Abstract
Objective
We investigated the efficacy of low-dose prednisolone (PSL) regimen in patients with generalized myasthenia gravis (MG) post-thymectomy and its correlation with long-term outcome.
Methods
This is a 2-year observational study. The subjects were aged 16–75 years, a Myasthenia Gravis Foundation of America (MGFA) clinical classification of II to IV, generalized MG after thymectomy. We selected a low-dose (5 mg/day) initiation and slowly incrementing (10 mg every 4 weeks) PSL therapy regimen. We collected the clinical characteristics, treatment-related data, and 2-year clinical outcomes of MG patients, and analyzed the effect of various factors on the achievement of the treatment target.
Results
Sixty-three generalized MG were recruited in our study. After 2 years of observation, 52 patients (82.5%) of generalized MG achieved treatment goal. Based on the maximum daily dose of PSL received, the MG patients were divided into 20 mg, 30 mg, and ≥ 40 mg groups. Subgroup analysis showed that the 20 mg group had the highest rate of achieving the treatment target (94.9%), followed by the 30 mg group (73.3%) and the lowest rate was among the ≥ 40 mg group (44.4%). Using a multivariate logistic regression analysis, we identified that the maximum daily dose of PSL 20 mg was the only positive, independent predictor of treatment goal achievement after 2 years.
Conclusion
Low-dose initiation, slowly incrementing PSL therapy is feasible for generalized MG patients after thymectomy. Early response to low-dose PSL therapy may predict better long-term outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The American Academy of Neurology (AAN) updated the guideline regarding the efficacy of thymectomy for MG treatment in 2020 [1], reporting significant benefits of thymectomy to patients with non-thymomatous acetylcholine receptor antibody (AChR Ab) positive generalized MG. The MGTX randomized trial [2] and the MGTX extension trial [3], which provided high-quality evidence for the guideline, have shown a reduction in the time-weighted average Quantitative Myasthenia Gravis (QMG) scores (score items see Supplemental Table 1) and PSL dose following thymectomy in generalized MG. For conventional MG therapy, oral corticosteroids remain the most common immunosuppressive drug. They are widely used with both dose escalation/de-escalation regimen [4]. Even in the international consensus guidelines, a widely accepted dose regimen for oral corticosteroids has not been proposed [5]. A multicentre cross-sectional study suggests that low-dose PSL treatment may enable achieving treatment targets earlier. It may also help maintain stabilized status better in patients with generalized MG [6].
Therefore, it seems reasonable that a low-dose PSL dosing regimen was selected as a subject of a clinical trial, especially in generalized MG patients following thymectomy. We used a low-dose initial, slowly increasing dose regimen and followed up for 2 years to analyze the long-term outcomes of the new regimen in the management of generalized MG.
Methods
Subjects and data collection
The study was a prospective, non-controlled study and has been approved (2013-研-104) by the Ethics Committee of the 2nd Affiliated Hospital of Harbin Medical University. All written informed consent was sought from all patients, prior to registration. We screened all patients with MG who were treated at the 2nd Affiliated Hospital of Harbin Medical University between January 1, 2013, and December 31, 2018. The diagnosis of MG is based on a typical history and clinical manifestation (fluctuating weakness of skeletal muscles) and any of the following 3 points, including elevated AChR Ab, positive response to cholinesterase inhibitors, and a decremental response of muscle to repetitive motor nerve stimulation.
Eligible MG patients were aged 16–75 years, and a Myasthenia Gravis Foundation of America (MGFA) clinical classification of II to IV [7] (see Supplemental Table 2 for details) has undergone thymectomy, and appropriate anticholinesterase therapy is acceptable, but corticosteroid or other immunosuppressive agents have never been used. Subjects who were pregnant or lactating, did not want to avoid pregnancy within 2 years, had contraindications to corticosteroids, or were accompanied by malignant tumor diseases were excluded from the study.
