Abstract
Amyotrophic lateral sclerosis (ALS) is a multisystemic disease compromising both the neuromuscular system and the cognitive status. Non-invasive ventilation (NIV) has been shown to improve survival and quality of life in ALS patients with respiratory failure, but scanty literature investigated which are the predictors of NIV tolerance. The aim of this study was to evaluate the impact of functional, cognitive, neurobehavioral, and respiratory status on NIV compliance and tolerance in patients with ALS. We retrospectively evaluated clinical data of ALS patients who consecutively underwent a NIV trial during hospitalization. Cognitive and neurobehavioral assessments have been performed using the Edinburgh Cognitive and Behavioral ALS Screen (ECAS), the Hospital Anxiety and Depression Scale (HADS), the Frontal Assessment Battery (FAB), the Raven’s 47 Colored Progressive Matrices (PM47), and the Neurobehavioral Rating Scale Revised (NRSR). Seventy-two patients (mean age ± SD; 63.9 ± 10.6 years) were included. Patients adapted were 63/72 (87.5%). The average time of adaptation was 7.82 ± 5.27 days. The time required to reach a satisfying NIV adaptation was significantly related to the presence of sialorrhea (p = 0.02), respiratory status (Borg Dyspnoea Scale, p = 0.006, and ALS-FRS-R respiratory subscore, p = 0.03) and behavioral and cognitive impairment (NRSR-F1, p = 0.04, NRSR- F5, p = 0.04). Presence of sialorrhea and neurobehavioral impairment, and absence of respiratory symptoms are negative predictors of NIV adaptation. This study highlights the need of a multidisciplinary patient-tailored approach including cognitive-behavioral assessment and a psychological support program to optimize patient’s training and compliance to NIV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Amyotrophic lateral sclerosis (ALS) is a heterogeneous neurodegenerative rare disease of adult life, leading to severe weakness of bulbar, limb, and respiratory muscles and consequent short life expectancy [1, 2]. A complex multistep process involving genetic and environmental factors is involved in ALS pathogenesis and clinical variability [3, 4]. Cognitive involvement is often associated with ALS and can vary from mild executive function impairment to a frontotemporal dementia (FDT) [1]. The cognitive deficit profile includes impairment of executive functions, verbal fluency, language, social cognition, and verbal memory. In 6–14% of patients, the cognitive and behavioral changes meet the criteria for a frontotemporal dementia (FTD) [5,6,7]. A cluster analysis indicated four patient subgroups: 49% with intact cognition, 32% with mild cognitive impairment, 13% with moderate impairment, and 6% with severe impairment [8].
/The medical therapy is still scanty, and management remains predominantly supportive, with a primary focus on the respiratory system, including mechanical support of ventilation and clearance of secretions [9, 10]. Non-invasive ventilation (NIV) is currently the treatment for ALS-related respiratory failure. It is well known that NIV alleviates respiratory symptoms, improves quality of life (QoL), and increases survival [9,10,11,12,13,14,15,16,17,18]. Unfortunately, a percentage between 28 and 67% of patients has been reported to not tolerate NIV use along the course of the disease, especially if they experienced a bulbar phenotype and the presence of sialorrhea [19,20,21]. However, an intensive educational training performed in a hospital multidisciplinary setting increases compliance and tolerance to NIV over the disease course [20].
Despite the burning need to define the predictor factors to NIV compliance in order to improve the outcome, no studies have systematically investigated the impact of each aspect of this multifaceted disease, including the cognitive and neurobehavioral status, in order to outline a specific patient-tailored training. The aim of this study was to evaluate how functional assessment of neurological status, respiratory involvement, and cognitive, emotional, and behavioral profile could modify the compliance and tolerance to NIV in patients with ALS.
Patients and methods
This is a retrospective study performed on patients, who underwent for the first time a NIV trial, consecutively hospitalized over a year at the Nemo Sud Clinical Center for Neuromuscular Disorders of Messina, Italy, and subsequently followed in outpatient clinic at least for one year on a 3-month basis. The study was approved by the Research Ethics Committee of the University of Messina School of Medicine Hospital, Policlinico “G. Martino,” Messina, Italy. Written informed consent was obtained from all participants enrolled in the study.
