Abstract
Tandem gait testing is an integral part of the neurological exam. It is informative in a wide variety of disorders ranging from cerebellar disease to vestibular and peripheral neuropathies, parkinsonism, and other neurodegenerative conditions. We discuss the history and development of tandem gait testing as well as its technique, utility, and limitations in the assessment of neurological conditions. Tandem gait has emerged as a tool in the assessment of cerebellar disease, Huntington disease, idiopathic Parkinson’s disease, atypical parkinsonism, peripheral neuropathies, and vestibulopathies. Its origin can be deduced from experimental observation and clinical experience as far back as the early nineteenth century. Despite the long history and ubiquitous performance of tandem gait testing, there is no standardized, guideline-based protocol to model for more homogenous research and clinical practices. Such a protocol should be developed using historical texts and manuscripts as well as the consensus of the medical research community. With standard protocols, further studies could define the sensitivity of abnormal tandem gait testing in cerebellar disorders, more diffuse neurodegeneration, and peripheral pathologies. Tandem gait can be a useful marker of dysfunction in neurologic conditions whose pathologies extend beyond the vermis or vestibulocerebellar module to include interconnected networks throughout the nervous system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Testing a patient’s ability to walk heel-to-toe (“tandem gait”) is described in classic neurology text books as a sensitive test for early cerebellar gait abnormalities [1,2,3,4]. Consequently, tandem gait (TG) abnormalities have been used as an argument for invoking the cerebellum as the site of dysfunction in diseases such as essential tremor [5, 6], where pathophysiology is still debated.
Observations from the nineteenth century experimental lesions and of patients who suffered various insults to the cerebellum evolved into the cerebellar exam that we know today [4]. Through these observations and more recent experimental evidence, we are able to localize cerebellar gait abnormalities to the cerebellar vermis, flocculonodular lobe, or cerebellar pathways communicating to brainstem nuclei [4, 5, 7,8,9].
Tandem gait testing extends beyond the examination of cerebellar function as a general test of balance [10]. It can be impaired in parkinsonism (though it is not part of any diagnostic criteria) [11,12,13], peripheral neuropathies [14,15,16], and vestibulopathies [17]. TG can help predict fall risk in Parkinson’s disease (PD) [11]. TG testing may be helpful in differentiating idiopathic PD from atypical parkinsonism (AP), including vascular parkinsonism [12, 13]. TG testing may be useful as a screening tool for patients with suspected peripheral neuropathy or vestibulopathy [16, 17].
The implementation of the TG examination varies from practitioner to practitioner and there is likely intra-practitioner inconsistency. Explicit guidelines have not been published. Descriptions of how patients are instructed to perform TG testing are conspicuously absent from some manuscripts utilizing TG as a parameter. And when the examination is described in a publication, there is heterogeneity in the protocol. Despite the absence of consensus guidelines, guidance is available in the description of TG testing in neurology textbooks and by the protocols used in classic manuscripts.
Tandem gait: historical allusions
Observations from experimental lesions, happenstance lesions, and traumas to the cerebellum evolved into the cerebellar exam (including gait exam) that we know today. One should note that tandem gait or heel-to-toe walking is not explicitly described in any of these historic documentations prior to the late twentieth century. The historical observations are summarized in Table 1.
Luigi Rolando, professor of anatomy in Turin, Italy, in Saggio sopra la vera struttura del cervello dell’uomo e degli animali e sopra le funzioni del sistema nervoso (1809), observed that partial resection of the median lobe of the cerebellum from a goat caused the animal to sway and fall [7]. Marie-Jean-Pierre Flourens, in Recherches expérimentales sur les propriétés et les fonctions du système nerveux dans les animaux vertébrés (1824), described staggering gait in a guinea pig and a dog following ablation of the cerebellum [7].
William Alexander Hammond in A Treatise on the Diseases of the Nervous System (1871) [7] and William Richard Gowers in A Manual of Diseases of the Nervous System [7, 18] describe the “drunken” gait of patient’s with cerebellar disease. Both Hammond and Gowers localize the gait abnormality to the middle cerebellar lobe or vermis. Hammond cites Nothnagel’s observation that a staggering gait “always denotes involvement of the middle lobe (vermis) of the cerebellum” [5].
