Abstract
Objective
This study assesses musculoskeletal ultrasound (MSUS) knowledge, attitudes, and practices among young rheumatologists in Mexico, aiming to identify barriers and facilitators to its clinical use.
Methods
An online survey distributed to a network of young rheumatologists captured demographics, institutional, and personal MSUS information. Multivariable analysis identified factors associated with positive MSUS attitudes.
Results
Ninety-six rheumatologists (39.18% national response rate) completed the survey. Of respondents (54.2% females, median age 35.1 years), 81.2% deemed MSUS necessary in clinical rheumatology. The main barriers included limited training access (56.2%) and required training time (54.1%). Lack of scientific evidence was not a major barrier (60.4%). Positive MSUS attitudes were associated with learning from conferences (p = 0.029) and colleagues (p = 0.005), formal (p = 0.043), and in-person training (p = 0.020), MSUS use in practice (p = 0.027), and use by radiologists in their institute (p < 0.001). Interest in learning MSUS (88.5%) was significantly higher in those with positive attitudes (94.4%, p < 0.001). Elastic net analysis identified key drivers, including learning MSUS from conferences, colleagues, and in residency; using MSUS in practice; respondent-performed MSUS; and MSUS use by radiologists. Statistically significant associations were found with using MSUS for synovitis/inflammatory joint disease (OR = 1.43, 95% CI 1.00–2.05) and MSUS use by radiologists in respondent’s institutes (OR = 1.70, 95% CI 1.20–2.90).
Conclusion
Most young rheumatologists in Mexico recognize the necessity of MSUS in clinical practice. By addressing identified barriers, encouraging rheumatologist-radiologist collaboration, and establishing a regulatory body to certify rheumatologist’s MSUS experience, there is an opportunity to empower them with the necessary skills for effective MSUS use, ultimately benefiting patient care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Musculoskeletal ultrasound (MSUS) has emerged as an indispensable, versatile tool in medical diagnostics, offering a non-invasive, cost-effective, and clinically practical means of diagnosing and managing a wide range of musculoskeletal pathologies [1, 2]. Over the years, MSUS has gained recognition, becoming pivotal for assessing and monitoring patients with rheumatic diseases as per national and international guidelines, including ACR (American College of Rheumatology) [3] and EULAR (European Alliance for Association in Rheumatology) [4, 5] recommendations. Its evolution has been marked by improved image resolution and real-time insights into joints and periarticular structures. This has enhanced precision in guiding essential medical procedures such as joint aspirations, injections, and biopsies [2, 6,7,8,9] as well as diagnosing and monitoring vasculitis [10] and Sjogren’s syndrome [11, 12]. This technological advancement drives the adoption of point-of-care ultrasound (POCUS), crucial for early diagnosis and resource-limited settings.
Ultrasound’s utility has driven progress in MSUS education, targeting residents in rheumatology, radiology, physical medicine and rehabilitation, and physical therapy [13]. The demand for comprehensive training transcends geographic boundaries. Achieving excellence in MSUS education requires regular, cohesive courses, tailored content, varied didactic methods, and standardized practice models [14]. International competency standards and a uniform curriculum, along with ongoing professional development, are crucial for global proficiency in MSUS education. While the significance of MSUS in rheumatology has grown, its integration is especially important in Mexico, where the burden of rheumatic and musculoskeletal disorders (RMDs) is particularly pronounced. Notably, RMDs account for 9.73% of disability-adjusted life years (DALY) among individuals aged 15–49 years in Mexico [15]. This growing burden of disease is exacerbated by the limited availability of certified rheumatologists, with only 0.67 per 100,000 inhabitants, underscoring the urgency of addressing this healthcare challenge [16].
Despite its proven utility, the seamless integration of MSUS into rheumatology practice faces unique challenges. These challenges are primarily due to the shortage of certified rheumatologists, a scarcity of formal MSUS training programs, and the current inactivity of the Mexican School of Musculoskeletal Ultrasound of the Mexican College of Rheumatology (ECOMER) [17, 18]. We highlight limited access to ultrasound education for rheumatologists, which hinders the widespread integration of this invaluable diagnostic tool into rheumatological care in Mexico. These challenges necessitate a comprehensive understanding of the factors influencing the adoption of MSUS among young rheumatologists in Mexico.
