Abstract
Objective
To explore the clinical and imaging features of patients with hypertrophic cranial pachymeningitis (HCP).
Methods
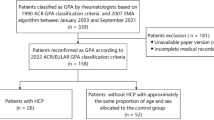
A retrospective study was performed on 22 patients with HCP diagnosed at the Affiliated Hospital of Xuzhou Medical University from February 2014 to September 2017.
Results
A headache was present as an initial symptom in 18 patients. The headache was associated with the loss of vision (2 cases), facial pain (1 case), and unsteady walking (1 case). Other symptoms included cranial nerve dysfunction (15 cases), cerebellar ataxia (4 cases), and sinus thrombosis (3 cases). In the laboratory tests, 7 patients showed an increased number of white blood cells, higher levels of C-reaction protein (CRP), and erythrocyte sedimentation rate (ESR). An elevated level of immunoglobulin G4 (IgG4) and the presence of the anti-neutrophil cytoplasmic antibody (ANCA) were found in 3 and 2 patients respectively. There were 17 patients who had abnormalities in their cerebrospinal fluid (CSF) on lumbar puncture. On magnetic resonance imaging (MRI), a local or generalized thickening was observed in the cerebral falx, the tentorium of the cerebellum, the fronto-parietal lobe, the occipito-parietal lobe, and the dura of skull base. A dural biopsy obtained in one case showed a variety of inflammatory changes. An immunohistochemical analysis revealed the positivity of CD138, IgG, and IgG4 in some cells. All 22 patients had a good response to corticosteroids.
Conclusion
HCP mainly leads to a headache and the paralysis of multiple cranial nerves. A biopsy and MRI are often required and serve as the basis for the diagnosis and effective therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hypertrophic cranial pachymeningitis (HCP) is recognized as a rare inflammatory disorder which leads to a diffuse thickening of the dura mater (Fig. 1). A headache and cranial nerve damage are the most common clinical manifestations of HCP. We retrospectively analyzed 22 cases of HCP diagnosed at the Affiliated Hospital of Xuzhou Medical University from February 2014 to September 2017. Additionally, we sought to explore the clinical and imaging features of HCP to improve the awareness of the disease among physicians.
Materials and methods
In this study, there were 11 males and 11 females, and their ages ranged from 17 to 62 years. None of them had a positive family history of the disease. There were 5 cases of acute onset while a chronic onset was reported in 17 cases. Their symptoms included the following: headache in 18 cases (needle-like pain in 1 case, rebound tenderness in 7 cases, distending pain in 3 cases, dull pain in 1 case, and dragging pain in 1 case), headache combined with loss of vision in 2 cases, facial pain in 1 case, unsteady walking in 1 case, cranial nerve dysfunctions in 15 cases (optic nerve was involved in 8 cases, abducens nerve in 7 cases, oculomotor nerve in 6 cases, trochlear nerve in 6 cases, auditory nerve in 4 cases, and glossopharyngeal nerve in 1 case), cerebellar ataxia in 4 cases, and sinus thrombosis in 3 cases. See Table 1 for details. Laboratory tests included the following: routine blood test, coagulation tests, biochemistry, erythrocyte sedimentation rate (ESR), tests for detection of C-reactive protein (CRP), autoimmune series test, CSF routine examinations, and dura mater biopsy. All 22 patients underwent magnetic resonance imaging (MRI) scans.