Charles Karsner Mills, in The Nervous System and Its Diseases, summarized the state of knowledge of the cerebellar examination at the close of the nineteenth century. He delineated syndromes caused by focal lesions of the cerebellum—including the observation that lesions of the anterior cerebellar vermis caused patients to fall forward and caudal vermis resulted in backwards falls [7].
The modern cerebellar exam, including gait testing, was developed from the observations of the nineteenth century. The 1911 edition of Church and Peterson’s Nervous and Mental Diseases [7] and the 1929 edition of Smith Ely Jelliffe and William Alanson White’s Diseases of the Nervous System. A Textbook of Neurology and Psychiatry detailed the cerebellar exam including descriptions of the gait abnormality expected from vermis lesions—quoting the descriptions of Rolando [7], Flourens [7], Hammond [7], Gowers [7, 18], and Mills [7].
In 1998, Bastian et al. [19] described the neurological exam of five children after the surgical transection of the posterior cerebellar vermis. All five children exhibited impaired TG without other abnormalities attributable to the cerebellum. Current experimental evidence also implicates lesions to the floculonodular lobe (particularly the nodulus) or its associated nuclei (fastigial nuclei) and efferent/afferent pathways in gait abnormalities—including description of tandem gait difficulty [9, 20]. It is also noted that such lesions can be difficult to distinguish from lesions of the medial cerebellum (or vermis) [9].
Tandem gait: more formal appearance in the neurological exam
Classic textbooks in neurology, including [1,2,3], discuss TG as an integral part of the cerebellar and gait exam. The test is applied as a means to evaluate cerebellar/vermian dysfunction. Finding an abnormality in TG can aid in detecting the mildest gait ataxia and possibly heralding a progressive gait disorder. It is implied that tandem gait is a sensitive test for early cerebellar dysfunction [1,2,3,4] (interesting to note, we have been unable to find any primary literature attempting to define this sensitivity). In DeJong’s text it is noted that TG stresses the multifactorial gait and balance mechanisms and that obesity and deconditioning can confound the exam [3].
The testing of TG has found a home within widely utilized rating scales to help define and quantify disease severity for clinical and research purposes. It is included in the Scale for the Assessment and Rating of Ataxia (SARA) [21] and the United Huntington’s Disease Rating Scale (UHDRS) [22] to help quantify gait dysfunction in cerebellar ataxias and Huntington’s disease (HD). The “gait” portion of the SARA quantifies gait abnormality with a 0 to 8 scoring system—with 0, 1, and 2 involving testing TG. The inclusion of testing TG in the SARA scale is in keeping with the historical association of TG with cerebellar disease. The bottom quartile of the scoring range involving TG is in line with the concept of TG heralding early cerebellar disease. The motor segment of the UHDRS includes a relatively simple 0 to 4 scoring method to quantify severity of the TG abnormality in patients with Huntington disease. UHDRS motor score has been shown to be predictive of carrying the HD mutation in at-risk patients [23]. We have not found a written statement as to the origin of this choice of assessment in a non-cerebellar disorder. Both of these scales include instructions on the performance of the TG exam.
Tandem gait has been studied as a marker of non-cerebellar disorders. Its utility in differentiating Parkinson’s disease and atypical parkinsonism has been studied. TG has also been studied as a screening tool in peripheral neuropathies and vestibulopathies. Protocols for TG testing are not standardized. There is no consensus guideline to instruct homogeneous examinations in research settings, although from publication to publication, there is similarity in testing instructions. The protocols used are variations on those described in classic manuscripts on TG in patients with vestibular disorders [16, 24].
