Abstract
Fibromyalgia (FM) is a condition characterized by chronic widespread pain whose pathogenesis is still not fully defined. Evidence based on structural and functional neuroimaging methods, electrophysiological, and morphological – skin biopsy – features demonstrated a central and peripheral nervous system involvement. A dysfunction in nociceptive inputs processing at the central level was highlighted as the primary cause of FM, but other data coming from different laboratories contributed to emphasize again the peripheral origin of FM. In fact, small fibers neuropathy (SFN) was observed in a large number of patients submitted to skin biopsy. The complex interaction between central and peripheral factors is opening a new scenario about the management of this neurological disorder. Whether proximal SFN is an initiating event leading to FM or is the consequence of stress-related insular hyper excitability remains unclear. Mild sufferance of peripheral afferents could function as a trigger for an exaggerated response of the so-called “salience matrix” in predisposed individuals. On the other side, the intriguing hypothesis rising from animal models could indicate that the cortical hyper function could cause peripheral small afferent damage. The research should go on the genetic origin of such peripheral and central abnormalities, the acquired facilitating factors, and the presence of different phenotypes in order to search for efficacious treatments, which are still lacking.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last years, new data about central and peripheral nervous system involvement are progressively changing the general view about fibromyalgia (FM) pathophysiology. In the past, FM has been considered a generalized painful syndrome based on a muscular low pain threshold [1,2,3], so muscle tenderness had a key role in clinical diagnosis [4]. However, the absence of chronic inflammatory process in muscles of FM patients raised the hypothesis of a self-sustained mechanism of chronic pain, based on neural phenomena of central and peripheral sensitization. Abnormal activity of nociceptors in muscles and deep tissues seemed a reliable cause of FM, though the hypothesis remained vague [5]. Overall, a dysfunction in nociceptive inputs processing at the central level was highlighted as the primary cause of FM, sustained by several clinical, psychophysiological, and neurophysiological evidence [6]. This view contributed to attenuate the diagnostic relevance of the tender points in the last clinical criteria, in favor of associated symptoms including comorbidities for central nervous system diseases as headache, depression, and sleep disturbances [7]. Other data coming from different laboratories contributed to emphasize again the peripheral origin of FM. In fact, small fibers neuropathy (SFN) was observed in a large number of patients submitted to skin biopsy. A recent meta-analysis reported 49% SFN prevalence across studies on FM populations [8]. The present narrative review, founded on the PUB-Med search in the time interval 2015–2020, aimed to shed light and summarize main findings on FM pathophysiology, by assessing:
-
1)
Evidence about central nervous system involvement, based on structural and functional neuroimaging and electrophysiological methods
-
2)
Evidence about peripheral nervous system involvement, based on electrophysiological and morphological – skin biopsy – features
-
3)
A final unified hypothesis on FM pathogenesis
Methods
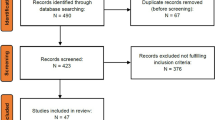
The present narrative review is based on the PubMed search in the time interval 2015–2020, using the following keywords: for the first aim, fibromyalgia and (a) magnetic resonance, functional magnetic resonance, functional neuroimaging, (b) pain-related evoked potentials, (c) EEG (Fig. 1).
For the second aim: fibromyalgia and (a) electroneurography, nerve conduction study, electromyography (b) microneurography, (d) skin biopsy, (e) corneal confocal microscopy (Fig. 2).
Criteria for the inclusion of the studies were the observance of the current FM diagnostic criteria [4, 7] and the case–control study design. Case reports and reviews were not considered, as well as studies reporting sleep studies, neurophysiological effects of drugs, and not pharmacological interventions. We also focalized on studies on resting-state or functional changes related to pain processing, avoiding to include studies on pure cognitive tasks or multimodal not painful stimulation.
Central nervous system involvement in fibromyalgia
The existence of the organic origin of FM was frequently questioned, and it was frequently considered a psychiatric disease or even a simulation or malinger syndrome [9]. However, the clinical and psychophysiological evidence of hyperalgesia and allodynia outlined the role of widespread central sensitization as the primary cause of the disease [6, 10]. According to the International Association for the Study of Pain (IASP), the definition of central sensitization is “increased responsiveness of nociceptive neurons in the central nervous system to their normal or subthreshold afferent input”. In the following paragraph, main results about neuroimaging and electrophysiological techniques are reported.
The use of functional neuroimaging methods has changed the scenario of research in chronic pain syndromes, giving evidence of brain mechanisms connected to central sensitization. The first FMRI studies described the increased activity of primary and secondary somatosensory cortex, temporal gyrus, inferior parietal cortex, putamen, cerebellum, and anterior insula during pressure pain in FM patients compared to controls [11, 12]. In the following years, different functional neuroimaging methods were applied in FM, diagnosed in accord with 1990 criteria, with the results of altered cortical activation and connectivity in regions devoted to pain processing and descending control, as summarized by Staud R. et al. [3].
More recent studies found altered expression of secondary hyperalgesia in patients with FM. The FMRI correlate was a different activity of the dorsolateral prefrontal cortex between patients and controls, with a possible defective descending inhibitory control [13].
Craggs et al. [14] found that in a small group of FM patients [4], effective connectivity pattern related to the experimental induced wind-up phenomenon was similar to that recorded in healthy controls, while in 40 FM patients compared with control subjects, Pujol et al. [15] found an abnormal pattern of functional connectivity among PAG, insula, somatosensory, visual, and auditory cortex and between SII and default mode network, with general weakness of sensory integration underlying clinical pain.
Studies in the 2015–2020 period
Functional neuroimaging FMRI
A huge number of fMRI studies were published on FM in the last years, using a different modality of pain stimulation and resting-state connectivity patterns. All the results converged toward a clear dysfunction of painful and multimodal stimuli processing, as well as a global disruption of main cortical networks. Failure in the activation of brainstem regions devoted to the inhibitory control emerged in an experiment based on the wind-up phenomenon [16]. Other aspects of pain processing, such as the pain after sensation, determined different brain activation in FM patients as compared to controls, particularly in the medial temporal lobe (amygdala, hippocampus, parahippocampal gyrus) [17]. Manipulation of attention with distraction from pain [18] and suggestion of pain stimuli intensity [19] caused different brain responses in FM patients in respect to healthy subjects, in key zones for pain modulation. The persistence of brain activation after pain stimulation suggested more generalized hypersensitivity and hypervigilance to salient sensory events [20].
