Abstract
Introduction
Nerve biopsy has been widely used to investigate patients with peripheral neuropathy, and in many centers, it is still a useful diagnostic tool in this setting. In this study, we reviewed the histopathological spectrum of the nerve biopsies performed in our center in a 30-year period and we analyzed their relevance in the clinical setting.
Materials and methods
Retrospective analysis of the retrieved data was done for cases of nerve biopsies performed in our institute between 1988 and 2018. Surgical technique and histopathological analysis were done accordingly to standard protocol.
Results
Complete clinical and pathological data were available only for 717 cases. The procedure was generally safe, with only 0.3% superimposed infection. Main pathological results were “unspecific” axonal polyneuropathy (49.8%), vasculitis neuropathy (9.3%), acquired demyelinating neuropathy (8.9%), and Charcot-Marie-Tooth (8.2%). Considering clinical-neurophysiological suspicion of vasculitis, nerve biopsy confirmed the diagnosis in 60.9% of cases.
Discussion
In conclusion, for inherited neuropathies, we do not recommend this invasive procedure, but we strongly suggest a genetic test. Conversely, in vasculitic neuropathies or in dysimmune neuropathies not clearly confirmed by neurophysiological examination, nerve biopsy continues to represent a useful and irreplaceable tool.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nerve biopsy has been largely used in past decades for the diagnosis of peripheral nerve diseases. Its usefulness in the past was principally based on the presence in many neuropathies of peculiar lesions that make the diagnosis simple in some cases. Finding in a pathological specimen amyloid deposits or cell infiltrations, or identifying the pattern of axonal loss (i.e., whether it is homogeneous or not among fascicles), sometimes is crucial for the diagnosis of amyloidosis, vasculitis, or immune nerve diseases [1]. Moreover, some lesions are so specific, such as the presence of very large axons in giant axonal neuropathy [2], or myelin out-foldings in Charcot-Marie-Tooth 4B [3], that nerve biopsy could be conclusive for the final diagnosis. In addition, other technics and instruments, such as immunohistochemistry and electronic microscopy, could improve the possibility of nerve biopsy to clarify many doubts in diagnosis and clinical management [4,5,6].
On the other hand, nerve biopsy has low sensibility in most of the diseases that could be easily identified: amyloid was found in 13 of 19 patients in a report including AL patients [7], and pathological evidences of nerve vasculitis are present in a variable percentage (20–58%) in different papers [8, 9]. Moreover, diagnosis in many neuropathies is based principally on clinical and neurophysiological features, or on genetic tests, indicating nerve biopsy only as a supportive criterion [10, 11].
Another problem is that in literature there are few shared guidelines about technical and evaluation procedures and they are based on short cases: generally, the interpretation of nerve biopsy is limited to a small number of expert pathologists and/or neurologists [12].
Peripheral Nerve Society guidelines restricted the use of nerve biopsy to few specific cases: nerve vasculitis, infectious neuritis (i.e., for leprosy), neuropathies for metabolic or storage deposits (amyloidosis, glycogenosis), chronic inflammatory neuropathies, primary or secondary neoplasia, and some genetic diseases with peculiar lesions (i.e., MTMR2 with myelin out-foldings) [12].
In this paper, we reviewed the histopathological spectrum of the nerve biopsies performed in our center in a 30-year period and we analyzed their relevance in the clinical setting.
Methods
Surgical procedure
All patients had their biopsies performed in our institution under local anesthesia, between 1988 and 2018. Nerve biopsies were taken from the sural nerve, posterior to the lateral malleolus. Approximately 4–5 cm of nerve were resected. Skin closure was done using 5–7 interrupted nylon sutures. A pressure bandage was applied post-operatively, and patients were instructed to rest as much as possible for 48 hours after surgery. Sutures were removed by the surgeon 10–14 days post-operatively.
