Abstract
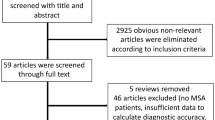
Differential diagnosis of progressive supranuclear palsy (PSP) and the parkinsonian variant of multiple system atrophy (MSA-P) from Parkinson’s disease (PD) can be difficult, particularly in atypical cases or early in the disease course. The Magnetic Resonance Parkinsonism Index (MRPI) utilizes linear and surface (planimetry) measurements and has been proposed as a dual MRI biomarker, with high values indicative of PSP and low values of MSA. The aim of this study was to examine the utility of simple linear MRI brainstem measurements, without the use of MRI planimetry, in the diagnosis of patients with Parkinsonism and compare them to the MRPI. A total of 51 patients (PSP: 24, MSA-P: 9, PD: 18) and 15 healthy controls were included. Simple linear MRI distances of brainstem structures were measured. These included midbrain and pons diameters as well as superior cerebellar peduncle (SCP) and middle cerebellar peduncle (MCP) widths. All relevant indices, including ratios and products, were also calculated. The SCP by midbrain product (SCP × midbrain) provided improved sensitivity (100 vs. 91%) and identical specificity (98%) for the diagnosis of PSP, compared to the MRPI. Neither the MRPI nor any of the linear measurements were able to discriminate MSA-P from PD. The SCP by midbrain product is a novel, potent MRI biomarker for PSP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Progressive supranuclear palsy (PSP) and the parkinsonian variant of multiple system atrophy (MSA-P) are neurodegenerative disorders with distinct clinical features. Differential diagnosis however is often difficult, particularly in early and/or atypical cases. Established clinical diagnostic criteria lack sensitivity [1, 2]. As a result, these patients are underdiagnosed and may receive a possible/probable diagnosis in later stages of their disease course. This raises the need for a biomarker to assist clinical diagnosis.
PSP is characterized by severe midbrain and superior cerebellar peduncle (SCP) atrophy [3], which may appear early in the disease course, years before the clinical presentation is complete [4]. In this context, brainstem measurements have been successfully used to predict PSP in patients with unclassified Parkinsonism [5].
MSA presents either as a cerebellar form (MSA-C) or a parkinsonian form (MSA-P). The former usually do no enter in the differential diagnosis of a patient with Parkinsonism, due to their predominant cerebellar signs. On the contrary, MSA-P patients may often be clinically indistinguishable from PSP and PD; however, they may also show pons and middle cerebellar peduncle atrophy (MCP) [6]. These data imply that a specific MRI atrophy pattern could assist in an early clinical diagnosis.
The topographic selectivity of brain atrophy has yielded several promising potential MRI biomarkers, by the use of variable MRI modalities, such as volumetry, diffusivity, and planimetry as well as simple linear measurements. Linear MRI measurements are easily performed and reproducible in routine MRI sequences and are therefore practical from a clinical standpoint. The remaining MRI modalities require elaborate MRI sequences, strict standardization of image acquisition, and/or burdensome post-acquisition analysis, which may pose difficulties in everyday clinical practice.
The midbrain/pons ratio [7] and particularly the Magnetic Resonance Parkinsonism Index (MRPI) have emerged as potent dual imaging biomarkers in Parkinson-plus patients [8]. The MRPI utilizes both linear and surface measurements (planimetry). It is calculated by multiplying the pons/midbrain surface ratio by the MCP/SCP width ratio (pons/midbrain × MCP/SCP). Higher values are supported to indicate PSP and lower values MSA. The MRPI has been proven to assist in the differential diagnosis of PSP from PD and vascular Parkinsonism [9, 10].
The aim of this study was to examine the utility of exclusively linear MRI brainstem distances in the differential diagnosis of prospectively diagnosed PSP and MSA-P patients and compare their diagnostic accuracy against the MRPI.
