Abstract
The purpose of this study was to analyze mastication and swallowing in the elderly and confirm the association with dysphagia characteristics. A questionnaire was developed to evaluate the masticating and swallowing functions of the elderly. Mastication was analyzed using electromyography, and tongue/lip pressures were measured using Iowa Oral Performance Instrument. The results of the questionnaire showed that statistical difference in the number of teeth between the group without and with, decreased ability to swallow, and there was a correlation with lip pressure. Additionally, the higher number of teeth, the higher muscle activity, and there is a positive correlation between the number of chews and the lip pressure. Consequently, our findings suggested oral health parameters are closely associated with mastication/swallowing ability. Finally, based on the results obtained for different foods tested, we suggested that texture-modified foods are necessary to enhance swallowing ability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aging is a physiological process during which physical functions gradually decline. The associated loss of muscle mass, in particular, leads to a significant reduction in bodily function. Such reduced muscle mass is often observed in the oral cavity, along with the consequent deterioration of oral motor abilities (Laguna et al., 2015). This is accompanied by three major types of disorders—masticatory dysfunction, dysphagia, and digestive disorders (Yoon and Lee, 2013).
The primary or four muscles of mastication in the oral cavity are the masseter, temporalis, medial pterygoid, and lateral pterygoid muscles. These muscles produce the movements required for mastication, such as the opening and closing of the mouth and forward and backward jaw movements. In addition, the main propulsion force for swallowing comes from the tongue, which moves food inside the oral cavity to an ideal position for mastication before pushing it into the pharynx to prepare for swallowing (Machida, 2017).
Dysphagia occurs when the tongue and lip muscle strength is reduced (Machida, 2017; Woo, 2020), and according to previous studies, older adults may experience dysphagia (Cho et al., 2015; Park, 2015). Furthermore, dental status, which includes the number of natural teeth, total number of teeth including prosthesis, and denture use, is associated with the risk of dysphagia (Son et al., 2018).
Insufficient nutritional intake due to dysphagia is ultimately associated with malnutrition and muscle loss. The incidence of aging-related dysphagia has steadily increased, causing older adults to struggle with obtaining adequate nutrients. This may lead to conditions such as malnutrition and dehydration, which can consequently result in the deterioration of physical health and, specifically, of the oral cavity (Lim, 2009).
The elderly prefer food with familiar tastes and textures and also desire to eat hard food. However, subjectively perceived hardness differs from objective hardness levels (Park et al., 2022); therefore, it is necessary to develop texture-modified food that reflects different hardness levels. Therefore, food with a modified texture is necessary for the elderly who face difficulties in swallowing or chewing, which are considered important factors in helping them obtain sufficient nutrients to maintain health and improve their quality of life (Peyron et al., 2017). Consequently, suitable food with a modified texture needs to be developed as ingredients used in Korean dishes are often hard, difficult to chew, and difficult to swallow. According to Shin et al. (2016), the elderly found meat (28.3%) as the most challenging of all food items to chew, followed by both seafood and vegetables, at 15.2%. In case of seafood, they reported difficulty in chewing ingredients with tough textures such as squid. Further, although Korean herbs are the main source of vitamins, minerals, and dietary fiber for the elderly (Iwasaki et al., 2014), they reported that herbs were also difficult to chew.
Recently, senior-friendly food manufacturing companies in Korea, including Ourhome, CJ Freshware, Foodmerce, Hyundai Green Food, Samsung Welstory, Shinsegae, and others, are in the process of developing and releasing various new products (Kim, 2017). Given this, there is a need for basic, analytical, and developmental research to facilitate the development of age-friendly food and research on the quality characteristics of currently commercially available senior-friendly food. However, research regarding the types of age-friendly foods, their physical properties, nutrition, hygiene, etc., has not yet been conducted in Korea or elsewhere (Jang, et al., 2021).
Accordingly, the purpose of this study was to analyze oral processes such as mastication and swallowing, along with oral muscle strength and tongue pressure; we also confirmed the relationship of these factors with dysphagia characteristics.