Connectivity patterns were found to be dysfunctional in FM patients. Truini et al. [21] studied 20 patients with FM and 15 controls, and found increased PAG connectivity with the insula, prefrontal cortex, and anterior cingulate, possibly causing altered descending inhibitory control. Attenuated PAG functional connectivity with regions associated with motor/executive functions, salience (SN), and default mode networks (DMN) was also negatively correlated with fibromyalgia disability and positively correlated with pain catastrophizing, in another FM group compared to controls [22]. PAG connections were differently activated in FM patients vs controls in the modulation of endogenous pain during others’ noxious stimulation observation [23]. The disrupted connectivity in the default mode network seemed related to acute rather than chronic pain in FM patients [24].
Resting-state FMRI showed different connectivity patterns during acute painful stimulation in FM patients compared to controls [25,26,27], while another study pointed out abnormal connectivity in the network processing both nociceptive and multimodal stimuli [28]. Hub connections and glutamate metabolism within the posterior insula were also correlated to clinical pain in FM [29] (Table 1).
PET
A general dysfunction in neurotransmission involved in pain modulation was reported in FM. A disturbance in dopamine neurotransmission emerged in 24 FM patients compared to 17 controls [30]. The study outlined the relationship between thermal threshold and D2/D3 receptor availability in caudate and striatum, with some differences linked to the comorbidity with depression.
Altered excitatory-inhibitory neurotransmission emerged in studies based on GABA receptors and glutamate metabolism [29, 31]. The role of microglia activation in functional changes leading to chronic pain in FM emerged by PET studies on proteins upgraded in activated glia [32]. A recent pilot study gave preliminary evidence about reduced cortical opioid receptor availability in a small FM group [33] (Table 2).
Structural MRI
Moderate evidence for changes in gray matter volume in the anterior cingulate cortex and prefrontal cortex emerged in several voxel-based morphometry-VBM studies [34]. Studies applying structural covariance network analysis outlined altered gray and white matter morphometry in cerebellar and frontal cortical regions in FM patients [35]. Moreover, volumes of cortical areas displayed a moderate classification accuracy of FM patients, which was less robust than clinical indicators [36]. Structural changes were not specific for FM, rather seemed to reflect generic cortical readjustments under chronic pain condition [37].
Reduction in hippocampus volume emerged in FM patients, for a possible atrophic mechanism consequent to excite toxicity due to dysfunctional glutamate neurotransmission [38]. More recently, a negative correlation between glutamate neurotransmission and volume of subparts of cingulated gyrus emerged in FM patients [39] (Table 3).
Summarizing, the large number of neuroimaging studies in FM, performed with different techniques and under different experimental procedures, outlined a clear disturbance in pain processing at the central level, with involvement of neurotransmission responsible for anti-nociception. The dysfunction could include several brain regions devoted to multimodal stimuli elaboration within a peculiar cognitive and emotional profile. Brain structure is not specifically altered, but most of studies indicated regional atrophies secondary to mechanisms of chronic pain.
Electrophysiological methods pain-related evoked potentials
Several studies employed pain-related evoked potentials in FM, in order to assess the functional status of nociceptive pathways, psychophysiological properties, and cognitive inference on pain processing. Laser-evoked potentials (LEPs) are specifically related to nociceptive afferents activation and confirmed increased cortical responses to painful stimuli [40] and reduced habituation in the course of repetitive sessions of stimulation [41]. These results would imply a dysfunction of experimental pain processing at the central level, a pattern largely described in diseases associated with FM, such as migraine [42]. Reduced habituation of vertex LEPs characterized the most of FM patients, while LEP amplitude varied among cases [43]. Cortical potentials obtained by painful superficial electrical stimulation, with specific properties for A-delta fibers (pain-related evoked potentials, PREPs), were found reduced in amplitude in a small cohort of FM patients, who also presented with proximal small fibers denervation and neuropathic features at the QST [44]. This study contributed to outline the relevance of small fibers pathology in FM patients, toward a neuropathic origin of pain.
In the last years, LEP studies confirmed the central dysfunction of pain processing in patients with FM. Truini et al. [21] conditioned a-delta LEPs with previous C fiber stimulation in a paired stimuli paradigm, and found reduced inhibition in FM patients, subtended by increased excitability within pain matrix (Table 2).
In the most of studies, LEP pattern was not congruent with the peripheral involvement of a-delta fibers. In fact, LEP vertex complex amplitude was within and even above normal limits in most of the patients [45]. Moreover, the presence of small fibers denervation did not influence pain sensitivity and cortical responses as assessed, respectively, by quantitative sensory testing (QST) and laser-evoked potentials in a cohort of FM patients [46]. An intriguing hypothesis was that reduced habituation could be a central mechanism able to compensate peripheral afferents loss and contrast the LEP amplitude reduction due to weak peripheral input [47].
A recent German study confirmed a congruent association between peripheral denervation, as assessed by skin biopsy and corneal confocal microscopy, PREP reduced amplitude, and severe FM picture, suggesting that small fiber pathology could have a clinical impact in a subgroup of patients [48]. Summarizing, studies on pain-related evoked responses suggested prevalent abnormalities of pain processing at the central level, except for subgroups of patients with severe small fiber pathology (Table 4). Summarizing, LEPs studies did not support a pattern of prevalent peripheral small fibers involvement in FM, rather a complex disturbance of pain processing at central level. While PREPs identified patients with small fibers impairment, their reliability in nociceptive system investigation was matter of debate [49]. A prevalent pattern of increased or reduced amplitude of LEPs could help in identifying different phenotypes within FM disease, with dominant central or peripheral nervous system involvement.
Resting-state and nociceptive-related EEG features
Several studies on FM reported abnormal resting-state and painful-related EEG rhythm patterns in wake condition. González-Roldán et al. [50] studied source localization of EEG oscillations by means of sLORETA software [51] in 20 FM females and 20 controls and found reduced power in the delta band, as well as enhanced power in beta band, located within right insula and superior and middle temporal gyrus, without correlations with clinical variables. The evaluation of coherence and phase synchronization between time series in 44 FM patients and 44 controls resulted in the detection of different functional connections within key cortical zones in pain processing, as pregenual anterior and posterior cingulate, dorsolateral prefrontal cortex, which was correlated with individual scores of disease disability [52]. Increased prefrontal and anterior cingulate theta activity significantly correlated with measures of tenderness in 19 female FM patients compared to 18 age- and sex-matched healthy controls. [53]. A magneto encephalogram (MEG) resting-state study indicated a reduction of global connectivity within default mode network, between middle/inferior temporal gyrus and visual cortex, in 18 FM patients compared to 19 controls. The longer pain duration was correlated with reduced connectivity between the inferior temporal gyrus and visual cortex, suggesting chronic pain as a cause of disrupted resting-state network [54]. A novel approach to EEG evaluation, based on changes of spatial configuration of short – 100 ms – time series, named microstate, in 46 female FM patients and 53 healthy controls, showed alterations lower occurrence and coverage of microstate in FM, indicating a sort of impaired cortical flexibility [55]. Though the EEG studies employed different types of analysis, results globally confirmed that FM patients could share abnormality in brain oscillation, common to different pain syndromes with prominent central dysfunction [56].