Patients and methods
Patients
Patients were consecutively and prospectively recruited between 2011 and 2014, as part of the Parkinson-plus Registry of our Department. All patients underwent a comprehensive neurological examination and a detailed neurological history was obtained. The minimal follow-up period was 2 years. Ancillary tests were performed in all patients as appropriate, to exclude secondary causes of Parkinsonism.
The Unified Parkinson’s Disease Rating Scale (UPDRS) motor examination (Part III) was performed in all patients. To document opthalmokinetic abnormalities, saccade velocity was semiquantitatively scored in each axis (up, down, left, right) as follows: 0, normal; 1, slight slowing; 2, medium slowing; 3, severe slowing; 4, no saccade. This produced a saccade velocity score from 0 to 16. Likewise, hypometria of gaze was scored in each axis as follows: 0, normal; 1, mild hypometria; 2, medium hypometria; 3, severe hypometria; 4, no movement. A total hypometria score from 0 to 16 was calculated.
All patients fulfilled the established criteria for probable progressive supranuclear palsy [11] or probable multiple system atrophy of the parkinsonian variant (MSA-P) [12]. Since all PSP patients fulfilled the “probable” criteria, only patients with a Richardson syndrome (PSP-RS) were included, with early postural instability and falls as well as early supranuclear gaze palsy. A group of 11 patients, fulfilling the UK Parkinson’s Disease Society Brain Bank criteria [13], were included for comparison reasons. Furthermore, 15 otherwise healthy individuals, with no history of neurological, psychiatric, or other major disease and no signs of Parkinsonism or cognitive dysfunction, served as a control group. They were admitted in our Department for non-relevant issues (headache, dizziness, etc.) and had a normal MRI. MSA-C patients were not included in the present study, because they do no enter in the differential diagnosis of a patient with Parkinsonism, due to their predominant cerebellar semiology.
The study was performed with the approval of the Scientific and Ethical Committee of our Hospital, according to the ethical guidelines of the 1964 Declaration of Helsinki. All patients (or in cases of compromised mental capacity the next of kin carer) gave written informed consent to participate in the study.
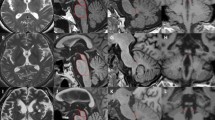
MRI acquisition
Magnetic resonance imaging was performed on a variety of high-field MRI units (Philips Medical Systems—Achieva 3.0 T (TX) and Intera 1.5 T, Siemens—Magnetom Avanto 1.5 T, Magnetom Epree 1.5 T, Magnetom Skyra 3 T and Magnetom Symphony 1.5 T and GE Medical Systems—Genesis Signa 1.5 T and Signa Excite 1.5 T). The sequences included T1-weighted axial, sagittal, and coronal images or 3D T1 W Turbo Field Echo sequences. MRI specifications were as follows: TR repetition time range 500–650 ms, TE echo time range 10–15 ms, FOV range 24–25 cm, matrix range 192 × 256 to 320 × 320, section thickness 1–5 mm, intersection spacing 1 mm.
Linear brainstem measurements were measured midsagittally, parallel to the chiasmatico-commissural plane. These included the following: the maximal antero-posterior (A-P) midbrain distance, the A-P pons distance, the A-P superior colliculus (SC), and the A-P inferior colliculus (IC) distance. Distances measured at the axial level included the maximal A-P midbrain and pons distances, as well as maximal SCP and MCP widths. Furthermore, maximal MCP width was also measured parasagittally. The SCP width were also measured coronally, as opposed to the methodology described by Quattrone et al. [8]. This was decided due to the lack of 3D T1 W Turbo Field Echo sequences in some of the patients (Supplementary Fig. 1).
To improve discriminative power for PSP and MSA, the products of midbrain × SCP and of pons × MCP, respectively, were also calculated. In an attempt to differentiate MSA from PSP, the midbrain/pons, MCP/SCP, and SC/IC distance ratios at all available planes were included. The MRPI, with replacement of the midbrain and pons surfaces by their respective maximal A-P midsagittal distances, was also reported (MRPI dist ). For comparison reasons, the MRPI (as described in the introduction) was also calculated.