Nerve analysis
After removal, the nerve specimen was prepared without delay. Routinely, we divided it into two specimens [13]. The first specimen was frozen, then stained with hematoxylin and eosin for study of interstitial tissue, vessels, or presence of inflammatory cells; when necessary, other stainings were performed (i.e., Congo red for detecting amyloid) or direct immunofluorescence was carried out to confirm or characterize inflammatory cells (i.e., CD4 or CD8) or protein deposits (i.e., amyloid or light chains) [13, 14]. The second one was fixed in 2.5% glutaraldehyde in 0.05 M sodium cacodylate buffer for 1–3 hours, then post-fixed in 1% osmium tetroxide and embedded in a resin (epoxy resin) and in LR-white (London-resin white) for immuno-electron microscopy [13]. In order to visualize nerve fiber alterations (i.e., axonal degeneration, loss of small- and large-diameter fibers, axonal sprouts, demyelinating fibers, onion-bulb formations), transverse semi-thin sections were stained with toluidine blue then examined under a light microscope. If necessary, after staining with uranyl acetate and lead citrate, ultrathin sections were examined by electron microscopy (EM) [13]: ultrastructural examination was valuable for a thorough study of a peripheral nerve and was usually carried out on cross sections, sometimes on longitudinal sections to study specific structures, such as nodes of Ranvier, intra-axonal mitochondria, etc. Nerve myelinated fiber density (on semi-thin sections) and unmyelinated fiber density (on ultrathin sections) were evaluated [13]. Teased nerve fiber analysis (dissociation of individual myelinated nerve fibers) was also performed when necessary [13].
Statistical analysis
Fisher’s exact test was used for comparing frequencies. The significance level was set at p < 0.05.
Results
Surgical procedure
Sural nerve biopsy was performed in 932 patients in the examined period. Complete clinical and pathological data were available only for 717 cases: 434 were male (60.5%) with a mean age at procedure of 54.9 years, and 283 were female (39.5%) with a mean age at procedure of 54.5 years. Only 5 biopsies (0.7%) were technically not satisfying because no fascicle was identified into.
In the first 16 years (1988–2003), 482 biopsies (67.2%) were performed, while the remaining 235 (32.8%) were done in the following 15 years (2004–2018): a great proportion (388 cases, 54.1%) of patients underwent biopsy in a 8-year period (1998–2005) (Fig. 1).
Age at biopsy varied consistently during the observation period (Table 1): generally, a high proportion of patients with young age underwent nerve biopsy in the 1988–2004 period (Table 1).
Nerve biopsy was generally a safe procedure: only in 2/717 (0.3%) patients we experienced a superimposed infection treated with antibiotic therapy. Reduced sensation in the distribution of the sural nerve, compared with the contralateral leg, was reported by 132/717 (18.4%) patients examined, although this was variable; only 72/717 (10%) reported pain.
Nerve analysis
Major pathological findings are summarized in Table 2. Sural nerve biopsy was diagnostic for a defined neuropathy in about a third of cases (235/717, 32.8%): main biopsy results are summarized in Table 3.
Considering a specific clinical suspicion, we observed a confirmation of clinical-neurophysiological diagnosis (or highly supportive information) for different conditions in the following proportion:
Vasculitic neuropathy: 67/110 (60.9%). Pathological findings were pathognomonic (fibrinoid necrosis with inflammatory infiltrates) or supportive (inflammatory infiltrates, asymmetrical axonal loss, sub-endoneurial edema, perineural microfasciculation). Direct immunofluorescence to characterize infiltrates was performed in 34/67 (50.7%) [15, 16] (Supplementary Fig. 1).
Amyloidotic neuropathy: 17/43 (39.5%). Pathological findings revealed amyloid deposits with positive Congo red staining. Direct immunofluorescence with anti-TTR or anti-light-chain (kappa and lambda) antibodies was available for 8/17 (47.0%), confirming TTR deposits in 7 cases and AL in the remaining one [17, 18] (Supplementary Fig. 2).
Chronic inflammatory demyelinating polyneuropathy (CIDP): 43/139 (30.9%). Pathological findings were heterogeneous, including axonal loss (with symmetric distribution or not), onion bulbs, inflammatory infiltrates, fibers with thin myelin sheath, and segmental demyelinations [10] (Supplementary Fig. 3).