Our study focuses on the primary objective of exploring musculoskeletal ultrasound (MSUS) integration among young rheumatologists in Mexico. Our aim is to identify and analyze factors influencing MSUS adoption, emphasizing facilitators and barriers. We strive to comprehend the pace of MSUS education and implementation in this demographic. Secondary objectives include evaluating the impact of introducing MSUS to medical students and residents on acceptance within the medical community. Additionally, we investigate practical MSUS applications in daily rheumatologist routines, highlighting its potential to enhance precision in diagnosis and improve patient outcomes. This work also scrutinizes obstacles impeding seamless integration, from logistical challenges to training issues. Finally, using the insights from experienced countries coupled with respondents’ preferences and results obtained from our research, we propose an approach that could help improve ultrasound education in rheumatology in the country. This multifaceted approach provides a detailed perspective on MSUS integration in Mexico, with broader implications for global healthcare practices.
Materials and methods
Design
We conducted a comprehensive mixed-methods study to gain insights into the awareness, education, and barriers and facilitators to implementing MSUS in clinical rheumatology practice across Mexico. Our research involved a diverse team of experts, including academic medical program directors, epidemiologists, biostatisticians, researchers, and healthcare professionals from Mexico, the United States, Spain, and Switzerland. We developed our Spanish-language questionnaire from an existing validated tool [19] in collaboration with rheumatologists and researchers. The survey featured 70 questions grouped into three main sections: (1) MSUS training, (2) MSUS usage, and (3) attitudes towards MSUS in rheumatology. Questions were presented in various formats, including multiple-choice, check-box, Likert-style (using a 1 to 5 scale for agreement), and open-ended free text comments.
Participants
Our survey targeted young rheumatologists (under 40 years old) and rheumatology residents in Mexico actively engaged in caring for patients with inflammatory RMDs. We distributed the survey through ReumaJoven (a network of young rheumatologists in Mexico), using email and social media channels in a snowball sampling technique. To ensure a robust response rate, our team reached out personally to physicians in different states, encouraging their participation. The data collection ran from February 21 to May 2, 2022, with reminder prompts sent as needed. Ethical approval was not required since the study solely involved anonymous responses from healthcare practitioners and did not involve patients.
Quantitative analyses
Our analysis centers on the relationship between three key dimensions of MSUS attitudes and behaviors in young rheumatologists in Mexico: (1) the need for MSUS in rheumatology practice in Mexico, (2) the use of MSUS by young rheumatologists in clinical practice, and (3) interest in learning MSUS among young rheumatologists in Mexico. Physician characteristics were initially summarized and assessed for association with MSUS attitudes and interest in learning MSUS using analysis of variance (ANOVA) and two sample t-tests for continuous characteristics, and chi-squared and Fisher’s exact tests for categorical characteristics (Table 1, Table S1). All analyses were performed in R V.4.2 [20]. Univariable logistic regression analyses assessed unadjusted associations between physician characteristics and MSUS attitudes.
Due to the extensive number of characteristics captured in the survey, multivariable associations between knowledge, attitudes, and practices and MSUS attitudes were assessed with elastic net regularization and variable selection. To prepare data for elastic net regression, we excluded survey items for which no data was captured and for which there was only one observed response value (uniform). Multiple imputation was performed to address missingness in the remaining data (excluding outcome variables) using the mice R package (v.3.15.0) [21]. K-fold cross-validation was used to determine the optimal lambda value in the glmnet R package (v.4.1–6) [22]. Regression models with elastic net were used to estimate odds ratios along with bootstrapped 95% confidence intervals (CI).
Qualitative analyses
Free text responses to questions about positive and negative MSUS attitudes, MSUS training, and additional comments were analyzed via qualitative content analysis using an inductive approach. This qualitative method involved two investigators (GPMR and AS) who repeatedly reviewed text responses for coding, categorization, and data abstraction. Responses were identified, extracted, and labelled with a code name to reflect the data characteristic (i.e., “need for more training”). Data analysis was conducted with a critical discussion of codes, subcategories, and main categories with the statistical scientist (AS) and input of a clinician (GPMR).
