Abstract
Objective
To investigate clinical risk factors that were associated with gender differences in thrombolysis therapy in stroke patients with incidence of obesity.
Method
Retrospective data of obese acute ischemic stroke patients were extracted from a stroke registry between January 2010 and June 2016. Gender differences in exclusion from rtPA or thrombolysis therapy were determined following an adjustment for differences in demographics, clinical risk factors using multiple regression analysis. Significant interactions between variables in the regression models were determined using variance inflation factors.
Results
A total of 1105 obese stroke patients were admitted, 549 were excluded from rtPA of which 51.7% were males and 48.3% were females. Among obese male stroke patients, age > 80 years (OR = 1.029, 95% CI, 1.005–1.054, P = 0.016), a history of peripheral vascular disease (OR = 3.008, 95% CI, 0.989–9.153, P = 0.052), and an elevated diastolic blood pressure (OR = 1.018, 95% CI, 1.001–1.035, P = 0.038) were associated with exclusion from rtPA therapy. In obese female stroke patients, coronary artery disease was associated with exclusion from rtPA (OR = 2.478, 95% CI, 1.270–4.836, P = 0.008) while antihypertensive therapy was associated with inclusion for rtPA (OR = 0.326, 95% CI, 0.139–0.764).
Conclusion
Elderly obese male stroke patients with elevated diastolic blood pressure, history of peripheral vascular disease, and obese female stroke patients with a history of coronary artery disease were more likely to be excluded from rtPA.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Irrespective of gender, obesity is a major health risk factor for stroke and more than 68% of adults in the USA are classified as overweight or obese [1]. Obesity leads to an estimated average of 238,454 deaths annually [2] and represents a major predictor of morbidity and mortality in both male and female stroke patients [3]. In general, gender and incidence of stroke have been investigated extensively [4,5,6]. Findings from these studies indicate that the incidence of stroke with age-specific adjustment is greater in men [7], while the overall lifetime risk of stroke is greater in women due to their longer average life expectancy [8,9,10]. Additionally, worse outcomes have been reported in women [11, 12]. Moreover, the relationship between obesity and the risk for ischemic stroke in both men and women has been investigated [13, 14]. Findings from these studies resulted in the recommendation for the treatment of obesity for primary and secondary prevention of stroke [15], indicating an association of gender and obesity with stroke prevalence and outcome.
While the relationship between obesity and the risk of stroke has been investigated extensively, the effect of clinical risk factors in obese stroke patients undergoing thrombolysis therapy has not been extensively studied. It is not known, for example, whether clinical risk factors in obese stroke patients is associated with the exclusion or inclusion of more obese male or female stroke patients from thrombolysis therapy. Obesity is assessed based on BMI and represents an independent risk factor for stroke [16]. It is the best predictor of stroke in women and the only significant predictor of stroke in men [17]. Although obesity is not an exclusion factor for thrombolysis therapy, specific clinical and demographic factors in obese stroke patients could affect the use of thrombolysis therapy and influence outcomes differently in obese male or female stroke population. For example, a combination of BMI, age stroke severity, and several clinical risk factors may act alone or in synergy to exclude more women or men from thrombolysis in stroke patients with obesity.
In an acute ischemic stroke population, women are less likely to receive thrombolysis treatment than men [18, 19]. The severity of stroke is worse in women than in men, but the existing gender difference is attenuated following thrombolysis therapy [20]. This suggests that there is a greater benefit of thrombolytic therapy in women when compared with men [9, 21, 22]. Whether such a benefit also persists for obese stroke women when compared with men is yet to be investigated. If a gender difference also persists within an obese stroke population, one possibility is that the proportion of clinical risk factors in obese male and female stroke patients is different such that more obese male stroke patients are excluded from rtPA when compared with females. This is because more clinical risk factors may be associated with the exclusion of more obese stroke males when compared with females. We tested this hypothesis in a population of obese male acute ischemic stroke patients and compared our results with obese female acute ischemic stroke patients. First, we identified demographic and clinical risk factors that are associated with gender differences in the exclusion of obese male and female stroke patients from thrombolysis therapy. Second, we determined demographic and clinical risk factors that are associated with exclusion of male or female ischemic stroke patients with incidence of obesity from rtPA. An increase in the use of rtPA in obese stroke population will require the identification of specific baseline clinical risk factors in males or females that can be targeted to improve the use of rtPA and treatment outcomes. The current study investigated clinical risk factors that can be managed to eliminate gender differences and improve the use of rtPA in the care of acute ischemic stroke population with obesity.