All patients had a diagnosis of probable/definite ALS, according to the El Escorial World Federation of Neurology revised criteria [22]. Patients were classified in bulbar or non-bulbar phenotypes, the latter including the following forms: classic, flail arm, flail leg, pure lower motor neuron, pure upper motor neuron, pyramidal, and respiratory [3]. All selected patients fulfilled accepted criteria for starting NIV and consented for a dedicated “in-ward” hospitalization [23].
ALS patients after diagnosis were followed in outpatient clinic by a multidisciplinary team. When they full-filled the criteria to start NIV, patients were hospitalized and underwent functional, pneumological, and psychological evaluations.
Functional evaluation
ALS Functional Rating Scale-Revised (ALSFRS-R) [24] has been administered. Its subscores were analyzed as follows: the “bulbar score” was obtained adding the results of items 1 to 3; item 2 was also separately analyzed for the presence of sialorrhea. We considered sialorrhea as present if the score calculated for the item 2 at ALS-FRS-R bulbar subscore was 0, 1, or 2; patients had no sialorrhea if the score was 3 or 4. The “upper limb,” “lower limb,” and “respiratory” scores were obtained adding the results of items 4 to 6, 7 to 9, and 10 to 12, respectively.
Psychological evaluation
We constructed a neuropsychological test battery to cover the main cognitive, emotional, and behavioral ALS-specific domains, while attempting to minimize motor demands, which would stress the majority of patients. The evaluation included the Raven’s 47 Colored Progressive Matrices (PM47) [25] and the Frontal Assessment Battery (FAB) [26], for measuring, respectively, non-verbal abstract reasoning and global executive dysfunction, both brief screening tools. The Edinburgh Cognitive and Behavioral ALS Screen (ECAS) [27] was used for its sensitiveness to cognitive/behavioral alterations in ALS patients, as evidence of a pre-symptomatic cognitive decline. The Hospital Anxiety and Depression Scale (HADS) was used to assess the contribution of mood disorders [28, 29].
Neurobehavioral aspects were evaluated by Neurobehavioral Rating Scale Revised (NRSR) [30] with its five factors:
-
1.
Factor I (deficit in intentional behavior; NRSR-F1) consisted of items pertaining to intentional or goal-oriented behavior such as decreased motivation and difficulty in planning.
-
2.
Factor II (lowering of emotional state; NRSR-F2) included depressive mood, anxiety, and emotional withdrawal.
-
3.
Factor III (deficit in the regulation of survival-oriented behavior/heightened emotional state; NRSR-F3) consisted of items such as irritability, disinhibition, hostility, and hyperactivity agitation.
-
4.
Factor IV (deficit in the regulation of arousal state; NRSR-F4) had items such as reduced alertness, inattention, and mental fatigability.
-
5.
Factor V (language and speech problems; NRSR-F5) consisted mainly of problems in speech and expressive and comprehension language skills.
Respiratory assessment and management
Forced vital capacity (FVC) was measured from flow-volume curves obtained with a pneumotachograph (MIR, Spirobank®, Rome, Italy) according to ATS/ERS standards in both upright and supine position [31]. Values were expressed as absolute values. Reference values were derived from published data [32]. Maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP) tests were, respectively, performed by an experienced operator with MicroRPM (Micro Medical, Kent, UK), who strongly advised the subjects to produce maximum inspiratory (Mueller maneuver) and expiratory (Valsalva maneuvers) efforts at near residual volume and total lung capacity, respectively. All tests were repeated at least three times, and highest value measured was recorded. Reference values were taken into account according to previously published data [33]. Arterial blood gas analysis was performed in seated position when the patient breathes room air. Overnight oximetry was performed in the first day of hospital admission by an oximeter with memory (Nonin Palmsat Model 2500, Plymouth, MN) when the patient breathe room air.
We administered to all patients the modified Borg Scale (MBS), an easy visuo-analogic scale that provides rapid information about the patient’s subjective state of dyspnea. It is rated from 0 to 10, being 0 equal to “no breathless at all” while 10 equal to “maximal” [34].
