Abstract
Introduction
Hereditary transthyretin amyloidosis with polyneuropathy (ATTRv-PN) remains a diagnostic challenge due to clinical, neurophysiological, and laboratory findings suggestive of other diagnoses, particularly chronic inflammatory demyelinating polyneuropathy (CIDP). In this cross-sectional prospective study, we aimed to investigate the utility of high-resolution ultrasonography of peripheral nerves as a diagnostic tool to differentiate ATTRv-PN from CIDP.
Methods
In 11 treatment-naive patients with genetically confirmed late-onset ATTRv-PN and 25 patients with CIDP, we collected clinical, electrodiagnostic, and high-resolution ultrasonography data of the peripheral nerves. In each patient, we used high-resolution ultrasonography to assess 26 nerve sites.
Results
Of the 11 patients with ATTRv-PN, two had electrodiagnostic study data compatible with a CIDP diagnosis. High-resolution ultrasonography showed that the cross-sectional area of the brachial plexus, median nerve at the axilla, arm, and forearm, ulnar nerve at the forearm, and peroneal nerve at the popliteal fossa were significantly smaller in the 11 ATTRv-PN patients than in CIDP patients. However, in the two patients with electrodiagnostic study data compatible with a CIDP diagnosis, high-resolution nerve ultrasonography data were comparable to those in patients with CIDP.
Conclusion
Although high-resolution ultrasonography of peripheral nerves provides reliable information in patients with ATTRv-PN, its usefulness as a standalone diagnostic tool to differentiate ATTRv-PN from CIDP might be limited.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hereditary transthyretin amyloidosis with polyneuropathy (ATTRv-PN) due to TTR gene mutations is a rare autosomal dominant disease with an estimated prevalence of 1/1,000,000 [1]. In endemic areas, ATTRv-PN usually presents as an early-onset length-dependent sensorimotor neuropathy with autonomic involvement associated with positive family history [2]. In non-endemic areas, ATTRv-PN is frequently associated with late onset, male predominance, early large fibre involvement with mild autonomic impairment, and often no family history [3, 4]. ATTRv-PN therefore manifests with a wide variety of clinical presentations, ranging from conventional length-dependent neuropathy to a non-length-dependent distribution of symptoms and signs. In patients with clinical evidence of non-length-dependent neuropathy distribution, occasional findings of demyelinating features on nerve conduction studies, albuminocytological dissociation on cerebrospinal fluid examination, and the lack of amyloid deposition in tissue biopsies may lead to misdiagnosis with demyelinating neuropathies, such as chronic inflammatory demyelinating polyneuropathy (CIDP) [5,6,7]. Misdiagnosis of late-onset ATTRv-PN is one of the main causes of diagnostic delay. Diagnostic delay ranges from 3 to 5 years, a significant amount of time considering the average survival of 6–12 years from symptom onset [8] and the recent availability of effective disease-modifying treatment options [2].
High-resolution ultrasound (HRUS) of peripheral nerves is a non-invasive, radiation-free, and easy-to-perform technique, and is currently considered a useful tool to support the diagnosis of peripheral neuropathies [9, 10]. In patients with CIDP [11, 12], HRUS commonly shows an increase in the nerve cross-sectional area (CSA) at non-entrapment sites, predominantly proximal sites. Similarly, nerve CSA enlargement at proximal sites has been reported in patients with ATTRv-PN [13,14,15,16,17].
Limited information is currently available on how HRUS findings might contribute to the diagnosis of late-onset ATTRv-PN and whether these abnormalities might be useful to distinguish between ATTRv-PN and CIDP. More information on HRUS abnormalities in patients with ATTRv-PN may reduce diagnostic delay and hasten the administration of effective disease-modifying treatment options [2].
In this cross-sectional prospective study, we used HRUS of peripheral nerves to identify specific HRUS abnormalities in patients with ATTRv-PN and CIDP and verify whether these abnormalities may help distinguish the two peripheral neuropathies.