Peripheral nervous system involvement
In the last decade, a growing body of evidence revealed peripheral nerve involvement in FM. In their first, work, Uceyler et al. [57] used skin biopsy from leg and thigh, QST, and pain-related evoked potentials and demonstrated a small fiber pathology in FM patients. Oaklander et al. [58], in the same year, described a loss of intraepidermal nerve fibers density (IENF) in a small cohort of FM patients. Only a few months later, similar reports came by the authors of this commentary [59] who found a non-length dependent loss of IENF in skin biopsy from leg, thigh, and fingertip in 14 out of 21 patients by Giannoccaro et al. [60] and who reported abnormal cutaneous innervation in 30% of FM by Kasmidis et al. [61]. In all FM patients described in these studies, nerve conduction studies were normal, confirming the integrity of a-beta sensory fibers. Serra et al. used microneurography and found abnormal ongoing activity of peripheral C nociceptors and increased mechanical sensitivity in FM and SFN patients compared to controls [62]. They found also an abnormal slowness of nerve conduction velocities after low-frequency stimulation in mechanosensitive C nociceptors as a distinctive feature in FM patients. The demonstration of this abnormal excitability of C fibers further pointed out a malfunction of the peripheral nerves that could contribute to the pain and tenderness suffered by patients with fibromyalgia.
Here, we report the results of peripheral nervous system exploration techniques in the last 5 years.
Studies in the 2015–2020 period
Electromyography and nerve conduction studies
The majority of studies employing nerve conduction study (NCS) reported normal motor and sensitive parameters in FM patients. Doppler et al. [63] explored skin biopsy and axon diameter in 32 patients with FM, 15 patients with small fibers neuropathy, and 24 normal controls. They also performed nerve conduction studies of the right tibiae (motor) and sural (sensory) nerves, which showed in all cases, including FM, normal values of nerve conduction velocity, sensory nerve action potential, compound motor action potential, F-wave latencies, and distal motor latencies [63]. The same group recently confirmed normal NCS in 117 women with FM, even in patients with the extent of small fiber pathology and symptom severity [48]. A more recent study [47] described normal NCS in 81 FM patients, including those (85%) with proximal small fibers denervation.
Fibromyalgia patients complying with carpal tunnel syndrome CTS) presented with the same median nerve abnormalities as the other CTS patients [64]. Muscle fiber conduction velocity was found increased in the not painful muscles of 22 FM patients compared to 21 controls, compatible with a central dysregulation of muscular posture [65]. Caro et al. [66] retrospectively revised EMG and ENG in a cohort of 29 FM patients, 26 FM patients with associated rheumatoid arthritis, and 14 controls and found EMG and ENG abnormalities compatible with polyneuropathy in 90% of FM patients. This study is in apparent contradiction with the most of EMG and ENG results published by other groups, but it lacks a previous neurological assessment of clinical signs of systemic polyneuropathy, able to exclude FM diagnosis. Moreover, another study conducted in a considerable number of FM patients (155) showed a mild sural and medial plantar (MP) response amplitudes reduction in those subjects reporting symptoms of neuropathic pain, distal small fibers neuropathy, and markers of metabolic syndrome [67].
Summarizing, nerve conduction study and electromyography are generally within normal limits in FM patients, but their routine execution could be useful to exclude possible misdiagnosis of polyneuropathies secondary to different causes, as metabolic sufferance,
Microneurography
Microneurography provides for direct recording of unmyelinated postganglionic sympathetic or afferent C fibers, using needles inserted into a peripheral nerve fascicle [68]. Few studies are reported in FM. The first one was published in 2014 [62], comparing 30 women with FM, 17 patients with small fibers neuropathy, and 9 controls. The authors observed abnormal C nociceptors function in 23 FM patients, with increased mechanical sensitivity, possibly contributing to the pain and tenderness suffered by patients with fibromyalgia. In their study inferring multimodal neurophysiological assessment in FM patients, Evdokimov et al. [48] confirmed C fiber spontaneous activity and mechanical sensitization in FM patients. Microneurography is an invasive and technically demanding procedure, but its employment in FM could give an aid in the detection of C fiber activity and mechanism of peripheral sensitization.
Confocal microscopy
Corneal confocal bio-microscopy provides in vivo structural images of the corneal stromal nerves and the sub-basal nerve plexus. Considering the elective innervation of the cornea by C fibers, corneal confocal bio-microscopy is a reliable method to assess small nerve fiber pathology [69]. Ramirez et al. [70] found reduced stromal nerve thickness and decreased sub-basal plexus nerve density in 17 FM patients with respect to controls.
Oudejans et al. [71] measured cornea nerve fiber density, branching density, and nerve fiber length in 39 FM patients, together with clinical and QST examination. They found decreased nerve fiber length in 44% of patients and nerve fiber density and branching in 10% and 28% of patients. Considering also the QST, they individuated 4 distinct phenotypes with different combinations of peripheral involvement and central sensitization and concluded for the heterogeneity of FM. The utility of corneal confocal microscopy in FM was confirmed in the following studies, which detected abnormalities in most of the patients, frequently in association with severity of clinical expression [48, 72]. In a double-blind placebo-controlled trial with tapentadol, the presence of corneal fiber abnormalities predicted the poor therapeutic response [73].
In a more recent study, changes in corneal innervation and Langerhans cells were detected in FM patients and those with small fiber neuropathy [74]. To summarize, corneal confocal microscopy confirmed the presence of small fibers impairment in FM, though the clinical picture did not resemble neuropathic pain, especially in patients with severe anxiety and depression [75] (Table 5).
Skin biopsy
Doppler et al. [63] demonstrated a reduction of diameter in dermal nerve fibers in FM patients compared to small fiber neuropathy (SFN) patients and control subjects [63].