Fregly et al. [24] described a battery of tests for patients with various vestibular disorders, including protocols for tandem gait testing that they call “walk eyes open” (Walk E/O) and “walk on floor eyes closed” (WOFEC). The complete battery included the “sharpened Romberg” (standing in tandem heel-to-toe position on the floor with eyes closed, arms folded against chest, and body erect for 60 s), standing with eyes opened and closed, and standing on each leg with eyes closed. The authors note that all tests were performed on hard floors (no carpets) with patients wearing shoes and patients were instructed to walk at a “normal” pace. They described Walk E/O as follows: “walking heel-to-toe with feet in strictly tandem position and arms folded against chest while in a body-erect position on a ¾-inchwide by 8-foot-long rail.” The original manuscript has a figure depicting a patient walking the rail in a narrowed spaced between two barricades. The WOFEC test was described as follows: “walking on the floor eyes closed in the stringent position of arms folded against chest, body erect, and feet aligned tandemly heel-to-toe.” Graphical examples of correct and incorrect tandem steps (including the heel of the leading foot not making contact with the toes of the trailing foot) are also depicted in the original manuscript. In a WOFEC test trial, a patient was asked to take a maximum of ten heel-to-toe steps (if they could complete the task) without sidestepping. In a given trial, the number of steps properly taken before making an error was the trial score. Errors included the following: sidestepping, stopping, opening the eyes, or unfolding the arms. The scores obtained on the best three of five trials were totaled and assigned as the test score; 30 being the maximum score obtainable by completing three perfect (ten completed steps) trials.
Variations of the TG testing protocols described are used in research. Protocols differ in the number of steps required per trial (8 [14] or 10 [24]?), number of trials allowed (3 [25] or 5[24]?), the use of a real or imaginary line, explicit instructions regarding arm position and body posture, testing with eyes opened and/or closed, and in terms of scoring systems used to determine normal versus abnormal. Testing with both eyes opened and closed is likely more important when examining patients with peripheral neuropathy or vestibular disorders compared to neurodegenerative processes. In fact, eyes-closed testing is more sensitive in detecting peripheral neuropathies [16] and vestibulopathies [24]. Testing with eyes closed is not described in any of the studies including TG testing in cerebellar disease, PD, or AP that we have come across.
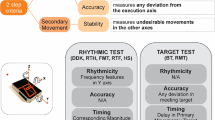
Technology can be employed for a more quantitative assessment of the physiological parameters of TG. These parameters include the following: gait velocity, cadence, and step length as well as measures of dynamic balance (percent time of gait cycle in single or double limb support, tandem missteps), gait symmetry (step time difference), and gait variability (variation in stride length and swing time). One such system is called the GAITRite (CIR Systems, Haverton, PA, USA)—a 4.6-m-long computerized mat that can measure and record the above parameters. The GAITRite was utilized by Rao et al. [26], Earhart et al. [27], and Kronenbuerger et al. [28] for quantitative gait analysis in patients with essential tremor (ET).
Tandem gait: essential tremor and the cerebellum
Underlying pathology in the cerebellum or its pathways likely plays a role in ET. Clinical evidence for this association includes the presence of intention and kinetic tremors in both patients with ET and those with other classic cerebellar disorders [29]. Functional and metabolic imaging studies suggest cerebellar involvement in ET [29]. And there are pathological studies strongly suggesting the relationship [30, 31].
Abnormal tandem gait can be detected in up to 50% of patients with ET [5, 6]. In Singer et al. [5], patients were graded to have a normal or abnormal TG based on the occurrence of two or more “out-of-line” steps out of ten successive tandem steps. Findings had to be reproduced twice before the gait was labeled as abnormal. Stolze et al. [6] utilized a three-dimensional opto-electronic movement analysis system to quantify gait characteristics. Patients were asked to walk 13 m on the floor in tandem and to walk on a treadmill in tandem for 60 s. They were given 5 min to familiarize themselves with the treadmill. A redline of tape was placed on the floor and on the treadmill to guide the steps. Arms were folded across the neck. In the case of ET, tandem gait difficulty has been associated with cranial tremors suggesting both may share an underlying pathophysiology as a midline cerebellar disturbance [32]. Worsening TG performance has also been associated with worse cognitive performance in patients with ET [33]. Detecting a TG abnormality in a patient with ET may imply more than a midline cerebellar dysfunction.