Methods
Patients
In this prospective study, we included consecutive patients with a genetically confirmed diagnosis of ATTRv-PN and patients with CIDP attending the Neuromuscular and Rare Disease Centre of Sant’Andrea Hospital, Rome from February 2015 to February 2020. We diagnosed ATTRv-PN based on symptoms or signs and nerve conduction study abnormalities in association with genetic test confirmation (Val30Met and non-Val30Met mutations of the TTR gene). We diagnosed CIDP according to the criteria of the European Federation of Neurological Societies (EFNS) and Peripheral Nerve Society (PNS) [18]. Exclusion criteria were age under 18 years, central nervous system disease, cognitive disturbances, or psychiatric disorders as assessed with clinical history and examination. Neuropathies other than ATTRv-PN and CIDP were excluded through a complete clinical and laboratory assessment [19]. All patients underwent an extensive electrodiagnostic investigation, including motor and sensory conduction study of median, ulnar, sural, peroneal, and tibial nerves. Based on electrodiagnostic study findings and EFNS/PNS criteria, peripheral neuropathy was classified as “neuropathy with” or “without demyelinating features” [18]. Disease severity was assessed in all patients by Medical Research Council (MRC)-80 and polyneuropathy disability (PND) scores. MRC-80 was calculated by summing the MRC score of arm abductors, elbow flexors, wrist extensors, first dorsal interosseous, hip flexors, knee extensors, foot dorsiflexors, and the extensor hallucis longus on both sides. PND was scored as stage 0: no impairment; stage I: sensory disturbances but preserved walking capability; stage II: impaired walking capability but ability to walk without a stick or crutches; stage IIIA: walking only with the help of one stick or crutch; stage IIIB: walking with the help of two sticks or crutches; and stage IV: confined to a wheelchair or bedridden [4]. In ATTRv-PN patients, we assessed the Neuropathy Impairment Score (NIS). NIS was calculated by the composite score of clinical impairments (weakness, reflex loss, and sensory loss) of 37 neuromuscular items on both sides, with a higher score indicating greater impairment [20]. A historical cohort of healthy subjects enrolled from our working facilities were used as normal controls to collect normative ranges of nerve CSA [11]. These CSA normative ranges were used to identify CSA abnormalities in the two groups of patients.
The study was approved by the local institutional review board. Written informed consent to participate was obtained from all participants.
Ultrasound evaluation
HRUS (General Electric Voluson E6 imaging system, GE Healthcare, Waukesha, WI, broadband linear transducer with frequency band 10–18 MHz), clinical assessment, and electrodiagnostic investigation were performed the same day. Three operators (ADP, GDP, and LL) blinded to clinical and neurophysiological examinations performed HRUS, while a fourth operator (LF) collected and matched the clinical records and HRUS data. In each patient, we investigated the nerve CSA of 26 nerve sites. The brachial plexus, median, ulnar, and peroneal nerves were scanned on both sides at the supraclavicular space, axilla, arm, elbow, forearm, wrist, popliteal fossa, and fibular head. Quantitative evaluation consisted of CSA measurement at the largest nerve point using the ellipse technique, or area tracing when the nerve had an irregular shape. For each patient, we considered a total number of nerve segment alterations calculated as the numerical sum of the detected enlarged sites considering plexus, axilla, arm, forearm, and popliteal fossa bilaterally. Nerve CSA at common entrapment sites (ulnar nerve at the elbow, ulnar and median nerves at the wrist, and peroneal nerve at the fibular head) was excluded from the assessment of the total number of nerve segments alterations to avoid confounding factors. To provide as objective an assessment as possible, we did not consider nerve trunk echogenicity in statistical analysis. Power Doppler sonography quantifying nerve vascularization was not performed.
Statistical analysis
In the statistical analysis, we considered each scanned segment on its own. Since most variables had a non-normal distribution, as assessed with the Kolmogorov-Smirnov test, we used non-parametric tests.
