Abstract
Simultaneous performance of motor and cognitive tasks may compete for common brain network resources in aging or patients with some neurological diseases, suggesting the occurrence of a cognitive-motor interference. While this phenomenon has been well described for multiple sclerosis (MS) patients, it never has been tested on asymptomatic subject with magnetic resonance imaging (MRI) findings suggestive of demyelinating disease (i.e., radiologically isolated syndrome: RIS). In this pilot study, 10 RIS subjects and 10 sex/age-matched healthy controls were tested by means of static posturography under eyes opened (single-task trial) and while performing two different cognitive tasks (semantic modified word list generation for first dual-task trial and phonemic semantic modified word list generation for second dual-task trial), to estimate the dual-task cost (DTC) of standing balance. In our sample, under cognitive interference (without any substantial differences between semantic and phonemic modified word list generation), the RIS group showed significance differences in CoP (center of pressure) total sway area, ellipse eccentricity, CoP sway path length, CoP median sway velocity along the AP (anteroposterior) axis and along the ML (mediolateral) axis, reflecting a higher negative DTC respect to healthy subjects (which have simply shown a statistical trend, failing to reach a significance, in some trials). The phenomenon of cognitive-motor interference might be unmasked by a dual-task posturography in RIS subjects, too. We hypothesize that this approach could be useful to early reveal the presence of a demyelinating disease and to reach a MS diagnosis in subjects otherwise classified as RIS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A variety of unexpected and abnormal findings in brain white matter are occasionally discovered during magnetic resonance imaging (MRI), usually in the setting of an investigation for some other reasons [1]. MRI findings suggestive of demyelinating disease in subjects without typical multiple sclerosis (MS) symptoms and with normal neurological findings are defined as radiologically isolated syndrome (RIS) [2]. Approximately two-thirds of persons with RIS show radiological progression and one-third develop neurological symptoms at 5-years follow-up [3]. Spinal cord lesions and the presence of oligoclonal bands in cerebrospinal fluid are important predictors of the clinical conversion [3, 4]. Thus, RIS could be considered a mild symptomatic MS, whose diagnosis failure depends on the low sensitivity of neurological evaluation. RIS patients’ management depends on the clinical signs and, therefore, introduction into clinical practice of tools and strategies that can reveal mild neurological deficits can be extremely useful and decisive to reach a definite diagnosis of MS.
Common MS symptoms are motor dysfunctions (such as deficits in gait and balance), as well as cognitive impairment (such as reductions in cognitive processing speed). Specifically, balance dysfunction is commonly reported (85%) by individuals with MS even in the absence of clinical disability [5]. Additionally, an estimated 65% of with MS report cognitive deficits [6] which can occur early in the disease course [7].
A cognitive impairment of the same profile as that of MS patients (associated with high T1 lesion volume and low cortical volume) was also found in subjects with RIS [8] and it would seem to have a prevalence similar to that of clinically isolated syndromes (CIS) [9]. Nonetheless, the predictive value of cognitive impairment in RIS subject is controver-sial. Indeed, it does not seem to be significantly associated to the risk of conversion to relapsing-remitting (RR) MS, a result in contrast to what is reported in CIS patients [9].
Therefore, as suggested by previous studies, cognitive tests should be used to identify neurological impairment in RIS patients, but, probably, they are not a sensitive tool to predicting the RIS conversion to a RRMS. For this reason, we believe that the simultaneous assessment of a motor and cognitive deficit may have a higher diagnostic and predictive value.
Motor and cognitive impairments are commonly examined independently of each other, although growing evidence demonstrates a strict connection between motor and cognitive performance [10, 11]. Dual-task costs (DTC) represent an operationalization of cognitive-motor interaction (CMI) and are often calculated by computing the percentage change in outcome measures from performance in isolation to dual-tasking performance [12].
We hypothesize that a dual-task approach could be useful in early revealing of the presence of undetected clinical signs (even in subjects without cognitive deficits), so to reach a MS diagnosis in subjects otherwise classified as RIS.
