Abstract
The comorbidity of headache and epilepsy is often seen in neurological practice. The objective of this study was to assess the prevalence, types of, and risk factors for headache in juvenile myoclonic epilepsy (JME). We assessed a total of 200 patients and 100 healthy controls in our study. Headache was classified in participants using a self-administered questionnaire. Demographical, clinical features and headache characteristics were recorded. Seizure and headache temporal profiles were noted. Headache was present in 111 (56%) patients and 50 (50%) healthy participants. From these patients, 47 (42.3%) JME patients had migraine [30 (27%) migraine without aura (MO), 17 (15.3%) migraine with aura (MA)], 52 (46.8%) had tension type headache (TTH), 4 (3.6%) had both migraine and TTH, and 8 (7.2%) had other non-primary headaches. In the healthy control group, migraine was detected in 16 (32%) subjects, TTH in 33 (66%), both migraine and TTH in 1 (2%) subject. A positive migraine family history and symptom relief with sleep were more frequent in JME patients (p = 0.01). Headache was classified as inter-ictal in 82 (79.6%) patients and peri-ictal in 21 (20.4%) patients. In conclusion, the present study revealed that headache frequency was not significantly different between JME patients and healthy controls (p > 0.05). However, migraine frequency was higher in JME patients than healthy controls. Some migraine and TTH characteristics were different in between groups. We suggest that our results support both genetic relationship and shared underlying hypothetical pathopysiological mechanisms between JME and headache, especially migraine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Headache disorders and epilepsies are frequently seen neurological disorders with paroxysmal clinical manifestations [1]. From a very early era, people have been aware of a link between headache and epilepsy, but the relationship between the two is still not fully understood. In 1888, John Hughlings Jackson mentioned a level of comorbidity between headache and seizure and in 1994, Ottman and Lipton demonstrated that migraine and epilepsy were often comorbid [2, 3].
In different studies, migraine frequency was reported as 5–18% in healthy population and 8–24% in epilepsy patients [2, 4, 5]. In parallel, epilepsy frequency was reported as 0.5–1.5% in healthy population and 1–17% in migraine patients [6,7,8]. Risk factors (positive family history, comorbid affective disorders), triggering factors (alcohol consumption, menstruation, and irregularity of sleep), and prophylactic medical agents (valproic acid and topiramate) are also similar. All suggests common pathophysiological mechanisms between migraine and epilepsy [3].
Juvenile myoclonic epilepsy (JME) is one of the most common idiopathic generalized epilepsies characterized by myoclonic jerks, generalized tonic-clonic seizures (GTCS), and absence seizures [9]. The syndrome was first described by Janz in 1985 [10]. Photosensitivity is reported in 30–90% of JME patients [11]. Myoclonic seizures and GTCS can be triggered by irregularity of sleep, being woken up, alcohol consumption, stress, menstruation, and deep mental activity [10].
According to the temporal profile, headache in epilepsy can be either inter-ictal or peri-ictal. Headaches in between seizures are known as inter-ictal headache (IIHA). On the other hand, peri-ictal headache (PIHA), known as seizure-related headache, has been classified in 3: as ictal headache (IHA—headache simultaneously or very close in time with seizure), pre-ictal headache (preIHA—headache preceding a seizure), and post-ictal headache (postIHA—headache following a seizure). Forty to sixty percent of all patients with epilepsy present PIHA at some time during their disease course [12]. In this study, we aimed to assess the prevalence, types, and risk factors of headache in JME patients in our epilepsy center and to compare the results with healthy subjects. Seizure and headache temporal profiles were evaluated.