Correlation between clinical variables (disease duration, MRC-80, PND, NIS) and the total number of nerve segments with HRUS alterations was assessed by Spearman’s test. We used the chi-square test to estimate frequency distribution differences in ordinal variables, and the Mann-Whitney test to assess differences in continuous variables between the two groups of patients. Two-sided p values were considered significant if <0.05 in all the analyses. We used GraphPad Prism 8.4 (GraphPad Software, Inc., San Diego, CA) for statistical analysis.
Results
Characteristics of ATTRv-PN patients
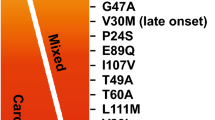
We included 11 patients with ATTRv-PN (8 males, 3 females) aged from 62 to 76 years (median 68 years, interquartile range (IQR) 67–75). Age at disease onset ranged from 60 to 73 years (median 65.5 years, IQR 61.5–72), while age at diagnosis ranged from 61 to 75 years (median 66.5 years, IQR 63.5–72). Disease duration ranged from 2 to 5 years (median 4 years, IQR 3–5). All patients were treatment naïve. Six patients were scored as PND stage I (n 3, 4, 5, 8, 9, 11), while 5 were scored as PND stage II (n 1, 2, 6, 7, 10). MRC-80 ranged from 56 to 80 (median 70, IQR 70–78), NIS ranged from 0 to 79.25 (median 43, IQR 0–55.25) (Table 1).
Although electrodiagnostic study showed that several patients had isolated or multiple abnormalities compatible with demyelination (i.e. slowed motor conduction velocity, delayed F-wave, compound motor action potential dispersion), these abnormalities fulfilled CIDP diagnostic criteria in only two patients.
Regardless of electrodiagnostic study findings, nerve CSA of median and ulnar nerves at the axilla and arm was significantly larger in patients than in healthy controls (p<0.001), while it was similar in patients and healthy controls at the forearm, both at median (p=0.959) and ulnar nerves (p=0.829), and larger in healthy controls than patients at the peroneal nerve at popliteal fossa (p=0.047). Out of the 11 patients with ATTRv-PN, 10 had quantitative HRUS abnormalities in a number of segments, ranging from 1 to 15 (median 2.5, IQR 1.7–5). Most patients had CSA abnormalities at proximal (three patients at the brachial plexus, seven at the median nerve at the axilla, seven at the median nerve at the arm, five at the median nerve at the elbow, two at the ulnar nerve at the axilla, four at the ulnar nerve at the arm) and entrapment sites (seven patients at the median nerve at the wrist, four at the ulnar nerve at the elbow, one at the ulnar nerve at the wrist, three at the peroneal nerve at the fibular head) (Table 2). One patient showed CSA changes of the median nerve at the carpal tunnel only. CSA changes occurred at distal sites of the median nerve (forearm) in two patients, one with demyelinating and another with non-demyelinating features as assessed with electrodiagnostic study (Fig. 1) (Table 3).
Nerve CSA, at non-entrapment points, was inversely correlated with MRC-80 (R=−0.265, p<0.001) and showed a positive correlation with NIS (R=0.298, p<0.001). We did not find any correlation between HRUS CSA and PND score.
Characteristics of CIDP patients
We included 25 patients with CIDP (17 males, 8 females) aged from 38 to 82 years (median 63 years, IQR 49.5–69.5). Disease duration ranged from 2 to 12 years (median 6 years, IQR 2–9). Patients were scored as PND stage I (14 patients), stage II (9 patients), or stage III (2 patients). MRC-80 ranged from 50 to 80 (median 76, IQR 65.5–78).
Eighteen patients had a chronic progressive disease course, while seven had a relapsing-remitting course. Fifteen patients were under immunomodulatory (8 prednisone, 6 intravenous immunoglobulin) or immunosuppressive (1 azathioprine) treatment, while 10 patients were not taking any specific disease-modifying treatment (8 were treatment naïve, 2 had been previously treated with intravenous immunoglobulin).