The following data were collected at baseline: gender, age, age at onset, disease duration, thymic histology, clinical status, MGFA classification, QMG score, AChR Ab status, and pyridostigmine use. The following data were collected at each visit: clinical status, medication requirements, adverse events, MGFA classification, QMG score, and MGFA post-intervention status (PIS) (see Supplemental Table 3 for details). The treatment goal of this study were defined as achieving one of complete stable remission (CSR), pharmacologic remission (PR), or minimal manifestation status (MMS) according to the MGFA-PIS classification, lasting > 12 months without recurrence. Patients were classified as “MMS or better group” or “No MMS group” based on whether treatment goal were achieved at the last follow-up. MMS or better is also the treatment target recommended by the MG international consensus [5].
Low-dose PSL dosing regimen
Upon enrolment (at baseline), patients received oral PSL at an initial dose of 5 mg per day. This was followed by weekly increases of 5 mg per day, until such time that the daily dose reached 20 mg (at 4 weeks). At the end of the fourth week, the patients completed the visit 1 (4 weeks ± 2 days). The standard for further adjustment of PSL dose was based on the MG symptoms, the QMG score [8], the MGFA score, and the achievement of MMS [7] at each visit. When the symptoms of MG improved over baseline/previous visit, the MGFA score was ≤ 2, and the QMG score decreased by at least 3 points compared to baseline; PSL doses remained unchanged. If the aforementioned changes were not observed, a daily dose of PSL was increased by 10 mg upon each visit. Once the patients reached MMS, the PSL dose would not be increased further. For some patients, PSL daily dose was increased to 30 mg upon visit 1 (4 weeks ± 2 days) and to 40 mg upon visit 2 (8 weeks ± 1 week). If subjects did not show improvement in symptoms by visit 3 (12 weeks ± 1 week), PSL doses would be increased to the maximum dose of 50 mg per day (Fig. 1), and be maintained at visit 4 (16 weeks ± 1 week). Figure 1 depicts the incremental PSL dosing regimen in a flowchart. From the 16th week, the follow-up interval was adjusted to 2–3 months. In either case, for patients who achieved and maintained MMS for 6 months or did not achieve MMS at 12 months, the PSL daily dose was reduced by 10 mg per month until it reached 20 mg per day. The subsequent daily dose was reduced by 5 mg every 2 months if MMS was maintained. During the PSL tapering period, if MG patients’ condition worsened, PSL daily dose was increased by 10 mg until the next visit. Concurrent with initial PSL, all subjects have been given azathioprine 2.0 mg/kg per day (or mycophenolate mofetil 1.5–2 g per day if they could not tolerate azathioprine). Upon initiation of PSL tapering, patients could not take more than 120 mg pyridostigmine per day.
Statistical analysis
The time-weighted average PSL dose was calculated by dividing the cumulative doses by the number of days from baseline to the last visit. Student’s T test and one-way analysis of variance (ANOVA) were used to compare continuous data between two or three groups, respectively. Pearson’s χ2 test was used to compare categorical variables between groups. Kaplan–Meier analysis and log-rank test were used to find the differences in time taken, to achieve treatment target among the subgroups. The multivariate logistic regression model was used to identify independent, predictive factors for achieving treatment goal 2 years after treatment initiation. Factors in the model included age; QMG score; age at onset (early onset and late onset); thymic histology (non-thymoma and thymoma); and the maximum daily dose of PSL (20 mg, 30 mg, and ≥ 40 mg). A P-value < 0.05 was considered to indicate statistical significance. Statistical analysis was performed using SPSS version 22.0 software.
Results
Demographic and baseline details
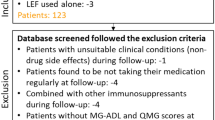
From January 1, 2013, to December 31, 2018, a total of 193 patients underwent screening. Of which 112 did not meet the inclusion criteria and were excluded from the study (see Supplemental Fig. 1 for details). Of the 81 patients eligible for inclusion, 7 patients who had significant improvement post-thymectomy did not consent to PSL treatment and withdrew from the trial. The remaining 74 patients with generalized MG participated in this study between January 2013 and December 2020. Finally, 63 patients completed 24 months of follow-up (7 lost to follow-up, 1 withdrew consent, 1 died 2 weeks after surgery, 1 withdrew due to necrosis of the femoral head, and 1 withdrew due to hepatitis B reproduction). Of the 63 patients, 34 were women and 29 were men. The mean age of onset was 44.6 ± 15.7 years, and the mean age at thymectomy was 45.9 ± 15.3 years. The mean duration of disease was 6.7 ± 4.0 years (range: 2.2–24.0 years). With a cutoff age of 50 years for distinguishing. Thirty-five patients (55.6%) were early-onset MG, 28 patients (44.4%) were late-onset MG. Forty-eight patients were tested for AChR Ab status, but these tests were not done in the same clinical trial center. Measuring range upper limit is different in different centers, and some of the AChR Ab titers cannot be accurately quantified because they exceed the upper limit. Therefore, we only qualitatively describe the AChR Ab status in Table 1. Other demographic data and baseline details, including thymic histology, MGFA classification, QMG score, and dose of pyridostigmine are shown in Table 1.