Tandem gait: beyond the cerebellum
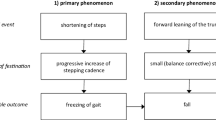
Abnormal TG is seen in conditions that extend beyond cerebellar dysfunction, including Parkinson’s disease and atypical parkinsonism, Huntington disease, peripheral neuropathies, and vestibulopathies. Abnormal TG in PD and AP (and probably in HD) suggests mediolateral balance impairment, which is seen earlier in AP compared to PD, and is attributed to extranigral lesions. Pathology may involve the cerebellum, cerebellar pathways, brain stem nuclei, and/or subcortical white matter often with associated MRI abnormalities [12, 13, 34]. Peripheral pathology, as in neuropathy or vestibulopathy, also confers an abnormal tandem gait exam. A normal gait, including capacity to walk in tandem, involves multiple systems (both neurologic and musculoskeletal) functioning normally and in concert (summarized in the following paragraph).
Optimal gait, in individuals with healthy nervous systems, requires the integration of the peripheral nervous system (including proprioceptive afferent and motor efferent fibers), spinal cord locomotion generators and tracts conveying central and peripheral information, and brainstem, cerebellar, subcortical, and cortical activities as well as a competent musculoskeletal system [35]. The basic pattern of locomotion is generated by central pattern generators, which in humans are dispersed over several spinal segments [36, 37]. This spinal cord network receives signals from descending pathways originating in several brainstem networks. Excitatory signals are sent the pattern generators by the medullary reticular formation, median raphe and parapyramidal serotonergic neurons, locus coeruleus noradrenergic neurons, and lateral hypothalamic dopaminergic neurons [34, 35]. The mesencephalic locomotor region (MLR), basal ganglia, and frontal cortical regions are also involved in the supraspinal control of these pattern generators. The MLR includes the pedunculopontine nucleus (PPN) pars compacta and pars dissipata, the cuneiform nucleus, and the subcuneiform nucleus. The PPN connects with the pontomedullary reticular formations caudally and with the basal ganglia and thalamus rostrally [36, 37]. Brainstem motor programs receive tonic suppression signals from the basal ganglia and excitatory stimulation by direct cortical input [36, 37]. The activation of a particular motor program follows the integration of cognitive, sensory, and limbic cortical inputs to the striatum and subsequent disinhibition of the appropriate brainstem system. The frontal cortex, including the supplementary motor area (SMA), is important in locomotion. While a decerebrate cat can walk on a treadmill, it can only walk in a stereotyped pattern unable to adapt its gait to the environment [36].
Lindholm et al. [11] offer a model to predict fall risk in PD combining TG assessment with retropulsion testing and a history of falls or near falls. This model was tested against a previously described fall prediction tool, the “3-step model,” which includes history of falls, history of freezing of gait, and a comfortable gait speed of 1.1 m/s. The two models were found to be comparable. To assess TG participants, they were instructed to take ten consecutive heel-to-toe steps along a straight line without walking aids or support and with eyes open. A score of 0–3 was given: 0 (no side steps), 1 (1 side step), 2 (multiple side steps), 3 (unable to take four consecutive steps). A score of 1 or more was deemed an abnormal TG performance. The same protocol and scoring system were utilized in other studies [13, 38, 39].
TG is not included in diagnostic criteria for PD or AP nor is it part of the UPDRS. Early medio-lateral balance involvement is considered a “red flag” for AP reflecting more widespread pathology [34, 38]. Detecting TG abnormalities is a useful clinical corollary for medio-lateral balance impairment. Abdo et al. [13], Nonnekes et al. [34], and Aerts et al. [12] reported the utility in detecting TG abnormality to help discriminate AP from PD. Abdo et al. [13] utilized the same testing protocol and scoring system as described above in Lindholm et al. [11]. Nonnekes et al. [34] offer more detailed instructions. Patients were asked to take ten consecutive steps along an imaginary straight, thin line. With each step, the heel of the leading foot should make contact with the toes of the trailing foot. An abnormal TG was scored if one or more side steps are taken. A practice trial was allowed, and a normal second trial was considered a normal TG exam. They suggest the examiner try to alleviate patient trepidation to avoid an overly cautious performance that could precipitate side steps. Aerts et al. [12] do not describe their protocol for assessing TG. Abnormal MRI findings, including those suggestive for multiple systems atrophy, progressive supranuclear palsy, and vascular parkinsonism, were more likely to be found in patients with parkinsonism and abnormal TG exams [12, 13].