Nerve CSA was significantly higher in patients than in healthy controls at all non-entrapment points (median nerve at the axilla, arm, and forearm, ulnar nerve at the axilla and arm, peroneal nerve at the popliteal fossa, and ulnar nerve at the forearm p<0.01).
All patients except one had HRUS abnormalities of at least one nerve segment. The number of nerve segments with HRUS abnormalities ranged from 2 to 21 (median 11, IQR 6–15) in each patient. HRUS alterations occurred in most patients at proximal sites (41.3%). Around one-third of scanned upper limb nerve segments at entrapment sites were abnormal (Table 3).
Comparison of HRUS characteristics between ATTRv-PN and CIDP patients
Although patients with ATTRv-PN were older than patients with CIDP (p=0.01), the two groups of patients had comparable disease duration, MRC-80 scores, and PND scores (Table 1). HRUS showed a lower number of affected nerve segments in patients with ATTRv-PN than in patients with CIDP (p<0.001). Nerve CSA in the 11 patients with ATTRv-PN was significantly lower than in CIDP patients at the brachial plexus, median nerve at the axilla, arm, and forearm, peroneal nerve at the popliteal fossa (p<0.01) and ulnar nerve at the forearm (p=0.03) (Fig. 2).
Nerve CSA of the 26 nerve sites in the two patients with ATTRv-PN and demyelinating features was comparable to that in CIDP patients. In patients with ATTRv-PN with non-demyelinating features of peripheral nerve damage, nerve CSA was significantly lower than that of CIDP patients at the brachial plexus, median nerve at the axilla, arm, and forearm, and peroneal nerve at the popliteal fossa (p<0.01). The ulnar nerve CSA difference at the forearm approached statistical significance (p=0.058).
Comparing ATTRv-PN patients with the eight treatment naïve CIDP patients, nerve CSA was significantly lower than that of CIDP at the brachial plexus, median nerve at the arm and forearm, and peroneal nerve at the popliteal fossa (p<0.05). The median nerve CSA difference at the axilla approached statistical significance (p=0.07).
Considering the distribution of HRUS abnormalities of median and ulnar nerves at proximal sites (median and ulnar nerves at the axilla and arm, median nerve at the elbow) compared with distal nerve segments (forearm), we observed prominent proximal nerve involvement in both diseases, which was statistically significant in CIDP (p<0.001) and approached significance in ATTRv-PN (p=0.06).
The frequency of HRUS abnormalities at entrapment points we found in ATTRv-PN patients was lower than that in CIDP patients (Table 3).
Discussion
In this cross-sectional prospective study, we used HRUS of peripheral nerves to show that nerve CSA at multiple non-entrapment nerve sites was significantly smaller in patients with ATTRv-PN than in patients with CIDP, though this difference might be negligible in patients with ATTRv-PN and pure demyelinating nerve damage. Our data on nerve CSA in patients with ATTRv-PN and CIDP might contribute to the diagnosis of ATTRv-PN in clinical practice.
We used electrodiagnostic study and applied the CIDP diagnostic criteria of the European Academy of Neurology/PNS (Joint Task Force of the EFNS and the PNS, 2010) [18] to distinguish patients with demyelinating features in the group of ATTRv-PN patients. Although several patients had isolated or multiple abnormalities compatible with demyelination, electrodiagnostic study abnormalities met CIDP criteria in only two patients. These findings are in line with previous studies showing that patients with late-onset ATTRv-PN seldom meet the clinical and electrodiagnostic study criteria for CIDP diagnosis [21].
Although we cannot exclude that distinct pathogenetic processes may underlie demyelinating and non-demyelinating types of ATTRv-PN, we believe that these two types of peripheral nerve damage reflect a pathophysiological continuum. Accordingly, we hypothesize that a common pathological process of different severity (e.g. amyloid fibril storage) may underlie a continuum of electrodiagnostic study changes, supporting the categorization of either demyelinating or non-demyelinating neuropathy based on the different effect of amyloid storage on the myelin sheath. The marked axonal loss in ATTRv-PN patients with demyelinating neuropathy may support this hypothesis [21]. However, it is still unknown how study abnormalities reflect pathological changes in the peripheral nerves of ATTRv-PN patients since most data were derived from sural nerve biopsy or autoptic material [3, 20].
