Abstract
Cluster headache (CH) has always been considered a type of primary headache affecting predominantly male subjects in early and medium adulthood. However, recent studies carried out in large case series of patients with CH show that not infrequently it may set in also after age 50; by contrast, onset before adolescence is very rare. Additionally, when onset occurs before age 14 or from the sixth decade of life onward, male predominance decreases to the point that in chronic forms CH predominantly affects the female sex. This particular pattern of the gender ratio in relation to onset in different age groups suggests that hormonal factors may actually play a role in the genesis of CH. In particular, future studies should be aimed at investigating the possible protective role of estrogen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epidemiologically, cluster headache (CH) is generally considered a disorder characterized by low prevalence in the general population, male predominance, and onset in early and medium adulthood [1,2,3].
While literature reports historically indicated a prevalence rate of 1‰ in the general population [1, 3], more recent data confirm that CH is a rather rare type of primary headache but demonstrate that it occurs more frequently, at a rate of about 3‰ [4, 5]. Chronic forms account for only slightly over 10% of all CH cases.
Male predominance, which was considered very marked in the past, with a male-to-female ratio of 5–7:1 [1, 6], is still present, but less remarkably so, the male-to-female ratio being now 2–3:1 [7,8,9]. Perhaps, this trend is the result of an actual increase in the disorder rate among women, even though we cannot exclude that it might be due to improved knowledge of CH by the medical community.
As to age at onset, the larger case series currently available for review have allowed investigators to gain further information and make interesting considerations [10, 11].
Age at onset: classical literature data
Mean age at onset of CH, as long since reported by several authors, is about 29–30 years [1,2,3, 12,13,14].
While it is believed that patients may continue to suffer from CH also in older age, possibly presenting an episodic form that has evolved into chronic or vice versa [15], there is a great lack of data on CH onset in the elderly.
Additionally, several authors generally—and far from specifically—report that CH onset is rare in childhood and adolescence [1, 3, 12]; however, such data are scarce and, above all, fail to indicate exactly below what age onset is most rare in children and adolescents. Indeed, reports span from sporadic descriptions of single cases with onset in childhood [16,17,18,19,20] to case series where the authors considered either overall cases with high rates of onset before age 20 [21] or cases distributed by decade of life with rates of onset that were very low in the first decade but were already high by the second one [3, 10]. However, owing to the highly specific peculiarities of the different stages of the second decade of life, this period should not be considered as a whole, but should be split in shorter age ranges for a more accurate assessment. Obviously, very large case series are needed to do this, but they are not easily available due to the low prevalence of CH. Therefore, in the literature, there is a lack of data on the possible onset of CH in the different stages of the first and especially of the second decade of life.
Only recently have we been able to review a large case series of CH patients consecutively referred to the University of Parma Headache Centre based on clinical records that were specially designed and filled in for such purpose. This enabled us to identify more accurately different features that characterize age at CH onset.
Age at onset: recent data
We conducted a study on 808 CH patients (585 men and 223 women) [10]. When we applied the diagnostic criteria of the latest international classifications of headache disorders [22, 23], we found that 686 (503 men and 183 women) had an episodic form of CH (ECH), 103 (66 men and 37 women) a chronic form (CCH), and 19 (16 men and three women) a form with an undefined temporal pattern, because its recent onset did not make it possible to attribute it to either form.
Mean age at onset was 30.2 years (30.1 in men and 30.4 in women). Patients with ECH had a mean age at onset of 29.7 years (29.5 in men and 29.0 in women), while those with CCH had a mean age at onset of 33.9 years (32.0 in men and 37.2 in women). Women with primary CCH, i.e., chronic ab initio, had a mean age at onset of 42.8 years, while those with secondary CCH, i.e., chronic evolved from episodic, did not differ from those with ECH.
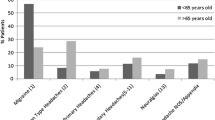
When we distributed the subjects by decade of age at onset, we found a peak in the third decade, both in men and in women with ECH (Table 1). Patients with CCH showed a bimodal pattern, which was far more marked in women (peaks in the second and the sixth decade) than in men (peaks in the third and the fifth decade) (Fig. 1).
Male predominance was clear in the CH cases with onset in the middle age ranges, while it tended to decrease in the extreme age ranges. In CCH patients, we even saw a reversal of the typical male-to-female ratio in cases with onset ≤ 15 years (M:F = 0.5:1) and ≥ 50 years (M:F = 0.6:1).
Late-onset CH
Anecdotal cases [18, 24,25,26] and small case series [2, 27, 28] indicate a possible onset of CH in older age, especially in women.
