Abstract
The purposes of this review were to give the optimal cutoffs of the Montreal Cognitive Assessment (MoCA) by comparing sensitivity and specificity under different cutoffs and compare the MoCA with other screening tools in post-stroke cognitive impairment (PSCI) determined by a neuropsychological evaluation. Articles were derived from a systematic search in PubMed, Web of science, Embase, and CINAHL and were assessed for internal validity by the Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2). The figure of risk of bias was made by Review Manager 5.3, and data of selected studies were synthesized by MetaDisc 1.4. Twelve diagnostic studies, involving 2130 patients, were included. The area under the curve (AUC) under cutoffs of 20v19, 21v20, and 26v25 are 0.90, 0.90, and 0.95, showing high predictive validity for PSCI screening within 1 month. When the sensitivity and specificity are equal important, the optimal cutoff is 20v19 (Youden Index = 0.58). Compared to the Mini-Mental State Examination (MMSE), the MoCA has higher sensitivity but lower specificity. The optimal cutoff differs in different stages of stroke. Both the MMSE and MoCA are appropriate screening tools for PSCI, and the use of these two tools should be in accordance with the aim of screening. The Addenbrooke’s Cognitive Examination-Revised (ACE-R) can act as a supplement for the MoCA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cognitive impairment (CI) is prevalent in stroke patients. More than two thirds of stroke patients in the acute stage [1] and 57.7% patients in 3–6 months [2] have different degrees of CI. Post-stroke cognitive impairment (PSCI) destroys functional status [3]; increases disability [4], institutionalization [5, 6], and mortality [5]; and brings great distress to patients and caregivers [4]. PSCI is also associated with higher stroke recurrence [7], higher costs of care [4], and lower quality of life [8]. Furthermore, the PSCI places a significant burden on the health care system [9].
Accurate and early detection of PSCI is meaningful for the clinicians and stroke patients, because it can help inform rehabilitation and discharge planning [10] and then may increase patients’ chances for returning to work and improve their quality of life [11]. Cognitive screening in patients with stroke is endorsed by guidelines and best practice recommendations [12, 13].
The formal neuropsychological assessment is a reliable means for evaluating CI [2]. However, it is time-consuming and unpractical in clinical assessments and large-scale studies [2, 14]. Therefore, a brief and sensitive screening tool is urgently needed [15].
Various approaches have been applied to PSCI screening, but there is no consensus on the optimal assessment [16]. The Mini-Mental State Examination (MMSE) is the most widely used screening tool, but it is doubted for inaccuracy in screening PSCI [6, 16]. The Addenbrooke’s Cognitive Examination-Revised (ACE-R) has had a large dissemination in the last years [17], but it has poor specificity for the detection of PSCI [18]. The 5-min protocol of Stroke-Canadian Stroke Network (NINDS-CSN 5-min protocol) consists of only verbally conducted tests, and it may be suitable for the early identification and screening of cognitive sequela of stroke [19]. The Montreal Cognitive Assessment (MoCA) is an increasingly popular cognitive screening tool which has good sensitivity and specificity in detecting CI and includes the assessment of multiple cognitive domains [11, 14, 20,21,22,23]. Moreover, the MoCA is recommended by the National Institute of Neurological Disorders and Stroke-Canadian Stroke Network (NINDS-CSN) for use in stroke prevention clinics (SPCs) [24]. However, the thresholds of the MoCA are set to assess mild cognitive impairment (MCI) in community-dwelling older adults and should be revised in stroke settings [25]. The cutoffs of the MoCA used in PSCI are diverse, and the optimal cutoff has no consensus.
The aims of this systematic review were (1) to identify and quantify studies reporting the diagnostic accuracy of the MoCA in stroke survivors; (2) to compare the sensitivity and specificity under different cutoffs of the MoCA and give the optimal cutoff in different stroke stages; and (3) to compare the MoCA with other screening tools (especially the MMSE) in stroke patients with PSCI determined by a neuropsychological evaluation.
Methods
Search strategies
This systematic review was performed based on the Test Accuracy Working Group of the Cochrane Collaboration and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines [26, 27]. A systematic literature search of multiple electronic databases (PubMed, Web of science, Embase, CINAHL) from inception to February 26, 2017, was conducted by two trained reviewers independently. The search was restricted to English and primary studies. The search terms (“stroke” or “post-stroke dementia” or “PSD” or “post-stroke cognitive impairment” or “PSCI”) and (“Montreal Cognitive Assessment” or “MoCA”) were used in title or abstract. The references of the included studies were also searched to identify additional studies.