Methods
Data collection
Retrospective data was collected from the stroke registry of the Greenville Health Care System (GHS) between January 2010 and June 2016. The registry contributes to the Get with The Guidelines (GWTG)–Stroke, a national registry of the American Heart Association and American Stroke Association, which represents a risk model that provides clinicians with a validated and practical bedside instrument for the stratification of mortality risk. The GHS registry has been described in previous studies [4, 9, 23,24,25,26,27,28,29,30]. A stroke neurologist determined whether the patient met the criteria for the description of acute stroke and retrieved. Stroke events were classified as ischemic stroke, transient ischemic attack, intracerebral hemorrhage, or subarachnoid hemorrhage based on the classification of stroke from the Classification of Cerebrovascular Diseases III [31]. In this study, we used data for acute ischemic stroke with incidence of obesity for our data analysis. All data for the patient’s demographics, clinical variables that were used for the study was abstracted by a nursing practitioner. Baseline clinical risk factors were extracted from documented patient medical history retrieved from medical records during admission to the GHS stroke unit. Demographic variables including age, race/ethnicity, and gender were collected. Data on admission date, prior medication use history including cholesterol reducers, antihypertensive and diabetes medications, pre-stroke and post-stroke ambulatory statuses, and past medical history were also collected. We abstracted data on clinical risk factors from patients’ medical records that include coronary artery disease (CAD), carotid stenosis, diabetes, dyslipidemia, atrial fibrillation/flutter, congestive heart failure (CHF), hypertension, transient ischemic attack (TIA) or previous stroke, smoking history, peripheral vascular disease (PVD), depression, evidence of drug use, chronic renal problems, and history of smoking. Data on laboratory analysis of patients’ blood or plasma samples for total serum cholesterol, blood sugar and serum creatinine concentrations, systolic, diastolic pressures, and BMI were also collected. Data were collected for patients within 24 h of stroke onset and 4.5 h rtPA protocol. Collected data were examined under quality control checks using established protocol to ascertain the quality of the data and to ensure against several types of errors including the interpretation or coding of data. Approval for this study was obtained from the ethics committee of the Greenville Health system in 2017. Since this is a retrospective data analysis, all data were de-identified, and the study did not involve patients and no consent was required.
Data analysis
All statistical analyses were performed utilizing SPSS Statistics Software version 24 (Chicago, IL). A univariate analysis was used to determine factors that were associated with receipt of recombinant tissue plasminogen activator (rtPA) in the study population. Descriptive statistics were calculated for the demographic and clinical characteristics of patients. All continuous variables are represented as mean (standard deviation) and comparisons between groups were made using Student’s t test. All discrete variables are represented as number (percentage) and comparisons between groups were made using Pearson’s chi-squared analyses. Univariate analysis was repeated to determine factors associated with receipt of rtPA in the separate rtPA/non-rtPA subgroups and by male and female gender.
Multivariate analysis using a stepwise conditional logistic regression was performed to determine demographic and clinical characteristics associated with exclusion from rtPA administration in the obese stroke population as well as in the male and female subgroups. The predictor variable for each of our logistic regression model was selected by stepwise regression and variables with P < 0.05 were retained in the model. For the goodness of fit test of how well our model fits the data, we used the Hosmer-Lemeshow test that reveals the strength of our prediction models. The discrimination capability for each of our fitted logistic models was determined using the receiver operating characteristic (ROC) curve and quantified by area under the ROC curve (AUC). Multicollinearity and significant interactions between independent variables were examined using variance inflation factors to confirm independence of variables included in the regression models. All statistical analysis was performed using SPSS Statistics Software Version 24.0, and a p value of less than 0.05 was used to determine significance.
