Abstract
There is an ample evidence that hypopigmentation of the skin along the Blaschko’s lines is frequently associated with neurological disorders. Nowadays, the term “Hypomelanosis of Ito” (HI) is applied when, together with the cutaneous lesions, various and multisystem organs are involved. Among these, the most frequent are cerebral manifestations, such as cognitive delay and epileptic seizures. For this reason, hypomelanosis of Ito has been included in the group of neurocutaneous syndromes, neurologic manifestations being one of the most frequent. Epileptic seizures have been reported in patients with this disorder, but in a very few particular attention has been focused on the type and frequency of epilepsy and on the response to the treatment. Herein, we report on five patients with HI who showed episodes of epileptic seizures with onset in childhood, in absence of malformative anomalies except for the skin lesions. A survey on the frequency and types of epileptic seizures in HI children and in the literature is reported.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term “Hypomelanosis of Ito” (HI) is used to describe hypopigmentation of the skin along the Blaschko’s lines. These lines represent the streams of growth of cutaneous cells derived from a limited number of precursors and are expression of highly varied genetic mosaicism due to the presence of different clones of cells in early embryogenesis [1, 2]. In his first description Ito [3] reported a 22-year-old female in whom the lesions were restricted only to the skin. Subsequently, it appeared evident that in some cases the cutaneous lesions could be associated with various and multiple organic developmental disorders. There are different terms to define hypomelanosis which in some individual appears as a single cutaneous sign while in others as a clinical manifestation of a multisystem disorder. Recently the term “linear nevoid hypomelanosis” (along the Blaschko’s lines) has been applied to those lesions affecting only the skin and the term hypomelanosis of Ito to lesions involving both the skin and other organs. Moreover, the frequent association of hypopigmented cutaneous lesions with disorders of the central nervous system, in particular with cognitive delay and epileptic seizures, has led to considering Hypomelanosis of Ito as a quite distinct entity which is currently included in the group of neurocutaneous diseases. According to its frequency, HI is reported as the fourth neurocutaneous syndrome in order after neurofibromatosis, tuberous sclerosis complex and Sturge-Weber syndrome [4–7]. Neurologic manifestations in patients with HI have been widely reported, but in a very few has particular attention been focused on the epileptic seizures, in term of frequency, type of seizures and response to treatment.
Herein, we report a set of five patients with HI who showed episodes of epileptic seizures starting in childhood, in absence of malformative anomalies except for the skin lesions. A survey on the frequency and types of epileptic episodes in HI children and in those from the literature are reported.
Patients and methods
Between the years 2006 and 2014, in the series of 56 cases of HI collected among the pediatric neurologic out and inpatients referring to the units of Pediatrics of the University Hospital “Policlinic Vittorio Emanuele”, Catania, Italy, five patients with cutaneous signs of hypopigmentation and epileptic episodes were enrolled for this study. The patients’ family history, physical examination, serial EEG, brain MRI and cognitive evaluation (IQ) were performed. In this report, we use the term Hypomelanosis of Ito to indicate the cutaneous manifestations which follow, in narrow or broad bands, the Blaschko’s lines associated with extracutaneous involvement.
The data included in the present study were collected from the literature provided by Google Scholar, Pubmed, and Scielo using the term Hypomelanosis of Ito. The inclusion on this review was limited to papers with four or more HI patients who presented with epileptic seizures and/or others cerebral complications.
Patient 1
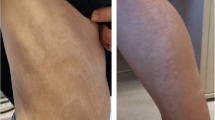
An 8-year-old male. Family history negative for skin anomalies. The child was born at term after a normal delivery. Birth-weight was 3,200 g, height 50 cm and head circumference 35 cm. He started to walk at the age of 14 months and pronounced first words at the age of 20 months. As referred by the parents, at the age of 2 years he had the first episode of generalized seizure triggered by high fever and lasting about 5 min. He had subsequent episodes of generalized tonic-clonic seizures sometime associated with fever but also without fever, treated with valproate. The epileptic episodes had a frequency of 2-3 for each year until the age of seven years. He first came to our observation at the age of 8 years with a further episode of generalized tonic-clonic seizures lasting about 8 min and blocked by rectal diazepam administration. At the clinical examination, the child showed hypochromic lesions distributed on the trunk and in the back more evident in the right side (Fig. 1). Linear streaks were also noticed in the left upper limb. Brain-MRI showed no anomalies. EEG showed the presence of generalized spike and wave discharges (Fig. 2). The patient showed a mild mental retardation (IQ 70) and no malformative anomalies were found. No other episodes of seizures were reported at follow-up 2 years later. He is still under treatment with valproate.