In our study, HRUS showed that nerve CSA at proximal nerve sites was significantly larger in the 11 patients with ATTRv-PN than in healthy controls and this difference persisted in the nine patients with non-demyelinating neuropathy. These findings are consistent with previous studies [13, 14] and suggest that HRUS evidence of increased nerve CSA at proximal nerve sites in patients with progressive peripheral neuropathy with axonal loss should prompt genetic testing for ATTRv-PN.
The increased nerve CSA we found at proximal sites in patients with ATTRv-PN is in line with nerve imaging studies in ATTRv-PN patients. The increase in nerve trunk size detected by HRUS and magnetic resonance imaging has been attributed to amyloid deposits in the endoneurium and blood vessels and the presence of endoneurial oedema [13, 14, 21, 22]. Similar morphological changes have also been detected in CIDP and have been attributed to the proliferation of Schwann cells caused by repeated demyelination and remyelination, endoneurial oedema, and the accumulation of amorphous substance in the endoneurium, likely derived from secondary products associated with nerve degeneration [23, 24]. These data introduce the hypothesis that the loss of distal nerve fibres, which is the most characteristic sign of ATTRv-PN, may represent the consequence of the lesion load in proximal nerve segments [22, 25,26,27].
Using HRUS, we showed that nerve CSA in our 11 patients with ATTRv-PN was smaller than that in patients with CIDP. In patients with ATTRv-PN, nerve CSA abnormalities predominantly affected proximal nerve sites, whereas CSA abnormalities involved both proximal and distal nerve sites in CIDP patients. Our data therefore indicate that HRUS might be a supportive tool to electrodiagnostic investigation in ATTRv-PN diagnostic work-up. Our findings are in line with a recent study [16] comparing HRUS changes in ATTRv-PN and CIDP patients. However, we admit that our results are hardly comparable to this study due to differences in genetic background, clinical characteristics, and study protocol.
When we analyzed nerve CSA in patients with and without demyelinating features as assessed with electrodiagnostic study, we found that nerve CSA was smaller in the nine patients with non-demyelinating features than in CIDP patients. However, in the two patients with electrodiagnostic study abnormalities compatible with CIDP criteria, nerve CSA was comparable to that of CIDP patients. Admittedly, these findings may hamper the usefulness of HRUS in distinguishing ATTRv-PN and CIDP and indirectly indicate that electrodiagnostic study must remain the main diagnostic tool for diagnosing peripheral nerve damage in patients with ATTRv-PN and CIDP.
Entrapment neuropathies, namely carpal tunnel syndrome and ulnar neuropathy at the elbow, are frequent and early complaints in patients with ATTRv-PN. At entrapment sites, nerve damage may be induced by both amyloid deposition in anatomically adjacent ligaments and nerve susceptibility to pressure injury [28] and increased amyloid storage in nerve sites that chronically undergo traumatic injuries. Unexpectedly, the frequency of HRUS abnormalities at entrapment points we found in ATTRv-PN patients was lower than that in CIDP patients. We observed HRUS alterations involving 16/88 (18.1%) nerves at entrapment points in ATTRv-PN subjects, a finding that may reflect ineffective nerve regenerative response to pressure damage in ATTRv-PN [29].
Study limitations
Admittedly, our study has several limitations. We included 11 patients with ATTRv-PN, of which only two had demyelinating features compatible with a CIDP diagnosis. We therefore cannot provide reliable information on whether HRUS of peripheral nerves reliably distinguishes ATTRv-PN mimicking CIDP. Further multicentre studies including large samples of patients with ATTRv-PN and pure demyelinating nerve damage are needed to verify whether HRUS is sensitive in distinguishing ATTRv-PN from CIDP. Since an effect of different therapies on nerve CSA in treated CIDP patients cannot be excluded, further studies including larger groups of CIDP treatment naïve patients may be needed. Based on the wide genetic variability of ATTRv-PN in our sample, we cannot exclude that our findings in a small population of late-onset ATTRv-PN patients may be different from the HRUS pattern in endemic areas.