A recent study carried out at the University of Parma Headache Centre [29] showed 73 patients (43 men and 30 women) with CH onset after age 50, including 56 with an episodic form and 17 with a chronic form. Of the latter, as many as 12 were women and only five were men.
Over 20% of patients with CH onset after age 50 had a chronic form. In these patients, there was a marked female predominance, with women accounting for 40% of cases (12/30 patients).
On the other hand, the gender ratio differs widely in chronic forms. In CCH with onset after age 50, the male-to-female ratio is 0.4:1 and is therefore reversed compared with episodic and chronic forms with onset before age 50 (2.5:1), as well as episodic forms with onset after age 50 (2.1:1).
The mean duration of cluster periods in patients with ECH was statistically significantly longer in those with onset after age 50 (69 vs 40 days), especially in women (80 vs 42 days).
Our study data [29] indicate that CH onset in mature adulthood and in old age is not a rare event and, at any rate, seems more frequent than was thought in the past. In accordance with Ekbom et al. [2], we observed that late onset of CH occurs more frequently in women with chronic forms. Moreover, if we consider that our female patients suffering from episodic forms with onset after age 50 had significantly longer cluster periods than those with onset at a younger age, we can conclude that late onset of CH in women is a negative prognostic factor.
Pediatric-onset CH
Based on our data [10, 11], CH onset before age 10 is an extremely rare event (9/808 or 1.1%) (4/585 in boys or 0.7% and 5/223 in girls or 2.2%), while it occurs quite often by the second decade of life (175/808 or 21.7%) (119/585 in boys or 20.3% and 56/223 in girls or 25.1%) (Table 1). If we distribute age at onset by 5-year groups, we see that within the second decade, there are marked differences in age at onset between the 10- to14-year groups (45/808 cases or 5.6%) (28/585 in boys or 4.8% and 17/223 in girls or 7.6%) and the 15- to 19-year groups (130/808 cases or 16.1%) (91/585 in boys or 15.6% and 39/223 in girls or 17.5%) (Fig. 2).
In addition, if we choose to consider as atypical an age at onset that affects less than 10% of cases, we see that it corresponds to ≤ 15 years in all CH cases (79/808 or 9.6%) and in male CH cases (52/585 or 8.9%) and to ≤ 14 years in female CH cases (22/223 or 9.9%).
Finally, if we consider as pediatric onset (PO), an age below 14 years, we see that among all CH patients, PO occurs only in less than 5%, or 38 cases, including 20 boys and 18 girls (Table 2). Seven of the 38 patients with PO had CCH and as many as six of them were girls.
The rate of delayed diagnosis after onset was almost double in CH patients with PO (about 21 years) compared with patients with later onset (about 11 years).
Compared with cases with adult onset (AO), PO cases reported a significantly greater family history of CH in females and of non-CH headache in males.
In PO males, CH by adulthood was characterized by clinical features that were significantly different from those of AO cases: increased frequency and duration of attacks and greater presence of symptoms accompanying pain, such as conjunctival injection and forehead and facial flushing, and of migraine-like features and nausea.
In three of the seven cases in which it was easier to trace back the clinical features of CH at onset because they were first observed before age 18, the duration of attacks was at the lower limit (15–30 min) of the range set by the international classifications [22, 23], and in five of them, cluster periods consisted of mini-bouts (3–7 days). The other clinical features were typical of CH.
Conclusions
In summary, our studies indicate that onset of CH may occur also after age 50, while it is very rare before adolescence. In addition, both in early and late-onset cases, we did not observe the male predominance typically associated with this type of primary headache; by contrast, we even saw an increased frequency of CH among female patients when we considered only CCH cases.
In the past, it was believed that male predominance, together with some physical features that were distinctive of patients with CH—taller than average stature, strong build, lion’s face—might depend on a specific hormonal profile. Therefore, the investigators’ attention focused on testosterone levels. However, the few studies carried out on this line of research were not able to prove any significant alterations [1, 30].
The current findings of increased CH frequency in females with onset before age 14, its increased frequency in males with onset between age 14 and age 50, and, again, its increase frequency in females with onset after age 50, corroborate the idea that hormonal factors may be involved in this type of headache. Therefore, it would be interesting to investigate a possible protective role played by estrogen.