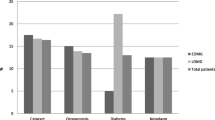
Treatment characteristics with PSL
According to the dosing regimen, MG patients were administrated different doses of PSL for varying durations. The treatment characteristics of subgroups are shown in Table 2. In fact, the maximum daily dose of PSL received by MG patients was divided into four levels: 20 mg, 30 mg, 40 mg, and 50 mg. However, an unexpected result was that more than 60% of patients received the maximum daily dose of PSL of 20 mg, while only a few patients received the maximum daily dose of 40 mg and 50 mg. For subgroup analysis, to avoid statistical bias caused by small sample size, patients in the 40 mg group and 50 mg group were combined. Thus, based on the maximum daily dose of PSL received, MG patients were divided into three groups: 20 mg group, 30 mg group, and ≥ 40 mg group. At month 24, the mean PSL daily dose in the ≥ 40 mg group was 7.8 ± 6.7 mg (0.0–15.0 mg), significantly higher than in the 20 mg (1.5 ± 3.0 mg) or 30 mg groups (3.8 ± 5.1 mg), P < 0.001. From month 0 to month 24, time-weighted mean PSL dose (14.6 ± 1.1 mg in the 20 mg group, 20.2 ± 1.6 mg in the 30 mg group, and 28.4 ± 3.5 mg in the ≥ 40 mg group); cumulative PSL dose (8.3 ± 1.8 g in the 20 mg group, 12.7 ± 1.9 g in the 30 mg group, and 19.1 ± 2.4 g in the ≥ 40 mg group); and PSL withdrawal rate (78.4% in the 20 mg group, 57.1% in the 30 mg group, and 37.5% in the ≥ 40 mg group) were significantly different between any two of the three groups (P < 0.05).
Time-event analysis with treatment target as an outcome event showed that the target achievement rate for all patients was 82.5% at 2 years, and the meantime to achieve treatment target was 17.1 months (95% CI, 16.2 to 18.0 months). Among the subset of patients receiving 20 mg PSL, a significantly higher proportion of patients reached treatment target (94.9%) in the least amount of time (15.9 months, 95% CI, 15.0 to 16.8 months), ≥ 40 mg group fewer proportion of patients reached the target (44.4%) and took the longest time (21.0 months, 95% CI, 18.6 to 23.3 months). The Kaplan–Meier plot with each of the subgroups is presented in Fig. 2.
Independent predictors for clinical outcome
Overall, at a 2-year follow-up, 52 patients (82.5%) had already achieved MMS or better and have lasted for more than 12 months; the meantime to MMS or better was 3.7 ± 2.3 months after the start of PSL therapy. To explore the factors affecting long-term clinical outcomes, demographic data and clinical characteristics at baseline, and treatment characteristics with PSL were taken as independent variables, and clinical outcomes as dependent variables, univariate analysis is used to screen variables. The eligible variables with P < 0.1 in univariate analysis, including baseline MGFA classification, baseline QMG score, thymus histology, and maximum daily dose of PSL, finally entered the multivariate logistic regression model. Analysis showed that the maximum daily dose of PSL 20 mg was the only independent predictor of treatment goal achievement after 2 years of treatment and was a positive predictor. After 2 years, the odds ratio (OR) (95% CI) was 6.727 (1.084 to 41.768, P = 0.041) for 20 mg group versus 30 mg group, and the OR (95% CI) was 23.125 (3.332 to 160.490, P = 0.001) for 20 mg group versus ≥ 40 mg group (Table 3).