Methods
Population
A total of 10 RIS subjects (seven women and three men; mean age 33.8 years, range 24–42 years) were recruited from two MS centers in Messina (Italy). These subjects had came to our attention after undergoing conventional brain 1.5 T MRI (performed a mean of 3.0 years earlier) for various medical conditions not suggestive of MS, i.e., headache (N = 7), traffic accident (N = 2), and research control (N = 1).
Brain white matter abnormalities were initially identified by a neuroradiologist and subsequently examined by an MS specialist at each clinical site to guarantee they fulfilled the Okuda criteria for RIS [13], which imply (1) the presence of white matter abnormalities suggestive of a demyelinating process (ovoid, well-circumscribed and measuring > 3 mm2) that satisfied Barkhof criteria (at least three of four criteria) for dissemination in space; (2) not better accounted for by other disease processes, such as vascular disease; and (3) no apparent impact on everyday functioning [14, 15].
After the initial MRI imaging, all subjects underwent a spinal cord MRI (demyelinating lesions were found in four subjects), but only five subjects agreed to undergo lumbar puncture for cerebrospinal analysis (oligoclonal bands were found in three samples). A neurologic examination and an accurate clinical history were performed by an expert neurologist to rule out MS. In addition, our subjects underwent a complete diagnostic work-up to rule out other medical conditions that could explain the white matter lesions (such as auto-antibody testing, coagulation parameters, serum homocysteine level and a cardiovascular screening).
A control group consisting of 10 healthy volunteers (five women and five men; mean age 35 years, range 29–41 years, friends or relatives of RIS subject) with no history of known psychiatric or neurological disorders, entered the study.
Study design and procedure
The present study was conducted in accordance with the Declaration of Helsinki. All procedures were approved by the ethics committee and written informed consent was obtained from all enrollees.
MRI was performed the same day the RIS subject and healthy volunteers underwent the balance study. All RIS subject MRIs were unchanged, while healthy volunteers did not show any brain abnormalities. A neuropsychological test battery (including the auditory verbal learning test, the STROOP test, and the verbal fluency test [16]) was conducted in a single session, 2 weeks before MRI and balance study, by experienced clinical neuropsychologists, who were blinded to the subjects’ status.
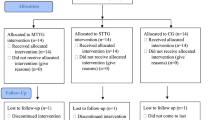
Each participant was tested by means of static postu-rography under single-task and dual-task conditions, using the same laboratory-grade force platform (MultiSensor Slim, Diasu Health Technologies®) according to standardized procedures [17]. The balance study was performed by an experienced physiatrist (A.L. L.), who was blinded to the MRI status. Three consecutive balance trials, each lasting 50 s and separated by 60 s of rest, were acquired. For the first trial, participants stood on a laboratory-grade force platform with eyes open, feet shoulder width apart and arms by their sides (single-task trial: STT). For the second (dual-task trial-1: DTT-1) and third trials (dual-task trial-2: DTT-2), participants stood in the same position with their eyes open and performed a concurrent cognitive test. According to some previous MS dual-task trials, the cognitive test we used was a semantic (e.g., listing animals) modified word list generation (se-WLG) for DTT-1, and phonemic (e.g., listing ‘A’ words) modified word list generation (ph-WLG) for DTT-2 [12, 18].
Outcome measures
Changes in postural control were determined by examining center of pressure (CoP) variation. CoP can be defined as the position of the global ground reaction force vector that accommodates the sway of the body. In simple terms, it is the point at which the pressure of the body over the soles of the feet would be if it was concentrated in one spot [17].
Overall, CoP total sway area (i.e., the area of the ellipse that encloses 95% of postural sway), ellipse eccentricity (i.e., the percentage ratio between the two semi axes of the ellipse: minor axis/major axis × 100), CoP sway path length (i.e., the sum of displacements on the force-measuring platform) and CoP median sway velocity along the anteroposterior (AP) and mediolateral (ML) axis were calculated and averaged over similar trials for each participant [17].
To quantify CoP variations, data were exported from the balance platform and processed using a dedicate software (Millimetrix®).