Results
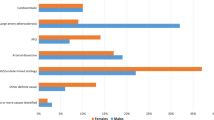
Fifty-one percent (n = 571) of the obese stroke population (n = 1105) were male while 48 % (n = 534) were female. The baseline demographic and clinical characteristics of male and obese female stroke patients are presented in Table 1. As shown in Table 1, excluded females were older (66.52 ± 15.9 years vs 64.28 ± 13.2 years, P = 0.001) than males and presented with a higher body mass index (BMI: 32.7 ± 7.20 vs 30.8 ± 4.95, P < 0.001). Pre-rtPA treatment clinical risk factors including atrial fib/flutter, carotid artery stenosis, diabetes, dyslipidemia, family history of obesity, heart failure, hypertension, previous stroke, previous TIA, peripheral vascular disease, and chronic renal problem were not significantly different between male and obese female stroke patients. Table 1 further reveals that patients taking cholesterol reducer, antihypertensive and diabetic medications were not significantly different between obese male and female stroke patients. The laboratory results indicate that cholesterol level was significantly higher in females (177.6 ± 50.6 mg/dl vs 168.2 ± 48.2 mg/dl, P = 0.003), while serum creatinine (1.38 ± 1.03 mg/dl vs 1.21 ± 1.16 mg/dl, P = 0.009) and diastolic blood pressure (85 ± 19 mmHg vs 82 ± 20 mmHg, P = 0.011) were significantly higher in males. Between females and males, blood glucose (156.3 ± 96.4, g/dl vs 153.8 ± 86.9, P = 0.649), and systolic blood pressure (151 ± 29 mmHg vs 153 ± 29 mmHg, P = 0.368) were not significantly different. In summary, a significant and higher number of obese stroke females presented with coronary artery disease, depression, a more severe stroke based on NIHSS baseline, whereas more obese stroke males presented with history of drug abuse and smoking.
The characterization of obese stroke patients by rtPA status and gender is shown in Table 2. A total of 284 male and 265 female obese stroke patients were excluded from rtPA. Obese female and male patients acute ischemic stroke patients excluded from rtPA were not significantly different in age (67.8 ± 15.72 vs 66.2 ± 13.30, P = 0.199). Females were more likely to present with a history of depression (28.3% vs 19.0%, P = 0.010) and a higher BMI (32.5 ± 8.05 vs 30.6 ± 4.52, P = 0.001), while males were more likely to have a history of drug abuse (12.3% vs 3.0%, P < 0.001) and elevated diastolic blood pressure (84 ± 22 vs. 80 ± 22, p = 0.032). Obese female stroke patients included for rtPA were more likely to be depressed (27.1% vs 15.3%, P = 0.001), have higher NIH scores (10.81 ± 8.33 vs 9.30 ± 7.7, P = 0.026), have a higher risk of mortality (7.1 ± 9.68 vs 5.1 ± 5.84 P = 0.020), higher BMI (32.9 ± 6.26 vs 31.0 ± 5.35, P < 0.001), and atrial fibrillation (16.0% vs 9.8%, P = 0.028) while male patients were more likely to present with coronary artery disease (36.2% vs 17.5%, P = 0.001), a history of smoking (32.1% vs 20.8%, P = 0.003) and drug abuse (10.5% vs 1.9%, P < 0.001). For the laboratory analysis, female patients were more likely to have elevated serum cholesterol (178.2 ± 52.1 mg/dl vs 166.9 ± 44.4 mg/dl, P = 0.007), while male patients were more likely to have elevated serum creatine (1.33 ± 1.06 mg/dL vs 1.09 ± 0.98 mg/dl, P = 0.005).
The results of the stepwise conditional logistic regression model for the exclusion or inclusion for rtPA in the obese stroke population without sorting by gender are presented in Table 3. Following adjustment, many of the established significant associations with gender in the univariate analysis were attenuated and became non-significant except for BMI (OR = 1.028, 95% CI, 1.000–1.057, P = 0.048), which was associated with exclusion, while antihypertensive medication (OR = 0.558, 95% CI, 0.330–0.946, P = 0.03), was significantly associated with inclusion for rtPA. The receiver operating characteristics (ROC) curve for the whole obese stroke population model is presented in Fig. 1. The discriminating capability of the model was good as shown by the ROC curve, with area under the curve (AUROC = 0.648, 95% CI; 0.600–0.697, P < 0.001). The ROC curve (Fig. 1) and the corresponding AUC reveal a 64.8% predictive capability of our model to discriminate clinical variables associated with an exclusion or inclusion from rtPA.
