 patients were included in our study (Fig. 1).
The range of TG/HDL-C in all participants was 0.33–8.37. The 227 patients included were stratified into three groups according to TG/HDL-C ratio quartile. The cutoff values of the TG/HDL-C quartiles were ≤ 1.07, 1.07–1.70, and ≥ 1.70. Comparisons of baseline characteristics among the three groups are shown in Table 1. Among the three groups, BMI (P = 0.014), Hcy level (P = 0.03), proportion of PSCI (P < 0.01), HbA1c level (P = 0.029), TG level (P < 0.01), HDL-C level (P < 0.01), LDL-C level (P = 0.02), and MoCA score (P = 0.001) showed significant differences, while other variables did not show any difference.
Characteristics between PSCI group and non-PSCI group
Of the 227 patients in the study, 134 (59.0%) were diagnosed with PSCI 3 months after stroke. Compared with patients without PSCI, patients with PSCI had greater age (P = 0.003), higher education level (P < 0.001), higher levels of TG (P < 0.001) and TG/HDL (P < 0.001), higher NIHSS score (P < 0.001), higher proportion of cortical infarct (P = 0.006), larger infarct volume (P < 0.001), and lower level of HDL (P = 0.001). However, no significant differences were found in gender, BMI, and other vascular risk factors (Table 2).
Risk factors associated with PSCI
The results of logistic regression analyses for the risk factors associated with PSCI are shown in Table 3. The univariate logistic regression analyses presented that age, education level, NIHSS scores, infarct volume, cortical infarction, stroke etiology, TG, HDL-C, and TG/HDL-C were all associated with PSCI (P < 0.05). All variables with a significant relationship at P < 0.15 in univariate analysis were entered into multivariate regression analysis, which showed that age (OR = 1.032, 95%CI = 1.003–1.062, P = 0.028), education level (OR = 0.151, 95%CI = 0.061–0.374, P < 0.001), cortical infarction (OR = 2.243, 95%CI = 1.086–4.633, P = 0.029), baseline NIHSS (OR = 1.312, 95%CI = 1.184–1.454, P < 0.001), and TG/HDL (OR = 3.940, 95%CI = 2.337–6.664, P < 0.001) were independently associated with PSCI.
ROC analysis to explore the predictive ability of TG/HDL-C to PSCI
ROC analysis was further conducted to explore the ability of TG/HDL-C to predict the subsequent development of PSCI. The results showed that the corresponding area under the curve (AUC) to indicate PSCI was 0.701 (95%CI = 0.635–0.768). The optimal cutoff value of TG/HDL-C for the diagnosis of PSCI was 1.564 with a sensitivity of 55.2% and a specificity of 80.6% (Fig. 2).
Discussion
We conducted this prospective study to explore the relationship between TG/HDL-C upon admission of AIS patients and PSCI at 3 months later. Results from the current study showed that patients in the third TG/HDL-C tertile had lower MoCA score (P = 0.001) and higher proportion of PSCI (P < 0.001) than those in the first and second tertiles. Further analysis indicated that higher TG/HDL-C was independently associated with increased risk of PSCI (OR = 3.940, 95%CI = 2.337–6.664, P < 0.001). The optimal cutoff value of TG/HDL-C to predict the appearance of PSCI was 1.564, and its corresponding sensitivity and specificity were 55.2% and 80.6%, respectively. Our results revealed that TG/HDL-C was an effective indicator of PSCI.
Our study showed that the prevalence of PSCI was 59.0% in our study group, which is in line with the previous research [18]. Similar to the results of previous reports [18,19,20,21,22], we also found that certain indicators like age, NIHSS score, education level, cerebral infarct volume, and proportion of cortical infarction differed significantly between the PSCI and non-PSCI groups. Meanwhile, patients in the PSCI group had lower TG and higher HDL-C and TG/HDL-C. Further analysis showed that age, education level, baseline NIHSS, cortical infarction, and TG/HDL were independently associated with PSCI.
Previous studies have found that dyslipidemia might be a risk factor of ischemic stroke and cognitive impairment or AD [19,20,21]. However, the prognostic significance of serum lipid levels remains conflicted, which may result from the clinically heterogeneous features of ischemic stroke. Several studies have reported that lower HDL-C or elevated TG could increase the risk of cognitive impairment in later life [21]. High serum TC and LDL-C have also been reported to be risk factors of cognitive impairment in elderly subjects respectively [10, 18, 22]. However, some other studies found conflicting results [23, 24].
Meanwhile, the close association of apolipoprotein E (ApoE) and cognitive impairment has been explicitly established. ApoE is a multifunctional protein that plays a crucial role in the transport of lipid and the mediation of dynamic lipid levels and lipid metabolism [25]. ApoE can not only directly modulate Aβ metabolism, but also affect cognitive function through Aβ-independent pathways by regulating neuronal function, lipid metabolism, or other related pathways [25, 26]. The APOE gene has been reported to be an important genetic risk factor for AD [26, 27]. Indeed, Farrer et al. [28] had reported that individuals who carry one ɛ4 allele bear a 2–fourfold higher AD risk, and those with two copies of ɛ4 have an 8–12-fold increased AD risk.