The rostral midbrain angle (angle of the anterior one half of the rostral midbrain border to a plane perpendicular to the respective posterior one half at the midsagittal section) was also calculated (Supplementary Fig. 2). This was performed in an effort to provide an objective, measurable substrate of the “hummingbird sign.” This sign is in part produced by the concave appearance of the rostral midbrain (which is convex in healthy controls). The interpeduncular angle at the axial plane was also measured.
Statistical analysis
Numerical variables were checked for normality and homogeneity of variances by the Shapiro Wilk’s and Levene’s tests, respectively. ANCOVA, using the diagnosis, gender, and magnetic field strength (1.5 vs. 3.0 T) as co-factors and age as a covariate, followed by post hoc analysis with Bonferroni correction for multiple comparisons or Kruskal-Wallis test (followed by Dunn’s post hoc test) were used as appropriate. Receiver operating characteristic (ROC) curve analysis was applied for determination of the diagnostic value of each biomarker. Nonparametric pairwise comparison of ROC curve AUCs was performed by use of the DeLong method. Spearman’s rank correlation coefficient was applied to correlate clinical with imaging data. All analyses were performed by IBM SPSS Statistics® version 22.0.0.0 (SPSS Inc., Chicago, IL, 2013) and MedCalc version 12.5 (MedCalc Software, Belgium, 2013). All graphs were designed using GraphPad Prism®, version 5.03 (GraphPad Software Inc., La Jolla, CA, 2009).
Results
A total of 66 patients were included in the study (PSP, n = 24; MSA-P, n = 9; PD, n = 18; ctrls, n = 15). Study groups did not differ significantly in respect to age, gender, or education (Table 1). PD patients had significantly greater disease duration, as expected. ANCOVA revealed significant effects by diagnostic group, but the models were not affected significantly by any of the co-factors and covariates.
The saccade velocity score correlated significantly with the A-P midbrain sagittal diameter (R = − 0.486, p = 0.22), midbrain/pons sagittal ratio (R = − 0.449, p = 0.036), SCP coronal width (R = − 0.647, p = 0.002), MCP sagittal to SCP coronal ratio (R = − 0.514, p = 0.020), MRPI (R = − 0.601, p = 0.005), and midbrain sagittal × SCP coronal product (r = − 0.621, p = 0.003). The hypometria score correlated with the SCP coronal width (R = − 0.561, p = 0.008), MRPI (R = − 0.454, p = 0.044), and midbrain sagittal × SCP coronal product (r = − 0.506, p = 0.019). No MRI measurement correlated with the UPDRS III score.
PSP patients exhibited significantly smaller midbrain distances and SCP widths compared to all other groups. Consequently, all midbrain and/or SCP-derived indices also differed significantly. Rostral midbrain and interpeduncular angles were significantly increased in PSP. Interestingly, PSP patients showed mild pons and MCP atrophy (Table 2).
MSA-P patients showed mild pons atrophy, which was not statistically significant. They did not differ from the control group in any of the simple linear measurements, with the exception of MCP atrophy, as measured at the sagittal plane.
PD patients did not differ from the control group in any of the MRI measurements.
No MRI measurement or index provided clinically useful (> 80%) combined sensitivity and specificity for the diagnosis of MSA-P. The MRPI (cut-off point of ≤ 10.9) discriminated MSA-P patients from the other groups, with a 100% sensitivity and 55% specificity. A MCP sag /SCP axial value of ≤ 2.32 had a 100% specificity and 67% sensitivity for MSA-P (Table 3, Supplementary Figs. 3 and 4).
In regard to PSP, the SCP × midbrain product (SCP coronally and A-P midbrain midsagittally measured) provided an excellent combination of sensitivity (100%) and specificity (98%) for the diagnosis of PSP (cut-off ≤ 30.9 mm2). In comparison to the MRPI, it provided improved sensitivity (100 vs. 91%). The MRPI, SCP cor , MRPI dist-axial , and midbrain/pons sag were also potent in discriminating PSP from all other groups. Pairwise comparison of ROC curve AUCs of these indices did not reveal significant differences (Table 4, Supplementary Figs. 5 and 6).