Mixed methods approach
After independent analyses of the quantitative and qualitative data, the results were assessed for the coincidence of coded free-text responses and responses to survey items about advantages, disadvantages, and barriers to MSUS to validate the results. The categories were correlated and those with a positive correlation were presented as coincident.
Results
Participants
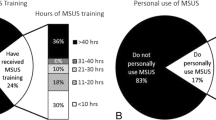
In total, 96 responses (39.18% national response rate; n = 245 Mexican College of Rheumatology members 40 years or younger in 2022) were collected from rheumatologists (residents n = 5, post-residency = 91) in 19 Mexican states (Table 1, Fig. 1, Table S1–2). Forty-seven (48.96%) respondents were concentrated in major urban populations in Mexico (Mexico City n = 29, 30.20%; Monterrey, Nuevo Leon n = 18, 18.75%) and 49 (51.04%) were distributed across 17 other states. Fifty-two (54.17%) respondents were female, with a median age of 35.08 years (interquartile range [IQR] 32.79–37.73 years). Most worked in public hospitals (n = 65, 67.71%) and private practices (n = 80, 83.33%), as residents (n = 5, 5.21%), professors (n = 37, 38.54%), and non-academic clinicians (n = 54, 56.25%).
MSUS attitudes
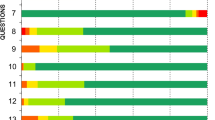
Overall, affordability (n = 63, 65.63%), accessibility (n = 62, 64.58%), and versatility (n = 60, 62.50%) were the most important advantages of MSUS compared with other forms of imaging, while variability in user skills (n = 53, 55.21%) and cost of the device (n = 45, 46.88%) were the most prominent disadvantages (Fig. 2a, b). The most prominent barriers to MSUS were lack of access to training (important or very important n = 54, 56.25%) and training time required (n = 52, 54.17%) (Fig. 2c). Lack of scientific evidence was not an important barrier to MSUS use (unimportant or very unimportant n = 58, 60.42%). Interest in learning MSUS was high (n = 85, 88.54%), with a particular interest in online classes (n = 72, 75.00%), clinical rotations (n = 67, 69.79%), and workshops (n = 58, 60.42%) (Fig. 2d).
Responses to questions about the advantages (a), disadvantages (b), barriers to implementing (c), and interest in learning (d) MSUS among young rheumatologists in Mexico. Responses are presented for the overall sample, as well as stratified by response to the need for MSUS in rheumatology practice in Mexico (positive, MSUS necessary; negative, MSUS not necessary)
Most (n = 78, 81.25%) reported MSUS is necessary in clinical rheumatology practice in Mexico (Table 1, Fig. 1). Respondents from 11 states (n = 19, 19.79%) unanimously reported the need for MSUS. The State of Mexico (n = 6/7, 85.71%), Nuevo Leon (n = 15/18, 83.33%), and Mexico City (n = 23/29, 79.31%) had the next highest rates of agreement with the need for MSUS, while both respondents from Tamaulipas (n = 2, 2.15%) reported MSUS is not needed. Among those with negative attitudes towards MSUS, less importance was placed on MSUS advantages (improved diagnostic acuity, negative n = 6, 33.33% vs. positive MSUS attitudes n = 46, 47.92%) (Fig. 2a, Table S1). Those with negative attitudes expressed more neutrality to MSUS disadvantages and barriers (training time required, negative n = 10, 62.50% vs. positive MSUS attitudes n = 25, 32.47%), and less interest in learning MSUS (negative n = 11, 61.11% vs. positive MSUS attitudes n = 74, 94.87%) (Fig. 2b–d, Table S1).
Quantitative results
Interest in learning MSUS was statistically significantly associated with MSUS use by radiologists in the respondent’s institute (interested n = 43, 50.59% vs. not interested n = 2, 18.18% p = 0.043), institutional availability of CT imaging (interested n = 63, 74.12% vs. not interested n = 4, 36.36% p = 0.016), and the belief that MSUS is or should become a standard tool in rheumatology (interested n = 84, 100.00% vs. not interested n = 9, 81.82% p = 0.012) (Table S1). Interest in learning MSUS (n = 85, 88.54%) was significantly increased in those reporting positive MSUS attitudes (n = 74, 94.49%, p < 0.001). Positive MSUS attitudes were statistically significantly associated with first learning about MSUS from conferences (p = 0.029) and colleagues (p = 0.005), use in the respondent’s practice (p = 0.027), specifically for the diagnosis of synovitis (p < 0.001), and MSUS use by radiologists in the respondent’s institute (p < 0.001) (Table 1).