According to literature data, DTC was determined by calculating the percentage change from single-task to dual-task conditions, (single-task − dual-task) / single-task × 100, and a negative DTC represents an increase in sway from single to dual-task conditions [12].
Statistical analysis
Descriptive analysis was performed for two groups: RIS subjects and healthy volunteers. Normal data distribution was evaluated using the Shapiro-Wilk normality test. In the intra-group analysis, we compared the parameters between SST (balance), DTT-1 (balance + semantic modified word list generation) and DTT-2 (balance + phonemic modified word list generation) in RIS subjects and control group by paired Student t test. For the inter-group analysis, Student t test for unpaired samples or Mann–Whitney U test, where appropriated, were applied to compare the parameters in all times. Analyses were performed using an open source R3.0 software package. A 95% of confidence level was set with a 5% alpha error. Statistical significance was set at p < 0.05.
Results
Intra-group analysis
No cognitive deficits were found in both RIS and healthy subjects (detailed results for all tests are reported in Table 1, together with normative benchmarks).
In RIS group, we found a statistically significant difference between the different trials (p < 0.001), except between DTT-1 and DTT-2 for CoP median sway velocity along the mediolateral axis (p = 0.46). In the control group, we did not find any significant difference between the trials (p = 0.06), except between SST and DTT-1 in CoP total sway area (p = 0.09), between DTT-1 and DTT-2 in ellipse eccentricity (p = 0.94), CoP median sway velocity along the AP axis (p = 0.25) and CoP median sway velocity along the ML axis (p = 0.16).
Inter-group analysis
No significant differences were found about age, cognitive test score, and postural parameters at SST. In DTT-1, we found a statistically significant difference between the different trials in CoP total sway area (p < 0.001), ellipse eccentricity (p < 0.001), CoP sway path length (p < 0.001), CoP median sway velocity along the AP axis (p < 0.001), and CoP median sway velocity along the ML axis (p < 0.001). In the same way, in DTT-2, we found a significant difference in CoP total sway area (p < 0.001), ellipse eccentricity (p < 0.001), CoP sway path length (p < 0.001), CoP median sway velocity along the AP axis (p = 0.001) and CoP median sway velocity along the ML axis (p < 0.001). Table 2 shows the inter-group analysis.
DTC analysis showed a statistically significant difference in almost all parameters between RIS subjects and healthy volunteers, as reported in Table 3.
In particular, we found a significant difference in CoP total sway area DTC between SST and DTT-1 (p = 0.0005) and SST vs DTT-2 (p = 0.0007), in CoP sway path length DTC between SST and DTT-1 (p = 0.002) and SST vs DTT-2 (p = 0.001), in CoP median sway velocity along the AP axis DTC between SST and DTT-1 (p = 0.0003) and SST vs DTT-2 (p = 0.0003), in CoP median sway velocity along the ML axis DTC between SST and DTT-1 (p < 0.001) and SST vs DTT-2 (p < 0.001). For ellipse eccentricity DTC a statistical trend between SST and DTT-1 (p = 0.06), but no significant difference between SST and DTT-2 (p = 0.14), were found.
Discussion
To the best of our knowledge, this is the first balance study using a dual-task approach in RIS subjects.
No cognitive deficits were found in our RIS subjects, a data in contrast to what was previously reported by other authors [8, 9, 19], probably due to small sample size or to the early stage of disease.
In our sample, the RIS group showed a statistically significant difference in CoP total sway area, ellipse eccentricity, CoP sway path length, CoP median sway velocity along the AP axis and along the ML axis, reflecting a more negative DTC than healthy subjects (which have simply shown a statistical trend, failing to reach the significance, in some trials). Figure 1 provides an example of some CoP parameters variation in a RIS subject during the three trials.
Commonly, cognitive-motor interferences are quantified as DTC by calculating the percentage change in outcome measures from single-task performance to dual-task performance [12].