An underlying peripheral neuropathy may cause an abnormal TG exam. In a study by Maksimovic et al. [14], patients with diabetes or impaired fasting glucose had more missteps in eight tandem steps using a visible line on the floor than healthy controls. As noted by the authors, the abnormal TG exam in this cohort is likely multifactorial including more diffuse microvascular disease and possible visual impairment in addition to peripheral neuropathy. A case has been reported of a patient with idiopathic PD who developed distal acquired demyelinating symmetric (DADS) neuropathy while using anti-TNF-alpha therapy [15]. His neuropathy manifested with abnormal TG, hypoesthesia, areflexia, and abnormal EMG. TG, sensory, and reflex exams normalized with discontinuation of the culprit medication. Cohen et al. [16] studied TG as a screening tool for peripheral neuropathy. It was found to be a sensitive test (made more sensitive when TG testing was performed with eyes closed). In this study, two trials were allowed: one with eyes open and the second with eyes closed. They recorded the maximum number of correctly performed tandem steps out of ten attempted steps. Side steps, making a space between the feet, and opening the eyes were considered errors. A quiet room with industrial carpeting was used for examinations.
Tandem gait: limitations
Tandem gait testing has been used in the assessment of patients with vestibular disorders for at least 5 decades [17, 24]. However, its utility as a screening test has been called into question by Cohen et al. [17]. The authors cited prior reports of less than 30% of normal participants being capable of performing five tandem steps with their eyes closed and of the decline of performance with age. They investigated if TG testing could distinguish patients with vestibulopathies from normal controls. They asked patients to walk for ten steps, heel-to-toe, without spaces between steps with eyes open followed by with eyes closed. The maximum number of correct, consecutive steps was recorded. Side steps, making a space between the feet, and opening the eyes were considered errors. All participants took significantly more consecutive steps with their eyes open than with eyes closed. Patients had a worse performance than controls in TG testing, but the magnitude of difference was not enough for the authors to consider TG testing a useful screening tool for vestibulopathy. Similar extrapolations were made from the results of Longridge and Mallinson [40] in patients with unilateral vestibulopathy compared to controls and of Kammerlind et al. [41] in patients with subjective dizziness and disequilibrium compared to controls.
It has been reported that performance of TG declines with age; thus, the age of the patient must be considered in grading a TG abnormality [17, 42,43,44]. With age comes increased risk of falls and gait abnormalities [45]. This increased risk is multifactorial including chronic diseases and disabilities that impair sensory (visual, vestibular, and proprioceptive), cognitive, neurologic, or musculoskeletal function [45]. In a manuscript by Fregly et al. [42], this decline in performance was noted to begin around age 45. They tested men with one trial of tandem walking on a 1.9-cm-wide beam with eyes open and one trial on a 5.7-cm-wide beam with eyes closed. Speers et al. [43] compared TG and tandem stance in healthy women of two age groups: mean 23.3 and mean 72 years of age. Tandem walk tasks were conducted with eyes open and along set of beams ranging in size from 15 cm down to 2.5 cm in width. Five trials were allowed per beam width. All of the younger women could complete the task on the widest beam while only 62% of the older woman could complete the same task.