All patients and caregivers received through an informative video detailed description of NIV technique and the potential benefit on survival and QoL. The video was then discussed by the same pulmonologist. Physician, nurse, and other healthcare assistants were constantly available for any other question during the period of the NIV trial. A diurnal initiation trial to NIV was performed for each patient with pressure support ventilators (Astral 150, ResMed, Saint-Priest, France or Trilogy 100, Philips Respironics, Murrysville, Pennsylvania, USA) in spontaneous/timed pressure support ventilation mode with a fixed back-up respiratory rate (12 breaths/min). The NIV trial included choice of the best fitting facial mask and setting of inspiratory pressure to maximal patient comfort, and expiratory pressure was set < 5 cmH2O at least 2 h of NIV under the direct supervision of a respiratory physician and physiotherapist. The ventilator setting was then adjusted in order to obtain optimum nocturnal oximetry normalization and NIV acceptance. During the night, patients from the inpatient group had nurses available on hand. Patients were recommended to use nocturnal NIV as much as possible until they had completely adapted to the therapy.
We defined “time of adaptation” as the number of days required by the patient to tolerate NIV for at least 4 h continuously during sleep. Objective adherence was measured via electronic download of usage data from NIV machine. After a NIV setup definition, all patients were allowed to extend hospitalization for an average extended period of approximately 1 week for comprehensive multidisciplinary treatment and to monitor patients’ compliance. During this period, any NIV setting adjustment was performed as needed. We used anticholinergic drugs to treat sialorrhea, when present.
Statistical analysis was made using a SAS 9.3 (SAS Institute, Inc., Cary, NC) software. Data were reported in text and tables as mean and standard deviation for continuous variables and numbers and percentages for those non-continuous. For each variable, we used a Shapiro-Wilk test to evaluate the normality of the distribution and Levene test to evaluate the homogeneity of variance. Correlation univariate analysis was made using the Pearson correlation coefficient and the non-parametric Spearman’s rank correlation coefficient as appropriate, using a p value < 0.20 [35], while for the multivariable analysis, the multiple regression model adjusting for age, sex, and respiratory assessments was used, with a significance level alpha < 0.05 [36].
Results
Seventy-two patients started the NIV training in our multidisciplinary setting and were included in the study. Demographic, clinical, functional, psychological, and respiratory data are shown in Table 1. According to the clinical characteristics, patients belonged to these phenotypes: 23 bulbar and 49 non-bulbar, which included 31 classic, 4 flail arm, 2 flail leg, 5 pure lower motor neuron, 5 pyramidal, and 2 respiratory forms.
In our cohort, the intellectual functioning and non-verbal reasoning were not involved, so we observed a preserved global mental functioning: at PM47 (normal/abnormal 65/7) evaluations. The executive functions, assessed with FAB, were involved in half of our patients (normal/borderline/abnormal 28/8/28). Patients obtained significant lower scores on ECAS ALS-specific functions than on the ALS non-specific sub-domains: ECAS total score (normal/abnormal 20/52); ECAS ALS-specific score (normal/abnormal 20/52), and ECAS ALS non-specific score (normal/abnormal 32/40). Therefore, in our series, we observed cognitive alterations consisting of executive functions, fluency, and language impairment. Neurobehavioral profile at NRSR was normal in the majority of patients in the following factors: Factor I (normal/abnormal 55/17) and Factor III (normal/abnormal 39/3). On the contrary, abnormalities were more frequently found in Factor II (normal/abnormal 20/52), Factor IV (normal/abnormal 30/42), and Factor V (normal/abnormal 28/44).
Patients adapted were 63/72 (87.5%). Nine patients showed low compliance and did not reach a successful adaptation. Two of these nine patients reached adaptation at 6-month follow-up. Interestingly, 7/9 patients had a bulbar phenotype with sialorrhea. Moreover, a significant proportion of these patients showed cognitive and behavioral alterations. The scores were abnormal in 5/9 at FAB, 8/9 at ECAS total score, and 7/9 at ECAS ALS-specific score and 8/9 at ECAS ALS non-specific score. NRSR scores were abnormal in 5/9 in Factors I and II, 4/9 in Factor III, and 6/9 in Factors IV and V.
