Abstract
Background
Vestibular migraine (VM) is considered the most common cause of spontaneous episodic vertigo and the second most common cause of vertigo. However, without a biomarker or a complete understanding of the pathophysiology, VM remains underrecognized and underdiagnosed. Therefore, definite diagnostic criteria are urgently needed. Meanwhile, VM should be clearly differentiated from other similar diseases. This paper may help clinicians improve the diagnostic rate of VM and reduce the rate of misdiagnosis. A PubMed search was performed using the following terms: vestibular migraine, migraine-associated vertigo/dizziness, migraine-related vertigo, migraine-related vestibulopathy, benign recurrent vertigo, vertiginous migraine, migraine, headache, vertigo, dizziness, and diagnosis. This paper also summarizes the diagnostic criteria and differential diagnoses of VM. The diagnosis of VM is based on the symptoms, degree, frequency, and duration of the vestibular episodes, a history of migraine, and the temporal association of migraine symptoms with vestibular episodes in at least 50% of cases, while ruling out what may be due to other reasons. In addition to vestibular symptoms and migraine, transient auditory symptoms, nausea, vomiting, and susceptibility to motion sickness may also be associated with VM. Thus, VM should be differentiated from other diseases such as Meniere’s disease, benign paroxysmal positional vertigo, migraine with brainstem aura, vestibular neuritis, posterior circulation ischemia, multiple lacunar infarction, vestibular paroxysmia, motion sickness, and episodic ataxia type 2.
Conclusion
Only if the diagnostic criteria of VM and differential diagnosis can be mastered clearly, we can make a definite diagnosis and treat patients properly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
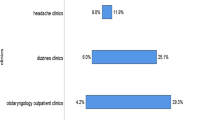
Vertigo and headache are common and debilitating symptoms in clinical neurology and otolaryngology. Since the initial report describing the association between migraine and vertigo, various studies have demonstrated that vestibular migraine (VM) is considered the most common cause of episodic vertigo in adults, children, and adolescents [1]. It has been increasingly recognized as a frequent cause of vertigo, which affects up to 1% of the general population, with female preponderance [2]. Familial occurrence is common. It has been reported in some patients with an autosomal dominant pattern of inheritance and decreased penetrance in men [3]. Despite its pervasiveness, many physicians, neurologists, and otolaryngologists have not mastered the correct diagnosis and proper treatment of vestibular migraine. Furthermore, there are many terms to describe the disease combining the symptoms of vertigo and headache. Although previously used names including migraine-associated vertigo/dizziness, migraine-related vertigo, migraine-related vestibulopathy, benign recurrent vertigo, vestibular migraine, vertiginous migraine, and migrainous vertigo were given to the association of migraine and vertigo, the term “vestibular migraine” has been convincingly advocated as a condition that stresses the particular vestibular manifestation of migraine, and thus best avoids confounding with nonvestibular dizziness related to migraine [4,5,6]. To study vestibular migraine in the future, we herein review the diagnostic methods to help clinicians promptly identify vestibular migraine, emphasizing clues for differential diagnosis.
Clinical presentation
The mechanisms underlying vestibular migraine are not completely understood. However, researchers have found that there are many triggers for vestibular migraine, and these triggers vary from person to person. Understanding these triggers can help patients avoid attacks of vestibular migraine. Similar to the triggers of migraine, the triggers of vestibular migraine include stress, anxiety, sleep disturbance, environmental factors (such as bright artificial light, barometric pressure variations), food (aged or ripened cheeses, foods containing large amounts of monosodium glutamate, smoked, cured, or processed meats), drinking (caffeine, alcohol, cola), hormonal fluctuations (such as during menstruation), and medications. In a Chinese study, researchers investigated the predisposing factors by means of questionnaires, memory diaries, and regular follow-up. The study demonstrated that sleep disorders, alright space intolerance, excessive stress, lack of exercise, and dietary preference may be associated with vestibular migraine attacks [7]. In a single-center retrospective study, the researchers found that the common triggers were stress (39.7%), bright light (26.7%), weather changes (26.0%), and sleep deprivation (26.0%) [8].
