Abstract
Anti-thrombotic activity and safety of nattokinase, an enzyme produced by Bacillus subtilis during soybean fermentation, were investigated in comparison with tissue-type plasminogen activator (t-PA). Carotid arterial thrombosis was produced with a FeCl3-soaked paper, followed by intravenous injection of nattokinase or t-PA. Nattokinase and t-PA delayed thrombus formation, near-fully (> 90%) inhibiting at 75 and 8.5 mg/kg, respectively. As adverse effects, t-PA induced petechial haemorrhage at 10 mg/kg in the lungs and thymus, and extensive bleeding at 20 mg/kg. Nattokinase also caused pulmonary haemorrhage from 300 mg/kg. Collectively, the standard safety margins (SSMs) for t-PA and nattokinase were calculated to be 1.2 and 4.0, respectively. Combinational treatment with dexamethasone (2 mg/kg) increased the efficacy and safety of t-PA and nattokinase, widening their SSMs to 2.4 and 8.0, respectively. The results indicate that nattokinase delayed thrombus formation and dissolved thrombi, and that nattokinase could be a good candidate anti-thrombotic agent with relatively-low haemorrhagic risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thrombosis due to embolic or haemorrhagic artery occlusion is one of the major causes of cerebrovascular diseases. Although platelets are important in the physiological homeostasis, their aggregation plays a crucial role in the thrombus formation (Majid et al., 2001). Upon arterial endothelial injury, coagulating factors are exposed or generated: i.e., adhesive ligands including collagen and von Willebrand Factors (vWF) as well as soluble agonists such as thrombin and adenosine diphosphate (ADP) facilitate adhesion of platelets to the injured arterial walls, activation, and aggregation (Jackson et al., 2003), and thereby hinder blood flow. It is well known that transition metals facilitate oxidative radical formation that causes cellular and tissue injuries, especially endothelial cell damage leading to thrombosis. Hence, application of ferric chloride (FeCl3) to arterial walls has been used to assess the anti-thrombotic efficacy of blood flow enhancers (Eckly et al., 2011; Jang et al., 2013; Lee et al., 2012).
Nattokinase, produced by Bacillus subtilis during soybean fermentation, was identified as a profibrinolytic serine protease rich in Natto, an Oriental traditional food (Ko et al., 2004; Kotb, 2014; Sumi et al., 1987, 1990). It was reported that nattokinase dissolved thrombi in vitro (Urano et al., 2001), and prevented carrageenan-induced rat-tail thrombosis in vivo (Kamiya et al., 2010; Xu et al., 2014). Nattokinase also preserved blood flow by inhibiting artificial thrombosis (Jang et al., 2013; Kamiya et al., 2010; Suzuki et al., 2003), in which inhibitory activities on the thromboxane formation and platelet aggregation were proposed as action mechanisms (Jang et al., 2013), and thereby improved shoulder stiffness, back pain, and coldness of the extremities (Hitosugi et al., 2015). It is well known that nattokinase decreases blood pressure in spontaneously hypertensive rats (Fujita et al., 2011) and in humans (Kim et al., 2008). Actually, nattokinase was recently approved by the Korea Ministry of Food and Drug Safety (MFDS) as a functional food improving blood flow.
Indeed, thrombolysis via intravenous injection of tissue-type plasminogen activator (t-PA) is the medical treatment approved only for acute ischemic stroke (Del Zoppo et al., 2009). However, up to 6.8% patients developed intracerebral haemorrhage after having received t-PA injection (Emberson et al., 2014). In a recent study, we demonstrated that oral pretreatment with nattokinase displayed anti-thrombotic activity in a FeCl3-induced carotid artery thrombosis model (Jang et al., 2013). From the former studies, it was strongly proposed that nattokinase may be useful not only for preservation and enhancement of normal endogenous fibrinolytic function, but also for dissolution of essential portion of the blood clots and thrombi. On the other hand, dexamethasone has been widely used to protect organs from intestinal ischemia–reperfusion-related injury (Zhang et al., 2013). Anti-inflammatory drugs including dexamethasone are also commonly prescribed during treatment of cerebral and cardiac strokes. In this context, we assessed the posttreatment efficacy (anti-thrombotic ativity) and safety (haemorrhagic adverse effect) of nattokinase and t-PA alone as well as in combination with dexamethasone, and suggested the effectiveness of nattokinase based on its SSM.