Discussion
Although there is no internationally accepted standard of treatment in generalized MG management, the universally accepted view now is that the long-term immunosuppressive therapy should be started [5, 9, 10], usually with a combination of PSL and azathioprine (level A recommendation) [9]. PSL is undoubtedly the first-line immunosuppressive agent for all generalized MG patients [11,12,13,14]. PSL combined with azathioprine is recommended to allow tapering the PSL to the lowest dose possible, while maintaining effect [11, 15, 16]. Results of a recent randomized clinical trial suggest that rapid tapering of PSL is feasible and does not affect long-term outcomes in patients with moderate to severe generalized MG treated with high-dose PSL with azathioprine [17]. In addition, the MGTX study [2] published in 2016 and the recently published MGTX extension study [3] provide evidence that thymectomy can improve clinical outcomes and reduce dependence on PSL in patients with generalized MG. Since both thymectomy and azathioprine can be used as steroid-sparing agents, when the generalized MG patients undergoing thymectomy would start PSL plus azathioprine treatment, we should reconsider the question of “how to use PSL and for how long?” We would certainly like to use PSL less, after all, the side effects of PSL [18] are obvious and well known. The Japanese clinical guidelines (GLs) for MG and some recent studies based on clinical data obtained in the Japan MG Registry study (JAMG-R) recommend that high-dose oral steroids as a treatment strategy in MG should be reconsidered for the high incidence of adverse reactions, reduced quality of life, and deteriorating mental health [6, 10, 19].
In the present study, PSL was given following a lower initial dose and slower escalation schedule in the generalized MG patients who underwent thymectomy. The maximum daily dose of PSL for all MG patients was confirmed within 16 weeks of treatment initiation according to the PSL dosing regimen. The results showed that 85.7% of patients reached their daily PSL dose to the maximum (20 to 30 mg) within 8 weeks of treatment initiation and did not increase their PSL dose for the entire period of follow-up. To exemplify, when the maximum daily dose of PSL was increased to 20–30 mg at week 8 of treatment, 85.7% of patients showed a sustained improvement in clinical features, which was reflected in subjective symptoms (improvement of symptoms), objective evaluation (QMG score is at least 3 points less than baseline), and MGFA classification (MGFA score ≤ 2). The results at 2 years follow-up showed that by the last visit, 82.5% of patients had achieved long-term treatment goal, which were comparable to other recent studies [20, 21] in China; the 20 mg group had the highest realization rate of treatment target and the shortest average time to reach the treatment target, and the ≥ 40 mg group had the lowest target achievement rate and the longest average target reaching time (Fig. 2). At 24 months, the PSL doses were reduced to 1.5 ± 3.0 mg and 3.8 ± 5.1 mg in the 20 mg groups and 30 mg groups, respectively, like the PSL dosing level of 5 mg per day or less, which has been recommended as a treatment target by Japanese experts in their national guideline for MG [10]. At the last follow-up, 78.4% of the patients in the 20 mg group had stopped PSL treatment, which was significantly higher than the other two groups. The time-weighted average was calculated by dividing the cumulative doses by the number of days from baseline to a time point, which can better reflect the average daily PSL dose during this period. In this study, the time-weighted mean PSL dose month 0–24 was 18.0 ± 5.2 mg, which was significantly lower than the doses’ level in the MGTX study [2, 3], and may be related to the slower incremental PSL dosing regimen and the combination of immunosuppressant. The results show that low dosage, slowly incrementing PSL therapy, is feasible for generalized MG patients. The earlier the clinical response to PSL appears in MG patients, the smaller the cumulative dose of PSL is used, and the earlier the treatment goal is achieved.
Multivariate regression analysis confirmed that patients in the 20 mg group had better outcomes at 2 years, and the maximum daily dose of PSL 20 mg was a predictor of achieving treatment goal. This may indicate that generalized MG patients post-thymectomy are more likely to achieve long-term treatment goal if their symptoms begin to improve within 4 weeks by treatment with 20 mg prednisone combine with azathioprine daily. A recently published study suggests a similar view that the treatment response at 6 months could be a predictor of the long-term clinical outcome [21]. Studies by Imai et al. also indicated that the response of MG patients to oral PSL was not associated with baseline disease severity, and patients who do not respond well to PSL need higher doses and longer periods of corticosteroid treatment [22]. Cumulative PSL dose was an independent negative predictor of prognosis at 1 year after treatment initiation [22].