Impaired cutaneous innervation prevailed at proximal leg level in further published FM case series, which also displayed impaired skin miRNA homeostasis [76]. Patients with distal denervation presented with more severe dysautonomia and paresthesia when compared with patients with normal skin biopsy [77]. The subset of patients with distal leg denervation (43 among 155) presented with signs of axonal large fibers neuropathy at NCS and metabolic syndrome [67]. The presence of SFN in fibromyalgia was also associated with a more severe phenotype [48].
Our recent study conducted in 81 FM patients showed a clear prevalence of proximal small fibers denervation (85%) with 12% of cases with proximal and distal small fibers neuropathy [47]. The clinical picture and comorbidities were similar among the different skin biopsy subgroups, as well as neurophysiological signs of altered pain processing at the central level. Fasolino et al. [46] confirmed the scarce adherence of clinical profile, delineated with QST, to a classical clinical phenotype of small fibers pathology [46]. Interestingly, adolescents with FM showed distal denervation in 50% of cases [78] (Table 6).
To summarize, most of the studies confirmed a loss of epidermal fibers in FM, but many contradictory results emerged. The prevalent distribution of epidermal nerve loss is different among studies, varying from typical SFN with increased distal/proximal ratio or prevalent proximal denervation. As a matter of fact, the most of studies concurred with a clinical picture not resembling SFN.
General remarks
There are concerns against both the hypotheses of prevalent central or peripheral nervous system involvement in FM. The incredible amount of studies reporting central dysfunction in pain processing would not be conclusive to define FM as a pure central nervous system disorder. Psychiatric comorbidity is prominent in FM patients, but it could a factor facilitating central sensitization, and not the primary cause of the disease [79]. In fact, central sensitization is quite independent of the primary cause of pain, occurring in nociceptive and neuropathic pain, defined as disorders with validated nerve damage at the central or peripheral level [80]. Chronic pain that arises without evidence of actual or threatened tissue damage or evidence for disease or lesion of the somatosensory system could be included in a separate category called nociplastic pain [81]. The subgroup of FM patients without evidence of small fibers impairment fully respond to the criteria for nociplastic pain, but similar mechanisms seem to coexist in the majority of patients presenting with peripheral denervation.
In peripheral neuropathic pain, factors favoring chronic evolution could rely on maladaptive processes within the central nervous system (CNS) [82]. Some neurophysiological signs could show a tendency toward a central amplification of pain even in patients with peripheral neuropathies. Reduced habituation of laser-evoked potentials displays an abnormal central pain processing in patients with painful radiculopathies [83]. In chronic nociceptive pain, like that occurring in osteoarthritis, there is an increased sensitivity to various experimental painful stimuli compared with age-matched controls, suggesting that central sensitization phenomena could accomplish and aggravate any type of pain as a factor favoring chronic evolution [84]. In fact, defining FM as a disorder within the central sensitization spectrum [80] does not explain its origin nor attribute it to a primary CNS disorder.
On the other side, the existence of peripheral small fibers denervation would explain several symptoms of FM, including overlapping syndromes, as postural tachycardia syndrome (PoTS), and systemic exercise intolerance disorder, formerly referred to as chronic fatigue syndrome [85]. The complexity of those syndromes may vary in relation to the prevalent involvement of small sensory and autonomic fibers and the presence of a focal, generalized, length/dependent, or not length-dependent process. However, the occurrence of epidermal nerve fiber loss has been found in several conditions involving peripheral and central nervous system [86,87,88,89,90]. Small fiber pathology may be the expression of a multisystem involvement caused by the same pathophysiological mechanisms underlying the respective disease and not the first pathophysiological event. The origin of small fibers damage is still not clear. A recent hypothesis about a specific immunological activity responsible for peripheral nociceptive afferent sensitization came from an experiment in animal treated with Igg from FM patients [91]. Fasolino et al. [46] found rare variants of voltage-gated sodium channels within FM cohort, including the SCN9A variant described in small fiber neuropathy. The genetic origin of small fibers involvement should be confirmed and worthy for specific studies.
Moreover, in an animal model study on rats [92] the bilateral deliver into the insula of glutamate transport inhibitor l-trans-Pyrrolidine-2,4-dicarboxylic acid (PDC), increasing endogenous glutamate, produced a persistent increase in multimodal pain behaviors and a decrease in peripheral nerve fibers. This preclinical finding provides preliminary support to the hypothesis that insular hyperactivity may be a casual factor in the development of small fiber pathology in FM.
On the other side, studies on patients with SFN [93] highlighted the influence of peripheral nerve degeneration on the functional connectivity of the brain circuits, implicating that deprivation of small fiber sensory inputs impairs emotional and cognitive processing of pain in the limbic system.
Conclusions
In the light of the above-reported arguments, the coexistence of both peripheral and central system involvement is established, according to FM as a wide spectrum of phenotypes, varying from clinical profiles more similar to SFN to features typical for nociplastic pain. The example of FM may be also extended to other neurological diseases where the functional and anatomical changes are not confined to the peripheral or central districts. Moreover, the complex interaction between central and peripheral factors is opening a new scenario about the management of many neurological disorders.
The first unresolved issue is the primary origin of FM, if peripheral or central. Whether non-length-dependent SFN is an initiating event leading to FM, or is the consequence of stress-related insular hyperexcitability, remains unclear. Mild sufferance of peripheral afferents, probably genetically or immunologically determined, could function as a trigger for an exaggerated response of the so-called “salience matrix” in predisposed individuals. A common genetic field could thus explain the peripheral mild denervation and the cortical hyperexcitability. On the other side, the intriguing hypothesis rising from animal models could indicate that the cortical hyperfunction could cause peripheral small afferent damage. The research should go on the genetic or immunological origin of such peripheral and central abnormalities, the acquired facilitating factors, and the presence of different phenotypes in order to search for efficacious treatments, which are still lacking [94]. A careful neurological examination, taking into consideration signs of central sensitization, psychopathological features, and autonomic involvement, could be mandatory. Routine screening for SFN may thus be useful at least for the recognition of treatable causes [76], and to look for further treatment strategies, and possible factors predicting response to current available drugs.
Data availability
Not applicable.
Code availability
Not applicable.
References
Mikkelsson M, Latikka P, Kautiainen H et al (1992) Muscle and bone pressure pain threshold and pain tolerance in fibromyalgia patients and controls. Arch Phys Med Rehabil 73:814–818
Kosek E,9 Ekholm J, Hansson P. (1995) Increased pressure pain sensibility in fibromyalgia patients is located deep to the skin but not restricted to muscle tissue. Pain. Dec;63(3):335–339. doi: https://doi.org/10.1016/0304-3959(95)00061-5.