Our results are in line with previous findings on MS patients, in which the use of dual-task paradigm to study postural stability is an emerging area of interest [20, 21]. In these patients, in fact, there is growing evidence that cognition may play an important role in balance deficit, traditionally attributed to neurological impairments of the locomotor system [21, 22]. Indeed, various authors demonstrated that two simultaneously performed tasks compete for the brain network resources which are critical for controlling postural stability, thus constraining even the less disabled MS patients to employ their own postural reserve in the more challenging dual-task condition [22, 23]. Postural stability, required for preserving steadiness during static and dynamic activities, is mediated by both higher “controlled” and lower “automatic” levels of processing, implying the involvement of proprioceptive afferents, sensorimotor integration and basal ganglia–cortical loops [21]. Some studies have suggested that, also in aging and in other neurological diseases (i.e., stroke, dementia, and Parkinson disease), balance can be negatively affected by the addition of a concurrent cognitive task (i.e., dual-task) [22, 24, 25]. These alterations in postural control, while subjects are engaged in a cognitive task, are indicative of cognitive-motor interference [22].
In our RIS sample, we found a significantly more neg-ative DTC in comparison to healthy subjects, due to an increase in sway from single to dual-task conditions, probably related to the brain damage [26]. About that, a recent conventional and functional MRI study, investigating the relationship between disease-altered structure/function and cognitive-postural interference phenomenon in MS patients, has raised the hypothesis that MS-related damage might have disconnected brain circuitry at two distinct levels: (a) between cerebellum, striatum, and pre-frontal areas, connected through the anterior and superior corona radiata; (b) between frontal lobes and anterior/midline nuclear groups of thalami, connected through the anterior thalamic peduncles [27]. These disconnections might have, in turn, impaired the integration of brain networks required to maintain adequate performance in dual-task situations [27].
In line with these findings, a recent MRI study showed a similar brain damage (i.e., thalamic volume loss and lower cortical volume, with thinning in some frontal and temporal cortical areas) in RIS patients compared to healthy controls [28].
It is possible that in RIS subjects, these brain network disconnections could be balanced by functional reorganization in key brain networks (due to a relatively milder microstructural damage of different withe matter tracts in comparison to MS patients) [29] and be clinically evident only when subjects are submitted to more demanding performances.
The evidence of how the dual-task paradigm affects balance parameters in RIS subjects, as well as in MS patients, may indicate that these two conditions could be a different expression of a single nosologic entity.
Conclusion
For the first time, our study demonstrated that subjects with an apparently asymptomatic demyelinating event had a greater decrement in postural stability (though triggered by a cognitive task interference) than the general population, suggesting that postural control consumes attentional resources even in the RIS condition.
This evidence supports the hypothesis that RIS could be considered not a preclinical condition, but a mild onset of MS.
A motor-cognitive dual-task paradigm may be a promising tool in predicting the RIS clinical progression so to better manage these “apparently” asymptomatic patients.
However, ours can be considered a pilot study and further efforts, based on a longitudinal study design with an adequate sample size (i.e., multicenter trials), are now required to confirm these preliminary results and to define their predictive power.