Elevated TG/HDL-C is acknowledged as a marker of insulin resistance and an independent predictor of cardiovascular risk [15, 29]. On the other hand, recent research found that lower levels of TG/HDL-C were associated with greater risk of hemorrhagic transformation and worse short-term outcomes after AIS [14, 15]. Nevertheless, that finding was limited to patients with large artery atherosclerosis stroke and the potential relationship between TG/HDL-C and PSCI was not explored. To our knowledge, the present study is the first research study to prospectively explore the possible correlation between TG/HDL-C and PSCI in AIS patients. We find that higher levels of TG/HDL-C at admission could increase the risk of PSCI. Therefore, TG/HDL-C ratio in the acute phase of ischemic stroke can be used as an indicator to predict the later occurrence of PSCI, which might guide the selection of timely rehabilitative interventions such as cognitive training, or efforts to rectify hyperlipidemia. The underlying mechanisms on the observed relationship between TG/HDL-C and PSCI remain unclear, but several potential pathways have been proposed. Previous research has reported that hypercholesterolemia might increase the production and deposition of amyloid beta peptides (Aβ) in the brain and promote the formation of neurotoxic fibrils and neuritis [10, 30, 31]. Some investigators have reported that HDL-C could prevent aggregation of Aβ and inflammation caused by neurodegenerative processes [32, 33]. Lower HDL-C levels have been previously reported to be associated with more severe white matter lesion changes, leading to AD and mild cognitive impairment [33]. The TG level has also been reported to be correlated with atherogenic and pro-inflammatory triglyceride-rich lipoproteins that may directly promote cognitive impairment [34]. We hypothesized that high TG concentration and low HDL concentration may contribute to cognitive sequelae, such that the TG/HDL-C ratio could be a sensitive predictor.
Our findings provide epidemiological evidence supporting the proposal that TG/HDL-C is a potential predictor of PSCI. However, some limitations should be pointed out in this study. First, our study was a single-center study, and the sample size was not large enough to support generalization, such that our findings should be further verified by a multi-center study with large samples. Second, several potential risk factors that may be associated with PSCI were not examined, notably among these the ApoE status, hypersensitive C-reactive protein, and 8-hydroxydeoxyguanosine. Third, due to the limited sample size, we did not make a more detailed classification of infarction location, but only considered cortical involvement as a factor. Fourth, we only investigated the baseline level of TG/HDL-C and did not conduct dynamic measures of TG/HDL-C over time after stroke, which may have sacrificed information about treatment effects on cognitive outcome. In addition, according to the strict exclusion criteria, quite a few AIS patients with massive infarction (n = 17) or severe aphasia (n = 24) or dysarthria (n = 11) were excluded, which might have resulted in bias.
Conclusion
This study demonstrated that higher levels of TG/HDL-C at admission in AIS patients could serve as a predictor for PSCI 3 months later. The underlying molecular mechanisms are not clear, which calls for further studies in large populations. Results imply that early intervention against hyperlipidemia might have a preventive effect on the development of PSCI.
Data availability
The data that support the findings of this study are available from Dingming Sun upon reasonable request.
References
Zhou M, Wang H, Zeng X et al (2019) Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 394:1145–1158
Brainin M, Tuomilehto J, Heiss WD et al (2015) Post-stroke cognitive decline: an update and perspectives for clinical research. Eur J Neurol 22(229–238):e13–e16
Pascoe M, Ski CF, Thompson DR et al (2019) Serum cholesterol, body mass index and smoking status do not predict long-term cognitive impairment in elderly stroke patients. J Neurol Sci 406:116476
Nys GM, van Zandvoort MJ, de Kort PL et al (2005) The prognostic value of domain-specific cognitive abilities in acute first-ever stroke. Neurology 64:821–827
Zhang X, Bi X (2020) Post-stroke cognitive impairment: a review focusing on molecular biomarkers. J Mol Neurosci 70:8
Rothenburg LS, Herrmann N, Swardfager W et al (2010) The relationship between inflammatory markers and post stroke cognitive impairment. J Geriatr Psych Neur 23:199–205
Zhu Z, Zhong C, Guo D et al (2019) Multiple biomarkers covering several pathways improve predictive ability for cognitive impairment among ischemic stroke patients with elevated blood pressure. Atherosclerosis 287:30–37
Kivipelto M, Helkala EL, Hanninen T et al (2001) Midlife vascular risk factors and late-life mild cognitive impairment: a population-based study. Neurology 56:1683–1689
Evans RM, Emsley CL, Gao S et al (2000) Serum cholesterol, APOE genotype, and the risk of Alzheimer’s disease: a population-based study of African Americans. Neurology 54:240–242