Four out of 63 deceased within a year. Three out of 63 required tracheostomy to be placed. Fifty-six out of 63 (89%) patients successfully completed a 1-year follow-up with a good tolerance to NIV. Non-invasive ventilation settings were changed as needed. The average time of adaptation was 7.82 ± 5.27 SD days.
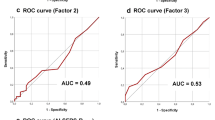
Correlation between time of adaptation and neurological, functional, cognitive, and neurobehavioral and respiratory data at univariate analysis is shown in Table 1. Sex, presence of sialorrhea, bulbar score, upper limb score, respiratory score, ECAS non-ALS-specific score, ECAS memory, ECAS visuo-spatial ability, NRSR-F1, NRSR-F4, NRSR-F5, Anxiety HADS, Depression HADS, blood gas analysis PaO2, blood gas analysis PaCO2, and Borg Dyspnea Scale showed a p < of 0.20 at univariate analysis and were considered for multivariable analysis. Statistical significance was confirmed only for NRSR-F1, NRSR-F5, ALS-FRS-R Respiratory score, Borg Dyspnea Scale scores, and presence of sialorrhea (Table 2).
Discussion
In 2006, a randomized controlled trial confirmed that NIV improves both QoL and survival in patients with ALS [11]. Unfortunately, not all ALS patients tolerate NIV. Different authors tried to identify which factors are related to a better NIV tolerance. Patients who used NIV were significantly more likely to be male and to have a gastrostomy tube, lower vital capacity, more severe disease, bulbar involvement, and poorer general health. Bulbar weakness has been associated with lower compliance [16, 18, 19, 21]. Interestingly, we did not find a significant correlation with general bulbar symptoms, as detected by the ALSFRS-R “bulbar score” encompassing speech, salivation, and swallowing but only with the presence of sialorrhea.
Almost 50% of ALS patients have impairment in saliva control during the course of the disease [37], caused not by an increasing of saliva production but by tongue spasticity together with oro-facial and palatino-lingual muscle control failure [38]. The difference in adaptation observed between patients presenting generic bulbar symptoms (difficulty in speech, swallowing, and salivation) and those presenting difficulty in salivation alone could be explained by some observations: (i) the three abilities, although governed by partially coincident muscles, do not necessarily deteriorate in parallel; (ii) in some patients, despite severe overall bulbar involvement, saliva management could be improved by anticholinergic treatment, thus making NIV adaptation difficulties, more related to a lack of response to drugs than to generic impairment in saliva management; and (iii) the amount of total saliva produced by the patient, or the characteristics of the saliva itself, could be relevant in causing difficulties in adapting to NIV. The stimulation of the sympathetic nervous system, induced by stress conditions, could lead to the production of a more dense saliva that is more difficult to manage in patients with NIV [39]. Further studies are necessary to better clarify the last two points.
We confirm in our cohort a consistent presence of patients with impairment of the neuropsychological abilities, particularly in language, verbal fluency, and executive functions. Moreover, an involvement of the neurobehavioral functions was frequently present with emotional withdrawal, deficit in the regulation of arousal state and mental fatigability, and problems in speech and expressive and comprehension language skills. Cognitive and behavioral impairment has been evaluated as possible negative predictor of NIV tolerance [40]. Our study had better specify which are cognitive and neurobehavioral changes that may interfere with NIV adaption. Executive dysfunction is the most prominent cognitive impairment and presents in about 50% of our ALS patients as previously reported [7]. We have found that impaired intentional or goal-oriented behavior such as decreased motivation/initiation, poor mental flexibility, planning, and linguistic impairments, such as deficits in oral expression/comprehension, may cause difficulties in the process of NIV adaptation. Patients who lack insight into disease severity and had severe deficits in planning and lack of initiative/motivation do not seem to understand the importance of adapting to NIV. A specific training involving caregiver with a prolonged stay in a neuro-rehabilitation clinic should be tried to give to these subsets of patients the right time to accept and be able to manage NIV.