Discussion
The present study investigated the utility of simple MRI measurements and indices in the differential diagnosis of Parkinson-plus patients. These measurements were then compared to the MRPI, which is supported to function as a dual imaging biomarker.
Many studies support the utility of the MRPI in the differential diagnosis of PSP from MSA-P, PD, and healthy controls [4, 14,15,16,17,18]. In our study, an MRPI value of > 12.6 was highly suggestive of PSP, in accordance to the literature.
Interestingly, in our cohort, the midbrain × SCP product provided comparable (and numerically superior) discriminative power for the diagnosis of PSP, compared to the MRPI. This could be attributed to the following: Firstly, PSP patients exhibited a degree of pons and MCP atrophy in our cohort. Indeed, pathological studies of PSP patients have supported this finding, by reporting concomitant pontine, in addition to the predominant midbrain atrophy in PSP patients [3, 19]. Secondly, MSA-P patients, did not exhibit pons atrophy in our study. Mild MCP atrophy was evident only in the sagittal plane. Thirdly, the methodology we applied to measure SCPs differed from the one described in the literature. More specifically, we measured the SCPs on a coronal plane, as opposed to the oblique coronal plane generated by 3D T1 W Turbo Field Echo sequences.
Taking this data into account, the incorporation of pons or MCP atrophy measurements in a MRI biomarker that intended to differentiate PSP from MSA-P does not increase (but could theoretically decrease) its discriminative power.
Furthermore, the midbrain × SCP product relies on linear MRI measurements and can therefore be applied in the everyday clinical setting, without requiring MRI planimetry measurement software. MRPI on the other hand requires both planimetry (pons and midbrain surface) and linear measurements (SCP and MCP widths).
Surprisingly, the MRPI did not provide adequate (> 80%) combined sensitivity and specificity for the diagnosis of MSA-P in our cohort, due to only mild pontine and MCP atrophy in these patients. This is in apparent disagreement with studies that have reported pons and MCP atrophy in MSA-P patients [8, 20]. However, as was the case in our study, in these reports, there was great overlap of individual values between PD and MSA-P patients. Moreover, only two studies have supported that MRI measurements (midbrain/pons ratio) can differentiate MSA from PD [7, 21]. However, these studies incorporated MSA-C patients.
Based on these findings, we hypothesize that the MRPI, although useful, may not be as diagnostically efficient as previously thought, especially for MSA-P. However, it is conceivable that low MRPI values may be particularly useful for MSA-C.
Our study, like most studies in the field, lacks pathologic confirmation, which would provide a “definite” diagnosis. Thus, we selected a prospective design for our study, contrary to the retrospective design of other studies, and all cases were followed up for at least 2 years. This may enhance the validity of clinical data and strengthen the clinical diagnosis. Furthermore, only patients with a “probable” diagnosis were included. Most relevant studies in the field have moderate cohort sizes, similar to our study. This is expected for such rare diseases as PSP and MSA-P.
Linear MRI measurements can greatly assist in the early differential diagnosis of PSP patients from both PD and MSA-P. However, they do not seem to be useful in the discrimination between MSA-P and PD, which is a common clinical scenario. Towards this direction, prospective studies combining MRI, clinical, and pathological data are needed.