Ma C, Yin Z, Zhu P et al (2017) Blood cholesterol in late-life and cognitive decline: a longitudinal study of the Chinese elderly. Mol Neurodegener 12:24
Salazar MR, Carbajal HA, Espeche WG et al (2012) Relation among the plasma triglyceride/high-density lipoprotein cholesterol concentration ratio, insulin resistance, and associated cardio-metabolic risk factors in men and women. Am J Cardiol 109:1749–1753
Onat A, Can G, Kaya H et al (2010) “Atherogenic index of plasma” (log10 triglyceride/high-density lipoprotein-cholesterol) predicts high blood pressure, diabetes, and vascular events. J Clin Lipidol 4:89–98
Tsuruya K, Yoshida H, Nagata M et al (2014) Association of the triglycerides to high-density lipoprotein cholesterol ratio with the risk of chronic kidney disease: analysis in a large Japanese population. Atherosclerosis 233:260–267
Deng Q, Li S, Wang H et al (2018) The short-term prognostic value of the triglyceride-to-high-density lipoprotein cholesterol ratio in acute ischemic stroke. Aging Dis 9:498
Deng QW, Liu YK, Zhang YQ et al (2019) Low triglyceride to high-density lipoprotein cholesterol ratio predicts hemorrhagic transformation in large atherosclerotic infarction of acute ischemic stroke. Aging (Albany NY) 11:1589–1601
Nasreddine ZS, Phillips NA, Bedirian V et al (2005) The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53:695–699
Lees R, Selvarajah J, Fenton C et al (2014) Test accuracy of cognitive screening tests for diagnosis of dementia and multidomain cognitive impairment in stroke. Stroke 45:3008–3018
Chen H, Du Y, Liu S et al (2019) Association between serum cholesterol levels and Alzheimer’s disease in China: a case-control study. Int J Food Sci Nutr 70:405–411
He Q, Li Q, Zhao J et al (2016) Relationship between plasma lipids and mild cognitive impairment in the elderly Chinese: a case-control study. Lipids Health Dis 15:146–153
Pokharel Y, Mouhanna F, Nambi V et al (2019) ApoB, small-dense LDL-C, Lp(a), LpPLA2 activity, and cognitive change. Neurology 92:e2580–e2593
Svensson T, Sawada N, Mimura M et al (2019) The association between midlife serum high-density lipoprotein and mild cognitive impairment and dementia after 19 years of follow-up. Transl Psychiat 9:26–32
Zhao B, Shang S, Li P et al (2019) The gender- and age- dependent relationships between serum lipids and cognitive impairment: a cross-sectional study in a rural area of Xi’an, China. Lipids Health Dis 18:4–14
Dupuy AM, Mas E, Ritchie K et al (2001) The relationship between apolipoprotein E4 and lipid metabolism is impaired in Alzheimer’s disease. Gerontology 47:213–218
Mielke MM, Montine T, Khachaturian AS (2012) Vascular diseases: one pathway toward new conceptual models of dementia. Alzheimers Dement 8:S69–S70
Hauser PS, Narayanaswami V, Ryan RO (2011) Apolipoprotein E: from lipid transport to neurobiology. Prog Lipid Res 50:62–74
Xu H, Finkelstein DI, Adlard PA (2014) Interactions of metals and apolipoprotein E in Alzheimer’s disease. Front Aging Neurosci 6:121
Marais AD (2021) Apolipoprotein E and atherosclerosis. Curr Atheroscler Rep 23:34
Farrer LA, Cupples LA, Haines JL, Hyman B, Kukull WA, Mayeux R (1997) Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease. A meta-analysis. APOE and Alzheimer Disease Meta Analysis Consortium. JAMA 278:1349–1356
Yatawara C, Guevarra AC, Ng KP et al (2020) The role of cerebral microbleeds in the incidence of post-stroke dementia. J Neurol Sci 412:116736
Kalaria RN (2012) Cerebrovascular disease and mechanisms of cognitive impairment. Stroke 43:2526–2534
Goulay R, Mena Romo L, Hol EM et al (2020) From stroke to dementia: a comprehensive review exposing tight interactions between stroke and amyloid-β formation. Transl Stroke Res 11:601–614
Svensson T, Sawada N, Mimura M et al (2019) The association between midlife serum high-density lipoprotein and mild cognitive impairment and dementia after 19 years of follow-up. Transl Psychiatry 9:26
Ohtani R, Nirengi S, Nakamura M et al (2018) High-density lipoprotein subclasses and mild cognitive impairment: Study of Outcome and aPolipoproteins in Dementia (STOP-Dementia)1. J Alzheimer’s Dis 66:289–296
Talayero BG, Sacks FM (2011) The role of triglycerides in atherosclerosis. Curr Cardiol Rep 13:544–552
Funding
This work was supported by the Science and Technology Bureau of Yancheng (YK2019005).
Author information
Authors and Affiliations
Contributions
DMS, YG, and YQC designed the study. HHZ, YQC, JC, LL, and CXL conducted the research. YQC and HHZ wrote the paper and analyzed the data. All authors reviewed and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethical approval
This study was conducted according to the protocol approved by the Human Subjects Research Ethics Board of The First People’s Hospital of Yancheng.
Informed consent
Written informed consent was obtained from all participants.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cheng, Y., Zhu, H., Chen, J. et al. Serum TG/HDL-C level at the acute phase of ischemic stroke is associated with post-stroke cognitive impairment. Neurol Sci 43, 5977–5984 (2022). https://doi.org/10.1007/s10072-022-06267-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06267-6