Abstract
Background
The current gold standard for evaluating normal and impaired motor performances includes the use of the information provided by the patient and the Unified Parkinson’s Disease Rating Scale (UPDRS). However, clinical rating scales are typically subjective and their time-limited duration may fail to capture daily fluctuations in motor symptoms resulting from Parkinson’s disease. Recently, a new tool has been proposed for objective and continuous assessment of movement disorders based on the evaluation of frequential data content from multi-axial sensors and the identification of specific movement patterns typically associated with disorders. This reduces the probability of confusing physiological or pathological movements occurring at the same frequency with a different movement pattern. However, the data provided by the tool have not yet been compared with the information provided by the typically used clinical rating scales.
Objectives
The aim of this work is to investigate the possible relationship between UPRDS scores and the information provided by the tool for continuous and long-term monitoring.
Materials and methods
In this study, 20 patients with hand tremor were recruited. The UPDRS scoring was performed by a neurologist. Then, continuous monitoring was performed; data were acquired by means of the proposed wrist-worn-device “PD-Watch” for 24 h and then processed in order to get information and indexes on motor symptoms. Finally, these indexes were correlated to the UPDRS scores.
Results
Results show that the concise indexes provided by the tool correlate well with some items in UPDRS Part III, and this correlation has allowed to provide a more direct and immediate meaning to the values of the concise indexes detected by the tool.
Conclusions
While results need to be extended with further studies, this can be considered useful information in the context of clinical trials and routine clinical practice for assessing motor symptoms and movement disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is the second most common neurodegenerative disorder [1], and the main motor symptoms include bradykinesia, rigidity, and tremors [2, 3]. There are various treatments for these motor symptoms [4] and though treatment with Levodopa is usually initially effective, around 50% of patients experience levodopa-induced dyskinesia (LID) after 5 and 10 years [5]. Both the diagnosis of PD and the assessment of its progression are essentially clinical and typically based on performing neurological examinations and motor tests [6]; particularly, the current gold standard for the evaluation of motor performances and impairments includes the use of the information provided by the patient, such as their motor symptom diary, and rating scales, such as the Unified Parkinson’s Disease Rating Scale (UPDRS) [7, 8]. However, patients’ self-reporting is not always reliable, and clinical rating scales are typically subjective, so the time-limited duration of the abovementioned clinical examinations may typically fail to capture daily fluctuations in PD motor symptoms [5, 9, 10]. In order to reduce these shortcomings, several devices and methods have been proposed for the objective and quantitative assessment of movement disorders and tremor due to PD [11,12,13]. However, some proposed methods and clinical trials require the presence of a clinician and, usually, do not allow continuous monitoring of movement disorders, determining that they might fail to capture variations in a patient’s continuously changing motor state. Therefore, various systems and methods have been proposed for the objective and continuous assessment of movement disorders and tremor due to PD, allowing monitoring of the patient’s continuously changing motor state for the whole day [14, 15]. Some of the proposed solutions are based on the use of wearable inertial measuring units and on the signal processing to evaluate the frequential content in the range in which motor symptoms due to PD typically occur (i.e., mainly up to about 12 Hz) [6, 16]. However, most typical habitual motor activities performed by patients may have a power spectrum (e.g., up to 20 Hz [17]) that overlaps with the range in which regular movements typically occur. As a consequence, solely evaluating the frequential content does not usually offer a reasonable distinction between movement disorders and normal daily motor activity.
In order to improve this, a recent tool (i.e., “PD-Watch”) has been proposed that evaluates the frequential data content coming from multi-axial sensors and identifies specific movement patterns that motor symptoms are typically associated with [18] (e.g., PD hand tremors usually occur between 3 and 7 Hz with a supination–pronation characteristic, while tremor in patients affected by essential tremor (ET) typically occurs between 5 and 10 Hz with a flexion–extension pattern [3]). With reference to PD-induced hand tremor detection, this tool checks if the movement frequency falls within the above quoted typical range and if it has a supination–pronation pattern [18]. This reduces the probability of being misled by other physiological or pathological movements occurring at same frequency as PD tremors, but with a movement pattern that differs from the characteristic supination–pronation motion. Therefore, this combined analysis has been used to refine distinguishing motor activity due to movement disorders from that due to patients’ normal daily activities, and one kind of movement disorder from another; moreover, preliminary data on the tool show an accuracy on the tremor detection of about 91% and on the dyskinesia detection of about 75% [19].
However, the results coming from the PD-Watch have not yet been compared with the information provided by the typically used clinical rating scales. Thus, the aim of this work is to investigate a possible relationship between UPRDS scores and the information provided by the tool following the continuous and long-term monitoring.