Study selection
Observational studies assessing PSCI by the MoCA were acceptable. Inclusion criteria included (1) studies recruiting stroke patients, (2) studies assessing PSCI by the MoCA, (3) studies setting the neuropsychological evaluation as the reference standard, and (4) papers published in English.
Exclusion criteria included (1) studies using the MoCA as the golden standard and (2) studies without a golden standard or essential data.
Two reviewers (D.S. and X.C.) independently reviewed the titles and abstracts of studies. Papers matching the predefined inclusion criteria or with no consensus between reviewers were reviewed in full text. Disagreements were resolved through discussions and consultations to the third reviewer (Z.L.).
Quality assessment and data extraction
The quality of studies was assessed by the Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) [28]. Two independent reviewers (D.S. and X.C.) used these 11 items of the QUADAS-2 to assess the methodological quality of the 12 studies, and disagreements were also resolved through discussions and consultations to the third reviewer (Z.L.). The following data were extracted by two independent reviewers (D.S. and X.C.) from the included studies: (1) descriptive aspects including the primary author, the year of publication, the reference standard, the sample, the MoCA assessment time (the stage of stroke), and the comparison type; (2) statistical aspects including the rate of PSCI assessed by reference standards, the cutoffs of the MoCA, the true positive (TP), the false negative (FN), the false positive (FP), the true negative (TN), the sensitivity, the specificity, the positive predictive value (PPV), and the negative predictive value (NPV). If any of the above data could not be found or calculated in an included study, it would be marked as “Unknown, UN.”
Statistical analysis
The figure of risk of bias was drawn by Review Manager 5.3 [29], and statistical analyses were conducted by MetaDisc 1.4 [30]. The random-effects model was recommended in pooled estimates of diagnostic meta-analyses to reflect inter-study heterogeneity [31]. Therefore, the pooled sensitivity, specificity, positive- and negative-likelihood ratios, and diagnostic odds ratios were all analyzed with a random-effects model. In the statistics of sROC curve, the area under the curve (AUC) and index Q* were used to measure test accuracy. The AUC reflected test accuracy as follows: uninformative if AUC = 0.5; low accuracy if 0.5 < AUC ≤ 0.7; moderate accuracy if 0.7 < AUC ≤ 0.9; very high accuracy if 0.9 < AUC < 1; and perfect if AUC = 1 [32]. The value of index Q*, where the sensitivity equals the specificity in a ROC curve, was defined as “1” if accuracy was 100% [33]. Heterogeneity between studies was verified with sight while having a common part in the confidence interval and estimation of efficacy through picture of a forest [34]. In addition, we investigated it by I2 test, whose significance was set at 5% and values were interpreted as follows: low heterogeneity if I2 ≤ 25%; moderate heterogeneity if 25% < I2 ≤ 75%; and high heterogeneity if I2 > 75% [35].
Results
Selection process
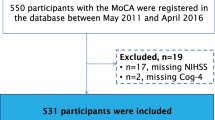
A total of 650 articles were retrieved in a systematic search, and 303 duplicates were removed. The titles and abstracts of the remaining 347 articles were examined, and 312 articles were excluded for irrelevant study contents, unsuitable study designs (including reviews, meetings, letters, and case reports), incorrect study objects, lacking a reference standard, and no use of the MoCA. Finally, 11 articles [2, 11, 14, 16, 20, 22, 36,37,38,39,40] were included after the full text review and 1 article [41] was added by reviewing references of these 11 selected articles. The process and outcome of the literature selection are presented in detail in Fig. 1.
Risk of bias in included studies
Among these 12 included articles, 7 [11, 14, 36,37,38,39,40] had a low risk of bias in all domains and items and all 12 had low applicability concerns. The risk of bias and applicability concerns in different domains are shown in Figs. 2 and 3.
Characteristics of selected studies
Twelve included studies were published from 2010 to 2017 and were all conducted in hospitals. All these studies applied the MoCA and set the formal neuropsychological assessment as the reference standard. Among these studies, seven [2, 14, 16, 20, 38, 39, 41] included patients with the stroke or transient ischemic attack (TIA) and five [11, 22, 36, 37, 40] included patients with the stroke. Seven studies [14, 22, 36,37,38, 40, 41] were from Western countries and five studies [2, 11, 16, 20, 39] were from Asian countries. The characteristics of the 12 studies are presented in Table 1.
Comparison of the MoCA and other scales
In the included studies, seven involved the comparison of the MoCA and other scales [2, 11, 14, 16, 20, 36, 41].