Materials and methods
Participants
Participants were encouraged to volunteer for the study by attaching promotional material to the bulletin board of the Seongdong Senior Welfare Center (Seoul, Korea) and announcing the study in advance. The study targeted elderly females aged 65 or older. Youmans and Stierwalt (2006) found that there are gender differences in maximum tongue strength during swallowing. Therefore to ensure consistency, our study only recruited female participants. The participants who showed abnormal mastication or severe dysfunction compared with that of the general population were excluded from the study. In addition, individual health issues that affected oral activities such as irregular teeth arrangement, excessive cavities, and periodontal diseases were also excluded. The study participants were recruited from December 3, 2021 to December 17, 2021. Informed consent was obtained from the participants, and ethics approval was obtained from the Institutional Bioethics Committee of Hanyang University (Approval number: HYUIRB-202112-009).
Test food
Three types of samples were purchased from the markets in Seongdong-gu to assess the tongue [using Gajami mousse; Easy Balance (Shinsegae Food, Co., Ltd, Seoul, Korea)], gums [using Gajami; Peacock (Shinsegae Food, Co., Ltd, Seoul, Korea)], and teeth [using Neobiani; Peacock (Shinsegae Food, Co., Ltd, Seoul, Korea)]. Gajami, commonly known as halibut or flatfish, is a fish from the family Pleuronectidae. Therefore, Gajami mousse is a type of mousse made from Gajami. Neobiani is a traditional Korean dish that refers to thinly sliced, marinated, and grilled beef.
Instrumental texture measurement
The hardness of the food samples was analyzed using a texture analyzer (TA.XT plus, Stable Micro Systems, Surrey, UK). For the Gajami mousse, a speed of 600 mm/min, a trigger force of 0.02 N, and a strain of 66.7% were used with a 20-mm cylinder probe, and the puncture test was carried out at a speed of 100 mm/min using a 5-mm rod probe on the Gajami and Neobiani samples.
Assessment of swallowing ability
In this study, a questionnaire was developed based on the Korean Dysphagia Handicap Index and the dysphagia risk screening system by J. Fukada, to assess mastication and swallowing in the elderly, and the feasibility of the questionnaire was reviewed by three rehabilitation medicine specialists. The questionnaire consisted of 20 questions and assessed 3 groups of factors—associated with chewing function, swallowing function, and other factors (Table 1). Scores were allocated on a scale of 0 to 3 with 3 points for “always,” 2 points for “often,” 1 point for “sometimes,” and 0 point for “not at all.”
The following seven items were added according to the recommendation of the rehabilitation medicine specialists and professors specializing in dysphagia: “I need dentures when I’m eating”; “I often have food that spills out of my mouth while chewing”; “I still have food in my mouth after swallowing”; “I cannot chew large hard foods with my teeth”; “I cannot use my teeth to chew small hard foods”; “Water or food comes out of my nose while eating”; “I have a dull voice during or after eating”; and “Even when I try to swallow, food gets stuck in my throat and will not pass.” The total score range was 0 to 60 points; the higher the score, the lower the swallowing ability.
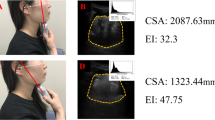
Assessment of masticatory ability
Masticatory characteristics were studied according to the textural–structural characteristics of the two types of food that were sold at the Shinsegae Food Mall (Gajami and Neobiani) and one type of food developed by Shinsegae Food, Easy Balance (Gajami mousse). The participants were evaluated using electromyography (EMG; LXM 5308, Daejeon Laksa, Daejeon, Korea) while chewing the provided food samples. The chewing time, the number of chews, and the number of swallows were recorded from the time the participants put the food in their mouths until it was swallowed. They were analyzed by linking the chewing with the hardness of the observed food. The participants were asked to sit upright in a chair and eat the food samples for performing EMG to assess masticatory characteristics. After thoroughly cleaning the skin surface, a pair of surface electrodes (T246H, Biopocket, Daejeon, Korea) were attached to the skin on the left and right masseter, temporalis, and neck muscles, and the electrodes of the 4-channel EMG device were also attached to these muscles. For testing, the chewing and swallowing factors of each participant were measured using EMG. The food samples were provided at room temperature (22 °C); 3 g of Gajami mousse was given per serving on a spoon, and 3 g of Gajami and Neobiani were given per serving with chopsticks.