Materials and methods
Materials
Nattokinase was obtained from Wako (Richmond, USA). The activity of nattokinase (360 IU/g) was determined via degradation of specific amido substrate (S-2222). t-PA (Actilyse®) and dexamethasone were obtained from Boehringer Ingelheim (Mannheim, Germany) and Ilsung Pharmaceuticals (Seoul, Korea), respectively. Nattokinase, t-PA, dexamethasone or their vehicle (saline) was intravenously injected (1 mL/kg).
Animals
Seven-week-old male Sprague–Dawley rats (body weight 200–220 g, Daehan-Biolink, Eumseong, Korea) were used for the experiments after 1-week acclimation to the laboratory environment. The animals were housed in a room with environmental conditions controlled to 22 ± 2 °C temperature, 40–70% relative humidity, and 12-h 150–300 lx light–dark cycle, and fed commercial rodent chow and purified tap water ad libitum. The animal study protocols were approved by the Institutional Animal Care and Use Committee of Chungbuk National University (CBNU), Korea. All animal experiments were conducted according to the Standard Operation Procedures of Laboratory Animal Research Center of CBNU.
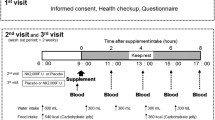
Assessment of anti-thrombotic effects
The rats (n = 8 per group) were anaesthesized by intramuscular injection of Zoletil® (Virbac, Carros cedex, France; 1 mL/kg). Under maintaining constant body temperature (36–37 °C) with a heating pad, the rats’ right carotid artery was isolated, and carefully dissected away surrounding tissues including the vagus nerve. Aortic blood flow rate was monitored with a laser Doppler flowmeter (AD Instruments, Colorado Springs, USA). Arterial thrombosis was induced by wrapping the exposed artery with a filter paper (3 mm in diameter) soaked with 25% FeCl3 near (5 mm anterior to) the flowmeter probe for 10 min (Jang et al., 2013, 2014). Five-min later, nattokinase (25–400 mg/kg) and t-PA (5–30 mg/kg) alone or combined with dexamethasone (2 mg/kg) were intravenously administered. The blood flow was monitored for 40 min. The rats were sacrificed under deep anaesthesia, and the visible thrombotic arteries were cut and fixed in 10% neutral formalin solution. Paraffin-embedded tissue sections were stained with hematoxylin–eosin, and examined the lesions under a light microscope.
Assessment of haemorrhagic adverse effects
The sacrificed rats were perfused via intraventricular injection of phosphate-buffered saline (PBS). The major organs were removed, and carefully examined for the surface haemorrhagic lesions. Paraffin-embedded tissue sections, after hematoxylin–eosin staining, were examined to confirm congestion and haemorrhage under a light microscope.
SSM, an index of the effectiveness and safety of therapeutics, was expressed as the ratio of toxic (haemorrhagic) dose to therapeutic dose of nattokinase and t-PA alone or in combination with dexamethasone.
Statistical analysis
The results are presented as mean ± standard deviation. The results was analyzed by one-way analysis of variance (ANOVA) followed by the Dunnett’s multiple-range test correction using SPSS version 12.0 (SPSS, Chicago, USA). P < 0.05 was considered statistically significant.
Results and discussion
Ten-min application of FeCl3 (25%) to the external surface of carotid artery decreased the blood flow, near-fully blocking in 40–50 min. However, intravenous injection of nattokinase in 5 min after 10-min application of FeCl3 maintained the blood flow by blocking thrombotic process in a dose-dependent manner (Fig. 1A). Notably, nattokinase fully inhibited the decrease in blood flow at 75 mg/kg and higher doses. By comparison, intravenously administered t-PA also suppressed the thrombosis in a dose-dependent manner, maintaining near-fully the blood flow at 8.5 mg/kg (Fig. 1B).
Effects of nattokinase (A) and tissue-type plasminogen activator (t-PA; B) on the carotid artery thrombosis induced by FeCl3 application outside the arterial wall. Nattokinase or t-PA were intravenously injected 5 min after FeCl3 exposure. ○: vehicle (phosphate-buffered saline), ▽: 25 mg/kg nattokinase or 5 mg/kg t-PA, □: 50 mg/kg nattokinase or 7.5 mg/kg t-PA; ◇: 75 mg/kg nattokinase or 8.5 mg/kg t-PA, △: 100 mg/kg nattokinase or 10 mg/kg t-PA
Dexamethasone (2 mg/kg) improved the blood flow to some extent, too (about 26.5%) (Fig. 2). Notably, dexamethasone further potentiated the efficacy of nattokinase (25–50 mg/kg; Fig. 2A, B), lowering the effective dosage of nattokinase. By comparison, dexamethasone did not significantly affect the efficacy of t-PA (5–7.5 mg/kg; Fig. 2C, D).