MoCA vs ACE-R
One study [14] compared the MoCA and the ACE-R for detecting mild cognitive impairment (MCI) at ≥ 1 year after the TIA or stroke. The optimal sensitivity and specificity for the MoCA were achieved under the cutoffs of approximately 25 to 26 (25v24, sensitivity = 0.77, specificity = 0.83; 26v25, sensitivity = 0.87, specificity = 0.63). The optimal sensitivity and specificity for the ACE-R were achieved under the cutoffs between 92 and 94 (ACE-R < 92, sensitivity = 0.72, specificity = 0.79; ACE-R < 94, sensitivity = 0.83, specificity = 0.73). Both the MoCA and the ACE-R have good sensitivity and specificity for MCI.
MoCA vs NINDS-CSN 5-min protocol
One study [20] compared the MoCA with the NINDS-CSN 5-min protocol and found that the MoCA had statistically larger AUCs in subacute stage [AUC (95% CI) 0.89 (0.85–0.93) vs 0.80 (0.74–0.87), P < 0.01] and 3–6 months after the stroke [AUC (95% CI) 0.90 (0.86–0.94) vs 0.83 (0.77–0.89), P < 0.01] for predicting patients with moderate-severe CI at 1 year.
MoCA vs MMSE
Six studies [2, 11, 14, 16, 36, 41] demonstrated the comparison of the MoCA and MMSE. Three [11, 14, 41] detected the CI and three [2, 16, 36] detected moderate-severe CI.
Both the MoCA and MMSE were of equivalent discriminatory abilities in detecting MCI within 2 or 3 weeks after stroke event [11, 41]. But compared to the MoCA, the MMSE was lacking in sensitivity for detecting MCI at ≥ 1 year after TIA or stroke [14] (only cutoffs of 29v28 or greater had sensitivities > 0.70).
Three studies [2, 16, 36] showed the comparison of the MoCA and MMSE for detecting moderate-severe CI under different cutoffs. One study [16] showed that the MMSE was lacking in sensitivity after acute stroke. Two studies [2, 36] found that both the MMSE and MoCA were of equivalent discriminatory abilities at 3–6 months after the stroke. The synthesis of these studies showed that the MMSE had higher specificity while the MoCA had higher sensitivity (details can be seen in Table 2).
Diagnostic test accuracy of the MoCA in stroke patients under different cutoffs
The 12 studies involved 2130 stroke or TIA patients in total. The cutoff points were various. Among the included articles, four studies [2, 37, 39, 40] set the optimal cutoff and the other eight studies [11, 14, 16, 20, 22, 36, 38, 41] analyzed the diagnostic test accuracy of the MoCA under different cutoffs. The range of the cutoff points was from 16v15 to 28v27. Studies with data under the same cutoff and stroke stage were synthesized. One study [20] had two groups of data in 2 weeks and 3–6 months after the stroke. One study [38] did not illustrate the stroke stage and could not be synthesized with other studies.
Distinguish CI from no cognitive impairment in stroke patients within 1 month after stroke
There were only two studies [22, 41] reporting diagnostic test accuracy of the MoCA under the cutoffs of 16v15, 17v16, 27v26, and 28v27. The pooled sensitivity and specificity were [0.54 (95% CI 0.34–0.64), 0.94 (95% CI 0.89–1.00)], [0.61 (95% CI 0.50–0.70), 0.95 (95% CI 0.87–0.99)], [0.99 (95% CI 0.95–1.00), 0.16 (95% CI 0.15–0.37)], [1.00 (95% CI 0.96–1.00), 0.19 (95% CI 0.10–0.30)] respectively.
The cutoff of 18v17 was used in three studies [20, 22, 41], and a total of 364 stroke patients were involved. The pooled sensitivity was 0.68 (95% CI 0.60–0.76) and heterogeneity between the articles was low, 15.0% (χ2 = 2.35, P > 0.05). The pooled specificity was 0.86 (95% CI 0.81–0.90), and heterogeneity between the articles was moderate, 65.3% (χ2 = 5.77, P > 0.05). The sROC AUC was 0.80 (SE = 0.07) while Q* value was 0.73 (SE = 0.06) (Fig. 4a).
The cutoff of 19v18 was used in three studies [20, 22, 41], and a total of 364 stroke patients were involved. The pooled sensitivity was 0.75 (95% CI 0.67–0.81), and heterogeneity between the articles was low,11.4% (χ2 = 2.17, P > 0.05). The pooled specificity was 0.83 (95% CI 0.78–0.87), and heterogeneity between the articles was moderate, 54.7% (χ2 = 4.41, P > 0.05). The sROC AUC was 0.88 (SE = 0.03) while Q* value was 0.81 (SE = 0.03) (Fig. 4b).