The participants then chewed and swallowed the food comfortably. This was repeated three times per sample with a 30 s rest between measurements to reduce fatigue. Talking or spitting the food was forbidden, and by placing sensors on their faces, the muscle activity during the opening and closing of their jaws was measured, thus capturing the chewing patterns of the participant.
Assessment of tongue and lip strength and endurance
In this study, the maximum pressure and average pressure at the center of the tongue and lip pressures were measured using the Iowa Oral Performance Instrument (IOPI; Tongue Pressure Strength-100; TPS-100; Cybermedic, Iksan, Korea). The IOPI consists of a tongue bulb, a connecting tube, a data output terminal, and a pressure terminal and can measure maximum and average values. The bulb, connected to a flexible tube, has a volume of about 2.8 mL and is filled with air (Clark and Solomon, 2012). When the pressure that compresses the air in the bulb increases, the pressure-sensing circuit of the IOPI senses the pressure, and the maximum and average values of the tongue and lip pressures can be obtained (Solomon et al., 2008; Youmans and Stierwalt, 2006). The holding time, initial time, maximum time, and fatigue were each measured three times. The study participants sat in a chair with a backrest, with both feet on the floor, hips flexed at 90°, and they were not resting on the backrest. The examiner sat face to face with the participant and placed the bulb between the center of the tongue and the roof of the mouth and used the IOPI to measure the tongue pressure three times. Each participant was given a rest period of 30 s after each measurement. Further, the bulb was fixed with a tongue depressor in the center of the lips, and three measurements were taken with 30 s rest periods (Abe et al. 2020). The resultant value was measured three times for each test item, and the average value was analyzed.
Statistical analysis
Descriptive statistics such as frequency, percentages, and the mean for all the variables were calculated using Statistical Package for the Social Sciences (SPSS) version 26.0 (SPSS Inc., Chicago, IL, USA). Significance was confirmed using the t-test for differences between the dysphagia and normal group, using the values of the number and state of teeth. In addition, the scores obtained from the questionnaire about swallowing and mastication and the results of the oral health analysis were correlated.
Results and discussion
General characteristics of the participants
The general characteristics of the 37 women who participated in this study are described below. The mean age, mean height, body weight, and body mass index (BMI) were 74.30 ± 5.72 years, 155.22 ± 5.51 cm, 55.76 ± 6.70 kg, and 23.18 ± 2.34, respectively. The mean BMI was within the upper 30% of the range for females in their 70s, indicating their overweight status.
According to the 7th Korea National Health and Nutrition Examination Survey (2016–2018) (Hong et al., 2021), the number of functional teeth ≥ 20 and < 20 among women aged 65 years or older (n = 1741) were 52.6 and 47.4%, respectively. In this study (n = 37), number of functional teeth ≥ 20 and < 20was 67.6 and 32.4%, respectively. This disparity is unsurprising due to differences in sample sizes and surveyed areas.
Hardness of test food
According to the Korean Industrial Standards (KS H 4897) (KS 2020), the food grades were categorized into three types based on hardness— 1st grade: able to eat with teeth (more than 50,000 to less than 500,000 N/m2), 2nd grade: able to eat with gums (more than 20,000 to less than 50,000 N/m2), and 3rd grade: able to eat with tongue (more than 1,500 to less than 20,000 N/m2). Correspondingly, the samples were categorized into three types:
1st grade (Neobiani; Peacock [Shinsegae Food], 330,329.27 ± 18,382.62 N/m2), 2nd grade (Gajami; Peacock [Shinsegae Food], 50,267.50 ± 4,706.79 N/m2), 3rd grade (Gajami mousse; Easy Balance [Shinsegae Food], 3,228.72 ± 132.48 N/m2)
Differences between the reduced swallowing ability and the normal groups
A questionnaire assessing mastication and swallowing ability in the elderly was given, and the participants were divided into the following two groups according to the mean scores (6.46 ± 5.67) of the questionnaire: participants with reduced swallowing ability (RS; n = 16, mean scores (2.30 ± 1.96)) and those with normal swallowing ability (NS; n = 21, mean scores (12.07 ± 4.35)) (Table 2). The two groups did not vary significantly with respect to age, height, body weight, or BMI. However, the number of teeth was significantly higher (p = 0.004) in the NS group (22.05 ± 7.64) than in the RS group (17.94 ± 11.17). Additionally, the maximum and mean values determined by IOPI (lip or tongue) revealed no significant difference.