Results
On blood examinations, 16 cases showed abnormalities in the autoimmune series test (positive antinuclear antibodies (ANA) in 5 cases, increased levels of IgG4 in 3 cases, positive anti-neutrophilic cytoplasmic antibody (ANCA) in 2 cases, positive anti-ds-DNA in 2 cases, positive SS-A in 2 cases, elevated rheumatic factor (RF) in 2 cases, positive MPO-Ab in 1 case, elevated levels of C3 and C4 in 1 case), 7 cases showed an increased number of white blood cells (WBCs) (11.3~23.5*10^9), and 7 cases had higher levels of CRP (20.6~171 mg/L) and ESR(21~81 mm/h). There were 17 cases who showed abnormalities in cerebrospinal fluid (CSF) routine and biochemical tests (6 cases with increased CSF pressure, 7 cases with increased CSF protein levels, 5 cases with a higher level of IgG and IgM, 3 cases with increased IgA, and 3 cases with increased WBC count), 19 cases whose CSF tumor exfoliated cells were negative. The remaining 3 cases underwent complete blood tumor examination, all of which were negative (see Table 1 for details). A dural biopsy performed in one case showed scattered lymphocytes and plasma cells among the hyaline degeneration vessels (Fig. 2). An immunohistochemical analysis revealed the presence of CD138, IgG, and IgG4 in some cells. MRI results showed the local or generalized thickening with uniform linear enhancement in the cerebral falx (6 cases), the tentorium of the cerebellum (8 cases), the fronto-parietal lobe (5 cases), occipito-parietal lobe (5 cases), the temporal lobe (3 cases), the pia mater (1 case), the posterior fossa (1 case), and the skull base (1 case). The T1-weighted images (T1WIs) of the thickened dura showed hypo-intense or iso-intense signals while the T2-weighted images (T2WIs) showed significant hypo-intense signals. A significant homogeneous enhancement of the thickened dura was observed on a contrast-enhanced MRI scan. All 22 patients were treated with corticosteroids. Among them, 10 cases were treated with intravenous infusion of prednisolone (20~60 mg); 6 cases were treated with an intravenous injection of dexamethasone (5~10 mg); 5 cases were treated with intravenous drip of methylprednisolone; and 1 case was treated with 300 mg methylprednisolone intravenous drip and gamma globulin combination therapy. The symptoms of all 22 patients were improved, and they were relapse-free on the follow-up after 1 month.
Discussion
Pathogenesis
HCP is characterized by an inflamed and thickened dura mater that can be idiopathic or secondary to a wide variety of other diseases. Clinically, the pathogenesis of secondary HCP is diverse. Its infectious etiologies include tuberculosis, syphilis, mycotic infection, and Lyme disease. Systemic inflammatory diseases associated with HP include sarcoidosis and Wegener’s granulomatosis. Autoimmune diseases include IgG4-related disease, vasculitis, and rheumatoid arthritis. It may also be the result of tumors and intracranial hypotension [1]. The exact cause is, however, unknown in most cases of HCP where it is labeled as idiopathic hypertrophic cranial pachymeningitis (IHCP) [2]. In our study, IHCP accounted for the largest proportion of the cases. This result was consistent with the survey of Yanekawa in Japan, which found out that 44% of the cases of HP were idiopathic. The ANCA-related HCP, especially temporal arteritis, is the most frequently diagnosed (34%) cause in the secondary HCP, followed by IgG4-related HCP (8.8%) [2, 3]. So far, there was no report of a co-existing ANCA-related and IgG4-related HCP [4].
ANCA-associated vasculitis (AAV) is recognized as the most common underlying mechanism of HCP in which B cell activation may play a key role in the pathogenesis of the disease [5]. Myeloperoxidase (MPO)-ANCA is the most important autoantibody present in the serum of Chinese patients with HCP, and it is more common as compared to RP3-ANCA. In our study, there was one patient with a weakly positive MPO-ANCA. In recent years, IgG4-related HCP has been recognized as one of the IgG4-RD spectra which occupies a certain proportion of IHCP [6]. Although the pathogenesis of IgG4-RD remains unclear, the latest studies have reported that it is a fibrotic inflammatory disease. Elevated levels of IgG4 in the serum and the CSF have been found in many newly diagnosed patients with HCP. An infiltration of IgG4-positive plasma cells has also been observed at the site of dura mater inflammation, suggesting that this fibrotic inflammatory immune response is triggered by a specific reaction of an unknown antigen. In this paper, 3 cases of HCP showed increased IgG4. In addition, a dural biopsy undertaken by one patient showed that IgG4 was present in individual cells.