The symptoms of vestibular migraine are heterogeneous in terms of frequency, duration, and association with headache [9]. Patients with vestibular migraine typically report many types of vestibular symptoms. The different vestibular symptoms that occur during vestibular migraine attacks include spontaneous vertigo, positional vertigo, head motion-induced dizziness/vertigo, postural unsteadiness, oscillopsia, visually induced dizziness/vertigo, and directional pulsion [10]. In patients with vestibular migraine, rotational or nonrotational vertigo can occur spontaneously or in association with a change in position [11]. Other frequent additional symptoms include imbalance, spatial disorientation, illusory motion, and nausea aggravated or provoked by head movements. Nausea and imbalance are frequent but non-specific accompaniments of acute vestibular migraine [12]. For individuals, different patients may experience different symptoms during different episodes. Headaches may accompany vestibular migraine episodes and are often less severe compared with their typical migraine-related headaches [10]; however, about 30% of all vestibular migraine attacks are not accompanied by headaches [11]. A retrospective cross-sectional study suggests that patients with vestibular migraine are more likely to have occipital headaches than patients with migraine without vestibular symptoms [13]. Meanwhile, some other related symptoms of vestibular migraine may occur before, during, or after vestibular symptoms.
Both the duration and frequency of attacks are highly variable between patients and individual patients over time [12]. Approximately 30% of vestibular migraine patients have attacks lasting minutes, 30% have episodes for hours, and another 30% have attacks over several days. The remaining 10% have episodes lasting seconds only, which tend to occur repeatedly during head motion, visual stimulation, or after changes in head position [14].
Other concomitant symptoms are also widespread in patients with vestibular migraine. These symptoms include lightheadedness, anxiety, depression, swimming sensation, photophobia, phonophobia, tinnitus, aural pressure, excessive motion sickness susceptibility, diminished hearing, and palpitations.
Diagnostic criteria
Despite their high prevalence and morbidity, vestibular migraines remain poorly understood [15]. According to previous research, physical examination and laboratory results are usually negative in patients with vestibular migraine, and there is no biomarker in these patients. Even so, MRI in patients with vestibular migraine mainly demonstrates multiple punctate equal T1 and long T2 signals on FLAIR (fluid-attenuated inversion recovery) in subcortical white matter [16]. Compared with healthy controls, fMRI (functional magnetic resonance imaging) demonstrates activation of brain areas related to integration of visual and vestibular cues (increased activation of the paracentral lobule and bilateral inferior parietal lobule and decreased activation of the left superior frontal gyrus, head of the caudate nucleus, left superior temporal gyrus, left parahippocampal gyrus, and right lingual gyrus) [17]. In a recent study of vestibular migraine using fMRI, patients with VM showed significantly lower amplitude of low-frequency fluctuation (ALFF) in the right putamen, and significantly higher ALFF in the right lingual gyrus. In addition, VM patients showed significantly higher functional connectivity (FC) among the cerebellum, the left dorsolateral superior frontal gyrus and the right putamen but significantly lower FC among the left median cingulate, paracingulate gyri, and the right putamen. There are functional abnormalities in nociceptive, vestibular, and visual cortex regions in patients with VM during the interictal period [18]. So far, the diagnosis of vestibular migraine is based on a history of migraine, the symptoms, degree, frequency, and duration of the vestibular episodes, the temporal association of migraine symptoms with vestibular episodes in at least 50% of cases, while ruling out what may be caused by other reasons [19]. Although the diagnostic criteria for vestibular migraine were initially identified in 2001, a more accurate description of the disease was reported in the Consensus Report of the Barany Society and the International Headache Society in 2012[20]. In 2018, the International Headache Society (IHS) created the latest consensus document with diagnostic criteria for vestibular migraine, which was added to the appendix of the new ICHD-3 version of the International Headache Classification (Table 1) [14].