The area under the ROC curve quantifies the overall ability of the model to discriminate between clinical risk factors with inclusion and those with exclusion from thrombolysis therapy in the whole obese stroke population. The discriminating ability of the model was good with area under the curve (AUROC = 0.648,95% CI, 0.600–0.697, P < 0.001). The model shows a strong predictive capability of 64.8% to discriminate variables associated with exclusion or inclusion for rtPA in the obese stroke population
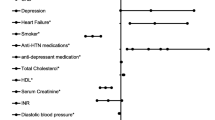
Further logistic regression was performed to focus primarily on the obese stroke patient subgroup separately to identify clinical and demographic risk factors that excluded obese male stroke patients from thrombolysis therapy (Table 4). As shown in Table 4, after adjustment, obese male stroke patients who were older (> 80) (OR = 1.029, 95% CI, 1.005–1.054, P = 0.016), presented with peripheral vascular disease (OR = 3.008, 95% CI, 0.989–9.153, P = 0.052), and had a higher diastolic blood pressure (OR = 1.018, 95% CI, 1.001–1.035, P = 0.038), were more likely to be excluded from rtPA. Figure 2 presents the area under the curve (AUROC = 0.675;95% CI, 0.600–0.697, p < 0.001), indicating that the discriminating ability of the regression model was good with a 67.5% predictive ability to discriminate clinical risk factors associated with exclusion and inclusion in obese male stroke patients.
The area under the ROC curve quantifies the overall ability of the model to discriminate between clinical risk factors with inclusion and those with exclusion from thrombolysis therapy in obese male stroke population. The discriminating ability of the regression model was good (67.5%). Area under the curve (AUROC = 0.675;95% CI, 0.600–0.697)
Obese female stroke patients (Table 5) were more likely to be excluded if they presented with coronary artery disease (OR = 2.478, 95% CI, 1.270–4.411, P = 0.008), and were more likely to receive rtPA if they were taking antihypertensive medications (OR = 0.326, 95% CI, 0.139–0.764, P = 0.010). The disseminative ability of our model was very good with a 72.9% predictive ability to discriminate clinical risk factors associated with exclusion and inclusion in obese female stroke patients. The area under the curve (AUROC = 0.729;(95% CI, 0.665–0.6793, P < 0.001) is presented in Fig. 3.
The area under the ROC curve quantifies the overall ability of the model to discriminate between clinical risk factors with inclusion and those with exclusion from thrombolysis therapy in the obese female stroke population model. The discriminating ability of the regression model was very good (72.9%) with area under the curve (AUROC = 0.729;95% CI, 0.665–0.6793, P < 0.001)
Discussion
In this study, we found that among obese female stroke patients, coronary artery disease was associated with exclusion from receiving rtPA while being on antihypertensive medication was associated with inclusion for rtPA. After adjusting for age and comorbidities in the whole obese stroke population without sorting by gender, we found that BMI was significantly associated with exclusion from rtPA, while being on antihypertensive medication was significantly associated with inclusion for rtPA treatment. These results changed after we focused the analysis to either the male or female obese stroke population.
In the obese male stroke patients, increasing age, elevated diastolic blood pressure, and the presence of peripheral vascular disease were each associated with exclusion from rtPA; these associations were not shown in the female-only or overall obese stroke populations. In the obese female stroke patients, the association of antihypertensive treatment with inclusion for rtPA that was observed in the obese stroke population did not disappear, but the effect of BMI was attenuated. Moreover, coronary artery disease was the only clinical risk factor that was associated with exclusion from thrombolysis therapy in the female obese stroke patients after the adjusted analysis.
We found that age was significantly different between obese males and females in the group of patients who received rtPA, with women being older on average, but was not significantly different in the no rtPA group in the univariate analysis. In our adjusted analysis, obese male stroke patients increasing were significantly associated with exclusion from rtPA therapy in the obese male-only stroke patient population, but not in the female-only or overall obese stroke patient populations. In stroke studies, a pattern towards a higher rate of exclusion for women has been reported [32,33,34], while other studies reported similarities in the rates for the administration of rtPA for both men and women stroke patients [35, 36]. Gender differences in pre-treatment risk factors are known to cause treatment delays [37, 38]. Therefore, it is also possible that such delays in obese elderly male stroke patients, especially in the pretreatment management of comorbidities such as diastolic blood pressure and peripheral vascular disease, could account for the higher exclusion rate of obese male stroke patients in the current study.