A major cause of decreased chewing ability in healthy older adults was tooth loss. Loss of teeth causes difficulty in breaking down food, thereby affecting bolus formation. The size of the food mass increases with the loss of teeth, and the poorly broken food mass returns to the back of the mouth; this leads to challenges in the oral transport and swallowing phase (Furuta and Yamashita, 2013). In fact, 46.2% of the elderly over the age of 65 in Korea reported that they felt discomfort in their ability to chew (Jung et al., 2017), which was determined using the “standardized swallowing assessment” and questionnaire, a screening test for swallowing disorders. In a study that examined the presence or absence of swallowing, 33.7% of the participants were found to have swallowing problems (Yang et al., 2013). In this study, it was confirmed that chewing became difficult due to the loss of teeth, and thus, swallowing ability decreased. Since swallowing problems can lead to malnutrition, dehydration, and aspiration pneumonia—which can become chronic, oral health conditions along with the overall health and quality of life of individuals are closely associated (Rönnefarth et al., 2020).
Differences between the group with ≤ 10 teeth and the group with ≥ 11 teeth
Based on the significant variation in the number of teeth, the participants were divided into two groups, participants with ten or fewer teeth (G ≤ 10) and those with eleven or more teeth (G ≥ 11), and the age of the two groups was analyzed. The result showed a significant difference (p = 0.048) between the two groups, with a mean age of 77.56 ± 6.27 years in the G ≤ 10 group and 73.25 ± 5.22 years in the G ≥ 11 group (Table 3). The maximum and mean lip pressure were 26.77 ± 11.18 kPa and 16.43 ± 6.08 kPa, respectively, in the G ≤ 10 group and 24.95 ± 16.68 kPa and 14.57 ± 7.71 kPa, respectively, in the G ≥ 11 group. Maximum and mean tongue pressure were 39.52 ± 13.13 kPa and 26.43 ± 13.13 kPa, respectively, in the G ≤ 10 group and 38.51 ± 11.60 kPa and 23.45 ± 11.76 kPa, respectively, in the G ≥ 11 group, indicating no significant difference between the groups. Concerning mastication of Gajami mousse, no significant difference was found in the right temporalis muscle activity between the two groups (G ≤ 10, 22.48 ± 14.06 µV.sec; G ≥ 11, 16.96 ± 12.55 µV.s) However, a significant difference (p = 0.020) was observed in the left temporalis muscle activity between the two groups for mastication of Gajami (G ≤ 10, 45.34 ± 49.51 µV.sec; G ≥ 11, 19.21 ± 16.99 µV.sec). In addition, a significant difference in muscle activity on the right side of the neck (p = 0.047) was found between the groups upon mastication of Gajami mousse (G ≤ 10, 66.61 ± 30.16 µV.sec; G ≥ 11 46.17 ± 22.65 µV.s), while no significant difference was seen on the left side of the neck (G ≤ 10, 66.76 ± 38.16 µV.sec; G ≥ 11 54.46 ± 41.96 µV.sec).
Several previous studies have shown that the masticatory ability of the elderly is associated with the number of residual teeth and functional tooth units (Ikebe et al., 2011; Ueno et al., 2010; Hatch et al., 2011). Markovic et al. (1999) showed that some individuals with dentures have significantly reduced occlusal force and masticatory muscle activity compared to those with natural teeth and have difficulty in chewing or breaking food to form a bolus due to irregular mastication activities (Hara et al., 2019). Therefore, it was confirmed that the number of teeth and muscle activity are associated and the loss of teeth leads to a decrease in swallowing ability.