Anti-MAG-associated neuropathy: 21/25 (84.0%). Pathological findings were heterogeneous, including variable degree of axonal loss, myelin out-foldings, widening myelin lamellae, and IgM deposition on the myelin sheath [14] (Supplementary Fig. 4).
In single cases, nerve biopsy showed specific clues for final diagnosis, namely giant axonal neuropathy [2], hereditary neuropathy with liability to pressure palsies [19], Charcot-Marie-Tooth 4B [3], Charcot-Marie-Tooth 2E [20], light-chain deposition disease [21], and isolated lymphoma of the peripheral nerve [22].
Discussion
Sural nerve biopsy has been widely used in our center in the last 30 years as a useful tool to diagnose peripheral neuropathy [14, 16,17,18,19,20,21,22,23,24,25]. The surgical procedure has been confirmed to be safe with only 0.3% of cases reporting serious side effects. In about 20% of patients, a different degree of hypoesthesia along the sural nerve sensory distribution was reported: probably, this low percentage is influenced by the underlying peripheral neuropathy that could affect the contralateral sural nerve too. Furthermore, pain that could worsen quality of life was reported by only 10% of the patients [26].
Considering the total amount of biopsies, a great proportion (67.2%) was done in the first 16 years; in our opinion, this data was influenced by the changing of indications during the years. Furthermore, about half of the biopsies was done only in 8 years (1998–2005), when the biopsy technique was diffuse and easy to perform, and the indications were wider.
Between 1988 and 2004, 25.7% of patients were 40 years old or younger compared with only 13.0% in the following period (p = 0.004): obviously, this result is explained by patients with inherited neuropathy that, before the diffusion of genetic tests, almost always underwent nerve biopsy [27]. Furthermore, also the number of biopsies diagnostic for CMT was significantly slightly higher in this period (1988–2004) if compared with the following one (2005–2018), confirming our hypothesis (Table 3).
Considering pathology, about 18% of the samples were found to be unremarkable or not evaluable, and the main conclusion (about 50%) was “unspecific” axonal neuropathy: this “diagnosis” showed a similar frequency in both periods examined (1988–2004 vs 2005–2018); conversely, “normal” pathological findings were less frequently observed in the last years (Table 3), probably indicating a more strict indication for the procedure.
However, similarly to other studies [28], we reached a pathological diagnosis in a quarter of cases. The most frequent diagnosis was vasculitis (9.3%), confirming this strong indication for nerve biopsy [29, 30]. Conversely, amyloidosis, which is also considered as a possible indication, was not so frequently found (2.7%): in the last years, even if this diagnosis for the genetic form was slightly more frequent if compared with that of the past (Table 3), we understood that negative biopsies are quite common in late-onset amyloidosis and do not exclude the diagnosis [17].
Considering the utility of nerve biopsy in confirming a clinical-electrophysiological suspicion, the highest rate of success was observed for vasculitis (60.9%); however, also in this condition, negative pathological findings do not exclude the diagnosis [15]. Diagnosis of vasculitis was also more frequent in the last years (Table 3), further confirming a more strict indication for nerve biopsy.
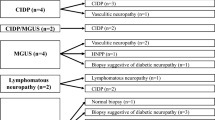
Regarding other inflammatory/dysimmune neuropathies, CIDP was diagnosed in about 30% of cases: pathological aspects of this disease are heterogeneous and could explain the data [31]. Considering all cases with pathological diagnosis of CIDP, in about a third of these (13/43, 30.2%), neurophysiological results were uncertain, so nerve biopsy turned out to be a crucial tool to confirm diagnosis; conversely, cerebrospinal fluid examination was available only for half of the patients (22/43, 51.2%), and it showed an increase of proteins in only a third of cases (7/22, 31.8%).
On the other hand, 84% of biopsies showed pathological findings confirmatory for anti-MAG neuropathy, but in these cases, the titer of antibodies led to the diagnosis [32]. Anti-MAG neuropathy was more frequently diagnosed in the last period (Table 3), considering the utility of nerve biopsy to detect uncommon mechanisms of nerve damage [14].
Finally, for single cases of rare diseases, nerve biopsy determined the diagnosis and therefore was the main diagnostic tool [33,34,35,36,37,38,39].