Patients and methods
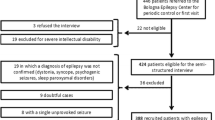
Two hundred patients between the ages of 12–55 and under the medical follow-up of epilepsy outpatient clinics in Bakirkoy Prof. Dr. Mazhar Osman Training and Research Hospital for Psychiatric, Neurologic and Neurosurgical Diseases in Istanbul, Turkey, with a diagnosis of JME due to ILAE (International League Against Epilepsy) 2010 criteria [13]. One hundred age- and sex-matched healthy volunteers were enrolled who were at least literate and without any disease. The ones who were illiterate were excluded. Two questionnaire forms were newly designed by the investigators: one involving questions about demographical, social, and clinical properties of JME patients and the other one involving questions about headache. Demographical and social properties of healthy volunteers were also noted. Data were collected from chart reviews and medical records retrospectively and from face-to-face interviews. Age, sex, educational level, family history of epilepsy, age of seizure onset, duration of disease, and antiepileptic drug (AED) treatments were recorded. A resistant epilepsy was defined as suffering from more than two myoclonic seizures a month or more than one GTCS a year.
Headache was classified according to International Classification of Headache Disorders criteria, III-beta [14]. For each headache type, questions inquired about lateralization, localization, quality, and treatment response. Headache in JME patients was also categorized as IIHA or PIHA (preIHA, IHA, and postIHA). PreIHA was defined as a headache starting at most 24 h before seizure onset and postIHA as headaches starting 3 hours after seizure and ending in 72 h.
Correlations were searched between headache characteristics and JME clinical manifestations.
The study was approved by the Local Ethic Committee of Bakirkoy Prof. Dr. Mazhar Osman Training and Research Hospital for Psychiatric, Neurologic and Neurosurgical Diseases. (The register number of the ethics committee: 30.12.2014/70787)
Statistical analysis
SPSS 21.0 statistical software was used for statistical analysis. Continuous variables are expressed as the mean ± SD; categorical variables are presented as frequencies and percentages. The chi-square test was used to compare the differences in categorical variables, and the T test was used to compare the quantitative variables between groups. A value of p < 0.05 was considered statistically significant.
Results
Two hundred JME patients and 100 healthy participants were enrolled. The mean age was 26.74 ± 8.46 (12–55) years and 28.3 ± 8.85 (12–55) years, respectively. One hundred fifteen (57.5%) patients and 56 (56%) healthy subjects were female. The mean age of seizure onset was 15.26 ± 4.1 (9–35) years and the mean time of disease duration was 10.70 ± 7.28 (1–35) years. Five patients were drug resistant. One hundred seventy-six (88%) patients were under monotherapy. The most frequently used AED were valproic acid (72%) and lamotrigine (23%).
In a group of 200 JME patients, 111 (56%) indicated headache. Out of 100 healthy controls, 50 (50%) indicated headache. Of 111 JME patients with headache, 70 (63.1%) were female; of 50 healthy subjects with headache, 30 (60%) were female. Forty-seven JME patients (23.5%) and 16 controls (16%) were identified as having migraine. The difference between the type and frequency of headache in JME patients and healthy subjects was not significant. Although an increase in migraine frequency is observed in patients, there are no significant differences between the patient and control groups who have migraine (p > 0.05) (Table 1).
Thirty-three (70.2%) JME patients with migraine had positive family history of migraine or epilepsy. On the other hand, only 6 (37.5%) control subjects with positive migraine family history were migraine sufferers. Family history of migraine or epilepsy was significantly more frequent in JME patients with migraine than controls (p = 0.01).
Headache was described as initiated from temple area by all otherwise healthy controls suffering from migraine. In JME group, temple area is also the most frequently noted headache initiation point (25p/53.2%), followed by vertex (12p/25.5%), forehead (7p/14.9%), and nucha (3p/6.4%). On the other hand, temple area was only one initiation point in all the control group and this difference is significant (p = 0.009). Headache lateralization, quality, initiation, and progression characteristics, frequency, and disturbance of sleep were similar between groups (p > 0.05) (Table 2).
Twenty-six out of 52 JME patients with TTH (50%) described their pain as throbbing, whereas 28 out of 33 control subjects with TTH (84.8%) described their pain as oppressive or constrictive. This difference was statistically significant (p < 0.001). Most of the JME patients with TTH (35p/67.3%) described their headache as having a slow initiation and acceleration. On the other hand, the vast majority of otherwise healthy subjects with TTH (25p/75.8%) noted their headache as starting slowly with a subsequent rapid acceleration. This difference was statistically significant (p < 0.001). TTH frequency was less than once a month in 15.4% of JME patients. On the other hand, TTH frequency was more than or equal to once a month in all controls. This difference was statistically significant (p = 0.02) (Table 3).