Patient 2
A 29-month-old female. The parents are healthy: the mother shows a cafè-au-lait spot 0.5 × 1 cm on the trunk. The mother had a risk of miscarriage during this pregnancy and was treated with anti-abortive drugs. The girl was born by cesarean section following a precocious placental abruption. Birth-weight was 2,800 g, height 49 cm, and head circumference 34 cm. The first steps of development were normal. She first came to our observation at the age of 3 years with a history of a seizure lasting a few minutes. Seven months later a focal seizure involving the face and the right arm with secondary generalization lasted 15–20 min. At the physical examination, the patient showed the presence of whorls and patches of hypochromic lesions localized on the trunk and bilateral linear streaks in the lower limbs. No malformation anomalies were noted. Brain-MRI was normal. No development delay was noticed. At the EEG, bilateral spike and waves were reported in the frontal regions. Treatment was started with valproate. No further convulsive episodes were reported at 1-year follow-up.
Patient 3
A 7-year-old male, the second child of healthy parents. He was born by cesarean section. The parents referred that he presented a normal development. The first seizure was reported at the age of 24 months. It was hemilateral of 25 min duration and localized in the left area. At the physical examination the child showed hypochromic lesions of whorls and patches sized, localized in the abdomen and in the right thigh and of linear streaks in the right upper limb. The epileptic seizures had a frequency of 3–4 per year despite valproate treatment and persisted to the age of 5 years. After a period of 2 years of remission, the seizures reappeared at the age of 7, initially localized in the left area and then generalized. EEG showed spike and slow waves in temporo-parietal regions prevalently in the right. Brain-MRI showed cisterna magna dilatation. The head circumference was above the 90 centile. No other malformation anomalies were noticed apart from moderate scoliosis. He does not show developmental delay. The child is still in treatment with valproate and no new episodes have been registered in the following 6 months.
Patient 4
A 10-year-old male was admitted for consultation due to frequent episodes of generalized epileptic seizures. We have followed this patient since the age of 4 years when he was first referred for a generalized tonic-clonic seizure of 20 min duration. He had a normal delivery, but from the first years of life he showed mild developmental delay and a reduction in head circumference. Brain-MRI did not show anomalies. The cutaneous hypochromic lesions were localized in the thorax and in the back with a configuration of whorls and patches (Fig. 3) and linear streaks on the posterior side of the upper left limb. The EEG showed the presence of generalized spike and waves discharges (Fig. 4). Treatment with sodium valproate reduced the frequency of the epileptic episodes of the type tonic–clonic generalized but they are still present with a recurrence of 1–2 per year.
Patient 5
An 11-year-old male: he first came at our observation at the age of 8 years for a complex febrile seizure. As reported by the parents, cutaneous lesions were present from the first months of age, gradually increasing to the age of 1 year, and prevalently localized in the trunk with pattern of whorls and patches. The parents reported that he had a focal seizure at the age of 9 years. He was again referred to us at the age of 11 years with a focal seizure lasting about 10 min, initially with eye deviation and then extending to the left side of the body. The EEG showed centro-temporal spikes and slow waves (Fig. 5). The cutaneous lesions were unmodified. No malformation anomalies were noted and brain MRI was normal. Treatment with valproate was started. No new seizures were recorded at the follow-up at 8 months and the school performance is good.
Discussion
Hypopigmented cutaneous lesion is a “phenotypic” expression of a single entity or a feature of a more complex disorder where, as seen in HI, the cutaneous signs are associated with different features involving mostly the brain, but also other structures [4–6].