Differential diagnosis
Meniere’s disease
Meniere’s disease (MD) is a chronic illness characterized by intermittent episodes of vertigo lasting from minutes to hours, with fluctuating sensorineural hearing loss, tinnitus, and aural pressure [21]. The diagnosis of vestibular migraine and Meniere’s disease is mainly based on clinical presentation. Both diseases are episodic vestibular syndromes defined by a set of associated symptoms such as tinnitus, hearing loss, or migraine features during attacks [22]. Because of the symptom overlap, the differential diagnosis between vestibular migraine and Meniere’s disease is difficult. However, hearing loss gradually occurs in patients with Meniere’s disease after many attacks, and nonprogressive sensorineural hearing loss may occur in vestibular migraine patients experiencing numerous episodes. A study elucidated that patients with Meniere’s disease or vestibular migraine have a different proinflammatory signature, and a cytokine panel could be used as biological markers for the differential diagnosis [22]. A prospective cohort study was conducted to study the differential diagnosis of vestibular migraine and Meniere’s disease using magnetic resonance imaging (MRI) of intratympanic gadolinium. They have shown that 3D-real-IR MRI may help differentiate between vestibular migraine and Meniere’s disease [23]. Another retrospective study suggests that MRI could be used to differentiate MD from VM patients with cochlear symptoms [24]. A prospective cohort study was conducted to determine whether cervical vestibular-evoked myogenic potential (VEMP) or ocular VEMP responses can differentiate between vestibular migraine and Meniere’s disease. They found that no VEMP test investigated segregated individuals with Meniere’s disease from those with vestibular migraine [25]. However, another retrospective study suggests that there is a more common saccular than utricular dysfunction in MD and a more permanent loss of otolith function in MD versus VM. The different patterns of o- and cVEMP responses might add to the differential diagnosis between MD and VM [26]. A new study found a higher proportion of abnormal electrocochleography (EcochG) in MD than in VM (p = 0.02) without any significant difference in the video head impulse test (vHIT) gain [27]. In a word, Meniere’s disease revealed later age of onset, more hearing loss, tinnitus, aural fullness, abnormal nystagmus, abnormal caloric testing results, and endolymphatic hydrops. Meanwhile, vestibular migraine revealed more headaches, photophobia, vomiting, and aura [28].
Benign paroxysmal positional vertigo
Benign paroxysmal positional vertigo (BPPV) is the most common cause of peripheral vertigo [29]. BPPV is characterized by spontaneous resolution after a period of time (benign), short-lasting episodes (paroxysmal), and symptoms provoked by head movements (positional) [30]. Patients with vestibular migraine or benign paroxysmal positional vertigo always have symptoms of episodic positional vertigo. Differentiating vestibular migraine from BPPV is critical because the treatment of each disorder is significantly different [31]. The positional vertigo in patients with vestibular migraine is different from BPPV in terms of the duration of the individual attack (often as long as the head position is maintained in vestibular migraine versus seconds only in BPPV) and duration of symptomatic episodes (minutes to days in vestibular migraine versus weeks in BPPV) [5]. Additionally, direct observation of the nystagmus pattern during acute episodes with positional testing can help distinguish between vestibular migraine and BPPV [10]. The nystagmus of vestibular migraine patients is persistent, lacks latency, and does not show correspondence to single semicircular canal characteristics [8, 32, 33]. On the contrary, the nystagmus of BPPV patients is characterized with short period of time, having a latent period, fatigability, angular transposition [31, 34].
Migraine with brainstem aura
Migraine with brainstem aura (MBA) was previously termed as basilar artery, basilar, and basilar-type migraines [35]. Migraine with brainstem aura is defined as a migraine with aura including at least two of the following fully reversible brainstem symptoms: dysarthria, vertigo, tinnitus, hypacusis, diplopia, ataxia not attributable to sensory deficit, decreased level of consciousness (GCS ≤ 13), and no motor or retinal symptoms [14, 36]. In addition to at least two posterior circulation symptoms, the symptoms must last from 5 to 60 min and be followed by a migraine headache [14]. However, vestibular migraines cannot meet these diagnostic criteria. In a controlled study, the researchers compared the clinical manifestations of basilar migraine with the clinical manifestations of migraine. As regard to differentiating between basilar type migraine and definite migrainous vertigo patients, the former revealed higher occurrence rates than the latter in relation to the frequency of vertigo attacks, neurological symptoms, and saccadic dysmetria [37].