Clinical feature
HCP occurs more commonly in adult males. Its clinical manifestations vary greatly depending on the sites of occurrence and include a chronic headache, cranial nerve palsies, cerebellar ataxia, seizures, and sinus thrombosis. The incidence of a headache is about 90%. The dural chronic inflammatory stimulation is the main cause of the headache which usually manifests as a progressive pain without a specific location or characteristics. In this study, there were 18 patients who presented themselves with the headache as the initial symptom. A headache combined with a loss of vision was observed in two patients. Besides, there were 3 patients whose headaches were misdiagnosed as a tension-type headache, and HCP was later confirmed in our hospital. Cranial nerve palsies are probably caused by the dural hypertrophy which narrows the gap and compresses the cranial nerves [7]. The second, third, and sixth cranial nerves are the most commonly involved in the patients with HCP [8], however, the injuries to all 12 cranial nerves have been reported in the literature. The involvement of ninth and twelfth cranial nerves is, nevertheless, relatively rare [9]. In our study, the optic nerve was involved in 8 cases, the abducens nerve in 7 cases, the oculomotor nerve in 6 cases, the trochlear nerve in 6 cases, the auditory nerve in 4 cases, and the glossopharyngeal nerve in 1 case. These results are consistent with the previous studies reported in the literature. In addition, 4 patients in our study showed cerebellar ataxia due to the compression of the cerebellum or cerebellopontine angles caused by the hypertrophy of the cerebellum. The dural inflammation can cause sinus thickening and drainage block which lead to cerebral edema and sinus thrombosis. This is probably the reason behind sinus thrombosis in 3 patients in this study. A hypertrophic dura may induce damage to the central nervous system. The inflammatory diffusion to adjacent structures caused the mastoiditis in two patients in our study.
Characteristics of imaging and laboratory examinations
A local or generalized thickening can be observed on MRI scans. The T1WIs of the thickened dura can show hypo-intense or iso-intense signals while the T2WIs can show significantly hypo-intense signals which are related to the fibrosis of dura mater. HCP usually displays a nodular or linearized enhancement pattern on contrast-enhanced MRI scans, especially on T1WIs. That enhancement indicates the proliferation of fibrous tissues and inflammatory areas [10]. The lesions are more commonly observed in the cerebellar tentorium, the falx cerebri, the bilateral frontal lobes, and the cavernous sinuses. The thickening of skull base dura is, however, rare [11]. In our study, the lesion location was falx cerebri in 6 cases, tentorium of the cerebellum in 8 cases, the fronto-parietal lobe in 5 cases, the occipito-parietal lobe in 5 cases, the temporal lobe in 3 cases, pia mater in 1 case, posterior fossa in 1 case, and the skull base in 1 case. In addition, a silent MRI of the brain can provide more accurate imaging evidence in the diagnosis of HCP. The biopsy of the dura can confirm the diagnosis of HCP. The dural biopsy may reveal significant hyperplasia and infiltration with multiple inflammatory cells including B lymphocytes, eosinophils, and macrophagocytes in fibrous tissues [12]. Some patients may show a chronic non-specific granulomatous hyperplasia, hyaline degeneration, epithelioid histiocytes, caseous necrosis, and Langerhans giant cells. In our study, one patient underwent a dural biopsy which showed lymphocytes and plasma cells spread among the hyaline degeneration vessels.
Differential diagnosis
-
i.
Spontaneous intracranial hypotension (SIH: The differentiating clinical features include orthostatic headache and a CSF pressure of less than 60 mmH2O. MR findings in SIH are subdural effusion, cerebral ptosis, pituitary enlargement, ventricular narrowing, and diffuse dura mater. Contrast-enhanced scans may show diffuse linear enhancement of meninges in the tentorial areas of the cerebellum, dural sinuses, and choroid plexuses. MR findings of SIHI are reversible and generally disappear with the resolution of intracranial pressure.
-
ii.
Metastatic meningeal carcinoma: The metastasis is usually from lung cancers, melanomas, and breast cancers. MR findings are diffuse thickening of the pia mater. Dural biopsy can be used to confirm the diagnosis.
-
iii.
Leptomeningeal and arachnoid lesions: Contrast-enhanced scans can show the involvement of brain gyri
-
iv.
Subarachnoid hemorrhage: Head CT scans can show high-density shadows in the sulcus and cerebral cistern.