The cutaneous lesions in HI appear as a hypopigmented areas consisting of unilateral or bilateral striations, swirls, patches or whorls involving mainly the trunk and with a linear distribution localized on the limbs. The pigmentary lesion usually appears at birth or more often during the first year of life. Multisystem involvement of HI is often reported, with manifestations affecting the CNS, scalp and hair, eyes, bones and musculoskeletal structures. Involvement of the CNS is the most frequent and it manifests with different clinical aspects, including intellective and motor delay, cerebral malformations as microcephaly or macrocephaly, epilepsy, ataxia and behavioral disturbances from attention deficit hyperactivity disorder (ADHD) to obsessive compulsive disorder (OCD) to autism spectrum disorder (ASD) [8–11].
The frequency of neurologic implication in HI is reported to be high, ranging approximately from 80 to 100 % [9, 12], and 10–40 % [13, 14]. The wide variability in the frequency of the extracutaneous involvement in HI patients is linked to the different department (e.g. pediatrics, neuropediatrics, dermatology, and genetics) where the diagnosis was made.
Intellective delay and epilepsy are, however, reported as the most frequent neurologic impairments associated with HI, ranging from 11 % to 100 % (see Table 1). In some patients the cognitive delay was reported borderline or mild and less frequently severe and in a few case associated with autism [9, 11].
Cerebral MRI in patients with HI and neurologic involvement may be normal or may be associated with white matter alterations and/or structural malformations [14–16]. Ruggieri et al. [16] reported a series of 13 patients affected by HI in 7 of whom anomalies of white matter were found. The white matter lesion observed by these Authors was related to altered or delayed myelination, disarray of cortical lamination or neuronal loss with wallerian degenerations [16]. The anomalies of the white matter were prevalently localized in the parietal periventricular and subcortical regions in both the hemispheres. Further MRI anomalies consisted of asymmetry of the cerebral hemispheres in one patient and atrophy of the cerebellar vermis in another. As with the results of this study [16], there appears to be a correlation between the CNS and the MRI anomalies: the patients with asymmetry of cerebral hemispheres had severe cognitive delay and epileptic seizures; the patient with hypoplasia of the cerebellar vermis presented clinical signs suggestive of autism spectrum disorder. Among the 13 patients with white matter involvement, two presented with the most extensive white matter involvement: one showing severe cognitive delay and episodes of focal seizures and one only focal seizures. Cerebellar hypoplasia or atrophy, hemimegalencephaly, gray matter heterotopies, blurred gray/white matter junction, pachygyria, poroencephaly, cortical dysplasia have been reported as examples of cerebral malformations in HI patients [17–21].
After cognitive delay, the second most frequent extracutaneous neurological manifestation in HI patients is represented by epileptic seizures, As reported in Table 1, [9–11, 13, 22–30], according to the literature, epileptic seizures are widely reported [22, 26, 28] with early onset (within the first year of life), and sometime refractory to anticonvulsant treatment.
Epileptic seizures in HI patients have been concerned to the frequency but there has been no extensive focus on these patients regarding the type and course of the epileptic crises. In the five patients studied here, the seizures manifested in a different way: in two patients the epileptic seizures were of generalized (GTCS) type, and in three of focal motor complex. Two also showed mild cognitive delay and in one the cerebral MRI revealed dilation of the cisterna magna. At short follow-up, the response to the treatment was good except for one patient who still continuous to present isolated seizures. Fleury [23] was the first to report epileptic episodes in 2 out 4 HI patients: in one of these patients the epileptic manifestations were focal temporal type. In a total of 13 patients, Ruggieri et al. [16] reported 6 young patients with epilepsy in 4 of whom the episodes were generalized tonic–clonic type and in 2 were focal. The largest group was described by Pasqual Castroviejo who reported 37 epileptic patients out of 76 (49 %): among these, 6 presented infantile spasms; 19 showed generalized tonic–clonic seizures; in 9 the seizures were focal and in 3 of myoclonic type. More recently, Assogba et al. [30] presented four HI patients with seizures: among these, one was drugs resistant and had episodes of generalized tonic–clonic seizures with normal brain MRI; another, in absence of neuroradiologic abnormalities, showed frequent frontal seizures partially controlled by antiepileptic drugs; the third patient suffered from mixed types of epileptic seizures including complex focal, generalized tonic–clonic, and tonic asymmetric, all were well-controlled by anticonvulsant treatment; the fourth patient showed focal seizures related to hemimegalencephaly and responding poorly to antiepileptic drugs.