Staud R (2011) Brain imaging in fibromyalgia syndrome. Clin Exp Rheumatol 29(6 Suppl 69):S109–S117
Wolfe F, Smythe HA, Yunus MB, et al. (1990) The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis and Rheumatism. Feb;33(2):160–72. https://doi.org/10.1002/art.1780330203
Staud R (2011) Peripheral pain mechanisms in chronic widespread pain. Best Pract Res Clin Rheumatol. Apr;25(2):155–64. https://doi.org/10.1016/j.berh.2010.01.010
Yunus MB (2015) (2015) Editorial review: an update on central sensitivity syndromes and the issues of nosology and psychobiology. Curr Rheumatol Rev 11(2):70–85
Wolfe F, Clauw DJ, Fitzcharles MA et al (2010) The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res 62:600–610. https://doi.org/10.1002/acr.20140
Grayston R, Czanner G, Elhadd K et al (2019) A systematic review and meta-analysis of the prevalence of small fiber pathology in fibromyalgia: implications for a new paradigm in fibromyalgia etiopathogenesis. Semin Arthritis Rheum 48(5):933–940. https://doi.org/10.1016/j.semarthrit.2018.08.003
Wolfe F, Walitt B (2013) Culture, science and the changing nature of fibromyalgia. Nat Rev Rheumatol 9(12):751–755
Palmer S, Bailey J, Brown C, Jones A, McCabe CS (2019) Sensory function and pain experience in arthritis, complex regional pain syndrome, fibromyalgia syndrome, and pain-free volunteers: a cross-sectional study. Clin J Pain 35(11):894–900
Gracely Rh, Petzke F, Wolf JM, Clauw DJ (2002) Functional magnetic resonance imaging evidence of augmented pain processing in fibromyalgia. Arthritis Rheum 46:1333–1343. https://doi.org/10.1002/art.10225
Williams DA, Gracely RH (2006) Biology and therapy of fibromyalgia. Functional magnetic resonance imaging findings in fibromyalgia. Arthritis Res Ther. 8(6):224.
Burgmer M, Pfleiderer B, Maihöfner C, Gaubitz M, Wessolleck E, Heuft G, Pogatzki-Zahn E (2012) Cerebral mechanisms of experimental hyperalgesia in fibromyalgia. Eur J Pain 16(5):636–647. https://doi.org/10.1002/j.1532-2149.2011.00058.x
Craggs JG, Staud R, Robinson ME, Perlstein WM, Price DD (2012) Effective connectivity among brain regions associated with slow temporal summation of C-fiber-evoked pain in fibromyalgia patients and healthy controls. J Pain 13(4):390–400. https://doi.org/10.1016/j.jpain.2012.01.002
Pujol J, Macià D, Garcia-Fontanals A, Blanco-Hinojo L, López-Solà M, Garcia-Blanco S, Poca-Dias V, et al. (20 The contribution of sensory system functional connectivity reduction to clinical pain in fibromyalgia. Pain. 155(8):1492–1503.
Bosma RL, Mojarad EA, Leung L, Pukall C, Staud R, Stroman PW (2016) FMRI of spinal and supra-spinal correlates of temporal pain summation in fibromyalgia patients. Hum Brain Mapp 37(4):1349–1360
Schreiber KL, Loggia ML, Kim J, Cahalan CM, Napadow V, Edwards RR (2017) Painful after-sensations in fibromyalgia are linked to catastrophizing and differences in brain response in the medial temporal lobe. J Pain 18(7):855–867. https://doi.org/10.1016/j.jpain.2017.02.437
Ellingson LD, Stegner AJ, Schwabacher IJ, Lindheimer JB, Cook DB (2018) Catastrophizing interferes with cognitive modulation of pain in women with fibromyalgia. Pain Med 19(12):2408–2422. https://doi.org/10.1093/pm/pny008
Sandström A, Ellerbrock I, Tour J, Kadetoff D, Jensen KB, Kosek E (2020) Neural correlates of conditioned pain responses in fibromyalgia subjects indicate preferential formation of new pain associations rather than extinction of irrelevant ones. Pain 161(9):2079–2088
Hubbard CS, Lazaridou A, Cahalan CM, Kim J, Edwards RR, Napadow V, Loggia ML (2020) Aberrant salience? Brain hyperactivation in response to pain onset and offset in fibromyalgia. Arthritis Rheumatol 72(7):1203–1213. https://doi.org/10.1002/art.41220
Truini A, Tinelli E, Gerardi MC, Calistri V, Iannuccelli C, La Cesa S, Tarsitani L, Mainero C, Sarzi-Puttini P, Cruccu G, Caramia F, Di Franco M (2016) Abnormal resting state functional connectivity of the periaqueductal grey in patients with fibromyalgia. Clin Exp Rheumatol 34(2 Suppl 96):S129–S133 PMID: 27157397
Coulombe MA, St Lawrence K, Moulin DE, Morley-Forster P, Shokouhi M, Nielson WR, Davis KD (2017) Lower functional connectivity of the periaqueductal gray is related to negative affect and clinical manifestations of Front Neuroanat 11:47. https://doi.org/10.3389/fnana.2017.00047
Harper DE, Ichesco E, Schrepf A, Hampson JP, Clauw DJ, Schmidt-Wilcke T, Harris RE, Harte SE (2018) Resting functional connectivity of the periaqueductal gray is associated with normal inhibition and pathological facilitation in conditioned pain modulation. J Pain 19(6):635.e1-635.e15. https://doi.org/10.1016/j.jpain.2018.01.001
Čeko M, Frangos E, Gracely J, Richards E, Wang B, Schweinhardt P, Catherine Bushnell M (2020) Default mode network changes in fibromyalgia patients are largely dependent on current clinical pain. Neuroimage 1(216):116877. https://doi.org/10.1016/j.neuroimage.2020.116877
Ichesco E, Puiu T, Hampson JP, Kairys AE, Clauw DJ, Harte SE, Peltier SJ, Harris RE, Schmidt-Wilcke T (2016) Altered fMRI resting-state connectivity in individuals with fibromyalgia on acute pain stimulation. Eur J Pain 20(7):1079–1089. https://doi.org/10.1002/ejp.832