It is interesting to note that younger children may have a poorer TG performance (in terms of speed) than older children. In establishing normative data for balance to be used in the Children Sport Concussion Assessment Tool, Brooks et al. [46] found children ages 5 to 7 years had more balance error in tandem stance and slower TG times than children ages 8 to 13 years. Participants in the study were asked to walk heel-to-toe along a 3-m line on both a stable and unstable surface. Age was noted to have a larger effect on tandem gait than tandem stance. Brooks et al. did not discuss the accuracy of steps in TG assessment in the manuscript. Gender did not play a role in TG performance in the studied age range. Nor did it in a similar study to obtain normative data in college-aged participants [47].
Tandem gait: strolling towards consensus
Though TG testing is a standard part of the neurological exam and has wide—and sometimes questioned—clinical utility, there is inconsistency, both in the clinic and in the literature, in the performance and interpretation of the exam. Guidance for proper and consistent testing can be found in neurology text books, in the descriptions included in widely utilized rating scales, and in the method sections of select publications. Again, explicit guidelines have not been published. Blumenfeld [48], in his discussion on TG testing, states a patient should be asked “to walk in a straight line while touching the heel of one foot to the toe of the other with each step.” The SARA [21] and UHDRS [22] are consistent in terms of suggesting that ten steps in tandem be attempted and evaluated. The corollary that TG should be attempted “without support” is additionally noted in the SARA scale. In many trials, patients are asked to take ten steps in a straight line, with eyes open, without support, with or without an actual line on the floor to mimic a “tight rope,” and are instructed with each step the heel of the leading foot should make contact with the toes of the trailing foot. If the first trial is abnormal, a second trial is often allowed. When testing TG in a patient with suspected peripheral neuropathy or vestibulopathy (as opposed to patients with suspected cerebellar disease or more diffuse pathology), a trial with eyes closed could be included to improve sensitivity. All patients should be asked to walk at a “normal” pace as walking to fast or slow may confound the exam.
The details of TG testing have not been formally studied and no formal guideline-based protocol exists. For example, the effect of using a real or imaginary line (or an actual beam or rod) to walk along is unknown. The number of trials allowed may affect results [49]. Dozza et al. [49], using different quantitative analyses, report improved performance in TG testing after practice trials. A standard means of grading TG testing is lacking. Some studies report a dichotomous normal or abnormal result defined by individual authors. Others report a graded scale, as in the SARA or UHDRS. The clinical importance of having a graded versus dichotomous result is unknown.
Conclusion
Tandem gait has emerged as a tool in the assessment of cerebellar disease, Huntington disease, idiopathic Parkinson’s disease, atypical parkinsonism, peripheral neuropathies, and vestibulopathies. Its origin can be deduced from experimental observation and clinical experience as far back as the early nineteenth century. The term “tandem gait” is only found in twentieth century literature. Lesions of the cerebellar vermis as well as the vestibulocerebellar module (flocculonodular lobe and lobule IX of the vermis—the paraflocculus) can impart an indistinguishable gait abnormality. It is now well-accepted that testing of tandem gait is a sensitive measure of cerebellar gait ataxia even in its mildest form and is a relevant exam finding in essential tremor and in HD.
Despite the long history and ubiquitous performance of TG testing, there is no standardized, guideline-based protocol to model for more homogenous research and clinical practices. Such a protocol should be developed using historical texts and manuscripts as well as the consensus of the medical-research community. Protocols may need to differ depending on the patient’s underlying pathology. Interpretation of TG testing should consider age-related factors. With standard protocols, further studies could define the sensitivity of abnormal TG testing in cerebellar disorders, more diffuse neurodegeneration, and in peripheral pathologies. TG can be a useful marker of dysfunction in neurologic conditions whose pathologies extend beyond the vermis or vestibulocerebellar module to include interconnected networks throughout the nervous system.