Differences between the denture group and natural teeth group
Table 4 presents the results of analyzing the differences between the two groups when they were divided into a denture group (DG; n = 10) and natural teeth group (NTG; n = 27). The questionnaire score was 8.69 ± 5.23 in the DG and 5.24 ± 5.64 in the NTG, with no significant difference between the two groups. The number of chews upon mastication of Gajami was significantly higher in the NTG (36.75 ± 25.98) group than in the DG (24.31 ± 12.28; p = 0.034).
According to a previous study, 48.1% of the elderly reported using partial dentures and 22.6% full dentures (Lee and Han, 2015). Thus, a total of 70.7% of 178 study participants used dentures. The high dependence on dentures in the elderly is ultimately associated with difficulty in mastication. In a study based on the 2009 National Nutrition Survey by Kim et al. 2012, it was reported that, of the three major nutrients, carbohydrate intake was the highest and protein intake was the lowest. In this study, we observed a significant difference in the number of times flounder was chewed between DG and NTG; flounder, the main protein source for Koreans, is a difficult ingredient for the elderly to chew. A previous study (Lee and Han, 2015) reported that, for the elderly, among the food items that were in high demand but insufficiently consumed due to difficulty in chewing or swallowing, fish ranked first for men, followed by meat and vegetables. Likewise, women also had the highest demand for fish. Therefore, the data suggest that the intake of fish decreased due to tooth loss or the use of dentures.
Correlation between the swallowability scores among participants
Table 5 presents the correlation between the questionnaire scores of all the participants (n = 37) and each variable; a significant difference (p < 0.05) was observed for the maximum lip pressure. However, no significant difference was observed among the other parameters. Generally, the muscles in the lower part of the face, such as the cheeks, lips, and tongue, are called the orofacial muscles. According to Clark and Solomon (2012), these orofacial muscles, especially those of the cheeks and lips, are affected by oral containment; they are responsible for the manipulation of food and provide sufficient strength for the functional movement of the tongue (Clark and Solomon, 2012; Solomon et al., 2008). Therefore, after swallowing food, participants with decreased sensation and movement in the mouth and face were likely to have food left in the tongue and mouth furrows, and oral movement may be delayed due to the weakening of these muscles.
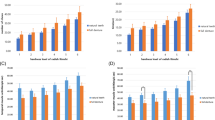
Correlation between the activation of muscles, masticating time, and the mastication number
In Fig. 1c and d, mastication time and the number of mastication for ingesting each of the three samples were assessed. Furthermore, the correlation between mastication time, the number of mastication, and muscle activity of temporalis and masseter were analyzed when participants (n = 37) ingested each of the three samples. As shown in Fig. 1, significant differences were found in the muscle activity, mastication time, and the number of mastication of the masseter muscle when the samples of Gajami mousse, Gajami, and Neobiani were ingested. In Fig. 1a, the muscle activity of the masseter muscle when the three samples were ingested is shown. In Fig. 1b, the muscle activity of the temporal during mastication of the three samples is plotted; it was confirmed that there was no significant difference. Figure 1c and d show significant differences in mastication time and number of chews when ingesting each of the three samples. As reported in previous studies, the hardness of food was detected during mastication, and it was confirmed that it affected jaw muscle activity, masticatory force, and mandibular movement (Mioche et al., 2004; Van der Bilt, 2011). Therefore, it was also confirmed in this study that food had a significant effect on the muscle activity of the masseter, mastication time, and number of chews required for swallowing ability.
Conclusion
Our findings suggested that oral health, determined based on the number of teeth, lip pressure, and denture use, was closely associated with the mastication and swallowing ability of the elderly. The results of this study demonstrated the effects of aging of the oral muscles in the lips and the consequent decline in muscle activity on masticatory functions.
To develop food suitable for consumption by elderly individuals, it is necessary to understand the various oral health characteristics and swallowing abilities of the elderly, emphasizing the importance of developing texture-modified food. However, this study was limited by region and gender. In the future, further studies on differently textured foods should be conducted based on the oral health and swallowing ability of the elderly by recruiting a larger number of participants of both sexes and covering a wider geographical region, preferably involving multiple institutions.