According to the temporal profile, among 103 JME patients with primary headache, 82 (79.6%) described IIHA and 21 (20.4%) described PIHA [8 preIHA ve 13 postIHA]. No statistically significant correlation was found between the primary headache type and the temporal relation of headache with seizure (p > 0.05) (Fig. 1).
There were five JME patients with resistant epilepsy, in which we defined resistant epilepsy as more than two myoclonic seizures a month. Among these five JME patients with resistant epilepsy, four described migraine, whereas only one described TTH.
Discussion
Headache is one of the most common comorbidities in epilepsy. The prevalence of headache in patients with unselected epilepsy was reported as between 52 and 66% [15,15,17]. Schankin et al. reported headache prevalence in 75 JME patients as 63% [15]. Other than that, there is a strong epidemiological association between epilepsy and migraine. The occurrence of both disorders in the same individual is also more frequent than is to be expected on the basis of occurrence by chance [18]. A prevalence of migraine was reported between 8 and 32.9% in respect to unselected epilepsy [8, 16, 17, 19]. Epilepsy prevalence in the migraine population is also high, ranging between 1 and 17% [20]. Schankin et al. reported migraine as more frequent among JME patients (41%) [15]. In our study, migraine frequency was 23.5% in JME patients and 16% in control group. Our control group migraine prevalence result (16%) was in line with the data of population-based migraine prevalence study done in our country in both 2008 (16.4%) and 2013 (16.7%) [21].
Migraine and epilepsy are both episodic disorders characterized by paroxysmal bursts of transient cerebral dysfunction. The mechanisms underlying the association of migraine and epilepsy have not been fully understood. Cortical spreading depression (CSD) is known to be the mechanism taking part in pathophysiology of migraine [21]. The higher frequency of migraine in JME might be explained by CSD’s being seen more often in patients with JME than controls. This is also consistent with the hypothesis that epileptic foci and CSD might facilitate each other [22]. Epileptic discharges with or without additional cortical epileptic signs or symptoms might stimulate the onset of CSD, resulting in activation of the trigeminovascular system and in headache [23].
Likewise, epilepsy is more frequent in patients suffering from migraine [6,7,8]. This may be explained by the hypothesis of excessive neocortical cellular excitability, the common pathophysiological mechanisms in migraine and epilepsy [17]. Ionotropic glutamate receptors play roles in both migraine and epilepsy, with N-methyl-Daspartate receptors that have critical role in CSD in migraine [18]. Some forms of epilepsy and migraine are known to be channelopathies and ionic channels seem to be the starting point of a common mechanism that leads to migraine and epilepsy [17, 18]. Genetic links are also present between the two disorders, particularly evident in the familial hemiplegic migraine. Also, anticonvulsants are found to be effective for both migraine and epilepsy, again pointing an overlap between the two disorders. Our study revealed higher migraine frequency in JME patients than otherwise healthy control group. However, whether migraine is more frequent in JME patients compared to other epileptic syndromes is still unclear. We hope that following this data, future studies concerning headache in epileptic syndromes other than JME may help form an idea.
Since JME has a strong genetical background, evident in fact that there is a positive family history of seizures in at least 40% of JME patients, headache in JME, especially migraine, is also thought to have a genetical background [24]. Schankin et al. had reported migraine frequency in first-degree relatives of JME patients as 22.5% [15]. In our study, family history of migraine or epilepsy in JME patients with migraine (70.2%) was more frequent. We thought our results may support the genetically background of migraine in JME patients, probably more than healthy population.
In our study, relief of pain with sleep is significantly more common in JME patients with migraine. It is known that excitability of the motor cortex is increased in JME patients and further enhanced after sleep deprivation, which triggers epileptic seizures. Likewise, irregularity of sleep triggers migraine attacks and sleep relieves pain. According to these common known facts about sleep effect on seizures and headache, our data may suggest a common underlying pathophysiology in both seizures and migraine in JME.