The cutoff of 20v19 was used in three studies [20, 22, 41], and a total of 364 stroke patients were involved. The pooled sensitivity was 0.80 (95% CI 0.73–0.86), and the pooled specificity was 0.78 (95% CI 0.72–0.82). The heterogeneity between the articles was moderate, 58.4% (χ2 = 4.81, P > 0.05) and 63.8% (χ2 = 5.52, P > 0.05). The sROC AUC was 0.90 (SE = 0.02) while Q* value was 0.83 (SE = 0.02) (Fig. 4c).
The cutoff of 21v20 was used in three studies [20, 22, 41], and a total of 364 stroke patients were involved. The pooled sensitivity was 0.85 (95% CI 0.78–0.90), and the pooled specificity was 0.72 (95% CI 0.66–0.77). Heterogeneity between the articles was moderate, 74.8% (χ2 = 7.94, P < 0.05) and 66.4% (χ2 = 5.95, P > 0.05), for the sensitivity and specificity, respectively. The sROC AUC was 0.90 (SE = 0.03) while Q* value was 0.83 (SE = 0.03) (Fig. 4d).
The cutoff of 22v21 was used in three studies [20, 22, 41], and a total of 364 stroke patients were involved. The pooled sensitivity was 0.87 (95% CI 0.81–0.92), and heterogeneity between the articles was high, 75.3% (χ2 = 8.09, P < 0.05). The pooled specificity was 0.65 (95% CI 0.60–0.71), and heterogeneity between the articles was moderate, 59.0% (χ2 = 4.87, P > 0.05). The sROC AUC was 0.85 (SE = 0.04) while Q* value was 0.79 (SE = 0.04) (Fig. 4e).
The cutoff of 23v22 was used in four studies [11, 20, 22, 41], and a total of 559 stroke patients were involved. The pooled sensitivity was 0.87 (95% CI 0.82–0.91), and the pooled specificity was 0.69 (95% CI 0.64–0.74). Heterogeneity between the articles was low, 17.3% (χ2 = 4.07, P > 0.05) and 0.0% (χ2 = 1.65, P > 0.05), for the sensitivity and specificity, respectively. The sROC AUC was 0.85 (SE = 0.05) while Q* value was 0.78 (SE = 0.04) (Fig. 4f).
The cutoff of 24v23 was used in three studies [11, 22, 41], and a total of 268 stroke patients were involved. The pooled sensitivity was 0.90 (95% CI 0.84–0.94), and the pooled specificity was 0.66 (95% CI 0.56–0.75). The heterogeneity between the articles was low, 0.0% (χ2 = 1.39, P > 0.05) and 18.0% (χ2 = 2.35, P > 0.05), for the sensitivity and specificity, respectively. The sROC AUC was 0.89 (SE = 0.06) while Q* value was 0.82 (SE = 0.06) (Fig. 4g).
The cutoff of 25v24 was used in three studies [22, 37, 41], and a total of 391 stroke patients were involved. The pooled sensitivity was 0.84 (95% CI 0.80–0.88), and the pooled specificity was 0.37 (95% CI 0.27–0.48). The heterogeneity between the articles was high, 79.5% (χ2 = 9.77, P < 0.05) and 75.9% (χ2 = 8.29, P < 0.05), for the sensitivity and specificity, respectively. The sROC AUC was 0.86 (SE = 0.59) while Q* value was 0.79 (SE = 0.57) (Fig. 4h).
The cutoff of 26v25 was used in three studies [11, 22, 41], and a total of 268 stroke patients were involved. The pooled sensitivity was 0.96 (95% CI 0.92–0.99), and heterogeneity between the articles was 0.0% (χ2 = 0.19, P > 0.05). The pooled specificity was 0.34 (95% CI 0.16–0.35), and heterogeneity between the articles was moderate, 53.5% (χ2 = 4.30, P > 0.05). The sROC AUC was 0.95 (SE = 0.11) while Q* value was 0.89 (SE = 0.14) (Fig. 4i).
The diagnostic test accuracy of the MoCA under different cutoffs in 1 month after the stroke is summarized in Table 3. The sROC AUC of 26v25 was the highest, and the diagnostic test accuracy of MoCA under the cutoff 26v25 was the highest. But, when the sensitivity and specificity are both important, 20v19 is the optimal cutoff.