References
Respondek G, Roeber S, Kretzschmar H, Troakes C, Al-Sarraj S, Gelpi E, Gaig C, Chiu WZ, van Swieten JC, Oertel WH, Höglinger GU (2013) Accuracy of the National Institute for Neurological Disorders and Stroke/Society for Progressive Supranuclear Palsy and neuroprotection and natural history in Parkinson plus syndromes criteria for the diagnosis of progressive supranuclear palsy. Mov Disord 28(4):504–509. https://doi.org/10.1002/mds.25327
Osaki Y, Ben-Shlomo Y, Lees AJ, Wenning GK, Quinn NP (2009) A validation exercise on the new consensus criteria for multiple system atrophy. Mov Disord 24(15):2272–2276. https://doi.org/10.1002/mds.22826
Hauw J-J, Daniel SE, Dickson D, Horoupian DS, Jellinger K, Lantos PL, McKee A, Tabaton M, Litvan I (1994) Preliminary NINDS neuropathologic criteria for Steele-Richardson-Olszewski syndrome (progressive supranuclear palsy). Neurology 44(11):2015–2019. https://doi.org/10.1212/WNL.44.11.2015
Slowinski J, Imamura A, Uitti RJ, Pooley RA, Strongosky AJ, Dickson DW, Broderick DF, Wszolek ZK (2008) MR imaging of brainstem atrophy in progressive supranuclear palsy. J Neurol 255(1):37–44. https://doi.org/10.1007/s00415-007-0656-y
Morelli M, Arabia G, Novellino F, Salsone M, Giofre L, Condino F, Messina D, Quattrone A (2011) MRI measurements predict PSP in unclassifiable Parkinsonisms: a cohort study. Neurology 77(11):1042–1047. https://doi.org/10.1212/WNL.0b013e31822e55d0
Trojanowski JQ, Revesz T (2007) Proposed neuropathological criteria for the post mortem diagnosis of multiple system atrophy. In: Neuropathol Appl Neurobiol pp 615–620
Kaasinen V, Kangassalo N, Gardberg M, Isotalo J, Karhu J, Parkkola R, Sonninen P (2015) Midbrain-to-pons ratio in autopsy-confirmed progressive supranuclear palsy: replication in an independent cohort. Neurol Sci 36(7):1251–1253. https://doi.org/10.1007/s10072-015-2184-3
Quattrone A, Nicoletti G, Messina D, Fera F, Condino F, Pugliese P, Lanza P, Barone P, Morgante L, Zappia M, Aguglia U, Gallo O (2008) MR imaging index for differentiation of progressive supranuclear palsy from Parkinson disease and the Parkinson variant of multiple system atrophy. Radiology 246(1):214–221. https://doi.org/10.1148/radiol.2453061703
Mostile G, Nicoletti A, Cicero CE, Cavallaro T, Bruno E, Dibilio V, Luca A, Sciacca G, Raciti L, Contrafatto D, Chiaramonte I, Zappia M (2016) Magnetic resonance Parkinsonism index in progressive supranuclear palsy and vascular parkinsonism. Neurol Sci 37(4):591–595. https://doi.org/10.1007/s10072-016-2489-x
Kim BC, Choi S-M, Choi K-H, Nam TS, Kim JT, Lee SH, Park MS, Yoon W (2017) MRI measurements of brainstem structures in patients with vascular parkinsonism, progressive supranuclear palsy, and Parkinson’s disease. Neurol Sci 38(4):627–633. https://doi.org/10.1007/s10072-017-2812-1
Litvan I, Agid Y, Calne D, Campbell G, Dubois B, Duvoisin RC, Goetz CG, Golbe LI, Grafman J, Growdon JH, Hallett M, Jankovic J, Quinn NP, Tolosa E, Zee DS (1996) Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome): report of the NINDS-SPSP international workshop. Neurology 47(1):1–9. https://doi.org/10.1212/WNL.47.1.1
Gilman S, Wenning GK, Low PA, Brooks DJ, Mathias CJ, Trojanowski JQ, Wood NW, Colosimo C, Durr A, Fowler CJ, Kaufmann H, Klockgether T, Lees A, Poewe W, Quinn N, Revesz T, Robertson D, Sandroni P, Seppi K, Vidailhet M (2008) Second consensus statement on the diagnosis of multiple system atrophy. Neurology 71(9):670–676. https://doi.org/10.1212/01.wnl.0000324625.00404.15