In conclusion, also in our cohort, we confirmed that sural nerve biopsy is a safe procedure. However, under suspicion of a genetic disease, such as CMT or amyloidosis, we do not recommend this invasive procedure, but we strongly suggest genetic tests directly. Conversely, in inflammatory neuropathies, such as vasculitis, or in dysimmune neuropathies not clearly confirmed by neurophysiological examination, nerve biopsy continues to represent a useful and irreplaceable tool.
References
Dyck PJ, Dyck PJB, Engelstad J (2005) Pathologic alterations of nerves. In: Dyck PJ, Thomas PK (eds) Peripheral neuropathy. Elsevier Saunders, Philadelphia, pp 747–751
Sabatelli M, Bertini E, Servidei S, Fernandez E, Magi S, Tonali P (1992) Giant axonal neuropathy: report on a case with focal fiber loss. Acta Neuropathol 83(5):543–546
Gambardella A, Bolino A, Muglia M, Valentino P, Bono F, Oliveri RL, Sabatelli M, Brancolini V, Van Broeckhoven C, Romeo G, Devoto M, Quattrone A (1998) Genetic heterogeneity in autosomal recessive hereditary motor and sensory neuropathy with focally folded myelin sheaths (CMT4B). Neurology 50(3):799–801
Mrak RE (2002) The Big Eye in the 21st century: The role of electron microscopy in modern diagnostic neuropathology. J Neuropathol Exp Neurol 61(12):1027–1039
Gabriel JM, Erne B, Bernasconi L, Tosi C, Probst A, Landmann L, Steck AJ (1998) Confocal microscopic localization of anti-myelin-associated glycoprotein autoantibodies in a patient with peripheral neuropathy initially lacking a detectable IgM gammopathy, Acta. Neuropathol 95(5):540–546
Gabriel CM, Howard R, Kinsella N, Lucas S, McColl I, Saldanha G, Hall SM, Hughes RA (2000) Prospective study of the usefulness of sural nerve biopsy. J Neurol Neurosurg Psychiatry 69(4):442–446
Adams D, Lozeron P, Theaudin M, Denier C, Fagniez O, Rerat K, Signate A, Corcia P, Lacroix C (2011). Varied patterns of inaugural light-chain (AL) amyloid polyneuropathy: a monocentric study of 24 patients. Amyloid 18 Suppl 1:98-100 doi: https://doi.org/10.3109/13506129.2011.574354036
Dyck PJ, Benstead TJ, Conn DL, Stevens JC, Windebank AJ, Low PA (1987). Nonsystemic vasculitic neuropathy. Brain 110 (Pt 4):843-853
Said G, Lacroix-Ciaudo C, Fujimura H, Blas C, Faux N (1988) The peripheral neuropathy of necrotizing arteritis: a clinicopathological study. Ann Neurol 23(5):461–465
Joint Task Force or the EFNS and the PNS. European Federation of Neurological Societies/Peripheral Nerve Society (2010) Guidelines on the management of chronic inflammatory demyelinating polyradiculoneuropathy: report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society. J Peripher Nerv Syst 15(1):1–9
Stojkovic T (2016) Hereditary neuropathies: an update. Rev Neurol (Paris) 172(12):775–778
Sommer CL, Brandner S, Dyck PJ, Harati Y, LaCroix C, Lammens M, Magy L, Mellgren SI, Morbin M, Navarro C, Powell HC, Schenone AE, Tan E, Urtizberea A, Weis J, Peripheral Nerve Society (2010) Peripheral Nerve Society guideline on processing and evaluation of nerve biopsies. J Peripher Nerv Syst 15(3):164–175. https://doi.org/10.1111/j.1529-8027.2010.00276.x
Vallat JM, Funalot B, Magy L (2011) Nerve biopsy: requirements for diagnosis and clinical value. Acta Neuropathol 121:313–326. https://doi.org/10.1007/s00401-011-0804-4