References
Katzman GL, Dagher AP, Patronas NJ (1999) Incidental findings on brain magnetic resonance imaging from 1000 asymptomatic volunteers. JAMA 282(1):36–39
Forslin Y, Granberg T, Jumah AA, Shams S, Aspelin P, Kristoffersen-Wiberg M, Martola J, Fredrikson S (2016) Incidence of radiologically isolated syndrome: a population-based study. AJNR Am J Neuroradiol 37(6):1017–1022. doi:10.3174/ajnr.A4660
Okuda DT, Siva A, Kantarci O, Inglese M, Katz I, Tutuncu M, Keegan BM, Donlon S, le Hua H, Vidal-Jordana A, Montalban X, Rovira A, Tintoré M, Amato MP, Brochet B, de Seze J, Brassat D, Vermersch P, De Stefano N, Sormani MP, Pelletier D, Lebrun C (2014) Radiologically Isolated Syndrome Consortium (RISC).; Club Francophone de la Sclérose en Plaques (CFSEP). Radiologically isolated syndrome: 5-year risk for an initial clinical event. PLoS One 9(3):e90509. doi:10.1371/journal.pone.0090509
Lebrun C, Cohen M, Chaussenot A, Mondot L, Chanalet S (2014) A prospective study of patients with brain MRI showing incidental t2 hyperintensities addressed as multiple sclerosis: a lot of work to do before treating. Neurol Ther 3(2):123–132. doi:10.1007/s40120-014-0024-7
Morrison S, Rynders CA, Sosnoff JJ (2016) Deficits in medio-lateral balance control and the implications for falls in individuals with multiple sclerosis. Gait Posture 49:148–154. doi:10.1016/j.gaitpost.2016.06.036
Amato MP, Zipoli V, Portaccio E (2008) Cognitive changes in multiple sclerosis. Expert Rev Neurother 8(10):1585–1596. doi:10.1586/14737175.8.10.1585
Amato MP, Portaccio E, Goretti B, Zipoli V, Hakiki B, Giannini M, Pastò L, Razzolini L (2010) Cognitive impairment in early stages of multiple sclerosis. Neurol Sci 31(Suppl 2):S211–S214. doi:10.1007/s10072-010-0376-4
Amato MP, Hakiki B, Goretti B, Rossi F, Stromillo ML, Giorgio A, Roscio M, Ghezzi A, Guidi L, Bartolozzi ML, Portaccio E, De Stefano N, Italian RIS/MS Study Group (2012) Association of MRI metrics and cognitive impairment in radiologically isolated syndromes. Neurology 78(5):309–314. doi:10.1212/WNL.0b013e31824528c9
Labiano-Fontcuberta A, Martínez-Ginés ML, Aladro Y, Ayuso L, Mitchell AJ, Puertas-Martín V, Cerezo M, Higueras Y, Benito-León J (2016) A comparison study of cognitive deficits in radiologically and clinically isolated syndromes. Mult Scler 22(2):250–253. doi:10.1177/1352458515591072
Monjezi S, Negahban H, Tajali S, Yadollahpour N, Majdinasab N (2017) Effects of dual-task balance training on postural performance in patients with multiple sclerosis: a double-blind, randomized controlled pilot trial. Clin Rehabil 31(2):234–241. doi:10.1177/0269215516639735
Fritz NE, Cheek FM, Nichols-Larsen DS (2015) Motor-cognitive dual-task training in persons with neurologic disorders: a systematic review. J Neurol Phys Ther 39(3):142–153. doi:10.1097/NPT.0000000000000090
Wajda DA, Sosnoff JJ (2015) Cognitive-motor interference in multiple sclerosis: a systematic review of evidence, correlates, and consequences. Biomed Res Int 2015:720856. doi:10.1155/2015/720856
Okuda DT, Mowry EM, Beheshtian A, Waubant E, Baranzini SE, Goodin DS, Hauser SL, Pelletier D (2009) Incidental MRI anomalies suggestive of multiple sclerosis: the radiologically isolated syndrome. Neurology 72(9):800–805. doi:10.1212/01.wnl.0000335764.14513.1a Neurology. 2009 Apr 7;72(14):1284
Barkhof F, Filippi M, Miller DH, Scheltens P, Campi A, Polman CH, Comi G, Adèr HJ, Losseff N, Valk J (1997) Comparison of MRI criteria at first presentation to predict conversion to clinically definite multiple sclerosis. Brain 120(Pt 11):2059–2069
Tintoré M, Rovira A, Martínez MJ, Rio J, Díaz-Villoslada P, Brieva L, Borrás C, Grivé E, Capellades J, Montalban X (2000) Isolated demyelinating syndromes: comparison of different MR imaging criteria to predict conversion to clinically definite multiple sclerosis. AJNR Am J Neuroradiol 21(4):702–706
Chillemi G, Scalera C, Terranova C, Calamuneri A, Buccafusca M, Dattola V, Rizzo V, Bruschetta D, Girlanda P, Quartarone A (2015) Cognitive processess and cognitive reserve in multiple sclerosis. Arch Ital Biol 153(1):19–24. doi:10.4449/aib.v153i1.3696
Ruhe A, Fejer R, Walker B (2010) The test-retest reliability of centre of pressure measures in bipedal static task conditions--a systematic review of the literature. Gait Posture 32(4):436–445. doi:10.1016/j.gaitpost.2010.09.012
Boes MK, Sosnoff JJ, Socie MJ, Sandroff BM, Pula JH, Motl RW (2012) Postural control in multiple sclerosis: effects of disability status and dual task. J Neurol Sci 315(1–2):44–48
Lebrun C, Blanc F, Brassat D, Zephir H (2010 Aug) De Seze J; CFSEP. Cognitive function in radiologically isolated syndrome. Mult Scler 16(8):919–925. doi:10.1177/1352458510375707
Learmonth YC, Ensari I, Motl RW. Cognitive Motor Interference in Multiple Sclerosis: Insights From a Systematic Quantitative Review. Arch Phys Med Rehabil 16. doi: 10.1016/j.apmr.2016.07.018.