Univariable analyses supported associations between positive MSUS attitudes and learning about MSUS from conferences (OR = 3.14, 95% CI 1.11–9.46, p = 0.034) and colleagues (OR = 5.03, 95% CI 1.63–19.0, p = 0.008), use in the respondent’s practice (general use OR = 3.66, 95% CI 1.21–11.0, p = 0.020; synovitis OR = 7.58, 95% CI 2.27–34.7, p = 0.003), and MSUS use by radiologists in the respondent’s institute (OR = 9.83, 95% CI 2.57–64.9, p = 0.004). Multivariable analysis using elastic net further identified drivers of positive MSUS attitudes, including learning about MSUS from conferences, colleagues, and in residency; MSUS use in the respondent’s practice, the respondent performing MSUS, and MSUS use for diagnosis or monitoring of synovitis; and MSUS use by radiologists in the respondent’s institute. Use of MSUS for diagnosis or monitoring of synovitis (OR = 1.43, 95% CI 1.00–2.05) and use of MSUS by radiologists in the respondent’s institute (OR = 1.70, 95% CI 1.20–2.90) were significantly associated with positive MSUS attitudes in the final multivariable analysis.
Qualitative results
Qualitative analysis of free text responses identified eight classes of positive MSUS attitudes, five classes of negative MSUS attitudes, four classes of known MSUS training options, and four classes of overall additional comments (Fig. 3). Positive MSUS responses focused on the utility of MSUS, the benefits of point-of-care (POCUS), the objectivity MSUS adds to clinical practice, its ability to assess and quantify disease activity, cost–benefit, the need for more MSUS in pediatric rheumatology practice, the non-harmful and non-invasive nature of MSUS, and its use for research. Negative responses focused on alternative imaging, the cost of the device, limitations associated with training availability and training access, MSUS as an operator-dependent tool, and the limited perceived utility. Known MSUS training included short-form conference courses and workshops, diploma programs, the EULAR certification, and the 1-year fellowship program. Additional comments focused on the need for MSUS to become routine in clinical practice, the need for more training options (with an emphasis on online and hybrid options), the utility of MSUS, and the barrier of lack of access to training opportunities and protected training time required to learn MSUS.
The respondents’ reasons for their positive or negative responses to the need for MSUS in rheumatology practice in Mexico (positive, MSUS necessary; negative, MSUS not necessary), their knowledge of training options, and additional respondent comments and their coincidence with respondent attitudes about the advantages, disadvantages, and barriers to implementing MSUS
Mixed methods results
Positive MSUS responses focusing on utility, objectivity, cost–benefit, the need for MSUS in pediatric rheumatology, and its use for research all notably coincided with the importance of training cost and the lack of access to training opportunities as barriers to the use of MSUS. Further, negative MSUS responses focusing on cost, the lack of access to training opportunities, and the training time required coincided with positive responses about the advantages of MSUS. These barriers may drive negative attitudes towards wider clinical use of MSUS despite clinicians’ awareness of its advantages. Only those reporting awareness of the MSUS fellowship also acknowledged the improved safety and versatility offered by MSUS, suggesting the presence of more established and comprehensive education opportunities may impact clinicians’ understanding of the benefits of MSUS and their consequent interest in implementing MSUS in their clinical practice. Lastly, those responding regarding the need for more training opportunities, with an emphasis on hybrid and online options, coincided with greater importance placed on MSUS advantages and training cost and time as key barriers, suggesting a particular interest in online and hybrid education.