Materials and methods
In this study, 20 patients affected by PD with hand tremor (and without any involuntary movements and dyskinesias) were recruited from the Neurology Unit of the Hospital of Potenza “San Carlo”, Italy. Patients provided informed consent prior to participation in the study. The study protocol was approved by the Ethics Committee of Basilicata, Italy.
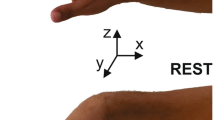
The UPRDS scoring was performed by a neurologist and with patients under medication; after neurological examination, continuous monitoring began. Patients were asked to wear the portable wearable system (i.e., “Parkinson’s Disease Watch, PD-Watch”) (Fig. 1a) on their wrist for continuous and objective measurements of motor activity in each patient’s normal environment. This wrist-worn device comprised a tri-axial accelerometer, a battery, a memory support, and a microcontroller unit. The duration of the recording period was set to 24 h and the data from the tri-axial accelerometer was sampled with a frequency of 100 Hz per channel. At the end of the 24-h acquisition period, recorded data were processed with the considered processing method (i.e., the so called “BL-method” [18]), which produced a report containing the information on the movement disorders trends during the day and on the concise indexes related to the cumulative duration and severity of the various possible hand tremor events detected during the entire duration of monitoring. Finally, this information was compared with the UPRDS score.
Wearable device and 24-h acquisition for a PD patient with hand tremor and dyskinesia. a Scheme of the PD-Watch wearable device. b Tremor and dyskinesia duration detected by the device during the trial in 30-min time intervals. c Results on the concise indexes detected by the tool during the 24-h acquisition
Figure 1 summarizes the main information provided by the tool at the end of signal processing for 24 h of acquisition in a PD patient with tremor and dyskinesia (similarly, in a PD patient with tremor and without any involuntary movements and dyskinesias, the main information provided and reported by the tool is only related to the tremors); Figure 1 b shows data on the tremor and dyskinesia duration detected by the device during the 24-h trial in time intervals of 30 min; Figure 1 c reports the value of the concise indexes on the cumulative duration and severity of the various possible movement disorders events detected during the entire duration of monitoring period. The description of these indexes has been reported previously [18] and is summarized below:
-
The LP index (lasting index) is related to the cumulative duration of the possible hand tremor events detected during the entire duration of 24-h monitoring period. The LP index was also reported in percentage form (LP%) as the ratio between the cumulative duration of symptoms and the duration of the acquisition.
-
The BP index (bustle intensity index) represents the tremor severity and intensity related to the entire duration of monitoring and, consequently, takes into account the entirety of the hand tremor events detected.
-
The BLP index was defined as the product between LP index and BP index and summarized both severity and duration of tremors detected during the entire duration of monitoring time.
Similarly, the BD, LD, and BLD indexes reported in Fig. 1c may be considered for the dyskinesia. Figure 1c shows that the results from continuous monitoring indicate an overall tremor duration of 48 min (i.e.. 0.8 h) and an overall dyskinesia duration of 1 h and 36 min (i.e., 1.6 h) during the whole day. Moreover, Fig. 2b provides details on the tremor and dyskinesia trends in 30-min time interval (e.g., between 19:00 and 19:30, tremor occurs for about 4 min and dyskinesia occurs for about 6 min).
Tremor temporal trends detected during the day by the tool represented in 30-min time intervals and compared between indexes provided by the tool and UPDRS scores. Data on the vertical axis of each plot refer to the temporal acquisition time and are represented according the format [mm-dd hh:mm] (i.e., month-day hour:minute). a Tremor temporal trend in a PD patient with items no. 3.17 and 3.18 of UPDRS equal to 0 value. LP index=0.7 h, BP index=0.68. b Tremor temporal trend in a PD patient with items no. 3.17 and 3.18 of UPDRS equal to 1 (LP index=3.5 h, BP index=11.1). c Tremor temporal trend in a PD patient with item no. 3.18 of UPDRS equal to 2 and with item no. 3.17 of UPDRS equal to 3 (LP index=5.4 h, BP index=46.2)
At the end of 24-h recording, the concise indexes obtained for each continuous monitoring sequence were compared with the UPDRS scoring. In particular, the LP index was compared with the UPDRS test score obtained at item no. 3.18 on the constancy and presence of tremor as detected by the examiner/neurologist; the BLP index was compared with the UPDRS test score obtained at item no. 2.10 on the overall shaking and tremor perceived by the patient during the week preceding the examination; the BP index was compared with the UPDRS test score for items no. 3.15, 3.16, and 3.17 on the amplitude of postural hand tremor, kinetic hand tremor, and rest tremor, respectively. In particular, the BP index was compared with both the maximum and mean values of the UPDRS score for items no. 3.15, 3.16, and 3.17. Even if the abovementioned tremors (i.e., postural, kinetic, and rest tremor) differed in terms of activation conditions, the possible tremor frequencies were practically the same for the various tremor and the action tremor usually has waveform similarities with rest tremor [16].