Furthermore, migraine pain duration was found longer in JME patients. We thought that this may be explained by patients’ avoidance to take analgesics, due to fear of possible AED interactions and decreasing seizure threshold. Similar to our findings, Gameleira et al. showed that migraine duration was more than 4 h in epilepsy patients [17].
In our study, 4 patients out of 5 drug resistant JME patients (80%) had migraine. Similarly in literature; Brodtkorb et al. found migraine in 5 out of 11 subjects with active epilepsy (45%) and in 4 out of 28 (14%) with epilepsy in remission [25]. Schankin et al. reported more frequent headaches in JME patients, who were suffering from more than 1 GTCS a month [15]. All these data suggest higher migraine frequency among patients suffering from resistant epilepsies. However, our sample size of drug resistant epilepsy was quite small.
According to the Multicenter Epidemiology of Headache in Turkey Study (2007), the 1-year prevalence of TTH was determined as 31.7% [26]. Gameleire reported TTH prevalence as 9.2% in epilepsy patients; Schankin et al. reported TTH prevalence as 40% in JME patients [15, 17]. Our study revealed TTH frequency in JME patients as 26%. On the other hand, 33% of otherwise healthy controls declared that TTH and migraine frequencies were similar among JME patients with headache (42.3%, 46.8%). Our TTH frequency in JME was lower than Schankin et al., just like migraine frequency. We thought that this difference may probably be due to different pain thresholds among people from different cultures.
Tension type headaches of JME patients were relieved mostly by either sleep or spontaneously. Similarly, healthy subjects with TTH need sleep to get well. This pain characteristic, relief with sleep, just like in migraine, may support the special effect of sleep-related factors in JME patients.
Another point is the possible clinical similarities of migraine and TTH in JME patients. In our study, what caught our attention is that some TTH characteristics resembled migraine-type headache characteristics, such as pain relief with sleep and being throbbing in nature. In literature, an electrophysiological similarity of TTH to MO was reported, supporting the hypothesis that some patients with TTH might be at the mild end of the migraine spectrum [26].
According to the temporal profile, in our study, IIHA frequency in JME patients were 41%. IIHA was the most frequent type described in JME patients with primary headache, independent from the primary headache type. In literature, IIHA frequency in patients with epilepsy was reported as between 19 and 31% [27, 28]. Of these IIHAs, 50% were TTH, 45.1% were migraine (15.9% migraine with aura, 29.2% migraine without aura), and 4.9% were both TTH and migraine. Duschaczek et al. reported IIHA frequency in epilepsy patients as 34.3%; of these, 19% were TTH and 11% were migraine [12]. Same study revealed PIHA frequency as 35% (62% TTH, 26% migraine). PIHAs were reported as preIHA in 20% and as postIHA in 80% patients in that study [12]. In our study, PIHA frequency in JME patients was 10.5%. 61.9% of PIHA were post-ictal and 38.1% were pre-ictal. Dushanczek et al. found TTH a little more frequent among IIHA types; however, study revealed similar frequencies of primary headache types among IIHAs [12]. Mainieri (2015) reported migraine predominance in pre- and post-ictal type headaches [29]. Ito and Sachner report that a majority of epilepsy patients with PIHA have headaches with characteristics that fit into IIHA [30]. In our study, migraine and TTH headache frequencies among pre- and post-ictal headaches were also similar. There was no IHA in our study. Ictal epileptic headache is diagnosed when headache is the only clinical feature of epileptiform discharges and resolves after administrating an intravenous anticonvulsant drug [31]. To put the diagnosis of IHA in clinics seems hard and may easily be missed. We thought that in our study, we may have missed such a difficult diagnosis because our data mostly relied on self-administered questionnaire results.
In conclusion, present study revealed similar headache frequencies in between JME and healthy controls. However, migraine frequency was higher in JME patients, and TTH was the most frequent headache type in healthy controls. Family history of migraine or epilepsy was higher in JME patients. Some pain characteristics of migraine (duration, localization, and relief with sleep) and some pain characteristics of TTH (quality, beginning, frequency, and duration) were different in JME patients and healthy controls. These differences of headache characteristics found in JME patients may suggest the role of common pathophysiology of headache and JME, as well as ongoing AED treatments. The primary headache types were not significantly different, whether it was an IIHA or PIHA headache. In conclusion, we suggest that our results support the genetic relationship, the shared hypothetical pathopysiological mechanisms, and prophylactic medical agents used between JME and headache, especially migraine.