Jarrahi B, Martucci KT, Nilakantan AS, Mackey S (2017) Investigating the BOLD spectral power of the intrinsic connectivity networks in fibromyalgia patients: a resting-state fMRI study. Annu Int Conf IEEE Eng Med Biol Soc 2017:497–500
Jarrahi B, Martucci KT, Nilakantan AS, Mackey S (2018) Cold water pressor test differentially modulates functional network connectivity in fibromyalgia patients compared with healthy controls. Annu Int Conf IEEE Eng Med Biol Soc 2018:578–582
López-Solà M, Woo CW, Pujol J, Deus J, Harrison BJ, Monfort J, Wager TD (2017) Towards a neurophysiological signature for fibromyalgia. Pain 158(1):34–47
Kaplan CM, Schrepf A, Vatansever D, Larkin TE, Mawla I, Ichesco E, Kochlefl L, Harte SE, Clauw DJ, Mashour GA, Harris RE (2019) Functional and neurochemical disruptions of brain hub topology in chronic pain. Pain 160(4):973–983
Ledermann K, Jenewein J, Sprott H, Hasler G, Schnyder U, Warnock G, Johayem A, Kollias S, Buck A, Martin C (2016) Relation of dopamine receptor 2 binding to pain perception in female fibromyalgia patients with and without depression--A [11C] racloprid Eur Neuropsychopharmacol. 26(2):320–330. https://doi.org/10.1016/j.euroneuro.2015.12.007
Pomares FB, Roy S, Funck T, Feier NA, Thiel A, Fitzcharles MA, Schweinhardt P (2020) Upregulation of cortical GABAA receptor concentration in fibromyalgia. Pain 161(1):74–82
Albrecht DS, Forsberg A, Sandström A, Bergan C, Kadetoff D, Protsenko E, Lampa J, Lee YC, Höglund CO, Catana C, Cervenka S, Akeju O, Lekander M, Cohen G, Halldin C, Taylor N, Kim M, Hooker JM, Edwards RR, Napadow V, Kosek E, Loggia ML (2018) Brain glial activation in fibromyalgia - a multi-site positron emission tomography investigation. Brain Behav Immun 75:72–83. https://doi.org/10.1016/j.bbi.2018.09.018
Üçeyler N, Buchholz HG, Kewenig S, Ament SJ, Birklein F, Schreckenberger M, Sommer C (2020) Cortical binding potential of opioid receptors in patients with fibromyalgia syndrome and reduced systemic interleukin-4 levels - a pilot study. Front Neurosci 14:512. https://doi.org/10.3389/fnins.2020.00512
Cagnie B, Coppieters I, Denecker S, Six J, Danneels L, Meeus M (2014) Central sensitization in fibromyalgia? A systematic review on structural and functional brain MRI. Semin Arthritis Rheum 44(1):68–75. https://doi.org/10.1016/j.semarthrit.2014.01.001
Kim H, Kim J, Loggia ML, Cahalan C, Garcia RG, Vangel MG, Wasan AD, Edwards RR, Napadow V (2015) Fibromyalgia is characterized by altered frontal and cerebellar structural covariance brain networks. Neuroimage Clin 7:667–677. https://doi.org/10.1016/j.nicl.2015.02.022
Robinson ME, O’Shea AM, Craggs JG, Price DD, Letzen JE, Staud R (2015) Comparison of machine classification algorithms for fibromyalgia: neuroimages versus self-report. J Pain 16(5):472–477
Sundermann B, Nayyeri MD, Pfleiderer B, Stahlberg K, Jünke L, Baie L, Dieckmann R, Liem D, Happe T, Burgmer M (2019) Subtle changes of gray matter volume in fibromyalgia reflect chronic musculoskeletal pain rather than disease-specific effects. Eur J Neurosci 50(12):3958–3967. https://doi.org/10.1111/ejn.14558
McCrae CS, O’Shea AM, Boissoneault J, Vatthauer KE, Robinson ME, Staud R, Perlstein WM, Craggs JG (2015) Fibromyalgia patients have reduced hippocampal volume compared with healthy controls. J Pain Res 30(8):47–52. https://doi.org/10.2147/JPR.S71959
Feraco P, Nigro S, Passamonti L, Grecucci A, Caligiuri ME, Gagliardo C, Bacci A (2020) Neurochemical correlates of brain atrophy in fibromyalgia syndrome: a magnetic resonance spectroscopy and cortical thickness study. Brain Sci 10(6):395. https://doi.org/10.3390/brainsci10060395
Gibson SJ, Littlejohn GO, Gorman MM, Helme RD, Granges G (1994) Altered heat pain thresholds and cerebral event-related potentials following painful CO2 laser stimulation in subjects with fibromyalgia syndrome. Pain 58(2):185–193
de Tommaso M, Federici A, Santostasi R et al (2011) Laser-evoked potentials habituation in fibromyalgia. J Pain 12(1):116–124. https://doi.org/10.1155/2017/9747148
de Tommaso M (2008) Laser-evoked potentials in primary headaches and cranial neuralgias. Expert Rev Neurother 8(9):1339–1345. https://doi.org/10.1586/14737175.8.9.1339
de Tommaso M, Ambrosini A, Brighina F et al (2014) Altered processing of sensory stimuli in patients with migraine. Nat Rev Neurol 10(3):144–155
Üçeyler N, Zeller D, Kahn AK, Kewenig S, Kittel-Schneider S, Schmid A, Casanova-Molla J, Reiners K, Sommer C (2013) Small fiber pathology in patients with fibromyalgia syndrome. Brain 136(Pt 6):1857–1867. https://doi.org/10.1093/brain/awt053
Van Assche DCF, Plaghki L, Masquelier E, Hatem SM (2020) Fibromyalgia syndrome-a laser-evoked potentials study unsupportive of small nerve fibre involvement. Eur J Pain 24(2):448–456. https://doi.org/10.1002/ejp.1501
Fasolino A, Di Stefano G, Leone C, Galosi E, Gioia C, Lucchino B, Terracciano A, Di Franco M, Cruccu G, Truini A (2020) Small-fibre pathology has no impact on somatosensory system function in patients with fibromyalgia. Pain 161(10):2385–2393
Vecchio E, Lombardi R, Paolini M, Libro G, Delussi M, Ricci K, Quitadamo SG, Gentile E, Girolamo F, Iannone F, Lauria G, de Tommaso M (2020) Peripheral and central nervous system correlates in fibromyalgia. Eur J Pain. 6(1).