Effects of nattokinase (A, B) and tissue-type plasminogen activator (t-PA; C, D) alone or in combination with dexamethasone on the carotid artery thrombosis induced by FeCl3 application outside the arterial wall. Nattokinase, t-PA or dexamethasone were intravenously injected 5 min after FeCl3 exposure. ○: vehicle (phosphate-buffered saline), ●: dexamethasone (2 mg/kg) alone, ▽: nattokinase (25 mg/kg) or t-PA (5 mg/kg) alone, ▼: nattokinase (25 mg/kg) or t-PA (5 mg/kg) plus dexamethasone, □: nattokinase (50 mg/kg) or t-PA (7.5 mg/kg) alone, ■: nattokinase (50 mg/kg) or t-PA (7.5 mg/kg) plus dexamethasone
As dissected 40 min after the application of FeCl3, the arteries were entirely plugged with thrombi in the animals treated with vehicle or dexamethasone (2 mg/kg) (Fig. 3). Interestingly, however, the thrombi were small and loose, without full obstruction of the arterial lumens, in the animals treated with nattokinase (25 mg/kg) or t-PA (5 mg/kg).
Representative findings of carotid arterial thrombi produced by FeCl3 application outside the arterial wall. Vehicle (phosphate-buffered saline, PBS), dexamethasone (Dexa; 2 mg/kg), nattokinase (Natto; 25 mg/kg) or tissue-type plasminogen activator (t-PA; 5 mg/kg) were intravenously injected 5 min after FeCl3 exposure
Although intravenous administration of nattokinase and t-PA exerted beneficial effects on blood flow impaired by oxidative vascular wall damage, they exhibited adverse effects at high doses. That is, nattokinase induced petechial haemorrhage in the internal organs (lungs and thymus) from 300 mg/kg (Fig. 4). Such gross haemorrhagic findings were confirmed under microscopic observations. t-PA also caused petechial haemorrhage in the lungs and thymus at 10 mg/kg, showing extensive congestion and bleeding from 20 mg/kg (Fig. 5). Notably, such haemorrhagic responses to thromobolytic compounds were attenuated by combinational treatment with dexamethasone (2 mg/kg), increasing the haemorrhagic dosages of nattokinase and t-PA to 400 and 20 mg/kg, respectively (Table 1).
Based on the ratio of therapeutic (effective) to toxic (haemorrhagic) doses, SSMs for nattokinase and t-PA were estimated to be 4.0 and 1.2, respectively (Table 1). Notably, dexamethasone enhanced the safety of both nattokinase and t-PA, doubling their SSMs to 8.0 and 2.4, respectively.
Nattokinase from B. subtilis Natto substantially blocked thrombus formation with relatively-low haemorrhagic risk. The SSM (4.0) of nattokinase was much wider that (1.2) of t-PA, and it was doubled in combination with dexamethasone (2 mg/kg) to 8.0.
FeCl3 triggers oxidative vascular endothelial injury, causing exposure of subendothelial extracellular matrix (ECM). Then, platelets interact with collagen and vWF in ECM via their specific platelet surface receptors, leading to adhesion of platelets to the injured vessels. Activated platelets undergo calcium mobilization and the release of ADP and thromboxane further accelerate recruitment and aggregation of platelets for thrombus formation (Furie and Furie, 2005). In previous studies, in addition to direct thrombolytic activity (Urano et al., 2001), nattokinase inhibited thromboxane formation and platelet aggregation in vitro, and thereby preserved blood flow by inhibiting artificial thrombosis in vivo (Jang et al., 2013; Suzuki et al., 2003). Indeed, after oral pretreatment, nattokinase fully prevented FeCl3-induced artery thrombosis at 400 mg/kg (Jang et al., 2013). Following intravenous posttreatment, the enough therapeutic (anti-thrombotic) efficacy of purified nattokinase was obtained at 75 mg/kg, which was achieved with 8.5 mg/kg t-PA.