Presence of respiratory symptoms is a strong predictor of good adaptation [23]. We confirm a strong correlation with the presence of respiratory symptoms at Borg Dyspnea Scale scores and “respiratory score” of the ALSFR-R. It is reasonable to hypothesize that a patient who experiences dyspnea is more motivated to use NIV, with immediate relief from symptoms. However, hypoxemia and hypercapnia not always coincide with dyspnea or may cause symptoms that patients sometimes do not attribute to respiratory failure, such as headache and daytime sleepiness [41]. Furthermore, a recent study has shown that an isolated increase of HCO3, although not associated with an increase in the frequency of respiratory symptoms, is related to a reduction in survival in ALS patients [42]. For this reason, patients without dyspnea, but who may benefit from starting NIV, should be carefully informed about its potential helpfulness.
A further key element involved in determining an effective NIV adaptation is the training setting. An adequate training aimed at patients and caregivers, in a hospital multidisciplinary setting, improves compliance and long-term tolerance, even between those patients with bulbar impairment. With this approach, adaptation to non-invasive ventilation can be reached in 95% of ALS patients [20]. In keeping with the previous report, we obtained a high rate of adaptation (87.5%) with slightly longer time required [20]. Probably, our approach, which gives to the patients all the time they require to be confident to NIV, before starting ventilation during the night sleep, has contributed to the good longtime tolerance.
The present study has some limitations. The main one is given by patients not adapted to NIV during hospitalization, whose correlations have not been performed in relation to possible predictive factors. However, the descriptive characteristics of these patients are in line with those of the patients who presented a prolonged adaptation time. Another limitation is the lack of objective evaluation methods for sialorrhea and dyspnea, whose quantification is based on self-reported evaluation scales.
Based on the results obtained in the present study, we propose to perform an outpatient screening before starting NIV. Considering item 2 of the ALS-FRS-R, patients with scores 3 and 4 can be selected. The next step will be to ascertain the presence of respiratory symptoms considering the MBS and the respiratory subscore of ALS-FRS-R; patients with presence of respiratory symptoms should be screened for a careful neurobehavioral and cognitive assessment possibly using NRSR, FAB, and ECAS. In the subsets of patients with a normal neurobehavioral function, we suggest to attempt a quick ambulatory approach avoiding hospitalization. For other patients, hospitalization in a multidisciplinary setting dedicated to neuromuscular diseases should be recommended.
In conclusion, our study suggests the importance of a multidisciplinary patient-tailored approach, including cognitive-behavioral assessment and psychological support program, to optimize patient’s training and compliance to NIV.
References
Hardiman O, Al-Chalabi A, Chio A, Corr EM, Logroscino G, Robberecht W, Shaw PJ, Simmons Z, van den Berg LH (2017) Amyotrophic lateral sclerosis. Nat Rev Dis Primers 3:17085
Chio A, Logroscino G, Traynor BJ, Collins J, Simeone JC, Goldstein LA, White LA (2013) Global epidemiology of amyotrophic lateral sclerosis: a systematic review of the published literature. Neuroepidemiology 41:118–130
Chiò A, Calvo A, Moglia C, Mazzini L, Mora G, PARALS study group (2011) Phenotypic heterogeneity of amyotrophic lateral sclerosis: a population based study. J Neurol Neurosurg Psychiatry 82:740–746
Al-Chalabi A, Calvo A, Chio A, Colville S, Ellis CM, Hardiman O, Heverin M, Howard RS, Huisman MHB, Keren N, Leigh PN, Mazzini L, Mora G, Orrell RW, Rooney J, Scott KM, Scotton WJ, Seelen M, Shaw CE, Sidle KS, Swingler R, Tsuda M, Veldink JH, Visser AE, van den Berg LH, Pearce N (2014) Analysis of amyotrophic lateral sclerosis as a multistep process: a population-based modelling study. Lancet Neurol 13:1108–1113