References
Daroff R, Fenichel G, Jankovic J, Mazziotta J (2012) Bradley’s neurology in clinical Practice. Elsevier Inc., Philadelphia, p 6e
Ropper AH, Samuels MA, Klein JP (2014) Chapter 7. Disorders of stance and sait. In: Ropper AH, Samuels MA, Klein JP (eds) Adams & Victor’s principles of neurology. McGraw-Hill, New York, p 10e
Campbell W (2005) Chapter 44. DeJong’s the neurologic examination. Lippincott Williams & Wilkins, Philadelphia, p 6e
Walter H (1990) Ch 69 The Cerebellum. In: Clinical Methods: The history, physical, and laboratory examinations, 3rd edn. Butterworths, Boston
Singer C, Sanchez-Ramos J, Weiner W (1994) Gait abnormality in essential tremor. Mov Disord 9:193–196
Stolze H, Petersen G, Raethjen J, Wenzelburger R, Deuschl G (2001) The gait disorder of advanced essential tremor. Brain 124:2278–2286
Fine E, Ionita C, Lohr L (2002) The history of the development of the cerebellar examination. Semin Neurol 22(4):375-84
Bastian A, Thach W (1995) Cerebellar outflow lesions: a comparison of movement deficits resulting from lesions at the levels of the cerebellum and thalamus. Ann Neurol 38:881–892
Haines DE, Mihailoff GA, Bloedel JR (2002) The cerebellum. In: Haines DE (ed) Fundamental neuroscience, 2nd edn. Churchill Livingstone, New York, pp 424–443
Pryse-Phillips W, Murray T (1992) Essential neurology: a concise textbook. Elsevier, New York
Lindholm B, Nilsson M, Hansson O (2016) External validation of a 3-step falls prediction model in mild Parkinson’s disease. J Neurol 263(12):2462–2469
Aerts M, Esselink R, Abdo W (2016) Ancillary investigations to diagnose parkinsonism: a prospective clinical study. J Neurol 262:346–356
Abdo WF, Borm GF, Munneke M, Verbeek MM, Esselink RA, Bloem BR (2006) Ten steps to identify atypical parkinsonism. J Neurol Neurosurg Psychiatry 77:1367–1369
Maksimovic A, Hanewinckel R, Verlinden V et al (2016) Gait characteristics in older adults with diabetes and impaired fasting glucose: the Rotterdam study. J Diabetes Complicat 30:61–66
McGinty R, McNamara B, Moore H (2015 Nov) DADS neuropathy associated with anti-TNF- α therapy. BMJ Case Rep 25:2015. https://doi.org/10.1136/bcr-2015-211781
Cohen H, Mulavara A, Peters B et al (2013) Sharpening the tandem walking test for screening peripheral neuropathy. South Med J 106:565–569
Cohen H, Mulavara A, Peters B et al (2012) Tests of walking balance for screening vestibular disorders. J Vestib Res 22:95–104
Gowers WR (1888) A manual of diseases of the nervous system. American ed. P. Blakiston, Philadelphia, pp 717–718
Bastian AJ, Mink JW, Kaufman BA, Thach WT (1998) Posterior vermal split syndrome. Ann Neurol 44(4):601–610
Christopher F, Saladin LK (1996) Ch. 9 Disorders of the cerebellum and its connections. In: Pathophysiology of the motor systems: principles and clinical presentations. 1st Ed. F. A. Davis Company
Marquer A, Barbieri G, Perennou D (2014) The assessment and treatment of postural disorders in cerebellar ataxia: a systematic review. Ann Phys Rehabil Med 57:67–78
Huntington Study Group (1996) Unified Huntington’s disease rating scale: reliability and consistency. Mov Disord 11:136–142
Oster E, Eberly S, Dorsey E, Kayson-Rubin E, Oakes D, Shoulson I (2015) Informativeness of early Huntington disease signs about gene status. J Huntingtons Dis 4(3):271–277
Fregly AR, Graybiel A, Smith MJ (1972) Walk on floor eyes closed (WOFEC): a new addition to an ataxia test battery. Aerosp Med 43(4):395–399
Lim E, Seo M, Woo S et al (2005) Relationship between essential tremor and cerebellar dysfunction according to age. J Clin Neurol 1(1):76–80
Rao AK, Gillman A, Louis ED (2011) Quantitative gait analysis in essential tremor reveals impairments that are mainained into advanced age. Gait Posture 34:65–70