Evdokimov D, Frank J, Klitsch A, Unterecker S, Warrings B, Serra J, Papagianni A, Saffer N, Altenschildesche MZ, C, Kampik D, Malik RA, Sommer C, Üçeyler N, (2019) Reduction of skin innervation is associated with a severe fibromyalgia phenotype. Ann Neurol 86(4):504–516. https://doi.org/10.1002/ana.25565
de Tommaso M, Santostasi R, Devitofrancesco V, Franco G, Vecchio E, Delussi M, Livrea P, Katzarava Z (2011) A comparative study of cortical responses evoked by transcutaneous electrical vs CO(2) laser stimulation. Clin Neurophysiol 122(12):2482–2487. https://doi.org/10.1016/j.clinph.2011.05.006
González-Roldán AM, Cifre I, Sitges C, Montoya P (2016) Altered dynamic of EEG oscillations in fibromyalgia patients at rest. Pain Med 17(6):1058–1068. https://doi.org/10.1093/pm/pnw023
Pascual-Marqui RD, Esslen M, Kochi K, Lehmann D (2002) Functional imaging with low-resolution brain electromagnetic tomography (LORETA): a review. Methods Find Exp Clin Pharmacol 24(suppl C):91–95
Vanneste S, Ost J, Van Havenbergh T, De Ridder D (2017) Resting state electrical brain activity and connectivity in fibromyalgia. PLoS ONE 12(6):e0178516. https://doi.org/10.1371/journal.pone.0178516
Fallon N, Chiu Y, Nurmikko T, Stancak A (2018) Altered theta oscillations in resting EEG of fibromyalgia syndrome patients. Eur J Pain 22(1):49–57. https://doi.org/10.1002/ejp.1076
Choe MK, Lim M, Kim JS, Lee DS, Chung CK (2018) Disrupted resting state network of fibromyalgia in theta frequency. Sci Rep 8(1):2064
González-Villar AJ, Triñanes Y, Gómez-Perretta C, Carrillo-de-la-Peña MT (2010) Patients with fibromyalgia show increased beta connectivity across distant networks and microstates alterations in resting-state electroencephalogram. Neuroimage. https://doi.org/10.1016/j.neuroimage.2020.117266
Ploner M, Sorg C, Gross J (2017) Brain rhythms of pain. Trends Cogn Sci 21(2):100–110. https://doi.org/10.1016/j.tics.2016.12.001
Uceyler N, Zeller D, Kahn AK, Kewenig S, Kittel-Schneider S, Schmid A, Sommer C (2013) Small fibre pathology in patients with fibromyalgia syndrome. Brain 136(6):1857–1867. https://doi.org/10.1093/brain/awt053
Oaklander AL, Klein MM (2013) Evidence of small-fiber polyneuropathy in unexplained, juvenile-onset, widespread pain syndromes. Pediatrics 131(4):e1091–e1100. https://doi.org/10.1542/peds.2012-2597
de Tommaso M, Nolano M, Iannone F, Vecchio E, Ricci K, Lorenzo M, Delussi M, Girolamo F, Lavolpe V, Provitera V, Stancanelli A, Lapadula G, Livrea P (2014) Update on laser-evoked potential findings in fibromyalgia patients in light of clinical and skin biopsy features. J Neurol 261(3):461–472
Giannoccaro MP, Donadio V, Incensi A, Avoni P, Liguori R (2014) Small nerve fiber involvement in patients referred for fibromyalgia. Muscle Nerve 49(5):757–759. https://doi.org/10.1002/mus.24156
Kosmidis ML, Koutsogeorgopoulou L, Alexopoulos H et al (2014) Reduction of intraepidermal nerve fiber density (IENFD) in the skin biopsies of patients with fibromyalgia: a controlled study. J Neurol Sci 347(1–2):143–147. https://doi.org/10.1016/j.jns.2014.09.035
Serra J, Collado A, Solà R, Antonelli F, Torres X, Salgueiro M, Quiles C, Bostock H (2014) Hyperexcitable C nociceptors in fibromyalgia. Ann Neurol 75(2):196–208
Doppler K, Rittner HL, Deckart M, Sommer C (2015) Reduced dermal nerve fiber diameter in skin biopsies of patients with fibromyalgia. Pain 156(11):2319–2325
Solmaz V, Yavuz S, İnanr A, Aksoy D, Pektaş E, Tekataş A, Kurt SG (2017) Investigation of nerve conduction studies of carpal tunnel syndrome cases with different risk factors: an electrodiagnostic study. J Clin Neurophysiol 34(2):139–143
Klaver-Krol EG, Rasker JJ, Klaver MM, Ten Klooster PM, Zwarts MJ (2019) Fibromyalgia: increased reactivity of the muscle membrane and a role of central regulation. Clin Neurophysiol 130(1):12–19
Caro XJ, Galbraith RG, Winter EF (2018) Evidence of peripheral large nerve involvement in fibromyalgia: a retrospective review of EMG and nerve conduction findings in 55 FM subjects. Eur J Rheumatol 5(2):104–110
Lawson VH, Grewal J, Hackshaw KV, Mongiovi PC, Stino AM (2018) Fibromyalgia syndrome and small fiber, early or mild sensory polyneuropathy. Muscle Nerve 58(5):625–630. https://doi.org/10.1002/mus.26131
Donadio V, Liguori R (2015) Microneurographic recording from unmyelinated nerve fibers in neurological disorders: an update. Clin Neurophysiol 126(3):437–445. https://doi.org/10.1016/j.clinph.2014.10.009
Tavakoli M, Marshall A, Pitceathly R, Fadavi H, Gow D, Roberts ME et al (2010) () Corneal confocal microscopy: a novel means to detect nerve fibre damage in idiopathic small fibre neuropathy. Exp Neurol 223:245–250. https://doi.org/10.1016/j.expneurol.2009.08.033
Ramirez M, Martinez-Martinez LA, Hernandez-Quintela E, Velazco-Casapia J, Varga A & Martinez-Lavin M (2015). Small fiber neuropathy in women with fibromyalgia. An in vivo assessment using corneal confocal bio-microscopy. Semin Arthritis Rheum, 45(2), 214–219. https://doi.org/10.1016/j.semarthrit.2015.03.003
Oudejans L, He X, Niesters M, Dahan A, Brines M, van Velzen M (2016) Cornea nerve fiber quantification and construction of phenotypes in patients with fibromyalgia. Sci Rep 6:23573
Erkan Turan K, Kocabeyoglu S, Unal-Cevik I, Bezci F, Akinci A, Irkec M (2018) Ocular surface alterations in the context of corneal in vivo confocal microscopic characteristics in patients with fibromyalgia. Cornea 37(2):205–210
van de Donk T, van Velzen M, Dahan A (2019) Niesters M (2019) Cornea nerve fibre state determines analgesic response to tapentadol in fibromyalgia patients without effective endogenous pain modulation. Eur J Pain 23(9):1586–1595. https://doi.org/10.1002/ejp.1435
Klitsch A, Evdokimov D, Frank J, Thomas D, Saffer N, Altenschildesche MZ, C, Sisignano M, Kampik D, Malik RA, Sommer C, Üçeyler N, (2020) Reduced association between dendritic cells and corneal sub-basal nerve fibers in patients with fibromyalgia syndrome. J Peripher Nerv Syst 25(1):9–18. https://doi.org/10.1111/jns.12360
Ramírez M, Guerra-Juárez A, Miyake DY, Sebastian-Arellano C, Estrada-Mata AG, González-Moyotl NJ, Rodríguez-Aguayo AM, Martínez-Lavin M, Martínez-Martínez LA (2020) Correlation between corneal nerve density and symptoms of small fiber neuropathy in patients with fibromyalgia: the confounding role of severe anxiety or depression. J Clin Rheumatol. 10.