References
Velioğlu SK, Yüzgül N (2010) The association between epilepsy and migraine. Epilepsia 16:167–172
Velioğlu SK, Ozmenoğlu M (1999) Migraine-related seizures in an epileptic population. Cephalalgia 19(9):797–801. https://doi.org/10.1046/j.1468-2982.1999.1909797.x
Yankovsky AE, Andermann F, Bernasconi A (2005) Characteristics of headache associated with intractable partial epilepsy. Epilepsia 46(8):1241–1245. https://doi.org/10.1111/j.1528-1167.2005.64804.x
Marks DA, Ehrenberg BL (1993) Migraine-related seizures in adults with epilepsy, with EEG correlation. Neurology 43(12):2476–2483. https://doi.org/10.1212/WNL.43.12.2476
Headache clasification Comitee of the International Headache Society (1988) Classification and diagnostic criteria for headache disorders. Cranial neuralgias and facial pain. Cephalalgia 8:1–96
Matias-Guiu J, Galiano L, Vioque J, Falip R, Martin R (1992) A case-control study to evaluate the association of epilepsy and migraine. Neuroepidemiology 11(4-6):313–314. https://doi.org/10.1159/000110947
Lipton RB, Ottman R, Ehrenberg BL, Hauser WA (1994) Comorbidity of migraine: the connection between migraine and epilepsy. Neurology 44:28–32
Andermann F (1987) Clinical features of migraine-epilepsy syndromes. In: Andermann F, Lugaresi E (eds) Migraine and epilepsy. Butterworths, London, pp 3–30
Nordli DR Jr (2005) Idiopathic generalized epilepsies recognized by the International League Against Epilepsy. Epilepsia 46(s9):48–56. https://doi.org/10.1111/j.1528-1167.2005.00313.x
Janz D (1985) Epilepsy with impulsive petit mal (juvenile myoclonic epilepsy). Acta Neurol Scand 72(5):449–459
Appleton R, Beirne M, Acomb B (2000) Photosensitivity in juvenile myoclonic epilepsy. Seizure 9(2):108–111. https://doi.org/10.1053/seiz.1999.0376
Duchaczek B, Ghaeni L, Matzen J, Holtkamp M (2013) Interictal and periictal headache in patients with epilepsy. Eur J Neurol 20(10):1360–1366. https://doi.org/10.1111/ene.12049
Berg AT, Berkovic SF, Brodie MJ, Buchhalter J, Cross JH, van Emde Boas W, Engel J, French J, Glauser TA, Mathern GW, Moshé SL, Nordli D, Plouin P, Scheffer IE (2010) Revised terminology and concepts for organization of seizures and epilepsies:report of the ILAE Commission on Classification and Terminology, 2005–2009. Epilepsia 51(4):676–685. https://doi.org/10.1111/j.1528-1167.2010.02522.x
Headache Classification Subcommitee of the International Headache Society (2013) The international classification of headache disorders: 3rd edition (beta version). Cephalalgia 33(9):629–808. https://doi.org/10.1177/0333102413485658
Schankin CJ, Rémi J, Klaus I, Petra Sostak P, Reinisch VM, Noachtar S et al (2011) Headache in juvenile myoclonic epilepsy. J Headache Pain 12(2):227–233. https://doi.org/10.1007/s10194-011-0332-6
Syvertsen M, Helde G, Stovner LJ, Brodtkorb E (2007) Headaches add to the burden of epilepsy. J Headache Pain 8(4):224–230. https://doi.org/10.1007/s10194-007-0398-3
Gameleira FT, Ataíde L Jr, Raposo MC (2013) Relations between epileptic seizures and headaches. Seizure 22(8):622–626. https://doi.org/10.1016/j.seizure.2013.04.016
Verrotti A, Striano P, Belcastro V, Matricardi S, Villa MP, Parisi P (2011) Migralepsy and related conditions: advances in pathophysiology and classification. Seizure 20(4):271–275. https://doi.org/10.1016/j.seizure.2011.02.012