Therefore, the BP and LP indexes on the intensity and duration of tremor were compared by considering some items in Part III (“motor examination”) of the UPDRS scale, which are related to tremor amplitude and presence as detected by the examiner/neurologist during the clinical examination. The BLP index on the combination of severity and duration of tremor was compared to a UPDRS item in Part II (“motor experiences of daily living”), which is based mainly on the patient’s feedback regarding their general perception of tremor during the week preceding the clinical examination.
Results
The UPDRS scores were compared with data from the considered tool for continuous monitoring of movement disorders. Figure 2 shows, for three patients with different tremor severity, the UPDRS scores for items no. 3.18 and no. 3.17, and the values of the LP and BP indexes on the cumulative duration and severity of tremors were compared for the monitoring period (i.e., 24 h). Figure 2 also shows a graphical representation of the tremors’ temporal trend during the day. Figure 2 a is related to a PD patient to whom items no. 3.17 and 3.18 of UPDRS scored 0, while results of continuous monitoring indicated an overall tremor duration of 42 min (i.e., 0.7 h) during the whole day and a maximum tremor severity in the time interval between 6:30 and 7:00 a.m. In this 30-min time interval, tremors occurred for about 5 min and with the highest intensity detected during the day. Similarly, Fig. 2b shows results for a PD patient with an UPDRS score of 1 to both items no. 3.17 and 3.18 and Fig. 2c shows results for a PD patient with an UPDRS score of 2 to item no. 3.18 and of 3 to item no. 3.17. Data reported in Fig. 2 illustrates a relationship between increasing values of the concise indexes provided by the wearable tool and increasing values of UPDRS scores.
Figure 3 shows the correlation with the UPDRS scores and the concise indexes LP, BP, and BLP detected through the wearable tool for continuous monitoring of movement disorders for all patients involved in the clinical trial. As well as the experimental data related to the final indexes for each patient, the plots also include the results of the linear regression fit analysis using the least squares correlation method. Table 1 summarizes the results of the linear regression analysis and reports the values of the regression coefficient, a, of the linear combinations and of the coefficient of determination, r2. Table 1 also illustrates the relationship for each concise index between the mean value and standard deviations with the corresponding UPDRS score values. Results show a good linear correlation between the LP index on the cumulative tremor duration during the day and the UPDRS scores of item 3.18 and on the constancy of tremor detected by the neurologist during the execution of the rating scale (r2 is equal to 0.744). Similarly, a good linear correlation existed between the BP index on the cumulative tremor intensity of the entire day and the maximum value of the UPDRS scores for items no. 3.15, 3.16, and 3.17 on the postural hand tremor, kinetic hand tremor, and rest tremor amplitude (r2 is equal to 0.779). This relationship has provided improved curve fitting parameters than those from the execution of linear regression by considering the mean value of the considered UPDRS items instead of their maximum value (r2 is equal to 0.515 if the mean of UPDRS items was considered). Finally, the correlation between the daily BLP index related to tremor severity and duration and UPDRS scores (item no. 2.10) on the overall shaking and tremor perceived by the patient during one week is characterized by a coefficient equal to 0.468. Moreover, Table 1 shows that the mean value of the LP index is equal to 3.3 (with a standard deviation of 0.4) for patients with value of 1 on item no. 3.18 of UPDRS and the mean value of the LP index is equal to 4.9 (with a standard deviation of 0.6) for patients with a value of 2 for item no. 3.18 of UPDRS. Similarly, Table 2 reports results of the correlation for the other concise indexes and UPDRS items involved.
Comparison between indexes provided by the tool and UPDRS scores. a Relationship between the LP index on the cumulative tremor duration during the day, the UPDRS scores of item 3.18 and the constancy of tremor detected by the neurologist during the execution of the rating scale (r2=0.744). b Relationship between the BP index on the cumulative tremor intensity related to the entire day and the maximum value of the UPDRS scores for items no. 3.15, 3.16, and 3.17 on the postural hand tremor, kinetic hand tremor, and rest tremor amplitude (r2=0.779). c Relationship between the BLP index related to both severity and duration of tremors detected during the entire day and UPDRS score obtained at item no. 2.10 on the overall shaking and tremor perceived by the patient during the week preceding the examination (r2=0.468)
Discussion
The current method of evaluating motor performances and impairments includes the use of the information provided by the patient and UPDRS. However, clinical rating scales are typically subjective and patient self-reporting is not always reliable. Moreover, the time-limited duration of the mentioned clinical examinations typically fails to capture daily fluctuations in PD motor symptoms.