Across quantitative and mixed methods analyses, we identified lack of access to training and training time required as systemic barriers to MSUS implementation. We propose these barriers impact an ecological model of clinical rheumatology practice, institutional resources, knowledge shared in the medical community, and the available scientific evidence (Fig. 4). We found the use of MSUS for diagnosis and monitoring synovitis and inflammatory joint disease in clinical practice, having radiologists who use MSUS in their institute, learning about MSUS from the medical community, and the strong scientific evidence surrounding MSUS all drive positive attitudes and impact motivation to implement MSUS. These results suggest that overcoming systemic barriers can help shift MSUS attitudes to drive improved medical care through wider use of MSUS.
Overview of facilitators and barriers to implementing MSUS in clinical practice. Systemic barriers to MSUS implementation impact the rheumatologist’s experience of their clinical practice, institutional resources, knowledge shared in the medical community, and the available scientific evidence. Notably, the use of MSUS for diagnosis and monitoring synovitis and inflammatory joint disease in clinical practice, having radiologists who use MSUS in their institute, learning about MSUS from the medical community, and the strong scientific evidence surrounding MSUS all drive positive attitudes and impact motivation to implement MSUS
We propose an approach for the integration of evidence-based MSUS education (Fig. 5). It is essential to reach a consensus on ultrasound training and develop a standardized curriculum to ensure the acquisition of essential knowledge by rheumatology residents. This knowledge base would enable young rheumatologists to advance their ultrasound training following residency, exploring more specialized and advanced topics. The establishment of a regulatory body, such as an ultrasound school for rheumatologists, is proposed to certify the rheumatologists’ experience. This regulatory body would consist not only of rheumatologist experts in ultrasound but also of radiologists with experience in MSUS to provide a valuable interdisciplinary perspective. Over a defined period, rheumatologists would have the opportunity to become certified in ultrasound.
Proposed scheme for integration of evidence-based MSUS education available both during (A) and after residency (B). It is essential to reach a consensus on the topics to be integrated into an introductory ultrasound training and develop a standardized curriculum to ensure the acquisition of essential knowledge by rheumatology residents, enabling them to identify normal sonoanatomy and common pathologies that require ultrasound for diagnosis. This knowledge base would enable young rheumatologists to advance their ultrasound training after residency, exploring more specialized and advanced topics. The establishment of a regulatory body, such as an ultrasound school for rheumatologists, is proposed to certify the rheumatologists’ experience. Over a defined period, here proposed as 3 years, rheumatologists would have the opportunity to complete the certification in ultrasound. Flexibility in the certification period would be beneficial to adapt to the diverse circumstances of students, allowing options to accelerate or extend the certification time according to individual needs
Discussion
This work sheds light on the current landscape of MSUS knowledge, attitudes, and practices among young rheumatologists in Mexico. Despite the recognized utility of MSUS in rheumatology, we uncover significant barriers to its widespread adoption in Mexico, particularly among younger practitioners. Our discussion delves into key themes, including the current state of MSUS education, unique challenges faced in Mexico, and impact of international models. Additionally, we explore the implications of our findings for MSUS integration into rheumatological care in Mexico and beyond, as well as propose an approach to overcome limitations and barriers.
Our findings underscore limited access to MSUS education among young rheumatologists in Mexico. Most respondents expressed interest in learning MSUS, but barriers such as a lack of access to training opportunities and the time required for training were identified as significant hurdles. These results align with recent work by Neubauer et al. (2023) [13] and Recker et al. (2023) [23] who identified the common challenge of an expertise bottleneck in MSUS education, in which trained expertise did not always translate to the expert guidance and feedback that is essential to pass on MSUS skills to other clinicians. Additional MSUS education challenges included insufficient ultrasound equipment in courses and insufficient time to practice clinical ultrasound. They suggest the integration of portable ultrasound and the development of more flexible education models, coupled with standardization and MSUS competency assessments, may overcome these challenges. Likewise, a national survey of POCUS integration in American medical schools found similar challenges, with nearly 95% of programs specifically identifying challenges owing to a lack of ultrasound-trained faculty, insufficient time provided for ultrasound training, and lack of equipment [24]. These challenges are common in post-graduate MSUS education as well, evidenced by the recent work by Horowitz et al. (2024) which identified institutional, logistical, and financial challenges as well as the lack of ultrasound expertise among rheumatologists as limiting factors in the implementation of advanced techniques like ultrasound-guided synovial biopsy in the United States [25]. Our results further resonate with international efforts to standardize MSUS education, demonstrated by initiatives in European countries, Canada, and the United States.