Distinguish CI from NCI in stroke patients within 3–6 months after stroke or TIA
There were two studies [20, 39] reporting diagnostic test accuracy of the MoCA under this situation. The sensitivity and specificity under different cutoffs could be seen in Table 1. The optimal cutoff in study [20] (21v20: sensitivity 0.83, specificity 0.80) was superior to the cutoff in study [39] (24v23: sensitivity 0.78, specificity 0.80). From current studies, the optimal cutoff for distinguishing CI from NCI in stroke patients within 3–6 months after the stroke of TIA is 21v20.
Distinguish CI from NCI in stroke patients at ≥ 1 year after stroke or TIA
There was one study [14] reporting diagnostic test accuracy under this situation. The sensitivity and specificity under different cutoffs can been seen in Table 1. In this study, the optimal cutoff for distinguishing CI from NCI at ≥ 1 year after the stroke or TIA was 24v23 and 26v25.
Distinguish moderate-severe CI from MCI and NCI in stroke patients within 1 month after stroke or TIA
Only one study [16] reported diagnostic test accuracy under this situation. The sensitivity and specificity under different cutoffs can been seen in Table 1. The optimal cutoff was 22v21.
Distinguish moderate-severe CI from MCI and NCI in stroke patients within 3–6 months after stroke or TIA
There were two studies [2, 36] reporting diagnostic test accuracy under this situation. The sensitivity and specificity under different cutoffs can been seen in Table 1. Two studies [2, 36] all reported the test accuracy under the cutoff 22v21, and the pooled sensitivity and specificity were 0.84 and 0.65. The pooled sensitivity and specificity were all lower than the optimal cutoff in study [36] (24v23: sensitivity 0.92, specificity 0.67). From current studies, the optimal cutoff for distinguishing moderate-severe CI from MCI and NCI in stroke patients within 3–6 months after the stroke or TIA is 24v23.
Discussion
Early detection of the PSCI is important, and a brief and accurate screening tool is urgently needed. The MMSE, the ACE-R, the NINDS-CSN 5-min protocol, and the MoCA are the most widely used tools for PSCI screening. We conducted this study to assess the discriminant validity of the MoCA and the other tools for detecting the PSCI determined by a neuropsychological battery and to find the optimal cutoff by performing a systematic review and meta-analysis of 12 studies.
Only one study [14] compared the MoCA and the ACE-R for detecting MCI at ≥ 1 year after the TIA or stroke and indicated that both these two tools have good sensitivity and specificity. Contrasting to this result, a former study [18] underlined that the ACE-R has poor specificity for the detection of cognitive impairment after stroke [18]. Different types and stages of disease may account for the difference. More studies are needed to verify the test accuracy of the ACE-R for detecting PSCI.
Compared to the NINDS-CSN 5-min protocol, the MoCA administered in subacute stage and 3–6 months after the stroke is superior in predicting moderate-severe CI at 1 year [20]. But, the NINDS-CSN 5-min protocol consists of only verbally conducted tests and can be used in patients with weakness of the dominant hand or visual field defect [19]. Therefore, it could act as a supplement for the MoCA.
Both the MoCA and MMSE have a similar ability to detect PSCI. Previous studies found that the MMSE had a ceiling effect and low sensitivity [6, 23, 42, 43]. The MoCA may be more suitable than the MMSE for assessing the CI in TBI and stroke patients after a long-term period since the onset [21, 42]. Compared to the MMSE, the MoCA has higher sensitivity but lower specificity. And, if the aim of screening is detecting only more severely cognitive-impaired patients, the MoCA’s superiority in sensitivity would be lost [36]. So, albeit the sensitivity is the most important quality in a screening tool [36], the uses of the MoCA and MMSE should be combined to optimize the PSCI screening.
The results of the systematic review can provide scientific evidence for choosing the optimal cutoffs of the MoCA in PSCI screening. As screening aims and stroke stages change, the optimal cutoff changes. While distinguishing the CI from the NCI, the optimal cutoffs are 26v25 within 1 month, 21v20 after 3–6 months, and 24v23 and 26v25 after 1 year since the stroke or TIA onset. While the sensitivity and specificity are both important, the optimal cutoff for distinguishing CI from NCI within 1 month is 20v19. While distinguishing moderate-severe CI from MCI and NCI, the optimal cutoffs are 22v21 within 1 month and 24v23 between 3 and 6 months since the stroke or TIA onset. The optimal cutoffs of the MoCA were diverse in previous studies and did not come to an agreement. The results of this study can provide reference for subsequent researches and clinical applications.