Currently available methods for objective and continuous assessment of movement disorders and tremor due to PD may allow monitoring of the patient’s continuously changing motor state for the whole day, but some systems do not allow a reasonable distinction between movement disorders and normal daily motor activity. Indeed, they are mainly based on a spectral analysis to check if the detected signal frequency is within the range in which motor symptoms due to PD typically occur, but the mere evaluation of this usually does not allow an accurate distinction because the usual frequential range of physiological and pathological movements may overlap. Recently, a tool has been proposed based on the combination of the evaluation of frequential content of data from multi-axial sensors and of the identification of specific movement patterns with which movement disorders are typically associated [18], thus reducing the probability of confusion between movement disorder detection by other physiological or pathological movements occurring at the same frequency but with a different movement pattern; preliminary data on the tool show an accuracy on the tremor detection of about 91% and on the dyskinesia detection of about 75% [19].
A comparison between data provided by the considered tool and information related to current gold standards and the UPDRS is useful and necessary in order to evaluate any possible correlations and potentially provide a meaningful and immediate impact to the values of the concise indexes detected by the tool. Nevertheless, it should be noted that the comparison is carried out between elements that are not completely homogeneous. Indeed, the considered tool may allow for the continuous and objective monitoring of some motor aspects, but no information on non-motor aspects are provided. Conversely, it may provide complementary information with the UPDRS by means of continuous and long-term monitoring of movement disorders for 24 h per day and not only for the limited time of clinical examinations. Therefore, the concise indexes LP, BP, and BLP obtained by the tools for each continuous monitoring sequence were compared with UPDRS scores.
As reported in Tables 1 and 2 and in Fig. 2 and 3, results show a good linear correlation between the LP index on the cumulative tremor duration during the day and item 3.18 of the UPDRS on the constancy/presence of tremor as detected by the neurologist during the execution of the rating scale (r2 =0.744). Similarly, a good linear correlation existed between the BP index on the cumulative tremor intensity related to the entire day and the maximum value of the UPDRS scores for items no. 3.15, 3.16, and 3.17 on tremor amplitude (r2=0.779). Finally, a lower coefficient of determination was found with reference to the correlation between the BLP index related to both severity and duration of tremors detected during the entire day and UPDRS scores obtained at item no. 2.10 on the overall shaking and tremor perceived by the patient during the week (r2=0.468). This lower coefficient of determination may be due to the choice of the UPDRS item involved in the comparison. UPDRS item no. 2.10 for the comparison with the BLP index was chosen due to the absence in the Part III of the UPDRS of a possible item whose meaning may be easily correlated to the BLP index. Indeed, the BP and LP indexes on the intensity and duration of tremor were compared by considering some items of the Part III of the UPDRS scale related to tremor amplitude and presence as detected by the examiner/neurologist during the clinical examination. The BLP index on the combination of severity and duration of tremor was compared to an UPDRS item which falls into Part II “motor experiences of daily living” and which is not based on the examiner/neurologist detection but mainly on the patients’ feedback and self-reporting, which is not always reliable [10].
Finally, from a general standpoint, results show that the concise indexes provided by the tool correlate well with the selected items of the UPDRS, and in particular, increasing values of the BP and LP indexes correspond to increasing scores of the selected UPDRS items. This correlation allows for the provision of a more direct and immediate meaning to the values of the concise indexes detected by the tool. While results need to be extended with further studies and more clinical trials involving other patients with various kinds and severity of symptoms and movement disorders, the proposed tool may be considered useful in the context of clinical trials and routine clinical practice for motor symptom and movement disorder assessments and as a useful, complementary, and suitable medical support for fine-tuning therapy and for finding the best possible therapeutic treatment for the patient.