Longitudinal studies with detailed HRUS examination in ATTRv-PN patients are needed to better correlate ultrasonographic data and neuropathological findings and to evaluate their changes over time.
Conclusion
Our cross-sectional prospective study showed that HRUS provides reliable information on nerve damage in patients with ATTRv-PN. Although HRUS data markedly differed between ATTRv-PN and CIDP patients, the two patients with ATTRv-PN mimicking CIDP had comparable HRUS findings to CIDP patients. This finding may hamper the usefulness of HRUS as a standalone technique for distinguishing between ATTRv-PN and CIDP.
References
Schmidt HH et al (2018) Estimating the global prevalence of transthyretin familial amyloid polyneuropathy: ATTR-FAP Global Prevalence. Muscle Nerve 57(5):829–837. https://doi.org/10.1002/mus.26034
Adams D, Koike H, Slama M, Coelho ET (2019) Hereditary transthyretin amyloidosis: a model of medical progress for a fatal disease. Nat Rev Neurol 15(7):387–404. https://doi.org/10.1038/s41582-019-0210-4
Koike H et al (2004) Pathology of early- vs late-onset TTR Met30 familial amyloid polyneuropathy. Neurology 63(1):129–138. https://doi.org/10.1212/01.WNL.0000132966.36437.12
Ando Y et al (2013) Guideline of transthyretin-related hereditary amyloidosis for clinicians. Orphanet J Rare Dis 8(1):31. https://doi.org/10.1186/1750-1172-8-31
Plante-Bordeneuve V (2007) Diagnostic pitfalls in sporadic transthyretin familial amyloid polyneuropathy (TTR-FAP) 7
Cakar A, Durmus-Tekce H, Parman EY (2019) Familial amyloid polyneuropathy. Arch Neuropsychiatr. https://doi.org/10.29399/npa.23502
Russo M et al (2020) ATTRv amyloidosis Italian Registry: clinical and epidemiological data. Amyloid 27(4):259–265. https://doi.org/10.1080/13506129.2020.1794807
Adams D et al (2020) Expert consensus recommendations to improve diagnosis of ATTR amyloidosis with polyneuropathy. J Neurol. https://doi.org/10.1007/s00415-019-09688-0
Walker FO (2017) Ultrasonography in peripheral nervous system diagnosis. Continuum: Lifelong Learn Neurol 23(5):1276–1294. https://doi.org/10.1212/CON.0000000000000522
Gonzalez NL, Hobson-Webb ELD (2019) Neuromuscular ultrasound in clinical practice: a review. Clin Neurophysiol Pract 4:148–163. https://doi.org/10.1016/j.cnp.2019.04.006
Di Pasquale A, Morino S, Loreti S, Bucci E, Vanacore N, Antonini EG (2015) Peripheral nerve ultrasound changes in CIDP and correlations with nerve conduction velocity. Neurology 84(8):803–809. https://doi.org/10.1212/WNL.0000000000001291
Goedee HS et al (2017) Diagnostic value of sonography in treatment-naive chronic inflammatory neuropathies. Neurology 88(2):143–151. https://doi.org/10.1212/WNL.0000000000003483
Granata G et al (2014) Ultrasound evaluation in transthyretin-related amyloid neuropathy: ultrasound in TTR-related neuropathy. Muscle Nerve 50(3):372–376. https://doi.org/10.1002/mus.24168
Salvalaggio A et al (2020) Nerve ultrasound in hereditary transthyretin amyloidosis: red flags and possible progression biomarkers. J Neurol. https://doi.org/10.1007/s00415-020-10127-8
Leonardi L et al (2020) Nerve ultrasonography findings as possible pitfall in differential diagnosis between hereditary transthyretin amyloidosis with polyneuropathy and chronic inflammatory demyelinating polyneuropathy. Neurol Sci. https://doi.org/10.1007/s10072-020-04717-7