References
Kudrow L (1980) Cluster headache. In: Mechanisms and management. Oxford University Press, New York
Manzoni GC, Terzano MG, Bono G, Micieli G, Martucci N, Nappi G (1983) Cluster headache – clinical findings in 180 patients. Cephalalgia 3:21–30
Ekbom K, Svensson DA, Träff H, Waldenlind E (2002) Age at onset and sex ratio in cluster headache: observations over three decades. Cephalalgia 22:94–100
Sjaastad O, Bakketeig LS (2003) Cluster headache prevalence. Vågå study of headache epidemiology. Cephalalgia 23:528–533
Torelli P, Beghi E, Manzoni GC (2005) Cluster headache prevalence in the Italian general population. Neurology 64:469–474
Ekbom K (1970) A clinical comparison of cluster headache and migraine. Acta Neurol Scand 46:1–44
Manzoni GC (1998) Gender ratio of cluster headache over the years: a possible role of changes in lifestyle. Cephalalgia 18:138–142
Bahra A, May A, Goadsby PJ (2002) Cluster headache. A prospective clinical study with diagnostic implications. Neurology 58:354–361
Rozen TD, Fishman RS (2012) Cluster headache in the United States of America: demographics, clinical characteristics, triggers, suicidality, and personal burden. Headache 52:99–113
Manzoni GC, Taga A, Russo M, Torelli P (2016) Age of onset of episodic and chronic cluster headache – a review of a large case series from a single headache centre. J Headache Pain 17:44
Taga A, Manzoni GC, Russo M, Paglia MV, Torelli P (2018) Childhood-onset cluster headache: observations from a personal case-series and review of the literature. Headache 58:443–454
Sutherland JM, Eadie MJ (1972) Cluster headache. Res Clin Stud Headache 3:92–125
Manzoni GC (1999) Cluster headache and lifestyle: remarks on a population of 374 male patients. Cephalalgia 19:88–94
Manzoni GC, Stovner LJ (2010) Epidemiology of headache. In: Headache NG, Moskowitz MA (eds) Handbook of clinical neurology, vol 97. Elsevier, Amsterdam, pp 3–22
Manzoni GC, Micieli G, Granella F, Tassorelli C, Zanferrari C, Cavallini A (1991) Cluster headache – course over ten years in 189 patients. Cephalalgia 11:169–174
Terzano MG, Manzoni GC, Maione R (1981) Cluster headache in one-year old infant? Headache 21:255–256
Garrido C, Tuna A, Ramos S, Temudo T (2001) Cluster headache in a 3 year old child. Rev Neurol 33:732–735
Evers S, Frese A, Majewski A, Albrecht O, Husstedt IW (2002) Age of onset in cluster headache: the clinical spectrum (three case reports). Cephalalgia 22:160–162
Kacinski M, Nowak A, Kroczka S, Gergont A (2009) Cluster headache in 2-year-old polish girl. Cephalalgia 29:1091–1094
Mariani R, Capuano A, Torriero R, Tarantino S, Properzi E, Vigevano F, Valeriani M (2014) Cluster headache in childhood: case series from a pediatric headache center. J Child Neurol 29:62–65
Zidverc-Trajkovic J, Markovic K, Radojicic A, Podgorac A, Sternic N (2014) Cluster headache: is age of onset important for clinical presentation? Cephalalgia 34:664–670
Headache Classification Committee of the International Headache Society (HIS) (2013) The international classification of headache disorders, 3rd edition (beta version). Cephalalgia 33:629–808
Headache Classification Committee of the International Headache Society (HIS) (2018) The International Classification of Headache Disorders, 3rd edition. Cephalalgia 38:1–211
Torelli P, Cologno D, Manzoni GC (1999) Gender ratio in cluster headache. In: Olesen J, Goadsby PJ (eds) Cluster Headache and Related Conditions. Oxford University Press, Oxford, pp 49–52
Lisotto C, Mainardi F, Maggioni F, Zanchin G (2004) Headache in elderly: a clinical study. J Headache Pain 5:36–41
Fischera M, Anneken K, Evers S (2005) Old age of onset in cluster headache. Headache 45(615):616
Solomon GD, Kunkle RS, Frame J (1990) Demographics of headache in elderly patients. Headache 30:273–276
Mosek A, Hering-Hanit R, Kuritzky A (2001) New-onset cluster headache in middle-age and elderly women. Cephalalgia 21:198–200
Manzoni GC, Maffezzoni M, Lambru G, Lana S, Latte L, Torelli P (2012) Late-onset cluster headache: some considerations about 73 cases. Neurol Sci 33(Suppl 1):S157–S159
Delaruelle Z, Ivanova TA, Khan S, Negro A, Ornello R, Raffaelli B, Terrin A, Mitsikostas DD, Reuter U, on behalf of the European Headache Federation School of Advanced Studies (EHF-SAS) (2018) Male and female sex hormones in primary headaches. J Headache Pain 19:117
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
This article does not contain any study with human subjects performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Manzoni, G.C., Camarda, C., Genovese, A. et al. Cluster headache in relation to different age groups. Neurol Sci 40 (Suppl 1), 9–13 (2019). https://doi.org/10.1007/s10072-019-03767-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-019-03767-w