There were several limitations of the present study. Firstly, considerable amount of related conference papers were deleted and it may be a loss of information. But, conference papers were lacking in necessary data and full texts, and the removal seemed to be reasonable. Secondly, due to a lack of researches, this study did not give the optimal cutoffs of the MoCA in all stroke stages.
Conclusion
Compared to the MMSE, the MoCA has higher sensitivity but lower specificity. Both the MMSE and MoCA are screening tools for the PSCI, and the use of these two tools should be in line with the aim of screening. The optimal cutoff differs in different stroke stages and screening aims. There is a lack of researches in diagnostic test accuracy of the MoCA in the detection of the PSCI under different stages, especially in 3 and 6–12 months.
References
Nys GM, van Zandvoort MJ, de Kort PL, Jansen BP, Kappelle LJ, de Haan EH (2005) Restrictions of the Mini-Mental State Examination in acute stroke. Arch Clin Neuropsychol 20(5):623–629. https://doi.org/10.1016/j.acn.2005.04.001
Dong Y, Venketasubramanian N, Chan BP, Sharma VK, Slavin MJ, Collinson SL et al (2012) Brief screening tests during acute admission in patients with mild stroke are predictive of vascular cognitive impairment 3-6 months after stroke. J Neurol Neurosurg Psychiatry 83(6):580–585. https://doi.org/10.1136/jnnp-2011-302070
Barker-Collo S, Feigin V (2006) The impact of neuropsychological deficits on functional stroke outcomes. Neuropsychol Rev 16(2):53–64. https://doi.org/10.1007/S11065-006-9007-5
Claesson L, Lindén T, Skoog I, Blomstrand C (2005) Cognitive impairment after stroke—impact on activities of daily living and costs of care for elderly people. Cerebrovasc Dis 19(2):102–109. https://doi.org/10.1159/000082787
Pasquini M, Leys D, Rousseaux M, Pasquier F, Hénon H (2007) Influence of cognitive impairment on the institutionalisation rate 3 years after a stroke. J Neurol Neurosurg Psychiatry 78(1):56–59. https://doi.org/10.1136/jnnp.2006.102533
Pendlebury ST, Cuthbertson FC, Welch SJ, Mehta Z, Rothwell PM (2010) Underestimation of cognitive impairment by Mini-Mental State Examination versus the Montreal Cognitive Assessment in patients with transient ischemic attack and stroke: a population-based study. Stroke 41(6):1290–1293. https://doi.org/10.1161/STROKEAHA.110.579888
Moroney JT, Bagiella E, Tatemichi TK, Paik MC, Stern Y, Desmond DW (1997) Dementia after stroke increases the risk of long-term stroke recurrence. Neurology 48(5):1317–1325. https://doi.org/10.1212/WNL.48.5.1317
Nys GM, van Zandvoort MJ, van der Worp HB, de Haan EH, de Kort PL, Kappelle LJ (2005) Early depressive symptoms after stroke: neuropsychological correlates and lesion characteristics. J Neurol Sci 228(1):27–33. https://doi.org/10.1016/j.jns.2004.09.031
Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, Moran AE, Sacco RL, Anderson L, Truelsen T, O'Donnell M, Venketasubramanian N, Barker-Collo S, Lawes CMM, Wang W, Shinohara Y, Witt E, Ezzati M, Naghavi M, Murray C (2014) Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 383(9913):245–254. https://doi.org/10.1016/S0140-6736(13)61953-4
van Heugten CM, Walton L, Hentschel U (2015) Can we forget the Mini-Mental State Examination? A systematic review of the validity of cognitive screening instruments within one month after stroke. Clin Rehabil 29(7):694–704. https://doi.org/10.1177/0269215514553012
Shen YJ, Wang WA, Huang FD, Chen J, Liu HY, Xia YL, Han M, Zhang L (2016) The use of MMSE and MoCA in patients with acute ischemic stroke in clinical. Int J Neurosci 126(5):442–447. https://doi.org/10.3109/00207454.2015.1031749
Eskes GA, Lanctôt KL, Herrmann N, Lindsay P, Bayley M, Bouvier L, Dawson D, Egi S, Gilchrist E, Green T, Gubitz G, Hill MD, Hopper T, Khan A, King A, Kirton A, Moorhouse P, Smith EE, Green J, Foley N, Salter K, Swartz RH, Heart Stroke Foundation Canada Canadian Stroke Best Practices Committees (2015) Canadian stroke best practice recommendations: mood, cognition and fatigue following stroke practice guidelines, update 2015. Int J Stroke 10(7):1130–1140. https://doi.org/10.1111/ijs.12557