It was also reported that subcutaneous injection of nattokinase substantially reduced the tail vein infarction in a carrageenan-induced tail thrombosis model (Kamiya et al., 2010; Xu et al., 2014). The results indicate that nattokinase also prevents inflammation-mediated vascular thrombosis, in addition to the beneficial effects on oxidative damage-induced thrombosis in the present study. It is of interest to note that intravenous administration of nattokinase enhanced fibrinolytic activity and the production of t-PA in the plasma (Fujita et al., 1995; Sumi et al., 1990). The findings represent possibilities of both the prevention and posttreatment therapy of ischemic diseases via inhibition of thrombus formation and facilitation of fibrinolysis, since nattokinase dissolves the fibrin clot (Suzuki et al., 2003; Urano et al., 2001).
Clinically, t-PA has been used for the emergency treatment of acute ischemic stroke (Del Zoppo et al., 2009; Konstantinides et al., 2001; The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group, 1995). However, t-PA therapy remains problematic due to its extremely-narrow window of efficacy (within 3 h after the onset of the stroke) and potential haemorrhagic adverse effect that may result in a fatal outcome (Emberson et al., 2014; Jin et al., 2014; Zivin, 1999). Although intracerebral haemorrhage is the most feared complication of t-PA, other potential adverse reactions including anaphylaxis and angioedema (Rudolf et al., 1999), systemic bleeding (Zhang et al., 2013), and myocardial rupture (Brass et al., 2000) occur less commonly. Indeed, intravenous injection of t-PA caused congestion and petechial haemorrhages in both the lungs and thymus at 10 mg/kg, a dosage not much higher than its effective dose (8.5 mg/kg). Furthermore, t-PA induced extensive bleeding from 20 mg/kg. The SSM of t-PA in the present FeCl3-triggered thrombosis model was found to be 1.2, indicative of a very narrow therapeutic window. Thus, there is a need for an effective alternative candidate from natural sources with minimal risk of adverse effects.
In comparison with t-PA, nattokinase showed therapeutic dosage of 75 mg/kg for full anti-thrombotic activity. It is of interest to note that nattokinase caused week petechiae in the lungs and thymus at 300 mg/kg, displaying an SSM of 4.0 that is much wider than that of t-PA (1.2). On the other hand, dexamethasone is one of the most frequently-prescribing anti-inflammatory drugs (Bronicki et al., 2000; El Azab et al., 2002; Heying et al., 2012). In addition, dexamethasone is a well-known membrane-stabilizing agent, effective for the prevention of high-altitude illness causing cerebral and pulmonary oedema (Fischer et al., 2001; Nieto Estrada et al., 2017; Zafren, 2014). In the present study, therefore, we investigated whether combinational treatment with dexamethasone affects both the anti-thrombotic and haemorrhagic potentials of nattokinase and t-PA.
As inferred from a previous report (Zhang et al., 2013), dexamethasone (2 mg/kg) delayed the thrombus formation to some extent (26.5%). In addition, dexamethasone slightly increased the anti-thrombotic activity of nattokinase, that is, decreasing nattokinase’s therapeutic dosage. By comparison, dexamethasone showed a negligible effect on the therapeutic dosage of t-PA. Interestingly, however, dexamethasone remarkably attenuated the haemorrhagic dosages of both nattokinase and t-PA, indicative of the corticosteroids’ membrane-stabilizing potential. Therefore, it is expected that the combinational treatment of nattokianse or t-PA plus dexamethasone may provide safer profiles by lowering the risk of haemorrhage.
In this study, it was demonstrated that nattokinase, especially in combination with dexamethasone, exerted an excellent anti-thrombotic activity at practically-low haemorrhagic risk. Although the preventive efficacy of nattokinase on the thrombus formation is well documented, this may be the first report on posttreatment therapeutic activity of nattokinase. Most importantly, nattokinase was much superior to t-PA, the traditional thrombolytic, in safety, which was confirmed to possess three-fold SSM. Although additional follow-up studies to clarify underlying mechanisms remain, it is proposed that nattokinase could be an attention-attractive candidate for the improvement of blood flow, and that combinational therapy with dexamethasone may provide a good effective and safe prescription.