Hughes AJ, Daniel SE, Kilford L, Lees AJ (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55(3):181–184. https://doi.org/10.1136/jnnp.55.3.181
Cosottini M, Ceravolo R, Faggioni L, Lazzarotti G, Michelassi MC, Bonuccelli U, Murri L, Bartolozzi C (2007) Assessment of midbrain atrophy in patients with progressive supranuclear palsy with routine magnetic resonance imaging. Acta Neurol Scand 116(1):37–42. https://doi.org/10.1111/j.1600-0404.2006.00767.x
Longoni G, Agosta F, Kostić VS, Stojković T, Pagani E, Stošić-Opinćal T, Filippi M (2011) MRI measurements of brainstem structures in patients with Richardson’s syndrome, progressive supranuclear palsy-parkinsonism, and Parkinson’s disease. Mov Disord 26(2):247–255. https://doi.org/10.1002/mds.23293
Morelli M, Arabia G, Salsone M, Novellino F, Giofrè L, Paletta R, Messina D, Nicoletti G, Condino F, Gallo O, Lanza P, Quattrone A (2011) Accuracy of magnetic resonance parkinsonism index for differentiation of progressive supranuclear palsy from probable or possible Parkinson disease. Mov Disord 26(3):527–533. https://doi.org/10.1002/mds.23529
Massey LA, Jager HR, Paviour DC, O'Sullivan SS, Ling H, Williams DR, Kallis C, Holton J, Revesz T, Burn DJ, Yousry T, Lees AJ, Fox NC, Micallef C (2011) The midbrain to pons ratio: a simple and specific MRI sign of progressive supranuclear palsy. Mov Disord 80(20):1856–1861. https://doi.org/10.1212/WNL.0b013e318292a2d2
Kim YH, Il MH, Kim YJ (2015) Utility of the midbrain tegmentum diameter in the differential diagnosis of progressive supranuclear palsy from idiopathic Parkinson’s disease. J Clin Neurol 11(3):268–274. https://doi.org/10.3988/jcn.2015.11.3.268
Aiba I, Hashizume Y, Yoshida M, Okuda S, Murakami N, Ujihira N (1997) Relationship between brainstem MRI and pathological findings in progressive supranuclear palsy--study in autopsy cases. J Neurol Sci 152(2):210–217. https://doi.org/10.1016/S0022-510X(97)00166-4
Hussl A, Mahlknecht P, Scherfler C, Esterhammer R, Schocke M, Poewe W, Seppi K (2010) Diagnostic accuracy of the magnetic resonance Parkinsonism index and the midbrain-to-pontine area ratio to differentiate progressive supranuclear palsy from Parkinson’s disease and the Parkinson variant of multiple system atrophy. Mov Disord 25(14):2444–2449. https://doi.org/10.1002/mds.23351
Massey LA, Jager HR, Paviour DC, O’Sullivan SS, Ling H, Williams DR, Kallis C, Holton J, Revesz T, Burn DJ, Yousry T, Lees AJ, Fox NC, Micallef C (2013) The midbrain to pons ratio: a simple and specific MRI sign of progressive supranuclear palsy. Neurology 80(20):1856–1861. https://doi.org/10.1212/WNL.0b013e318292a2d2
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was performed with the approval of the Scientific and Ethical Committee of our Hospital, according to the ethical guidelines of the 1964 Declaration of Helsinki. All patients (or in cases of compromised mental capacity the next of kin carer) gave written informed consent to participate in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
ESM 1
(PDF 4184 kb)
Rights and permissions
About this article
Cite this article
Constantinides, V.C., Paraskevas, G.P., Stamboulis, E. et al. Simple linear brainstem MRI measurements in the differential diagnosis of progressive supranuclear palsy from the parkinsonian variant of multiple system atrophy. Neurol Sci 39, 359–364 (2018). https://doi.org/10.1007/s10072-017-3212-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-017-3212-2