Vestibular neuritis
Vestibular neuritis (VN) is the sixth leading cause of vertigo with an incidence of 8% according to large population studies [38]. It is a disease of the unilateral peripheral vestibular system. The primary symptoms of vestibular neuritis are characterized by rotatory vertigo with an acute onset lasting several days, horizontal spontaneous nystagmus (with a rotational component) toward the unaffected ear, a pathologic head impulse toward the affected ear, a deviation of the subject visual vertical toward the affected ear, postural imbalance with falls toward the affected ear, and nausea [39]. Most cases of vestibular migraine are caused by viral infection, either in the inner ear or other parts of the body. Therefore, vestibular migraine can be differentiated from vestibular neuritis based on the history of infection and the duration of the episode. Vestibular neuritis always has a history of upper respiratory tract infection that lasts for several days. Moreover, glucocorticoid therapy and vestibular rehabilitation are effective for treating vestibular neuritis. The symptoms of vestibular migraine are self-limiting. However, vestibular migraines do not meet the diagnostic criteria.
Posterior circulation ischemia
Isolated transient vertigo can be the symptom of posterior circulation ischemia (PCI). Therefore, it is essential to differentiate isolated vertigo of a cerebrovascular origin from that of a more benign origin (such as vestibular migraine), as patients with cerebral ischemia have a much higher risk of future stroke than those with peripheral vertigo [40]. Symptoms of posterior circulation ischemia can range from simple orthostatic dizziness to episodic transient ischemic attacks and stroke [41]. These symptoms of posterior circulation ischemia are characterized by intermittent episodes of multiple neurological symptoms including motor and sensory symptoms, occurring unilaterally or bilaterally, ataxia of gait, dysmetria, diplopia, dysarthria and bilateral homonymous hemianopsia, vertigo, and tinnitus [42]. Besides vertigo, patients with posterior circulation ischemia have other neurological deficit symptoms, and high-risk factors associated with cerebrovascular diseases. These high-risk factors include elderly people, abnormal blood pressure, abnormal blood fat, pathoglycemia, and arteriosclerosis. In contrast, the mean age of vestibular migraine is younger than that of posterior circulation ischemia, with a female preponderance. Motion sickness, motion sensitivity, photophobia, and phonophobia are significant differential highlights of vestibular migraine. Otherwise, cerebral MRI may be an important examination for differential diagnosis [43].
Multiple lacunar infarction
Multiple lacunar infarctions (MLI) occur when one of the arteries that provide blood to the brain’s deep structures is blocked. These arteries are small and uniquely vulnerable. High blood pressure and diabetes mellitus are the most important causes of multiple lacunar infarctions. The symptoms of lacunar stroke vary depending on the part of the damaged brain. Symptoms can include weakness or paralysis of the face, arm, legs, feet or toes, sudden numbness, difficulty speaking, clumsiness of the hand or arm, and other neurological symptoms. Although the MRI lesion features of multiple lacunar infarctions are similar to the MRI lesion features of vestibular migraine, they are actually different. The manifestations of MRI in patients with vestibular migraine are mainly multiple punctuate equal T1 and long T2 signals or high signals on fluid-attenuated inversion recovery (FLAIR) in the semioval center, subcortical white matter, or near white matter. Furthermore, MRI changes in vestibular migraine patients have their own specific clinical characteristics (such as visual aura, photophobia, and phonophobia) and are mainly seen in females with visual aura [16]. However, the MRI lesions of multiple lacunar infarctions are mainly located in the basal ganglia region, accompanied by leukoaraiosis in the periventricular region [44]. In addition, the features of MRI signals in multiple lacunar infarction patients are primarily multiple punctuate long T1 and long T2 signals or high signals on FLAIR [16].