Earhart GM, Clark BR, Tabbal SD, Perlmutter JS (2009) Gait and balance in essential tremor: variable effects of bilateral thalamic stimulation. Mov Disord 24(3):386–391
Kronenbuerger M, Konczak J, Ziegler W, Buderath P, Frank B, Coenen VA et al (2009) Balance and motor speech impairment in essential tremor. Cerebellum (Lon- don England) 8(3):389–398
Jankovic J (2002) Essential tremor: a heterogeneous disorder. Mov Disord 17:638–644
Louis et al (2007) Neuropathological changes in essential tremor. Brain 130:3297–3307
Erickson-Davis et al (2010) “Hairy baskets” associated with degenerative purkinje cell changes in essential tremor. J Neuropathol Exp Neurol 69:262–271
Louis E, Rios E, Rao A (2010) Tandem gait performance in essential tremor: clinical correlates and association with midline tremor. Mov Disord 25(11):1633–1638
Louis E, Rao A (2014) Tandem gait performance in essential tremor patients correlates with cognitive function. Cerebellum Ataxias 1:19
Nonnekes J, Aerts M, Abdo W (2014) Medio-lateral balance impairment differentiates between Parkinson’s disease and atypical parkinsonism. J Park Dis 4:567–569
Jankovic J (2015) Gait Disorders. Neurol Clin 33:249–268
Nutt JG, Bastiaan BR, Nir G, Hallet M, Horak FB, Nieuwboer A (2011) Freezing of gait: moving forward on a mysterious clinical phenomenon. Lancet Neurol 10:734–744
Snijders AH, Takakusaki K, Debu B, Lozano AM, Krishna V, Fasano A, Aziz TZ, Papa SM, Factor SA, Hallet M (2016) Physiology of freezing of gait. Ann Neurol 80:644–659
Bloem B, Grimbergen Y, Cramer M et al (2001) Prospective assessment of falls in Parkinson’s disease. J Neurol 248(11):950–958
Dennison A, Noorigian J, Robinson K et al (2007) Falling in Parkinson disease: identifying and prioritizing risk factors in recurrent fallers. Am J Phys Med Rehabil 86(8):621–632
Longridge N, Mallinson A (2010 Jul) Clinical Romberg testing does not detect vestibular disease. Otol Neurotol 31(5):803–806
Kammerlind A, Larsson P, Ledin T et al (2005) Reliability of clinical balance tests and subjective ratings in dizziness and disequilibirum. Adv Physiother 7:96–107
Fregly A, Smith M, Graybiel A (1973 Jan) Revised normative standards of performance of men on a quantitative ataxia test battery. Acta Otolaryngol 75(1):10–16
Speers R, Ashton-Miller J, Schultz A et al (1998) Age differences in abilities to perform tandem stand and walk tasks of graded difficulty. Gait Posture 7(3):207–213
Vereeck L, Wuyts F, Truijen S et al (2008) Clinical assessment of balance: normative data, and gender and age effects. Int J Audiol 47(2):67–75
Tinetti M, Speechley M (1989) Prevention of falls among the elderly. NEJM 320:1055–1059
Brooks AM, Snedden TR, Mixis B, Hetzel S, McGuine TA (2017) Establishing baseline normative values for the children sport concussison assessment tool. JAMA Pediatr 171(7):670–677
Oldman JR, DiFabio MS, Kaminski TW, DeWolf RM, Buckley TA (2016) Normative tandem gait in collegiate student-athletes: implications for clinical concussion assessment. Sports Health 9(4):305–311
Blumenfeld H (2002) Neuroanatomy through clinical cases. Sinauer Associates Inc., Sunderland
Dozza M, Wall C, Peterka R et al (2007) Effects of practicing tandem gait with and without vibrotactile biofeedback in subjects with unilateral vestibular loss. J Vestib Res 17(4):195–204
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Margolesky, J., Singer, C. How tandem gait stumbled into the neurological exam: a review. Neurol Sci 39, 23–29 (2018). https://doi.org/10.1007/s10072-017-3108-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-017-3108-1