National Institute for Health and Clinical Excellence (2013) Stroke rehabilitation: long term rehabilitation after stroke. www.guidance.nice.org.uk/CG162. Accessed 26 February 2017
Pendlebury ST, Mariz J, Bull L, Mehta Z, Rothwell PM (2012) MoCA, ACE-R, and MMSE versus the National Institute of Neurological Disorders and Stroke-Canadian Stroke Network vascular cognitive impairment harmonization standards neuropsychological battery after TIA and stroke. Stroke 43(2):464–469. https://doi.org/10.1161/STROKEAHA.111.633586
Mancuso M, Varalta V, Sardella L, Capitani D, Zoccolotti P, Antonucci G et al (2016) Italian normative data for a stroke specific cognitive screening tool: the Oxford Cognitive Screen (OCS). Neurol Sci 37(10):1713–1721. https://doi.org/10.1007/s10072-016-2650-6
Dong Y, Sharma VK, Chan BP, Venketasubramanian N, Teoh HL, Seet RC et al (2010) The Montreal Cognitive Assessment (MoCA) is superior to the Mini-Mental State Examination (MMSE) for the detection of vascular cognitive impairment after acute stroke. J Neurol Sci 299(1–2):15–18. https://doi.org/10.1016/j.jns.2010.08.051
Pigliautile M, Chiesi F, Rossetti S, Conestabile Della Staffa M, Ricci M, Federici S et al (2015) Normative data for the ACE-R in an Italian population sample. Neurol Sci 36(12):2185–2190. https://doi.org/10.1007/s10072-015-2330-y
Morris K, Hacker V, Lincoln NB (2012) The validity of the Addenbrooke’s Cognitive Examination-Revised (ACE-R) in acute stroke. Disabil Rehabil 34(3):189–195. https://doi.org/10.3109/09638288.2011.591884
Lim JS, Oh MS, Lee JH, Jung S, Kim C, Jang MU, Lee SH, Kim YJ, Kim Y, Park J, Kang Y, Yu KH, Lee BC (2017) Prediction of post-stroke dementia using NINDS-CSN 5-minute neuropsychology protocol in acute stroke. Int Psychogeriatr 29(5):777–784. https://doi.org/10.1017/S1041610216002520
Dong YH, Xu J, Chan BPL, Seet RCS, Venketasubramanian N, Teoh HL et al (2016) The Montreal cognitive assessment is superior to national institute of neurological disease and stroke-Canadian stroke network 5-minute protocol in predicting vascular cognitive impairment at 1 year. BMC Neurol 16(1):no pagination. https://doi.org/10.1186/s12883-016-0570-y
Zhang H, Zhang XN, Zhang HL, Huang L, Chi QQ, Zhang X, Yun XP (2016) Differences in cognitive profiles between traumatic brain injury and stroke: a comparison of the Montreal Cognitive Assessment and Mini-Mental State Examination. Chin J Traumatol 19(5):271–274. https://doi.org/10.1016/j.cjtee.2015.03.007
Salvadori E, Pasi M, Poggesi A, Chiti G, Inzitari D, Pantoni L (2013) Predictive value of MoCA in the acute phase of stroke on the diagnosis of mid-term cognitive impairment. J Neurol 260(9):2220–2227. https://doi.org/10.1007/s00415-013-6962-7
Pendlebury ST, Markwick A, de Jager CA, Zamboni G, Wilcock GK, Rothwell PM (2012) Differences in cognitive profile between TIA, stroke and elderly memory research subjects: a comparison of the MMSE and MoCA. Cerebrovasc Dis 34(1):48–54. https://doi.org/10.1159/000338905
Hachinski V, Iadecola C, Petersen RC, Breteler MM, Nyenhuis DL, Black SE, Powers WJ, DeCarli C, Merino JG, Kalaria RN, Vinters HV, Holtzman DM, Rosenberg GA, Wallin A, Dichgans M, Marler JR, Leblanc GG (2006) National Institute of Neurological Disorders and Stroke-Canadian Stroke Network vascular cognitive impairment harmonization standards. Stroke 37(9):2220–2241. https://doi.org/10.1161/01.STR.0000237236.88823.47
Davis DH, Creavin ST, Yip JL, Noel-Storr AH, Brayne C, Cullum S (2015) Montreal cognitive assessment for the diagnosis of Alzheimer’s disease and other dementias. Cochrane Database Syst Rev (10):CD010775. https://doi.org/10.1002/14651858.CD010775.pub2
Leeflang MM, Deeks JJ, Gatsonis C, Bossuyt PM (2008) Systematic reviews of diagnostic test accuracy. Ann Intern Med 149(12):889–897. https://doi.org/10.7326/0003-4819-149-12-200812160-00008