Vestibular paroxysmia
Vestibular paroxysmia (VP) is defined by an episodic vestibular disorder that usually presents with a high frequency of short vertiginous attacks, and the presence of microvascular compression of the eighth cranial nerve [45]. The course of the disease is usually chronic (often longer than three months) with some patients suffering hundreds of attacks per year. It is supposed that vestibular paroxysmia occurs due to compression of the eighth cranial nerve (otherwise known as the vestibulocochlear nerve) by an artery. Researchers have found that treatment with antiseizure medication (carbamazepine/oxcarbazepine) and surgical treatment has been shown to reduce the intensity, frequency, and duration of attacks. Thus, the diagnostic criteria for vestibular paroxysmia were published by the Classification Committee of the Barany Society in 2016. The diagnosis of VP is mainly based on the patient’s history and requires (A) at least ten attacks of spontaneous spinning or non-spinning vertigo, (B) duration less than 1 min, (C) stereotyped phenomenology in a particular patient, (D) response to treatment with carbamazepine/oxcarbazepine, and (E) not better accounted for by another diagnosis [46]. However, the characteristics of vestibular migraine compared with vestibular paroxysmia are current or history of migraine, usually less frequency of attacks, and the longer duration of the attacks (5 min to 72 h), and most attacks are accompanied by other migrainous symptoms.
Motion sickness
Motion sickness (MoS) describes a set of common and complex autonomic symptoms caused by incongruent sensory impressions under conditions of motion [47]. The typical signs and symptoms of motion sickness are quite different, including the central nervous system, gastrointestinal, and autonomic symptoms. Specifically, they manifest as initial dizziness, physical distress, fatigue, yawning, facial pallor, oversensitivity to smell, sweating, headache, and, once fully developed, nausea and vomiting with apathy and fear of annihilation [48], Migraine is linked with various comorbid conditions, the most prominent being motion sickness. Moreover, migraine sufferers have heightened vulnerability to motion sickness [49]. Hence, the susceptibility to motion sickness may be associated with vestibular migraine [50]. Despite the correlation, we may differentiate the diagnosis from history, inducing factors, initial symptoms, and accompanying symptoms.
Episodic ataxia type 2
Episodic ataxia type 2 (EA2) is a rare autosomal dominant neuronal disorder resulting from mutations in the Cav2.1 subunit of P/Q-type calcium channels [51]. It manifests with recurrent disabling attacks of imbalance, episodic vertigo, ataxia, nystagmus, in patients with a history of migraine, and can be provoked by physical exertion or emotional stress [52]. Episodic ataxia 2 usually begins in early childhood, most often before the age of 20 years. Brain MRI may demonstrate cerebellar vermis atrophy [53]. For most patients with episodic ataxia type 2, acetazolamide is effective in controlling or reducing the frequency and severity of attacks. Although it may be difficult to differentiate vestibular migraine from episodic ataxia type 2 based on clinical manifestations alone, clues from family history, age of onset, triggers, brain MRI, and response to acetazolamide can be helpful [10].
The differential diagnosis of vestibular migraine is shown in Table 2.
Conclusion
Despite being the most common cause of episodic vertigo, vestibular migraine is still an underdiagnosed and inadequately treated disease. However, with the recent addition of new diagnostic criteria in the appendix of the ICHD-3 in 2018, future studies on vestibular migraine will aid in the characterization of this disorder. Without specific and precise biomarkers, the differential diagnosis to rule out other diseases mainly depends on clinical manifestations. Only if the diagnosis criteria of vestibular migraine and differential diagnosis can be mastered clearly can we enroll patients with vestibular migraine for further studies. Ultimately, we can make a definite diagnosis and treat the patients properly.