(A) Correlation between the three samples with respect to the activation of the masticatory muscle; (B) Correlation between the three samples with respect to the activation of the temporal muscle; (C) Correlation between the three samples with respect to the mastication time; and (D) Correlation between the three samples with respect to the number of chews. ***Significant difference (p < 0.001)
References
Abe T, Won V, Spitz RW, Viana RB, Bell ZW, Yamada Y, Loenneke JP. Influence of sex and resistance training status on orofacial muscle strength and morphology in healthy adults between the ages of 18 and 40: A cross-sectional study. American Journal of Human Biology. 6: e23401. (2020)
Cho SY, Choung RS, Saito YA, Schleck CD, Zinsmeister AR, Locke Iii GR, Talley NJ. Prevalence and risk factors for dysphagia: a USA community study. Neurogastroenterology and Motility: The Official Journal of the European Gastrointestinal Motility Society. 27: 212-219. (2015)
Clark HM, Solomon NP. Age and sex differences in orofacial strength. Dysphagia. 1: 2-9. (2012)
Fukada J. Development of dysphagia risk screening system for elderly persons. The Japanese Journal of Dysphagia Rehabilitation. 1: 31-42. (2006)
Furuta M, Yamashita Y. Oral health and swallowing problems. Current Physical Medicine and Rehabilitation Reports. 1: 216-222. (2013)
Hara K, Tohara H, Kenichiro K, Yamaguchi K, Ariya C, Yoshimi K, Nakane A, Minakuchi S. Association between tongue muscle strength and masticatory muscle strength. Journal of Oral Rehabilitation. 46: 134-139. (2019)
Hatch JP, Shinkai RS, Sakai S, Rugh JD, Paunovich ED. Determinants of masticatory performance in dentate adults. Archives of Oral Biology. 7: 641-648. (2011)
Hong JH, Lee YJ, Kim TH, Kim RE, Chung WJ. Oral Health Status and Behavior Factors Associated with Self-Rated Health Status among the Elderly in South Korea: The 7th Korea National Health and Nutrition Examination Survey (2016–2018). Health Policy and Management. 31: 74-90. (2021)
Ikebe K, Matsuda KI, Kagawa R, Enoki K, Yoshida M, Maeda Y, Nokubi T. Association of masticatory performance with age, gender, number of teeth, occlusal force and salivary flow in Japanese older adults: is ageing a risk factor for masticatory dysfunction?. Archives of Oral Biology. 56: 991-996. (2011)
Iwasaki M, Taylor GW, Manz MC, Yoshihara A, Sato M, Muramatsu K, Watanabe R, Miyazaki H. Oral health status: relationship to nutrient and food intake among 80- year-old Japanese adults. Community Dentistry and Oral Epidemiology. 42: 441-450. (2014)
Jang MS, Kim PH, Oh JY, Park SY, Kim YY, Kang SI, Kim JS. Quality Characteristics of Domestic Commercial Senior-friendly Foods. Korean Journal of Fisheries and Aquatic Sciences. 54: 251-260. (2021)
Jung KH, Oh YH, Lee YK, Oh MA, Kang EN, Kim KR, Hwang NH, Kim SJ, Lee SH, Lee SK, Hong SY. 2017 National Elderly Survey (11-1352000-000672-12), Seoul: Korea Institute for Health and Social Affairs. (in Korean). (2017)
Kim YJ. Requirement and status of domestic silver foods. Food Industry and Nutrition. 22: 1-5. (2017)
Korean Industrial Standards (KS). 2020 Seniors Friendly Foods (KS H 4897). 2020 [cited 2021 Dec 27]. Available from: https://eks.kr/streamdocs/view/sd;streamdocsId=72059203773233835.