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, QUADAS-2 Group et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155(8):529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
Review Manager (RevMan) [Computer Program] (2014) Version 5.3. Copenhagen, Denmark: The Nordic Cochrane Centre, The Cochrane Collaboration
Zamora J, Abraira V, Muriel A, Khan K, Coomarasamy A (2006) Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol 6(1):31. https://doi.org/10.1186/1471-2288-6-31
The Cochrane Collaboration (2013) Cochrane handbook for systematic reviews of diagnostic test accuracy. http://srdta.cochrane.org/. Accessed 26 Feb 2017
Greiner M, Pfeiffer D, Smith RD (2000) Principles and practical application of the receiver-operating characteristic analysis for diagnostic tests. Prev Vet Med 45(1–2):23–41
Walter SD (2002) Properties of the summary receiver operating characteristic (SROC) curve for diagnostic test data. Stat Med 21(9):1237–1256. https://doi.org/10.1002/sim.1099
Park SH, Lee HS (2016) Assessing predictive validity of pressure ulcer risk scales—a systematic review and meta-analysis. Iran J Public Health 45(2):122–133
Higgins JPT, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558. https://doi.org/10.1002/sim.1186
Cumming TB, Churilov L, Linden T, Bernhardt J (2013) Montreal Cognitive Assessment and Mini-Mental State Examination are both valid cognitive tools in stroke. Acta Neurol Scand 128(2):122–129. https://doi.org/10.1111/ane.12084
Chan E, Altendorff S, Healy C, Werring DJ, Cipolotti L (2017) The test accuracy of the Montreal Cognitive Assessment (MoCA) by stroke lateralisation. J Neurol Sci 373:100–104. https://doi.org/10.1016/j.jns.2016.12.028
Swartz RH, Cayley ML, Lanctôt KL, Murray BJ, Smith EE, Sahlas DJ, Herrmann N, Cohen A, Thorpe KE (2016) Validating a pragmatic approach to cognitive screening in stroke prevention clinics using the Montreal Cognitive Assessment. Stroke 47(3):807–813. https://doi.org/10.1161/STROKEAHA.115.011036
Dong Y, Slavin MJ, Chan BP, Venketasubramanian N, Sharma VK, Collinson SL et al (2014) Improving screening for vascular cognitive impairment at three to six months after mild ischemic stroke and transient ischemic attack. Int Psychogeriatr 26(05):787–793. https://doi.org/10.1017/S1041610213002457
Chan E, Khan S, Oliver R, Gill SK, Werring DJ, Cipolotti L (2014) Underestimation of cognitive impairments by the Montreal Cognitive Assessment (MoCA) in an acute stroke unit population. J Neurol Sci 343(1–2):176–179. https://doi.org/10.1016/j.jns.2014.05.005
Godefroy O, Fickl A, Roussel M, Auribault C, Bugnicourt JM, Lamy C, Canaple S, Petitnicolas G (2011) Is the Montreal cognitive assessment superior to the mini-mental state examination to detect poststroke cognitive impairment? A study with neuropsychological evaluation. Stroke 42(6):1712–1716. https://doi.org/10.1161/STROKEAHA.110
Delavaran H, Jönsson AC, Lövkvist H, Iwarsson S, Elmståhl S, Norrving B, Lindgren A (2017) Cognitive function in stroke survivors: a 10-year follow-up study. Acta Neurol Scand 136(3):187–194. https://doi.org/10.1111/ane.12709
Jacquin A, Binquet C, Rouaud O, Graule-Petot A, Daubail B, Osseby GV, Bonithon-Kopp C, Giroud M, Béjot Y (2014) Post-stroke cognitive impairment: high prevalence and determining factors in a cohort of mild stroke. J Alzheimers Dis 40(4):1029–1038. https://doi.org/10.3233/JAD-131580
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
All analyses were based on previous published studies, thus no ethical approval and patient consent are required.
Rights and permissions
About this article
Cite this article
Shi, D., Chen, X. & Li, Z. Diagnostic test accuracy of the Montreal Cognitive Assessment in the detection of post-stroke cognitive impairment under different stages and cutoffs: a systematic review and meta-analysis. Neurol Sci 39, 705–716 (2018). https://doi.org/10.1007/s10072-018-3254-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-018-3254-0