In univariate analysis, MGFA classification, baseline QMG score, and thymic histology were also candidate predictors, but these confounders were excluded after multivariate analysis. Whether thymomatous patients had worse outcomes has long been controversial. Some authors agreed with us [23,24,25,26], and the others supported thymomatous pathology as a prognostic factor [27,28,29,30,31]. Overall, the low-dose PSL treatment was feasible in generalized MG over 2 years of follow-up. PSL daily dose ≤ 10 mg within 14 days of initial treatment reduced the likelihood of steroid-induced initial worsening in MG [32]. Within 8 weeks, the maximum daily dose of PSL was increased up to 20–30 mg improved symptoms in most MG patients (85.7%). From month 0 to month 24, the time-weighted mean PSL dose was lower than expected, which helped to reduce the adverse effect caused by corticosteroid exposure [33, 34]. The complete follow-up data showed an overall favorable prognosis, with 82.5% of the patients achieving treatment goal and 63.5% of the patients withdrew PSL, suggesting that with the PSL dosing regimen, “less is not necessarily more.”
At present, there is no clear and internationally recognized guideline for PSL therapy in MG patient [1,2,3,4,5]. In our study, although the overall prognosis for the majority of patients was good, 10–15% of patients did not achieve the treatment goal, especially those who received a high dose of PSL due to poor response in the early stage of treatment. Therefore, early identification of refractory patients and offering them an optimal treatment regimen needs to be addressed.
The limitation of the present study is that it is a non-control design at a single center. Not all patients were tested for AChR Ab, and so we could not properly analyze the correlation between AChR Ab status and long-term outcome. In addition, the time of longitudinal follow-up was relatively short. Toward a more complete understanding of the disease course to MG, we should continue to follow up these patients in the future.
Abbreviations
- AChR Ab:
-
Acetylcholine receptor antibody
- AAN:
-
American Academy Neurology
- CSR:
-
Complete stable remission
- MMS:
-
Minimal manifestation status
- MG:
-
Myasthenia gravis
- MGFA:
-
Myasthenia Gravis Foundation of America
- PR:
-
Pharmacologic remission
- PIS:
-
Post-intervention status
- PSL:
-
Prednisolone
- QMG:
-
Quantitative myasthenia gravis
References
Gronseth GS, Barohn R, Narayanaswami P (2020) Practice advisory: thymectomy for myasthenia gravis (practice parameter update): report of the guideline development, dissemination, and implementation subcommittee of the American Academy of Neurology. Neurology 94:705–709. https://doi.org/10.1212/WNL.0000000000009294
Wolfe GI, Kaminski HJ, Aban IB et al (2016) Randomized trial of thymectomy in myasthenia gravis. N Engl J Med 375:511–522. https://doi.org/10.1056/NEJMoa1602489
Wolfe GI, Kaminski HJ, Aban IB et al (2019) Long-term effect of thymectomy plus prednisone versus prednisone alone in patients with non-thymomatous myasthenia gravis: 2-year extension of the MGTX randomised trial. Lancet Neurol 18:259–268. https://doi.org/10.1016/S1474-4422(18)30392-2
Meriggioli MN, Sanders DB (2009) Autoimmune myasthenia gravis: emerging clinical and biological heterogeneity. Lancet Neurol 8:475–490. https://doi.org/10.1016/S1474-4422(09)70063-8
Sanders DB, Wolfe GI, Benatar M et al (2016) International consensus guidance for management of myasthenia gravis: executive summary. Neurology 87:419–425. https://doi.org/10.1212/WNL.0000000000002790