Luigetti M, Conte A, Montano N, Del Grande A, Madia F, Lo Monaco M, Laurenti L, Sabatelli M (2012) Clinical and pathological heterogeneity in a series of 31 patients with IgM-related neuropathy. J Neurol Sci 319(1-2):75–80. https://doi.org/10.1016/j.jns.2012.05.012
Said G, Lacroix C (2005) Primary and secondary vasculitic neuropathy. J Neurol 252(6):633–641
Luigetti M, Del Grande A, Romano A, Sabatelli M (2013) Uncommon pathological findings in sural nerve biopsy from a patient with Churg-Strauss related multiple mononeuropathy. Acta Reumatol Port 38(4):286–289
Luigetti M, Conte A, Del Grande A, Bisogni G, Madia F, Lo Monaco M, Laurenti L, Obici L, Merlini G, Sabatelli M (2013) TTR-related amyloid neuropathy: clinical, electrophysiological and pathological findings in 15 unrelated patients. Neurol Sci 34(7):1057–1063. https://doi.org/10.1007/s10072-012-1105-y
Luigetti M, Papacci M, Bartoletti S, Marcaccio A, Romano A, Sabatelli M (2012) AL amyloid neuropathy mimicking a chronic inflammatory demyelinating polyneuropathy. Amyloid 19(1):53–55. https://doi.org/10.3109/13506129.2011.650247
Luigetti M, Del Grande A, Conte A, Lo Monaco M, Bisogni G, Romano A, Zollino M, Rossini PM, Sabatelli M (2014) Clinical, neurophysiological and pathological findings of HNPP patients with 17p12 deletion: a single-centre experience. J Neurol Sci 341(1-2):46–50. https://doi.org/10.1016/j.jns.2014.03.046
Luigetti M, Padua L, Coraci D, Fabrizi GM, Romano A, Sabatelli M (2016) Nerve ultrasound in CMT2E/CMT1F due to NEFL mutation: confirmation of an axonal pathology. Clin Neurophysiol 127(9):2990–2991. https://doi.org/10.1016/j.clinph.2016.06.024
Luigetti M, Frisullo G, Laurenti L, Conte A, Madia F, Profice P, Batocchi AP, Montano N, Tarnani M, Tonali PA, Sabatelli M (2010) Light chain deposition in peripheral nerve as a cause of mononeuritis multiplex in Waldenström’s macroglobulinaemia. J Neurol Sci 291(1–2):89–91. https://doi.org/10.1016/j.jns.2010.01.018
Del Grande A, Sabatelli M, Luigetti M, Conte A, Granata G, Rufini V, Del Ciello A, Gaudino S, Fernandez E, Hohaus S, Coli A, Lauriola L (2014) Primary multifocal lymphoma of peripheral nervous system: case report and review of the literature. Muscle Nerve 50(6):1016–1022. https://doi.org/10.1002/mus.24354
Magi S, Sabatelli M, Mignogna T, Porcu C, Tonali P (1992) Acute axonal idiopathic polyneuropathy: a Guillain-Barré syndrome variant? Ital J Neurol Sci 13(6):481–486
Sabatelli M, Mignogna T, Lippi G, Servidei S, Manfredi G, Ricci E, Bertini E, Lo Monaco M, Tonali P (1994) Autosomal recessive hypermyelinating neuropathy. Acta Neuropathol 87(4):337–342
Luigetti M, Fabrizi GM, Bisogni G, Romano A, Taioli F, Ferrarini M, Bernardo D, Rossini PM, Sabatelli M (2016) Charcot-Marie-Tooth type 2 and distal hereditary motor neuropathy: clinical, neurophysiological and genetic findings from a single-centre experience. Clin Neurol Neurosurg 144:67–71. https://doi.org/10.1016/j.clineuro.2016.03.007
Solders G (1988) Discomfort after fascicular sural nerve biopsy. Acta Neurol Scand 77(6):503–504
Pareyson D (1999) Guidelines for the diagnosis of Charcot-Marie-Tooth disease and related neuropathies. Ad hoc Working Group of the Peripheral Nervous System Study Group, Italian Neurological Society. Ital J Neurol Sci 20(4):207–216