Abbreviations
- VM:
-
Vestibular migraine
- IHS:
-
The International Headache Society
- ICHD-3:
-
The International Classification of Headache Disorders, 3rd Edition
- MD:
-
Meniere’s disease
- EcochG:
-
Abnormal electrocochleography
- vHIT:
-
Video head impulse test
- BPPV:
-
Benign paroxysmal positional vertigo
- MBA:
-
Migraine with brainstem aura
- VN:
-
Vestibular neuritis
- PCI:
-
Posterior circulation ischemia
- MRI:
-
Magnetic resonance imaging
- fMRI:
-
Functional magnetic resonance imaging
- FLAIR:
-
Fluid-attenuated inversion recovery
- ALFF:
-
Amplitude of low-frequency fluctuation
- FC:
-
Functional connectivity
- MLI:
-
Multiple lacunar infarctions
- VP:
-
Vestibular paroxysmia
- MoS:
-
Motion sickness
- EA2:
-
Episodic ataxia type 2
References
Dieterich M, Obermann M, Celebisoy N (2016) Vestibular migraine: the most frequent entity of episodic vertigo. J Neurol 263(Suppl 1):S82–S89
Tedeschi G et al (2015) Vestibular migraine pathophysiology: insights from structural and functional neuroimaging. Neurol Sci 36(Suppl 1):37–40
Luzeiro I et al (2016) Vestibular migraine: clinical challenges and opportunities for multidisciplinarity. Behav Neurol 2016:6179805
Akdal G (2013) Vestibular migraine. Noro Psikiyatr Ars 50(Suppl 1):S56–S59
Lempert T (2013) Vestibular migraine. Semin Neurol 33(3):212–218
Cherian N (2013) Vertigo as a migraine phenomenon. Curr Neurol Neurosci Rep 13(4):343
Xiao BJ, Bi Y, Zheng TH (2019) investigation on the triggers and the effect of healthy education on recurrence of vestibular migraine. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 33(7):577–580
Beh SC et al (2019) The Spectrum of vestibular migraine: clinical features, triggers, and examination findings. Headache 59(5):727–740
Park JH, Viirre E (2010) Vestibular migraine may be an important cause of dizziness/vertigo in perimenopausal period. Med Hypotheses 75(5):409–414
Beh SC (2019) Vestibular migraine: how to sort it out and what to do about it. J Neuroophthalmol 39(2):208–219
Stolte B et al (2015) Vestibular migraine. Cephalalgia 35(3):262–270
Lempert T, Neuhauser H (2009) Epidemiology of vertigo, migraine and vestibular migraine. J Neurol 256(3):333–338
Wattiez AS et al (2020) Patients with vestibular migraine are more likely to have occipital headaches than those with migraine without vestibular symptoms. Headache 60(8):1581–1591
(2018) Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia 38(1):1–211
King S et al (2019) Self-motion perception is sensitized in vestibular migraine: pathophysiologic and clinical implications. Sci Rep 9(1):14323
Qiu F et al (2017) Analysis of the clinical features of vestibular migraine with MRI changes. Zhonghua Yi Xue Za Zhi 97(14):1049–1053
Teggi R et al (2016) A review of recent literature on functional MRI and personal experience in two cases of definite vestibular migraine. Neurol Sci 37(9):1399–1402
Wang S et al (2021) A resting-state functional MRI study in patients with vestibular migraine during interictal period. Acta Neurol Belg. https://doi.org/10.1007/s13760-021-01639-9
Sohn JH (2016) Recent advances in the understanding of vestibular migraine. Behav Neurol 2016:1801845
Celik O et al (2020) The effectiveness of medical prophylactic treatment on vestibular migraine and its effect on the quality of life. J Int Adv Otol 16(1):28–33
Sajjadi H, Paparella MM (2008) Meniere’s disease. Lancet 372(9636):406–414
Flook M et al (2019) Differential proinflammatory signature in vestibular migraine and meniere disease. Front Immunol 10:1229
Sun W et al (2017) Magnetic resonance imaging of intratympanic gadolinium helps differentiate vestibular migraine from Meniere disease. Laryngoscope 127(10):2382–2388
Eliezer M et al (2021) Recurrent vestibulopathy: are cVEMP, oVEMP and inner ear MRI useful to distinguish patients with Meniere’s disease and vestibular migraine? Eur Arch Otorhinolaryngol. https://doi.org/10.1007/s00405-021-06716-6
Zuniga MG et al (2012) Can vestibular-evoked myogenic potentials help differentiate Meniere disease from vestibular migraine? Otolaryngol Head Neck Surg 146(5):788–796