Leinders M, Doppler K, Klein T, Deckart M, Rittner H, Sommer C, Üçeyler N (2016) Increased cutaneous miR-let-7d expression correlates with small nerve fiber pathology in patients with fibromyalgia syndrome. Pain 157(11):2493–2503
Lodahl, M., Treister, R., & Oaklander, A. L. (2018). Specific symptoms may discriminate between fibromyalgia patients with vs without objective test evidence of small-fiber polyneuropathy. Pain Rep 3(1):e633
Boneparth A, Chen S, Horton DB, Moorthy LN, Farquhar I, Downs HM, Lee H, Oaklander AL (2020). Epidermal neurite density in skin biopsies from patients whith juvenile fibromyalgia. J Rheumatol. 15:jrheum.200378. https://doi.org/10.3899/jrheum.200378
Kleykamp BA, Ferguson MC, McNicol E, Bixho I, Arnold LM, Edwards RR et al (2021) The prevalence of psychiatric and chronic pain comorbidities in fibromyalgia: an ACTTION systematic review. Semin Arthritis Rheum 51(1):166–174. https://doi.org/10.1016/j.semarthrit.2020.10.006
Arendt-Nielsen L, Morlion B, Perrot S et al (2018) Assessment and manifestation of central sensitisation across different chronic pain conditions. Eur J Pain 22(2):216–241. https://doi.org/10.1002/ejp.1140
Aydede M, Shriver A (2018) Recently introduced definition of “nociplastic pain” by the International Association for the Study of Pain needs better formulation. Pain 159(6):1176–1177
Meacham K, Shepherd A, Mohapatra DP, Haroutounian S. (2017) Neuropathic pain: central vs. peripheral mechanisms. Curr Pain Headache Rep. 21(6):28. https://doi.org/10.1007/s11916-017-0629-5
Hüllemann P, von der Brelie C, Manthey G et al (2017) Reduced laser-evoked potential habituation detects abnormal central pain processing in painful radiculopathy patients. Eur J Pain 21(5):918–926. https://doi.org/10.1002/ejp.994
Lee, Y.C., Lu, B., Bathon, J.M., Haythornthwaite, J.A., Smith, M.T, Page GG, Edwards RR (2011). Pain sensitivity and pain reactivity in osteoarthritis. Arthritis Care Res (Hoboken)63, 320–327. https://doi.org/10.1002/acr.20373
Martinez-Lavin M (2018) Fibromyalgia and small fiber neuropathy: the plot thickens! Clin Rheumatol 37(12):3167–3171
Nolano M, Manganelli F, Provitera V et al (2015) Small nerve fiber involvement in CMT1A. Neurology 84(4):407–414. https://doi.org/10.1212/WNL.0000000000001188
Nolano M, Provitera V, Crisci C et al (2001) Small fibers involvement in Friedreich’s ataxia. Ann Neurol 50(1):17–25. https://doi.org/10.1002/ana.1283
Nolano M, Provitera V, Donadio V et al (2016) Cutaneous sensory and autonomic denervation in CADASIL. Neurology 86(11):1039–1044. https://doi.org/10.1212/WNL.0000000000002468
Nolano M, Provitera V, Estraneo A et al (2008) Sensory deficit in Parkinson’s disease: evidence of a cutaneous denervation. Brain 131(Pt 7):1903–1911. https://doi.org/10.1093/brain/awn102
Nolano M, Provitera V, Manganelli F et al (2017) Non-motor involvement in amyotrophic lateral sclerosis: new insight from nerve and vessel analysis in skin biopsy. Neuropathol Appl Neurobiol 43(2):119–132. https://doi.org/10.1111/nan.12332
Goebel A, Krock E, Gentry C, Israel MR, Jurczak A, Urbina CM, et al. (2021) Passive transfer of fibromyalgia symptoms from patients to mice. J Clin Invest. 1;131(13):e144201. doi: https://doi.org/10.1172/JCI144201.
Harte SE, Clauw DJ, Hayes JM, Feldman EL, St Charles IC & Watson CJ (2017) Reduced intraepidermal nerve fiber density after a sustained increase in insular glutamate: a proof-of-concept study examining the pathogenesis of small fiber pathology in fibromyalgia. Pain Rep, 2(3), e590.
Hsieh PC, Tseng MT, Chao CC, Lin YH, Tseng WI, Liu KH et al (2015) (2015) Imaging signatures of altered brain responses in small-fiber neuropathy: reduced functional connectivity of the limbic system after peripheral nerve degeneration. Pain 156(5):904–916. https://doi.org/10.1097/j.pain.0000000000000128
Macfarlane GJ, Kronisch C, Dean LE et al (2017) EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis 76(2):318–328. https://doi.org/10.1136/annrheumdis-2016-209724
Funding
There are no specific funds for this submission
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
None.
Consent to participate (include appropriate statements)
Not applicable.
Consent for publication (include appropriate statements)
Not applicable.
Conflict of interest/Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Tommaso, M., Vecchio, E. & Nolano, M. The puzzle of fibromyalgia between central sensitization syndrome and small fiber neuropathy: a narrative review on neurophysiological and morphological evidence. Neurol Sci 43, 1667–1684 (2022). https://doi.org/10.1007/s10072-021-05806-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05806-x