References
Brass LM, Lichtman JH, Wang Y, Gurwitz JH, Radford MJ, Krumholz HM. Intracranial hemorrhage associated with thrombolytic therapy for elderly patients with acute myocardial infarction. Stroke 31: 1802–1811 (2000)
Bronicki RA, Backer CL, Baden HP, Mavroudis C, Crawford SE, Green TP. Dexamethasone reduces the inflammatory response to cardiopulmonary bypass in children. Ann. Thorac. Surg. 69: 1490–1495 (2000)
Del Zoppo GJ, Saver JL, Jauch EC, Adams HP Jr; American Heart Association Stroke Council. Expansion of the time window for treatment of acute ischemic stroke with intravenous tissue plasminogen activator: a science advisory from the American Heart Association/American Stroke Association. Stroke 40: 2945–2948 (2009)
Eckly A, Hechler B, Freund M, Zerr M, Cazenave JP, Lanza F, Mangin PH, Gachet C. Mechanisms underlying FeCl3-induced arterial thrombosis. J. Thromb. Haemost. 9: 779–789 (2011)
El Azab SR, Rosseel PM, de Lange JJ, Groeneveld AB, van Strik R, van Wijk EM, Scheffer GJ. Dexamethasone decreases the pro- to anti-inflammatory cytokine ratio during cardiac surgery. Br. J. Anaesth. 88: 496–501 (2002)
Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, Brott T, Cohen G, Davis S, Donnan G, Grotta J, Howard G, Kaste M, Koga M, von Kummer R, Lansberg M, Lindley RI, Murray G, Olivot JM, Parsons M, Tilley B, Toni D, Toyoda K, Wahlgren N, Wardlaw J, Whiteley W, del Zoppo GJ, Baigent C, Sandercock P, Hacke W; Stroke Thrombolysis Trialists’ Collaborative Group. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 384: 1929–1935 (2014)
Fischer S, Renz D, Schaper W, Karliczek GF. In vitro effects of dexamethasone on hypoxia-induced hyperpermeability and expression of vascular endothelial growth factor. Eur. J. Pharmacol. 411: 231–243 (2001)
Fujita M, Hong K, Ito Y, Fujii R, Kariya K, Nishimuro S. Thrombolytic effect of nattokinase on a chemically induced thrombosis model in rat. Biol. Pharm. Bull. 18: 1387–1391 (1995)
Fujita M, Ohnishi K, Takaoka S, Ogasawara K, Fukuyama R, Nakamuta H. Antihypertensive effects of continuous oral administration of nattokinase and its fragments in spontaneously hypertensive rats. Biol. Pharm. Bull. 34: 1696–1701 (2011)
Furie B, Furie BC. Thrombus formation in vivo. J. Clin. Invest. 115: 3355–3362 (2005)
Heying R, Wehage E, Schumacher K, Tassani P, Haas F, Lange R, Hess J, Seghaye MC. Dexamethasone pretreatment provides antiinflammatory and myocardial protection in neonatal arterial switch operation. Ann. Thorac. Surg. 93: 869–876 (2012)
Hitosugi M, Hamada K, Misaka K. Effects of Bacillus subtilis var. natto products on symptoms caused by blood flow disturbance in female patients with lifestyle diseases. Int. J. Gen. Med. 8: 41–66 (2015)
Jackson SP, Nesbitt WS, Kulkarni S. Signaling events underlying thrombus formation. J. Thromb. Haemost. 1: 1602–1612 (2003)
Jang JY, Kim TS, Cai J, Kim J, Kim Y, Shin K, Kim KS, Park SK, Lee SP, Choi EK, Rhee MH, Kim YB. Nattokinase improves blood flow by inhibiting platelet aggregation and thrombus formation. Lab. Anim. Res. 29: 221–225 (2013)
Jang JY, Kim TS, Cai J, Kim J, Kim Y, Shin K, Kim KS, Lee SP, Kang MH, Choi EK, Rhee MH, Kim YB. Perilla oil improves blood flow through inhibition of platelet aggregation and thrombus formation. Lab. Anim. Res. 30: 21–27 (2014)
Jin X, Liu J, Liu W. Early ischemic blood brain barrier damage: a potential indicator for hemorrhagic transformation following tissue plasminogen activator (tPA) thrombolysis? Curr. Neurovasc. Res. 11: 254–262 (2014)
Kamiya S, Hagimori M, Ogasawara M, Arakawa M. In vivo evaluation method of the effect of nattokinase on carrageenan-induced tail thrombosis in a rat model. Acta Haematol. 124: 218–224 (2010)