Dlugaiczyk J, Habs M, Dieterich M (2020) Vestibular evoked myogenic potentials in vestibular migraine and Meniere’s disease: cVEMPs make the difference. J Neurol 267(Suppl 1):169–180
Martines F et al (2020) Comparison of electrocochleography and video head impulse test findings in vestibular migraine and meniere disease: a preliminary study. J Int Adv Otol 16(2):183–189
Tabet P, Saliba I (2017) Meniere’s disease and vestibular migraine: updates and review of the literature. J Clin Med Res 9(9):733–744
Oya R et al (2019) Clinical significance of cervical and ocular vestibular evoked myogenic potentials in benign paroxysmal positional vertigo: a meta-analysis. Eur Arch Otorhinolaryngol 276(12):3257–3265
Turk B et al (2021) Benign paroxysmal positional vertigo: comparison of idiopathic BPPV and BPPV secondary to vestibular neuritis. Ear Nose Throat J 100(7):532–535
Beh SC (2018) Horizontal direction-changing positional nystagmus and vertigo: a case of vestibular migraine masquerading as horizontal canal BPPV. Headache 58(7):1113–1117
von Brevern M et al (2005) Acute migrainous vertigo: clinical and oculographic findings. Brain 128(Pt 2):365–374
Polensek SH, Tusa RJ (2010) Nystagmus during attacks of vestibular migraine: an aid in diagnosis. Audiol Neurootol 15(4):241–246
Roberts RA, Gans RE, Kastner AH (2006) Differentiation of migrainous positional vertigo (MPV) from horizontal canal benign paroxysmal positional vertigo (HC-BPPV). Int J Audiol 45(4):224–226
Bharani AK et al (1985) Basilar artery migraine. J Assoc Physicians India 33(3):239
Demarquay G et al (2018) Migraine with brainstem aura: why not a cortical origin? Cephalalgia 38(10):1687–1695
Wang CT, Lai MS, Young YH (2009) Relationship between basilar-type migraine and migrainous vertigo. Headache 49(3):426–434
Emiliano De Schutter D, Perez Fernandez N (2017) Relapsing ipsilateral vestibular neuritis. Case Rep Otolaryngol 2017:3628402
Strupp M, Brandt T (2009) Vestibular neuritis. Semin Neurol 29(5):509–519
Blasberg TF et al (2017) Isolated transient vertigo: posterior circulation ischemia or benign origin? BMC Neurol 17(1):111
Misra M et al (2004) Multidisciplinary treatment of posterior circulation ischemia. Neurol Res 26(1):67–73
Ueda K, Toole JF, McHenry LC Jr (1979) Carotid and vertebrobasilar transient ischemic attacks: clinical and angiographic correlation. Neurology 29(8):1094–1101
Wu Z et al (2007) Differential diagnosis between vertigo of posterior circulation ischemia and migrainous vertigo. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 21(16):721–723
Qi XK (2019) Pay attention to the differential diagnosis between vestibular migraine and multiple lacunar infarction. Zhonghua Nei Ke Za Zhi 58(6):409–411
Ihtijarevic B et al (2019) Symptoms and signs in 22 patients with vestibular paroxysmia. Clin Otolaryngol 44(4):682–687
Strupp M et al (2016) Vestibular paroxysmia: diagnostic criteria. J Vestib Res 26(5–6):409–415
Koch A et al (2018) The neurophysiology and treatment of motion sickness. Dtsch Arztebl Int 115(41):687–696
Strupp M et al (2018) Prevalence of motion sickness in various vestibular disorders: a study on 749 patients. J Neurol 265(Suppl 1):95–97
Cuomo-Granston A, Drummond PD (2010) Migraine and motion sickness: what is the link? Prog Neurobiol 91(4):300–312
Abouzari M et al (2020) The relationship between vestibular migraine and motion sickness susceptibility. Otol Neurotol 41(8):1116–1121
Dorgans K et al (2017) Characterization of the dominant inheritance mechanism of Episodic Ataxia type 2. Neurobiol Dis 106:110–123
Strupp M, Zwergal A, Brandt T (2007) Episodic ataxia type 2. Neurotherapeutics 4(2):267–273
Mantuano E et al (2010) Identification of novel and recurrent CACNA1A gene mutations in fifteen patients with episodic ataxia type 2. J Neurol Sci 291(1–2):30–36
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shen, Y., Qi, X. Update on diagnosis and differential diagnosis of vestibular migraine. Neurol Sci 43, 1659–1666 (2022). https://doi.org/10.1007/s10072-022-05872-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-05872-9