Imai T, Utsugisawa K, Murai H et al (2018) Oral corticosteroid dosing regimen and long-term prognosis in generalised myasthenia gravis: a multicentre cross-sectional study in Japan. J Neurol Neurosurg Psychiatry 89:513–517. https://doi.org/10.1136/jnnp-2017-316625
Jaretzki A 3rd, Barohn RJ, Ernstoff RM et al (2000) Myasthenia gravis: recommendations for clinical research standards. Task Force of the Medical Scientific Advisory Board of the Myasthenia Gravis Foundation of America. Neurology 55:16–23. https://doi.org/10.1212/wnl.55.1.16
Barohn RJ, McIntire D, Herbelin L et al (1998) Reliability testing of the quantitative myasthenia gravis score. Ann N Y Acad Sci 841:769–772. https://doi.org/10.1111/j.1749-6632.1998.tb11015.x
Skeie GO, Apostolski S, Evoli A et al (2010) Guidelines for treatment of autoimmune neuromuscular transmission disorders. Eur J Neurol 17:893–902. https://doi.org/10.1111/j.1468-1331.2010.03019.x
Murai H, Utsugisawa K, Nagane Y et al (2018) Rationale for the clinical guidelines for myasthenia gravis in Japan. Ann N Y Acad Sci 1413:35–40. https://doi.org/10.1111/nyas.13544
Sanders DB, Evoli A (2010) Immunosuppressive therapies in myasthenia gravis. Autoimmunity 43(5–6):428–435. https://doi.org/10.3109/08916930903518107
Kerty E, Elsais A, Argov Z, Evoli A, Gilhus NE (2014) EFNS/ENS Guidelines for the treatment of ocular myasthenia. Eur J Neurol 21(5):687–693. https://doi.org/10.1111/ene.12359
Melzer N, Ruck T, Fuhr P, Gold R, Hohlfeld R, Marx A, Melms A, Tackenberg B, Schalke B, Schneider-Gold C, Zimprich F, Meuth SG, Wiendl H (2016) Clinical features, pathogenesis, and treatment of myasthenia gravis: a supplement to the Guidelines of the German Neurological Society. J Neurol 263(8):1473–1494. https://doi.org/10.1007/s00415-016-8045-z
Evoli A, Antonini G, Antozzi C, DiMuzio A, Habetswallner F, Iani C, Inghilleri M, Liguori R, Mantegazza R, Massa R, Pegoraro E, Ricciardi R, Rodolico C (2019) Italian recommendations for the diagnosis and treatment of myasthenia gravis. Neurol Sci 40(6):1111–1124. https://doi.org/10.1007/s10072-019-03746-1
Palace J, Newsom-Davis J, Lecky B (1998) A randomized double-blind trial of prednisolone alone or with azathioprine in myasthenia gravis. Myasthenia Gravis Study Group Neurology 50:1778–1783. https://doi.org/10.1212/wnl.50.6.1778
Gilhus NE, Skeie GO, Romi F et al (2016) Myasthenia gravis - autoantibody characteristics and their implications for therapy. Nat Rev Neurol 12:259–268. https://doi.org/10.1038/nrneurol.2016.44
Sharshar T, Porcher R, Demeret S, Tranchant C, Gueguen A, Eymard B, Nadaj-Pakleza A, Spinazzi M, Grimaldi L, Birnbaum S, Friedman D, Clair B; MYACOR Study Group. Comparison of corticosteroid tapering regimens in myasthenia gravis: a randomized clinical trial. JAMA Neurol. 2021;78(4):426–433. https://doi.org/10.1001/jamaneurol.2020.5407
Pascuzzi RM, Coslett HB, Johns TR (1984) Long-term corticosteroid treatment of myasthenia gravis: report of 116 patients. Ann Neurol 15:291–298. https://doi.org/10.1002/ana.410150316
Utsugisawa K, Suzuki S, Nagane Y et al (2014) Health-related quality-of-life and treatment targets in myasthenia gravis. Muscle Nerve 50:493–500. https://doi.org/10.1002/mus.24213
Lee CY, Lam CL, Pang SY et al (2015) Clinical outcome of generalized myasthenia gravis in Hong Kong Chinese. J Neuroimmunol 289:177–181. https://doi.org/10.1016/j.jneuroim.2015.10.018
Chen D, Peng Y, Li Z et al (2020) Prognostic Analysis of Thymoma-associated myasthenia gravis (MG) in Chinese patients and its implication of MG management: experiences from a tertiary hospital. Neuropsychiatr Dis Treat 16:959–967. https://doi.org/10.2147/NDT.S243519