References
Pringsheim T, Jette N, Frolkis A, Steeves TD (2014) The prevalence of Parkinson’s disease: a systematic review and meta-analysis. Mov Disord 29:1583–1590
Guttman M, Kish SJ, Furukawa Y (2003) Current concepts in the diagnosis and management of Parkinson’s disease. Canadian Med Ass J 168:293–301
Janckovic J (2008) Parkinson’s disease: clinical features and diagnosis. J Neurol Neurosurg Psychiatry 79:368–376
Fox SH, Katzenschlager R, Lim SY, Barton B, de Bie RMA, Seppi K, Coelho M, Sampaio C (2018) International Parkinson and movement disorder society evidence-based medicine review: update on treatments for the motor symptoms of Parkinson’s disease. Mov Disord 3:1248–1266
Dunnewold RJ, Jacobi CE, van Hilten JJ (1997) Quantitative assessment of bradykinesia in patients with Parkinson’s disease. J Neurosci Methods 74:107–112
de Lau LML, Breteler MMB (2006) Epidemiology of Parkinson’s disease. Lancet Neurol 5:525–535
Movement Disorder Society Task Force on Rating Scales for Parkinson’s Disease (2003) The Unified Parkinson’s disease rating scale (UPDRS): status and recommendations. Mov Disord 18:738–750
Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, Poewe W, Sampaio C, Stern MB, Dodel R, Dubois B, Holloway R, Jankovic J, Kulisevsky J, Lang AE, Lees A, Leurgans S, LeWitt PA, Nyenhuis D, Olanow CW, Rascol O, Schrag A, Teresi JA, van Hilten JJ, LaPelle N (2008) Movement Disorder Society-Sponsored Revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): Scale Presentation and Clinimetric Testing Results. Mov Disord 23:2129–2170
Barroso Júnior MC, Esteves GP, Nunes TP, Silva LM, Faria ACD, Melo PL (2011) A telemedicine instrument for remote evaluation of tremor: design and initial applications in fatigue and patients with Parkinson’s disease. Biomed Eng Online 10:1–14
Brown RG, MacCarthy B, Jahanshahi M, Marsden CD (1989) Accuracy of self-reported disability in patients with Parkinsonism. Arch Neurol 46:955–959
Waerling RD, Kjaer TW (2020) A systematic review of impairment focussed technology in neurology. Disability and Rehabilitation: Assistive Technology:1–14. https://doi.org/10.1080/17483107.2020.1776776
Ferreira-Sánchez MDR, Moreno-Verdú M, Cano-de-la-Cuerda R (2020) Quantitative measurement of rigidity in Parkinson’s disease: a systematic review. Sensors 20:880
Cai G, Huang Y, Luo S, Lin Z, Dai H, Ye Q (2017) Continuous quantitative monitoring of physical activity in Parkinson’s disease patients by using wearable devices: a case-control study. Neurol Sci 38:1657–1663
Espay AJ, Bonato P, Nahab FB, Maetzler W, Dean JM, Klucken J, Eskofier BM, Merola A, Horak F, Lang AE, Reilmann R, Giuffrida J, Nieuwboer A, Horne M, Little MA, Litvan I, Simuni T, Dorsey ER, Burack MA, Kubota K, Kamondi A, Godinho C, Daneault J, Mitsi G, Krinke L, Hausdorff JM, Bloem BR, Papapetropoulos S (2016) Technology in Parkinson disease: challenges and opportunities. Mov Disord 31:1272–1282
Godinho C, Domingos J, Cunha G, Santos AT (2016) A systematic review of the characteristics and validity of monitoring technologies to assess Parkinson’s disease. J NeuroEng Rehab 13:1–10
Bhatia KP, Bain P, Bajaj N, Elble RJ, Hallett M, Louis ED, Raethjen J, Stamelou M, Testa CM, Deuschl G (2018) Consensus Statement on the classification of tremors. From the Task Force on Tremor of the International Parkinson and Movement Disorder Society organize a program to provide the Movement Disorder. Mov Disord 33:75–87
Mathie MJ, Coster AC, Lovell NH, Celler BG (2004) Accelerometry providing an integrated practical method for long-term ambulatory monitoring of human movement. Physiol Meas 25:R1–R20
Battista L, Romaniello A (2018) A novel device for continuous monitoring of tremor and other motor symptoms. Neurol Sci 39:1333–1343
Battista L, Casali M, Coletti C, Grassini P, Radicati FG, Stocchi F (2020) A preliminary investigation on the accuracy of the wearable systems for continuous monitoring of movement disorders. Proceedings of the 6th Conference of Italian Academy on movement disorders. P6. Available at https://www.accademialimpedismov.it/web/image/51617/AbstractCongressoVirtualeAccademiaLIMPE_DISMOV_2020.pdf
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Research involving human participants and/or animals
Yes, human participants. The study protocol was approved by the Ethics Committee of Basilicata, Italy.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
Eng. Luigi Battista holds intellectual property rights for a wearable system for Parkinson’s disease. Dr. Antonietta Romaniello has nothing to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Battista, L., Romaniello, A. A wearable tool for continuous monitoring of movement disorders: clinical assessment and comparison with tremor scores. Neurol Sci 42, 4241–4248 (2021). https://doi.org/10.1007/s10072-021-05120-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05120-6