Consonni M, Iannaccone S, Cerami C, Frasson P, Lacerenza M, Lunetta C, Corbo M, Cappa SF (2013) The cognitive and behavioural profile of amyotrophic lateral sclerosis: application of the consensus criteria. Behav Neurol 27:143–153
Montuschi A, Iazzolino B, Calvo A, Moglia C, Lopiano L, Restagno G, Brunetti M, Ossola I, Lo Presti A, Cammarosano S, Canosa A, Chiò A (2015) Cognitive correlates in amyotrophic lateral sclerosis: a population-based study in Italy. J Neurol Neurosurg Psychiatry 86:168–173
Murphy J, Factor-Litvak P, Goetz R, Lomen-Hoerth C, Nagy PL, Hupf J, Singleton J, Woolley S, Andrews H, Heitzman D, Bedlack RS, Katz JS, Barohn RJ, Sorenson EJ, Oskarsson B, Fernandes Filho JA, Kasarskis EJ, Mozaffar T, Rollins YD, Nations SP, Swenson AJ, Koczon-Jaremko BA, Mitsumoto H, ALS COSMOS (2016) Cognitive-behavioral screening reveals prevalent impairment in a large multicenter ALS cohort. Neurology. 86:813–820
Benbrika S, Desgranges B, Eustache F, Viader F (2019) Cognitive, emotional and psychological manifestations in amyotrophic lateral sclerosis at baseline and overtime: a review. Front Neurosci 13:951
Aboussouan LS, Mireles-Cabodevila E (2013) Respiratory support in patients with amyotrophic lateral sclerosis. Respir Care 58:1555–1558
Radunovic A, Annane D, Rafiq MK, Brassington R, Mustfa N (2017) Mechanical ventilation for amyotrophic lateral sclerosis/motor neuron disease. Cochrane Database Syst Rev 10:CD004427
Bourke SC, Tomlinson M, Williams TL, Bullock RE, Shaw PJ, Gibson GJ (2006) Effects of non-invasive ventilation on survival and quality of life in patients with amyotrophic lateral sclerosis: a randomised controlled trial. Lancet Neurol 5:140–147
Lechtzin N, Scott Y, Busse AM, Clawson LL, Kimball R, Wiener CM (2007) Early use of non-invasive ventilation prolongs survival in subjects with ALS. Amyotroph Lateral Scler 8:185–188
Pinto AC, Evangelista T, Carvalho M, Alves MA, Sales Luís ML (1995) Respiratory assistance with a non-invasive ventilator (Bipap) in MND/ALS patients: survival rates in a controlled trial. J Neurol Sci 129(Suppl):19–26
Kleopa KA, Sherman M, Neal B, Romano GJ, Heiman-Patterson T (1999) Bipap improves survival and rate of pulmonary function decline in patients with ALS. J Neurol Sci 164:82–88
Aboussouan LS, Khan SU, Meeker DP, Stelmach K, Mitsumoto H (1997) Effect of noninvasive positive-pressure ventilation on survival in amyotrophic lateral sclerosis. Ann Intern Med 127:450–453
Lo Coco D, Marchese S, Pesco MC, La Bella V, Piccoli F, Lo Coco A (2006) Noninvasive positive-pressure ventilation in ALS: predictors of tolerance and survival. Neurology 67:761–765
Lyall RA, Donaldson N, Fleming T, Wood C, Newsom-Davis I, Polkey MI, Leigh PN, Moxham J (2001) A prospective study of quality of life in ALS patients treated with noninvasive ventilation. Neurology 57:153–156
Bourke SC, Bullock RE, Williams TL, Shaw PJ, Gibson GJ (2003) Noninvasive ventilation in ALS: indications and effect on quality of life. Neurology 61:171–177
Gruis KL, Brown DL, Schoennemann A, Zebarah VA, Feldman EL (2005) Predictors of noninvasive ventilation tolerance in patients with amyotrophic lateral sclerosis. Muscle Nerve 32:808–811
Volanti P, Cibella F, Sarvà M, De Cicco D, Spanevello A, Mora G, La Bella V (2011) Predictors of non-invasive ventilation tolerance in amyotrophic lateral sclerosis. J Neurol Sci 303:114–118
Aboussouan LS, Khan SU, Banerjee M, Arroliga AC, Mitsumoto H (2001) Objective measures of the efficacy of noninvasive positive-pressure ventilation in amyotrophic lateral sclerosis. Muscle Nerve 24:403–409
Brooks BR, Miller RG, Swash M, Munsat TL, World Federation of Neurology Research Group on Motor Neuron Diseases (2000) El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord 1:293–299