Mercan F, Kara B, Tiftikcioglu BI, Mercan E, Sertpoyraz FM (2016) Effects of motor-motor and motor-cognitive tasks on balance in patients with multiple sclerosis. Mult Scler Relat Disord 7:85–91. doi:10.1016/j.msard.2016.03.015
Brecl Jakob G, Remšak T, Šega Jazbec S, Horvat Ledinek A, Rot U (2017) Step initiation interferes with working memory in nondisabled patients with the earliest multiple sclerosis-a dual-task study. Gait Posture 51:201–207. doi:10.1016/j.gaitpost.2016.10.016
Wajda DA, Motl RW, Sosnoff JJ (2014) Correlates of dual task cost of standing balance in individuals with multiple sclerosis. Gait Posture 40(3):352–356. doi:10.1016/j.gaitpost.2014.04.209
Tramontano M, Morone G, Curcio A, Temperoni G, Medici A, Morelli D, Caltagirone C, Paolucci S, Iosa M (2017) Maintaining gait stability during dual walking task: effects of age and neurological disorders. Eur J Phys Rehabil Med 53(1):7–13. doi:10.23736/S1973-9087.16.04203-9
Nieuwhof F, Bloem BR, Reelick MF, Aarts E, Maidan I, Mirelman A, Hausdorff JM, Toni I, Helmich RC (2017) Impaired dual tasking in Parkinson’s disease is associated with reduced focusing of cortico-striatal activity. Brain. doi:10.1093/brain/awx042
Prosperini L, Castelli L, Sellitto G, De Luca F, De Giglio L, Gurreri F, Pozzilli C (2015) Investigating the phenomenon of “cognitive-motor interference” in multiple sclerosis by means of dual-task posturography. Gait Posture 41(3):780–785. doi:10.1016/j.gaitpost.2015.02.002
Ruggieri S, Fanelli F, Castelli L, Petsas N, De Giglio L, Prosperini L. Lesion symptom map of cognitive-postural interference in multiple sclerosis. Mult Scler 2017 :1352458517701313. doi: 10.1177/1352458517701313.
Labiano-Fontcuberta A, Mato-Abad V, Álvarez-Linera J, Hernández-Tamames JA, Martínez-Ginés ML, Aladro Y, Ayuso L, Domingo-Santos Á, Benito-León J (2016) Gray matter involvement in radiologically isolated syndrome. Medicine (Baltimore) 95(13):e3208. doi:10.1097/MD.0000000000003208
Giorgio A, Stromillo ML, De Leucio A, Rossi F, Brandes I, Hakiki B, Portaccio E, Amato MP, De Stefano N (2015) Appraisal of brain connectivity in radiologically isolated syndrome by modeling imaging measures. J Neurosci 35(2):550–558. doi:10.1523/JNEUROSCI.2557-14.2015
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author(s) declare that they have no competing interests.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Rights and permissions
About this article
Cite this article
Dattola, V., Logiudice, A.L., Bonanno, L. et al. Does the radiologically isolated syndrome exist? A dual-task cost pilot study. Neurol Sci 38, 2007–2013 (2017). https://doi.org/10.1007/s10072-017-3094-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-017-3094-3