Treatment
Corticosteroids are the first-line therapy for HCP. Corticosteroids, however, usually only lead to a temporary improvement in the symptoms. A recurrence rate of about 16% has been reported. For patients who suffer a relapse, the symptoms are controlled by administering corticosteroids followed by an immunosuppressive therapy. Some studies have reported that intravenous cyclophosphamide can achieve long-term improvement in some patients which suggests a considerable promise of azathioprine, cyclophosphamide, and other immunosuppressive drugs in the treatment of HCP [11]. In addition, rituximab is another viable option for patients with long-term remission of HCP. Due to the blood-brain barrier effect, the drug concentration in the meninges is not stable. Hence, intravenous rituximab has a limited therapeutic effect. Therefore, an intrathecal injection of rituximab may present an effective and safe treatment. Surgical interventional therapy is reserved for patients who do not respond to drugs or have severe neurological deficits, followed by corticosteroids and immunosuppressive agents. In this study, all 22 patients were treated with corticosteroids (methylprednisolone, dexamethasone, and prednisolone). Their clinical states were improved, and there was no recurrence on the follow-up after 1 month.
In summary, HCP is a chronic inflammatory disease in which the lesions are located in the dura and lead to neurological dysfunction. Although the number of reported cases of HCP is increasing gradually, however, large-scale clinical trials are required to explore its etiology which is still not clear.
References
Vale TC, Duani H, Macedo DL (2013) Cranial hypertrophic pachymeningitis secondary to neurocysticercosis. Neurol Sci 34:401–403. https://doi.org/10.1007/s10072-012-1002-4
Han F, Zhong DR, Hao HL, Kong WZ, Zhu YC, Guan HZ, Cui LY (2016) Cranial and lumbosacral hypertrophic pachymeningitis associated with systemic lupus erythematosus: a case report. Medicine (Baltimore) 95(39):e4737
Kaga H, Komatsuda A, Saito M, Nara M, Omokawa A, Togashi M, Okuyama S, Wakui H, Takahashi N (2018) Anti-neutrophil cytoplasmic antibody-associated vasculitis complicated by periaortitis and cranial hypertrophic pachymeningitis: a report of an autopsy case. Intern Med 57(1):107–113
Popkirov S, Kowalski T, Schlegel U, Skodda S (2015) Immunoglobulin-G4-related hypertrophic pachymeningitis with antineutrophil cytoplasmatic antibodies effectively treated with rituximab. J Clin Neurosci 22(6):1038–1040
Shimojima Y, Kishida D, Sekijima Y (2017) Increased BAFF and APRIL levels in the cerebrospinal fluid of patients with anti-neutrophil cytoplasmic antibody-related hypertrophic pachymeningitis. Cytokine 99:305–309
Shen Y, Dai T, Wu W (2016) The clinical diagnosis and treatment of hypertrophic dural inflammation. Chin J Intern Med 55(3):234–236. https://doi.org/10.3760/cma.j.issn.0578-1426.2016.03.018.
Lin Z, Zhang H, Dai L (2013) The clinical and imaging features of hypertrophic meningitis. A report of 13 cases. J Apoplexy Neuropathy 30(9):801–803
Russo A, Silvestro M, Cirillo M, Tessitore A, Tedeschi G (2017) Idiopathic hypertrophic pachymeningitis mimicking hemicrania continua: an unusual clinical case. Cephalalgia. https://doi.org/10.1177/0333102417708773
Della-Torre E, Campochiaro C, Cassione EB, Albano L, Gerevini S, Bianchi-Marzoli S, Bozzolo E, Passerini G, Lanzillotta M (2018) Intrathecal rituximab for IgG-related hypertrophic pachymeningitis. J Neurol Neurosurg Psychiatry 89(4):441–444
Zhou J, Yang Y, Chen S (2014) The clinical and imaging features of hypertrophic meningitis. Guangdong Med 10:1547–1548,1549
Hahn LD, Fulbright R, Baehring JM (2016) Hypertrophic pachymeningitis. J Neurol Sci 367:278–283
Huang K, Xu Q, Ma Y, Zhan R, Shen J, Pan J (2017) Cerebral venous sinus thrombosis secondary to idiopathic hypertrophic cranial pachymeningitis: case report and review of literature. World Neurosurg 106:1052.e13–1052.e21
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Chen, H., Zhang, W., Jing, J. et al. The clinical and imaging features of hypertrophic pachymeningitis: a clinical analysis on 22 patients. Neurol Sci 40, 269–274 (2019). https://doi.org/10.1007/s10072-018-3619-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-018-3619-4