According to the data collected from the literature, the presence of epileptic seizures has been reported in 140 out of 415; mental retardation in 215 out of 415; a relationship between epileptic seizures and malformations localized in the brain or involving other districts in 60 out of 97 patients. The lack of correlation between the extension of the skin lesions or brain MRI anomalies and severity of the epileptic seizures has been reported in some studies [27, 30].
In the present group of five children, the short-term prognosis for the seizures was good: four patients responded well to treatment and one partially. It should be underlined that the children reported here did not present clear malformative anomalies in the brain or other districts.
Reviewing the data taken from the literature and from our personal experience, we found that epileptic seizures may be a feature (5 children out of 56 HI patients) and also a heterogeneous epileptic manifestation of HI. The episodes may be generalized tonic–clonic, focal, myoclonic, or infantile spasm types; they may be resistant or responsive to treatment. HI seems to be a chameleonic disease in which the cutaneous involvement is only one of several presentations with which the disorder may manifest: the presence or less, the extent and the severity of the features, including intellective delay and epileptic seizures, may be widely expressed in this disorder.
References
Happle R (1993) Mosaicism in human skin. Understanding the patterns and mechanisms. Arch Dermatol 129:1460–1470
Happle R (1998) Incontinentia pigmenti versus hypomelanosis of Ito: the whys and wherefores of a confusing issue. Am J Med Genet 79:64–65
Ito M (1952) Studies of melanin XI. Incontinentia pigmenti achromians: a singular case of nevus depigmentosus systematicus bilateralis. Tohoku Exper Med 55(suppl):57–59
Sybert VP (1994) Hypomelanosis of Ito: a description, not a diagnosis. J Invest Dermatol 103:141S–143S
Taibjee SM, Bennett DC, Moss C (2004) Abnormal pigmentation in hypomelanosis of Ito and pigmentary mosaicism: the role of pigmentary genes. B J Dermatol 151:269–282
Ruggieri M, Pavone L (2000) Hypomelanosis of Ito: clinical syndrome or just phenotype? J Child Neurol 15:635–644
Küster W, König A (1999) Hypomelanosis of Ito: no entity, but a cutaneous sign of mosaicism. Am J Med Genet 85:346–350
Jelinek JE, Bart RS, Shiff GM (1973) Hypomelanosis of Ito (“Incontinentia pigmenti achromians”). Arch Dermatol 107:596–601
Pascual-Castroviejo I, Lopez Martin V, Tendero A, Martinez Bermejo A, Lopez-Terradas JM, Roche C et al (1989) Epidemiología y experiencia personal de los trastornos neuroectodérmicos. In: Pascual-Castroviejo I (ed) Trastornos Neuroectodérmicos. JR Prous, Barcelona, pp 1–71
Ruiz-Maldonado R, Toussaint S, Tamayo L, Laterza A, del Castillo V (1992) Hypomelanosis of Ito: diagnostic criteria and report of 41 cases. Pediat Dermatol 9:1–10
Zappella M (1993) Autism and hypomelanosis of Ito in twins. Develop Med Child Neurol 35:826–832
Hara M, Kozasa M, Mituisi Y, Yajima K, Saito K, Fukuyama Y (1989) Ito syndrome (Hypomelanosis of Ito) as a cause of intractable epilepsy. In: Pascual-Castroviejo I (ed) Trastornos Neuroectodérmicos. JR Prous, Barcelona, pp 221–225
Nehal KS, Pe Benito R, Orlow SJ (1996) Analysis of 54 cases of hypopigmentation and hyperpigmentation along the lines of Blaschko. Arch Dermatol 132:1167–1170