In general, obesity is evaluated on the basis of BMI values; it is an independent risk factor for stroke [16], a prominent predictor of stroke in women and a sole predictor of stroke in men [17]. In our adjusted analysis, the effect of BMI disappeared while the effect of older age significantly excluded more obese male stroke patients than females from thrombolysis therapy. While obesity itself is not an exclusion factor for thrombolysis therapy, our results reveal that a demographic factor such as age and specific baseline clinical risk factors including diastolic blood pressure and peripheral vascular disease in obese stroke patients, rather than obesity alone could exclude more obese male stroke patients than females from thrombolysis therapy. These findings suggest that the synergy between age as a demographic variable and clinical risk factors in obese stroke patients may act to exclude more men than women from thrombolysis therapy. Our findings suggest age-associated differences in pretreatment comorbidities between obese male and female stroke patients.
The established gender difference in this study is comparable with other studies that investigated gender differences in stroke [4, 10, 24, 39,40,41]. We found that more obese male than female stroke patients were excluded from thrombolysis therapy. In obese stroke patients, we did not find a significant gender difference in race or medical history of dyslipidemia, heart failure, hypertension, previous stroke, previous TIA, and chronic renal problem. Other studies reported that men stroke patients are more likely to present with a history of heart disease [41], prevalence of smoking [42], and incidence of dyslipidemia [43], while women are more likely to present with atrial fibrillation [44]. In our study, increasing age, an elevated diastolic blood pressure and a history of peripheral vascular disease were associated with exclusion from rtPA therapy in obese males, while a history of coronary artery disease was associated with exclusion from rtPA in obese females.
Several limitations should be considered in interpreting the findings of this study. This is a retrospective data analysis with a tendency of bias in selection. Moreover, there is a potential of incorrect categorization of obesity which could inaccurately affect the relationship between obesity and stroke in our data analysis. Additionally, our study is from one institution which may inhibit the generalization of the results because of the possibility of a selection bias. Data for anthropometric measures including body fat distribution and abdominal obesity should have been included in a study that evaluates obesity and stroke but was not available in our dataset. However, in this study, we determined whether clinical risk factors that excluded men and women from thrombolysis therapy differ in a stroke population with obesity. Our findings indicate that adjusted odds ratios established gender differences in demographic and pretreatment risk factors that excluded more men than women from thrombolysis therapy in a stroke population with obesity.
Conclusion
The current study reveals that more clinical risk factors excluded more obese male stroke patients than females. Increasing age, history of peripheral vascular disease, and elevated diastolic blood pressure were significantly associated with exclusion from thrombolysis in obese males, while coronary artery disease was associated with exclusion from thrombolysis in obese females. More research is necessary to develop measures for identified clinical risk factors associated with exclusion from rtPA in order to improve the use of thrombolysis therapy for obese stroke patients irrespective of gender.