Morelot-Panzini C, Bruneteau G, Gonzalez-Bermejo J (2019) NIV in amyotrophic lateral sclerosis: the ‘when’ and ‘how’ of the matter. Respirology 24:521–530
Cedarbaum JM, Stambler N, Malta E, Fuller C, Hilt D, Thurmond B, Nakanishi A (1999) The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. BDNF ALS Study Group (Phase III). J Neurol Sci 169:13–21
Carlesimo GA, Caltagirone C, Gainotti G (1996) The mental deterioration battery: normative data, diagnostic reliability and qualitative analyses of cognitive impairment. The Group for the Standardization of the Mental Deterioration Battery. Eur Neurol 36:378–384
Appollonio I, Leone M, Isella V, Piamarta F, Consoli T, Villa ML, Forapani E, Russo A, Nichelli P (2005) The Frontal Assessment Battery (FAB): normative values in an Italian population sample. Neurol Sci 26:108–116
Abrahams S, Newton J, Niven E, Foley J, Bak TH (2014) Screening for cognition and behaviour changes in ALS. Amyotroph Lateral Scler Frontotemporal Degener 15:9–14
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370
Bjelland I, Dahl AA, Haug TT, Neckelmann D (2002) The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 52:69–77
Vanier M, Mazaux JM, Lambert J, Dassa C, Levin HS (2000) Assessment of neuropsychologic impairments after head injury: interrater reliability and factorial and criterion validity of the Neurobehavioral Rating Scale-Revised. Arch Phys Med Rehabil 81:796–806
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen OF, Pellegrino R, Viegi G, Wanger J, Force AET (2005) Standardisation of spirometry. Eur Respir J 26:319–338
Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH, Enright PL, Hankinson JL, Ip MS, Zheng J, Stocks J, Initiative ERSGLF (2012) Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J 40:1324–1343
Wilson SH, Cooke NT, Edwards RH, Spiro SG (1984) Predicted normal values for maximal respiratory pressures in caucasian adults and children. Thorax 39:535–538
Kendrick KR, Baxi SC, Smith RM (2000) Usefulness of the modified 0-10 Borg scale in assessing the degree of dyspnea in patients with COPD and asthma. J Emerg Nurs 26:216–222
Maldonado G, Greenland S (1993) Simulation study of confounder-selection strategies. Am J Epidemiol 138:923–936
Copper A, Weekes TJ (1983) Data, models, and statistical analysis, Rowman & Littlefield, pp 50-51.
Tysnes O-B (2008) Treatment of sialorrhea in amyotrophic lateral sclerosis. Acta Neurol Scand 188:77–81
Garuti G, Rao F, Ribuffo V, Sansone VA (2019) Sialorrhea in patients with ALS: current treatment options. Degener Neurol Neuromuscul Dis 9:19–26
Kontis TC, Johns ME (2006) Anatomy and physiology of the salivary glands. In: Bailay BJ (ed) Head and Neck Surgery Otolaryngology, 4th ed. Lippincott Williams & Wilkins, Philadelphia, pp 531–539
Chiò A, Ilardi A, Cammarosano S, Moglia C, Montuschi A, Calvo A (2012) Neurobehavioral dysfunction in ALS has a negative effect on outcome and use of PEG and NIV. Neurology 78:1085–1089
Dyspnea. Mechanisms, assessment, and management: a consensus statement. American Thoracic Society (1999) Am J Respir Crit Care Med 159:321-340
Manera U, Torrieri MC, Moglia C, Viglione M, Daviddi MAR, Matteoni E, Solero L, Palumbo F, Vasta R, Canosa A, D’Ovidio F, Focaraccio L, Mattei A, Mora G, Calvo A, Chiò A (2020) The role of arterial blood gas analysis (ABG) in amyotrophic lateral sclerosis respiratory monitorin. J Neurol Neurosurg Psychiatry 2020
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Research Ethics Committee of the University of Messina School of Medicine Hospital, Policlinico “G. Martino,” Messina, Italy. Written informed consent was obtained from all participants enrolled in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Russo, M., Bonanno, C., Profazio, C. et al. Which are the factors influencing NIV adaptation and tolerance in ALS patients?. Neurol Sci 42, 1023–1029 (2021). https://doi.org/10.1007/s10072-020-04624-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04624-x