Deprez M, Ceuterick-de Groote C, Schoenen J, Reznik M, Martin JJ (2000) Nerve biopsy: indications and contribution to the diagnosis of peripheral neuropathy. The experience of the Born Bunge Foundation University of Antwerp and University of Liege between 1987 and 1997. Acta Neurol Belg 100(3):162–166
Collins MP, Hadden RD (2017) The nonsystemic vasculitic neuropathies. Nat Rev Neurol 13(5):302–316. https://doi.org/10.1038/nrneurol.2017.42
Kulshreshtha D, Malhotra KP, Maurya PK, Singh AK, Thacker AK, Husain N (2017) Nerve biopsy in Indian patients with mononeuropathy multiplex of undetermined etiology. Muscle Nerve 55(1):23–27. https://doi.org/10.1002/mus.25179
Said G, Krarup C (2013) Chronic inflammatory demyelinative polyneuropathy. Handb Clin Neurol 115:403–413. https://doi.org/10.1016/B978-0-444-52902-2.00022-9
Dalakas MC (2018) Advances in the diagnosis, immunopathogenesis and therapies of IgM-anti-MAG antibody-mediated neuropathies. Ther Adv Neurol Disord 11:1756285617746640. https://doi.org/10.1177/1756285617746640
Luigetti M, Fabrizi GM, Madia F, Ferrarini M, Conte A, Del Grande A, Tasca G, Tonali PA, Sabatelli M (2010) A novel HSPB1 mutation in an Italian patient with CMT2/dHMN phenotype. J Neurol Sci 298(1–2):114–117. https://doi.org/10.1016/j.jns.2010.09.008
Luigetti M, Taroni F, Milani M, Del Grande A, Romano A, Bisogni G, Conte A, Contaldo I, Mercuri E, Sabatelli M (2014) Clinical, electrophysiological and pathological findings in a patient with Charcot-Marie-Tooth disease 4D caused by the NDRG1 Lom mutation. J Neurol Sci 345(1–2):271–273. https://doi.org/10.1016/j.jns.2014.07.042
Ciotti P, Luigetti M, Geroldi A, Capponi S, Pezzini I, Gulli R, Pazzaglia C, Padua L, Massa R, Mandich P, Bellone E (2014) A novel LITAF/SIMPLE mutation within a family with a demyelinating form of Charcot-Marie-Tooth disease. J Neurol Sci 343(1–2):183–186. https://doi.org/10.1016/j.jns.2014.05.029
Sabatelli M, Quaranta L, Madia F, Lippi G, Conte A, Lo Monaco M, Di Trapani G, Rafi MA, Wenger DA, Vaccaro AM, Tonali P (2012) Peripheral neuropathy with hypomyelinating features in adult-onset Krabbe’s disease. Neuromuscul Disord 12(4):386–391
Sabatelli M, Mignogna T, Lippi G, Servidei S, Zollino M, Padua L, Lo Monaco M, De Armas L, Mereu ML, Tonali P (1998) Hereditary motor and sensory neuropathy with deafness, mental retardation, and absence of sensory large myelinated fibers: confirmation of a new entity. Am J Med Genet 75(3):309–313
Sabatelli M, Mignogna T, Lippi G, Porcu C, Tonali P (1996) Intramyelinic edema in chronic inflammatory demyelinating polyneuropathy. Clin Neuropathol 15(1):17–21
Luigetti M, Primiano G, Bisogni G, Cuccagna C, Carrozzo R, Obici L, Bernardo D, Sancricca C, Servidei S (2018) Progressive axonal polyneuropathy in a mitochondrial disorder: an uncommon association with familial amyloid neuropathy. Amyloid 25(4):261–262. https://doi.org/10.1080/13506129.2018.1506919
Acknowledgments
We thank the patients for their participation in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
ESM 1 (DOCX 2987 kb)
Rights and permissions
About this article
Cite this article
Luigetti, M., Di Paolantonio, A., Bisogni, G. et al. Sural nerve biopsy in peripheral neuropathies: 30-year experience from a single center. Neurol Sci 41, 341–346 (2020). https://doi.org/10.1007/s10072-019-04082-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-019-04082-0