References
Flegal KM, Carroll MD, Kit BK, Ogden CL (2012) Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 307:491–497
Flegal KM, Graubard BI, Williamson DF, Gail MH (2007) Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA 298:2028–2037
Dorner TE, Rieder A (2012) Obesity paradox in elderly patients with cardiovascular diseases. Int J Cardiol 155:56–65
Fredwall M, Sternberg S, Blackhurst D, Lee A, Leacock R, Nathaniel TI (2016) Gender differences in exclusion criteria for recombinant tissue-type plasminogen activator. J Stroke Cerebrovasc Dis 25:2569–2574
Gargano JW, Wehner S, Reeves M (2008) Sex differences in acute stroke care in a statewide stroke registry. Stroke 39:24–29
Li B, Wang T, Lou YZ, Guo XF, Gu HF, Zhu YX et al (2015) Sex differences in outcomes and associated risk factors after acute ischemic stroke in elderly patients: a prospective follow-up study. J Stroke Cerebrovasc Dis 24:2277–2284
Michel P, Odier C, Rutgers M, Reichhart M, Maeder P, Meuli R et al (2010) The acute stroke registry and analysis of Lausanne (ASTRAL) design and baseline analysis of an ischemic stroke registry including acute multimodal imaging. Stroke 41:2491–2498
Di Carlo A, Lamassa M, Consoli D, Valentia V, Inzitari D (2010) Sex differences in presentation, severity, and management of stroke in a population-based study. Neurology 75:670–671
Gainey J, Brechtel L, Konklin S, Madeline L, Lowther E, Blum B et al (2018) In a stroke cohort with incident hypertension; are more women than men likely to be excluded from recombinant tissue-type plasminogen activator (rtPA)? J Neurol Sci 387:139–146
Gibson CL (2013) Cerebral ischemic stroke: is gender important? J Cereb Blood Flow Metab 33:1355–1361
Rao ZZ, Gu HQ, Li ZX, Wang YL, Wang YJ (2018) Disparities in outcomes among inpatient stroke in women associated with rural-urban insurance status in China. Stroke 49
Reeves MJ, Bushnell CD, Howard G, Gargano JW, Duncan PW, Lynch G et al (2008) Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol 7:915–926
Mitchell AB, Cole JW, McArdle PF, Cheng YC, Ryan KA, Sparks MJ et al (2015) Obesity increases risk of ischemic stroke in young adults. Stroke 46:1690–1692
Wang HJ, Si QJ, Shan ZL, Guo YT, Lin K, Zhao XN et al (2015) Effects of body mass index on risks for ischemic stroke, thromboembolism, and mortality in Chinese atrial fibrillation patients: a single-center experience. PLoS One 10
Kernan (2014) Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association (vol 45, pg 2160, 2014). Stroke 45:E172-E
O'Donnell MJ, Xavier D, Liu LS, Zhang HY, Chin SL, Rao-Melacini P et al (2010) Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 376:112–123
Toss F, Wiklund P, Franks PW, Eriksson M, Gustafson Y, Hallmans G et al (2011) Abdominal and gynoid adiposity and the risk of stroke. Int J Obes 35:1427–1432
Reeves M, Bhatt A, Jajou P, Brown M, Lisabeth L (2009) Sex differences in the use of intravenous rt-PA thrombolysis treatment for acute ischemic stroke a meta-analysis. Stroke 40:1743–1749
Blum B, Wormack L, Holtel M, Penwell A, Lari S, Walker B et al (2019) Gender and thrombolysis therapy in stroke patients with incidence of dyslipidemia. BMC Womens Health 19
Meseguer E, Mazighi M, Labreuche J, Arnaiz C, Cabrejo L, Slaoui T et al (2009) Outcomes of intravenous recombinant tissue plasminogen activator therapy according to gender a clinical registry study and systematic review. Stroke 40:2104–2110
Gainey J, Blum B, Bowie B, Cooley K, Madeline L, Ervin EL et al (2018) Stroke and dyslipidemia: clinical risk factors in the telestroke versus non-telestroke. Lipids Health Dis 17
Wapshott T, Blum B, Williams K, Nathaniel TI (2017) Investigation of gender differences and exclusive criteria in a diabetic acute ischemic stroke population treated with recombinant tissue-type plasminogen activator (rtPA). J Vasc Interv Neurol 9:26–32
Nathaniel TI, Cochran T, Chaves J, Fulmer E, Sosa C, Yi S et al (2016) Co-morbid conditions in use of recombinant tissue plasminogen activator (rt-PA) for the treatment of acute ischaemic stroke. Brain Inj 30:1261–1265
Colello MJ, Ivey LE, Gainey J, Faulkner RV, Johnson A, Brechtel L et al (2018) Pharmacological thrombolysis for acute ischemic stroke treatment: gender differences in clinical risk factors. Adv Med Sci 63:100–106