Kim JY, Gum SN, Paik JK, Lim HH, Kim KC, Ogasawara K, Inoue K, Park S, Jang Y, Lee JH. Effects of nattokinase on blood pressure: a randomized, controlled trial. Hypertens. Res. 31: 1583–1588 (2008)
Ko JH, Yan JP, Zhu L, Qi YP. Identification of two novel fibrinolytic enzymes from Bacillus subtilis QK02. Comp. Biochem. Physiol. C Toxicol. Pharmacol. 137: 65–74 (2004)
Konstantinides S, Schafer K, Thinnes T, Loskutoff DJ. Plasminogen activator inhibitor-1 and its cofactor vitronectin stabilize arterial thrombi after vascular injury in mice. Circulation 103: 576–583 (2001)
Kotb E. The biotechnological potential of fibrinolytic enzymes in the dissolution of endogenous blood thrombi. Biotechnol. Prog. 30: 656–672 (2014)
Lee JJ, Yang H, Yoo YM, Hong SS, Lee D, Lee HJ, Lee HJ, Myung CS, Choi KC, Jeung EB. Morusinol extracted from Morus alba inhibits arterial thrombosis and modulates platelet activation for the treatment of cardiovascular disease. J. Atheroscler. Thromb. 19: 516–522 (2012)
Majid A, Delanty N, Kantor J. Antiplatelet agents for secondary prevention of ischemic stroke. Ann. Pharmacother. 35: 1241–1247 (2001)
Nieto Estrada VH, Molano Franco D, Medina RD, Gonzalez Garay AG, Martí-Carvajal AJ, Arevalo-Rodriguez I. Interventions for preventing high altitude illness: Part 1. Commonly-used classes of drugs. Cochrane Database Syst. Rev. 6: CD009761 (2017)
Rudolf J, Grond M, Prince WS, Schmülling S, Heiss WD. Evidence of anaphylaxy after alteplase infusion. Stroke 30: 1142–1143 (1999)
Sumi H, Hamada H, Nakanishi K, Hiratani H. Enhancement of the fibrinolytic activity in plasma by oral administration of nattokinase. Acta Haematol. 84: 139–143 (1990)
Sumi H, Hamada H, Tsushima H, Mihara H, Muraki H. A novel fibrinolytic enzyme (nattokinase) in the vegetable cheese Natto; a typical and popular soybean food in the Japanese diet. Experientia 43: 1110–1111 (1987)
Suzuki Y, Kondo K, Matsumoto Y, Zhao BQ, Otsuguro K, Maeda T, Tsukamoto Y, Urano T, Umemura K. Dietary supplementation of fermented soybean, natto, suppresses intimal thickening and modulates the lysis of mural thrombi after endothelial injury in rat femoral artery. Life Sci 73: 1289–1298 (2003)
The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N. Engl. J. Med. 333: 1581–1587 (1995)
Urano T, Ihara H, Umemura K, Suzuki Y, Oike M, Akita S, Tsukamoto Y, Suzuki I, Takada A. The profibrinolytic enzyme subtilisin NAT purified from Bacillus subtilis Cleaves and inactivates plasminogen activator inhibitor type 1. J. Biol. Chem. 276: 24690–24696 (2001)
Xu J, Du M, Yang X, Chen Q, Chen H, Lin DH. Thrombolytic effects in vivo of nattokinase in a carrageenan-induced rat model of thrombosis. Acta Haematol. 132: 247–253 (2014)
Zafren K. Prevention of high altitude illness. Travel Med. Infect. Dis. 12: 29–39 (2014)
Zhang Y, Houng A, Reed G. Synergistic inhibitors halt brain and systemic hemorrhage after tissue plasminogen activator treatment for ischemic stroke. Stroke 44: ATP260 (2013)
Zivin JA. Thrombolytic stroke therapy: past, present, and future. Neurology 53: 14–19 (1999)
Acknowledgements
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science and ICT (2017R1A2A2A05069417).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We certify that there is no conflict of interest in the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guo, H., Ban, YH., Cha, Y. et al. Comparative anti-thrombotic activity and haemorrhagic adverse effect of nattokinase and tissue-type plasminogen activator. Food Sci Biotechnol 28, 1535–1542 (2019). https://doi.org/10.1007/s10068-019-00580-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10068-019-00580-1