Stevenson SB (2006) Epilepsy and migraine headache: is there a connection? J Pediatr Health Care 20(3):167–171. https://doi.org/10.1016/j.pedhc.2005.10.014
Caminero A, Manso-Calderon R (2014) Links between headaches and epilepsy: current knowledge and terminology. Neurologia 29(8):453–463. https://doi.org/10.1016/j.nrl.2011.10.016
Baykan B, Ertas M, Karlı N, Uluduz D, Uygunoglu U, Ekizoglu E, Kocasoy Orhan E, Saip S, Zarifoglu M, Siva A (2015) Migraine incidence in 5 years: a population-based prospective longitudinal study in Turkey. J Headache Pain 16(1):103. https://doi.org/10.1186/s10194-015-0589-2
Parisi P (2009) Why is migraine rarely, and not usually, the sole ictal epileptic manifestation? Seizure 18(5):309–312. https://doi.org/10.1016/j.seizure.2009.01.010
Parisi P (2009) Who’s still afraid of the link between headache and epilepsy? Some reactions to and reflections on the article by Marte Helene Bjork and co-workers. J Headache Pain 10(5):327–329. https://doi.org/10.1007/s10194-009-0149-8
Liu AW, Delgada-Escueta AV, Gee MN, Serratosa JM, Zhang QW, Alonso ME et al (1996) Juvenile myoclonic epilepsy in chromosome 6p12-q11: locus heterogeneity and recombinations. Am J Med Genet 63(3):438–446. https://doi.org/10.1002/(SICI)1096-8628(19960614)63:3<438::AID-AJMG5>3.0.CO;2-N
Brodtkorb E, Bakken IJ, Sjaastad O (2008) Comorbidity of migraine and epilepsy in a Norwegian community. Eur J Neurol 15(12):1421–1423. https://doi.org/10.1111/j.1468-1331.2008.02353.x
Ozkul Y, Ay H (2007) Habituation of sympathetic skin response in migraine and tension type headache. Auton Neurosci 134(1-2):81–84. https://doi.org/10.1016/j.autneu.2007.02.006
Kwan P, Man CB, Leung H, Yu E, Wong KS (2008) Headache in patients with epilepsy: a prospective incidence study. Epilepsia 49(6):1099–1102. https://doi.org/10.1111/j.1528-1167.2008.01574.x
Bernasconi A, Andermann F, Bernasconi N, Reutens DC, Dubeau F (2001) Lateralizing value of peri-ictal headache: a study of 100 patients with partial epilepsy. Neurology 56(1):130–132
Mainieri G, Cevoli S, Giannini G, Zummo L, Leta C, Broli M, Ferri L, Santucci M, Posar A, Avoni P, Cortelli P, Tinuper P, Bisulli F (2015) Headache in epilepsy: prevalence and clinical features. J Headache Pain 16(1):72. https://doi.org/10.1186/s10194-015-0556-y
Ito M, Schachter SC (1996) Frequency and characteristics of interictal headaches in patients with epilepsy. J Epilepsy 9(2):83–86. https://doi.org/10.1016/0896-6974(96)00004-7
Mameniskiene R, Karmonaite I, Zagorskis R (2016) The burden of headache in people with epilepsy. Seizure 41:120–126. https://doi.org/10.1016/j.seizure.2016.07.018
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Local Ethic Committee of Bakirkoy Prof. Dr. Mazhar Osman Training and Research Hospital for Psychiatric, Neurologic and Neurosurgical Diseases. (The register number of the ethics committee: 30.12.2014/70787)
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Dedei Daryan, M., Güveli, B.T., Baslo, S.A. et al. Prevalence and clinical characteristics of headache in juvenile myoclonic epilepsy: experience from a tertiary epilepsy center. Neurol Sci 39, 519–525 (2018). https://doi.org/10.1007/s10072-017-3232-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-017-3232-y