Ruggieri M (2000) Familial hypomelanosis of Ito: implications for genetic counseling. Am J Med Genet 95:82–84
Edelstein S, Naidich TP, Newton TH (2004) The rare phakomatoses. Neuroimaging Clin N Am 14:185-217, vii
Ruggieri M, Tizano G, Mazzone D, Tiné A, Pavone L (1996) Involvement of the white matter in hypomelanosis of Ito (incontinentia pigmenti achromiens). Neurology 46:485–492
Ross DL, Liwnicz BH, Chun RWM, Gilbert E (1982) Hypomelanosis of Ito (incontinentia pigmenti achromians)—a clinicopathologic study: macrocephaly and gray matter heterotopias. Neurology 32:1013–1016
Turleau C, Taillard F, Doussau de Bezignan M, Delépine N, Desbois JC, de Grouchy J (1984) Hypomelanosis of Ito (incontinentia pigmenti achromians) and mosaicism for a microdeletion of 15 q1. Hum Genet 74:185–187
Ardinger HH, Bell WE (1986) Hypomelanosis of Ito Wood’s light and magnetic resonance imaging as diagnostic measures. Arch Neurol 43:848–850
Malherbe V, Pariente D, Tardieu M, Lacroix C, Venencie PY, Hibon D et al (1993) Central nervous system lesions in hypomelanosis of Ito: an MRI and pathological study. J Neurol 240:302–304
Ono J, Harada K, Kodaka R, Ishida M, Okada S (1997) Regional cortical dysplasia associated with suspected hypomelanosis of Ito. Pediatr Neurol 17:252–254
Schwartz MF, Esterly NB, Fretzin DF, Pergament E, Rozenfeld IH (1977) Hypomelanosis of Ito (incontinentia pigmenti achromians): a neurocutaneous syndrome. J Pediatr 90:236–240
Fleury P, Dingemans K, de Groot WP, Oranje AP, Voûte PA, Woerdeman MJ et al (1986) Ito’s hypomelanosis (incontinentia pigmenti achromians). A review of four cases. Clin Neurol Neurosurg 88:39–44
Glover MT, Brett EM, Atherton DJ (1989) Hypomelanosis of Ito: spectrum of the disease. J Pediatr 115:75–80
Esquivel EE, Pitt MC, Boyd SG (1991) EEG findings in hypomelanosis of Ito. Neuropediatrics 22:216–219
Steiner J, Adamsbaum C, Desguerres I, Lalande G, Raynaud F, Ponsot G (1996) Hypomelanosis of Ito and brain abnormalities: MRI findings and literature review. Pediatr Radiol 26:763–768
Pascual-Castroviejo I, Roche MC, Martinez Fernandez V, Pérez-Romero M, Escudero RM, Garcia-Peñas JJ et al (1994) Incontinentia pigmenti: MR demonstration of brain changes. Am J Neuroradiol 115:1521–1527
Ruggieri V, Granama N, Palacios C (1998) Nervous system involvement in 30 children with Hypomelanosis of Ito. Brain Dev 20:372
Pavone L, Ruggieri M, Spalice A, Pavone P, Savasta S, Iannetti P (2006) “Hypomelanosis of Ito”. In: Curatolo P, Riva D (eds) Neurocutaneous Syndromes in children, John Libbey Eurotext, pp. 25-32
Assogba K, Ferlazzo E, Striano P, Calarese T, Villeneuve N, Ivanov I et al (2010) Heterogeneous seizure manifestations in Hypomelanosis of Ito: report of four new cases and review of the literature. Neurol Sci 31:9–16
Acknowledgments
The authors wish to thank Prof. Mike Wilkinson who assisted in the proof-reading of the manuscript.
Conflict of interest
The authors have no financial disclosures or conflicts of interest to declare concerning this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pavone, P., Praticò, A.D., Ruggieri, M. et al. Hypomelanosis of Ito: a round on the frequency and type of epileptic complications. Neurol Sci 36, 1173–1180 (2015). https://doi.org/10.1007/s10072-014-2049-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-014-2049-1