Gainey J, Brecthtel J, Blum B, Keels A, Madeline L, Lowther E et al (2018) Functional outcome measures of recombinant tissue plasminogen activator–treated stroke patients in the Telestroke technology. J Exp Neurosci 12:1–11
Brecthel L, Gainey J, Penwell A, Nathaniel TI (2018) Predictors of thrombolysis in the telestroke and non telestroke settings for hypertensive acute ischemic stroke patients. BMC Neurol 18
Brian Fazzone GM, Black L-A, Williams J-A, Leacock R, Sternberg S, Blackhurst D, Nelson A, Nathaniel TI (2016) Exclusion and inclusion criteria for thrombolytic therapy in an ischemic stroke population. J Neurol Disord Stroke 4:1112
Cochran T, Chaves J, Fulmer E, Blackhurst D, Sternberg S, Leacock R et al (2014) Analysis of comorbidities in ischemic stroke patients. Neurology 82(Supplement):278
Lawson TR, Brown IE, Westerkam DL, Blackhurst DW, Sternberg S, Leacock R et al (2015) Tissue plasminogen activator (rt-PA) in acute ischemic stroke: outcomes associated with ambulation. Restor Neurol Neurosci 33:301–308
Lawson T, Brown I, Westerkam D, Blackhurst D, Sternberg S, Leacock R, et al (2015) A new diagnostic tool for measuring the effectiveness of intravenous tissue plasminogen activator (r-pa) In The Treatment Of Acute Ischemic Stroke Internnational stroke conference. 4:P346
Whisnant JP, Basford JR, Bernstein EF (1990) Special report from the National Institute of Neurological Disorders and Stroke. Classification of cerebrovascular diseases III. Stroke 4:637–676
Asdaghi N, Romano JG, Wang KF, Ciliberti-Vargas MA, Koch S, Gardener H et al (2016) Sex disparities in ischemic stroke care FL-PR CReSD study (Florida-Puerto Rico collaboration to reduce stroke disparities). Stroke 47:2618–2626
Sposato LA, Zamora R, Zurru C, Esnaola MM, Fustinoni O, Saposnik G (2008) Sex disparities in ischemic stroke care and outcome in an emerging country. The argentinian national stroke registry (ReNACer). Neurology 70:A202-A
Reed SD, Cramer SC, Blough DK, Meyer K, Jarvik JG (2001) Treatment with tissue plasminogen activator and inpatient mortality rates for patients with ischemic stroke treated in community hospitals. Stroke 32:1832–1839
Katzan IL, Hammer MD, Hixson ED, Furlan AJ, Abou-Chebl A, Nadzam DM et al (2004) Utilization of intravenous tissue plasminogen activator for acute ischemic stroke. Arch Neurol 61:346–350
Hills NK, Johnston SC (2006) Why are eligible thrombolysis candidates left untreated? Am J Prev Med 31:S210–S2S6
Gargano JW, Wehner S, Reeves MJ (2007) Sex differences in clinical presentation among confirmed acute stroke admissions from a statewide stroke registry. Stroke 38:508
Labiche LA, Chan WY, Saldin KR, Morgenstern LB (2002) Sex and acute stroke presentation. Ann Emerg Med 40:453–460
Tolibova N, Vakhabova N (2017) Gender differences in stroke subtypes, severity, risk factors, and outcomes among elderly patients with acute ischemic stroke in Uzbekistan. J Neurol Sci 381:377
Zrelak PA (2018) Gender differences in symptom perception and care-seeking behavior in acute stroke. Stroke 49
Simpson CR, Wilson C, Hannaford PC, Williams D (2005) Evidence for age and sex differences in the secondary prevention of stroke in Scottish primary care. Stroke 36:1771–1775
Syamlal G, Mazurek JM, Dube SR (2014) Gender differences in smoking among US working adults. Am J Prev Med 47:467–475
Gonzalez-Rivas JP, Nieto-Martinez R, Brajkovich I, Ugel E, Risquez A (2018) Prevalence of dyslipidemias in three regions in Venezuela: the VEMSOLS study results. Arq Bras Cardiol 110:30–35
Kapral MK, Fang JM, Hill MD, Silver F, Richards J, Jaigobin C et al (2005) Sex differences in stroke care and outcomes - results from the registry of the Canadian stroke network. Stroke 36:809–814
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Approval for this study was obtained from the ethics committee of the Greenville Health system in 2017. Since this is a retrospective data analysis, all data were de-identified, and the study did not involve patients and no consent was required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Blum, B., Penwell, A., Wormack, L. et al. Gender and thrombolysis therapy in acute ischemic stroke patients with incidence of obesity. Neurol Sci 40, 1829–1839 (2019). https://doi.org/10.1007/s10072-019-03902-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-019-03902-7