Du K et al (2021) Nerve ultrasound comparison between transthyretin familial amyloid polyneuropathy and chronic inflammatory demyelinating polyneuropathy. Front Neurol 12:632096. https://doi.org/10.3389/fneur.2021.632096
Salvalaggio A et al Progressive brachial plexus enlargement in hereditary transthyretin amyloidosis. J Neurol 9
Joint Task Force of the EFNS and the PNS (2010) European Federation of Neurological Societies/Peripheral Nerve Society Guideline on management of chronic inflammatory demyelinating polyradiculoneuropathy: report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society - First Revision. J Peripheral Nerv Syst 15(1):1–9. https://doi.org/10.1111/j.1529-8027.2010.00245.x
England JD et al (2009) Practice parameter: the evaluation of distal symmetric polyneuropathy: the role of laboratory and genetic testing (an evidence-based review 1:9
Dyck PJ et al (2005) History of standard scoring, notation, and summation of neuromuscular signs. A current survey and recommendation. J Peripher Nerv Syst 10(2):158–173. https://doi.org/10.1111/j.1085-9489.2005.0010206.x
Lozeron P et al (2018) Transthyretin amyloid polyneuropathies mimicking a demyelinating polyneuropathy. Neurology 91(2):e143–e152. https://doi.org/10.1212/WNL.0000000000005777
Fujitake J et al (2003) Late-onset familial amyloid polyneuropathy: an autopsy study of two Japanese brothers. Amyloid 10(3):198–205. https://doi.org/10.3109/13506120308999001
Matsuda M, Ikeda S-I, Sakurai S, Nezu A, Yanagisawa N, Inuzuka ET (1996) Hypertrophic neuritis due to chronic inflammatory demyelinating polyradiculoneuropathy (CIDP): a postmortem pathological study 7
Mathey EK et al (2015) Chronic inflammatory demyelinating polyradiculoneuropathy: from pathology to phenotype. J Neurol Neurosurg Psychiatry 86(9):973–985. https://doi.org/10.1136/jnnp-2014-309697
Hanyu N, Ikeda S-I, Nakadai A, Yanagisawa N, Powell EHC (1989) Peripheral nerve pathological findings in familial amyloid polyneuropathy: a correlative study of proximal sciatic nerve and sural nerve lesions. Ann Neurol 25(4):340–350. https://doi.org/10.1002/ana.410250405
Pham M et al (2011) Proximal neuropathic lesions in distal symmetric diabetic polyneuropathy: findings of high-resolution magnetic resonance neurography. Diabetes Care 34(3):721–723. https://doi.org/10.2337/dc10-1491
Khoshnoodi MA, Truelove S, Burakgazi A, Hoke A, Mammen AL, Polydefkis EM (2016) Longitudinal assessment of small fiber neuropathy: evidence of a non–length-dependent distal axonopathy. JAMA Neurol 73(6):684. https://doi.org/10.1001/jamaneurol.2016.0057
Sueyoshi T et al (2011) Wild-type transthyretin-derived amyloidosis in various ligaments and tendons. Human Pathol 42(9):1259–1264. https://doi.org/10.1016/j.humpath.2010.11.017
Fleming CE, Saraiva MJ, Sousa EMM (2007) Transthyretin enhances nerve regeneration: transthyretin enhances nerve regeneration. J Neurochem 103(2):831–839. https://doi.org/10.1111/j.1471-4159.2007.04828.x
Acknowledgements
We would like to thank Melissa Kerr for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has relevant conflict of interest to declare.
Ethical approval
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Leonardi, L., Di Pietro, G., Di Pasquale, A. et al. High-resolution ultrasound of peripheral nerves in late-onset hereditary transthyretin amyloidosis with polyneuropathy: similarities and differences with CIDP. Neurol Sci 43, 3387–3394 (2022). https://doi.org/10.1007/s10072-021-05749-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05749-3