Imai T, Suzuki S, Tsuda E, Nagane Y, Murai H, Masuda M, Konno S, Suzuki Y, Nakane S, Fujihara K, Suzuki N, Utsugisawa K (2015) Oral corticosteroid therapy and present disease status in myasthenia gravis. Muscle Nerve 51(5):692–696. https://doi.org/10.1002/mus.24438
Huang CS, Hsu HS, Huang BS et al (2005) Factors influencing the outcome of transsternal thymectomy for myasthenia gravis. Acta Neurol Scand 112:108–114. https://doi.org/10.1111/j.1600-0404.2005.00424.x
de Perrot M, Liu J, Bril V et al (2002) Prognostic significance of thymomas in patients with myasthenia gravis. Ann Thorac Surg 74:1658–1662. https://doi.org/10.1016/s0003-4975(02)04083-3
Tsinzerling N, Lefvert AK, Matell G et al (2007) Myasthenia gravis: a long term follow-up study of Swedish patients with specific reference to thymic histology. J Neurol Neurosurg Psychiatry 78:1109–1112. https://doi.org/10.1136/jnnp.2006.109488
Andersen JB, Gilhus NE, Sanders DB (2016) Factors affecting outcome in myasthenia gravis. Muscle Nerve 54:1041–1049. https://doi.org/10.1002/mus.25205
Tomschik M, Hilger E, Rath J et al (2020) Subgroup stratification and outcome in recently diagnosed generalized myasthenia gravis. Neurology 95:e1426–e1436. https://doi.org/10.1212/WNL.0000000000010209
Papatestas AE, Genkins G, Kornfeld P et al (1987) Effects of thymectomy in myasthenia gravis. Ann Surg 206:79–88. https://doi.org/10.1097/00000658-198707000-00013
Kim H, Lim YM, Lee EJ et al (2018) Factors predicting remission in thymectomized patients with acetylcholine receptor antibody-positive myasthenia gravis. Muscle Nerve 58:796–800. https://doi.org/10.1002/mus.26300
Kaufman AJ, Palatt J, Sivak M et al (2016) Thymectomy for myasthenia gravis: complete stable remission and associated prognostic factors in over 1000 cases. Semin Thorac Cardiovasc Surg 28:561–568. https://doi.org/10.1053/j.semtcvs.2016.04.002
Yu S, Li F, Chen B et al (2015) Eight-year follow-up of patients with myasthenia gravis after thymectomy. Acta Neurol Scand 131:94–101. https://doi.org/10.1111/ane.12289
Kanai T, Uzawa A, Kawaguchi N et al (2019) Predictive score for oral corticosteroid-induced initial worsening of seropositive generalized myasthenia gravis. J Neurol Sci 396:8–11. https://doi.org/10.1016/j.jns.2018.10.018
Suzuki Y, Utsugisawa K, Suzuki S et al (2011) Factors associated with depressive state in patients with myasthenia gravis: a multicentre cross-sectional study. BMJ Open 1:e000313. https://doi.org/10.1136/bmjopen-2011-000313
Masuda M, Utsugisawa K, Suzuki S et al (2012) The MG-QOL15 Japanese version: validation and associations with clinical factors. Muscle Nerve 46(2):166–173. https://doi.org/10.1002/mus.23398
Acknowledgements
We thank all the staff involved in this study, as well as the patients and their families for their participation and cooperation. This work was supported by the Heilongjiang Provincial Postdoctoral Science Foundation (LBH-Z16149) and the Scientific Research Fund of the Second Affiliated Hospital of Harbin Medical University (KYCX2018-18).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
The study was approved by the Ethics Committee of the 2nd affiliated hospital of Harbin Medical University.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, Y., Li, F., Zhu, H. et al. Less is not necessarily more: low-dose corticosteroid therapy and long-term prognosis in generalized myasthenia gravis after thymectomy. Neurol Sci 43, 3949–3956 (2022). https://doi.org/10.1007/s10072-022-05897-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-05897-0