Kim YS, Lee Y, Chung YS, Lee DJ, Joo NS, Hong D. Prevalence of sarcopenia and sarcopenic obesity in the Korean population based on the fourth Korean National Health and Nutritional Examination Surveys. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 67: 1107-1113. (2012)
Laguna L, Sarkar A, Artigas G, Chen J. A quantitative assessment of the eating capability in the elderly individuals. Physiology and Behavior. 147: 274-281. (2015)
Lee GY, Han JA. Demand for elderly food development: Relation to oral and overall health-Focused on the elderly who are using senior welfare centers in Seoul. Journal of the Korean Society of Food Science and Nutrition. 44: 370-378. (2015)
Lim JH. Conservative treatment of Dysphagia. Brain & Neurorehabilitation. 2: 108-112. (2009)
Machida N, Tohara H, Hara K, Kumakura A, Wakasugi Y, Nakane A, Minakuchi S. Effects of aging and sarcopenia on tongue pressure and jaw-opening force. Geriatrics & Gerontology International. 17: 295-301. (2017)
Markovic D, Petrovic L, Primovic S. Specifics of mastication with complete dentures. Medicinski Pregled. 52: 464-468. (1999)
Mioche L, Bourdiol P, Monier S, Martin JF, Cormier D. Changes in jaw muscles activity with age: effects on food bolus properties. Physiology & Behavior. 82: 621-627. (2004)
Park SJ. Dysphagia risk and associated factors among community-dwelling elders. Journal of the Korean Society of Food Science and Nutrition. 44: 49-56. (2015)
Park YS, Hong HP, Ryu SR, Lee S, Shin WS. Effects of textured food masticatory performance in older people with different dental conditions. BMC Geriatrics. 22: 1-12. (2022)
Peyron MA, Woda A, Bourdiol P, Hennequin M. Age-related changes in mastication. Journal of Oral Rehabilitation. 44: 299-312. (2017)
Rönnefarth M, Hanisch N, Brandt AU, Mähler A, Endres M, Paul F, Doss S. Dysphagia affecting quality of life in cerebellar ataxia—A large survey. The Cerebellum. 19: 437-445. (2020)
Shin KJ, Lee EJ, Lee S, J. Study on demand elderly foods and food preferences among elderly people at senior welfare centers in Seoul. Journal of the East Asian Society of Dietary Life. 26: 1-10. (2016)
Solomon NP, Clark HM, Makashay MJ, Newman LA. Assessment of orofacial strength in patients with dysarthria. Journal of Medical Speech-Language Pathology. 16: 251-258. (2008)
Son HJ, Park YM, Yim SY, Heo YR, Son MK. Prevalence and influencing factors of dysphagia in elderly patients. Oral Biology Research. 4: 208-215. (2018)
Ueno M, Yanagisawa T, Shinada K, Ohara S, Kawaguchi Y. Category of functional tooth units in relation to the number of teeth and masticatory ability in Japanese adults. Clinical Oral Investigations. 14: 113-119. (2010)
Van der Bilt A. Assessment of mastication with implications for oral rehabilitation: a review. Journal of Oral Rehabilitation. 38: 754-780. (2011)
Woo KS. The effectiveness of oral neurocognitive rehabilitation therapy on dysphagia and dysarthria of stroke patients. Journal of Korean Society of Neurocognitive Rehabilitation. 2: 1-8. (2020)
Yang EJ, Kim MH, Lim JY, Paik NJ. Oropharyngeal dysphagia in a community-based elderly cohort: the Korean longitudinal study on health and aging. Journal of Korean Medical Science. 28: 1534-1539. (2013)
Yoon JH, Lee HJ. Perceptions on evaluation and treatment of swallowing disorders in speech-language pathologists. Phonetics and Speech Sciences. 5: 43-51. (2013)
Youmans SR, Stierwalt JA. Measures of tongue function related to normal swallowing. Dysphagia. 21: 102-111. (2006)
Acknowledgments
This work was supported by the Korea Institute of Planning and Evaluation for Technology in Food, Agriculture and Forestry (IPET) through the High Value-added Food Technology Development Program, funded by the Ministry of Agriculture, Food and Rural Affairs (MAFRA) (321032031SB010 and 321022041SB010).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interest
On behalf of all the authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, HJ., Park, YS., Choi, KJ. et al. Impact of varying food hardness on mastication/swallowing. Food Sci Biotechnol 32, 959–967 (2023). https://doi.org/10.1007/s10068-022-01237-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10068-022-01237-2