In contrast to comprehensive approaches taken in some European countries, the only formal MSUS certification program for rheumatologists in Mexico, to the best of our knowledge and that of respondents, is a limited-access 1-year fellowship at INR (Instituto Nacional de Rehabilitación) in Mexico City [26]. The historical role of ECOMER in introducing MSUS in Mexico is acknowledged, but its current inactivity highlights existing challenges in maintaining consistent and accessible ultrasound education for rheumatologists [17]. Despite over two decades of progress in embedding MSUS knowledge among Mexican rheumatologists, the pace has been slow, with unfulfilled objectives such as incorporating ultrasound training in rheumatology centers across the country [17]. The absence of a dedicated curriculum, lack of MSUS training opportunities during residency, and limited access to post-residency training programs highlight a persistent gap in achieving widespread integration of ultrasound in rheumatology in Mexico. Although awareness of ultrasound’s usefulness has permeated the younger generation of rheumatologists, the crucial task of imparting hands-on skills for independent use during rheumatologists’ residency remains unaccomplished, rendering the inception of MSUS incomplete.
This study draws attention to the influence of international models on MSUS education. Europe has its own MSUS in rheumatology certification through EULAR, consisting of an online introductory course and the basic, intermediate, and advanced in-person courses, which are offered to European and international rheumatologists [27]. If we focus on a local European perspective, two countries, Spain and Switzerland, serve as examples where MSUS training is introduced during residency. In Spain, the Spanish Society of Rheumatology’s Ultrasound School offers courses from the first year of residency, divided into levels (introductory, basic, intermediate, and advanced) available for all residents [28]. Specialized optional training continues during rheumatology specialty, and MSUS is crucial for clinical practice, with a high degree of education satisfaction contributing to the improvement of rheumatologists’ skills [29]. In Switzerland, rheumatologists must learn ultrasound as part of their specialist training[30]. Competencies include attendance of basic, intermediate, and advanced MSUS courses, supervised examinations, and mentoring by Swiss Ultrasound Society (SGUM) tutors. Swiss training involves both SGUM courses with a structured 48-h curriculum, and EULAR courses. A final exam and 400 ultrasound examinations (200 supervised and 200 self-reported) with a balanced distribution on the musculoskeletal system are required for certification [31]. The approach of both countries ensures a comprehensive understanding and practical application of MSUS in rheumatology.
In Canada and the United States, the dawn of ultrasound in rheumatology has begun. In Canada, the expert consensus recommendations for MSUS education in Canadian rheumatology residency training programs [32] in addition to courses offered by CRUS (Canadian Rheumatology Ultrasound Society) [33], and similar efforts in the United States to train rheumatologists through the Ultrasound School of North American Rheumatologists (USSONAR)[34] and satellite courses, as well as the MSUS curriculum [35] and MSUS certification in Rheumatology (RhMSUS) [36] offered by the ACR. These initiatives reflect a global interest in standardizing MSUS education and provide a framework for adapting educational strategies to local contexts.
While these models, international collaboration, and the exchange of expertise are invaluable benchmarks, it is essential to consider unique healthcare landscapes and resource constraints in each country. The collaborative efforts observed in other countries may serve as inspiration for the development of a tailored approach that addresses the specific needs of young rheumatologists in Mexico.
These results highlight the challenges faced by young rheumatologists in Mexico, including limited access to training and the absence of a standardized curriculum. The positive correlation between MSUS attitudes and learning from colleagues, in-person training, and institutional support suggests potential avenues for overcoming challenges. Identification of specific drivers of positive attitudes, such as the use of MSUS for diagnosis or monitoring of inflammatory joint disease and the presence of radiologists using MSUS in respondents’ institutes, provides actionable insights. This underlines the importance of interdisciplinary collaboration and support within healthcare institutions. This can guide the development of targeted interventions to enhance MSUS education and facilitate its integration into routine clinical practice.
While we were analytically limited by sample size, our study captured nearly 40% of our target population across diverse geographies and states, enabling a robust assessment of MSUS in young rheumatologists in Mexico. With an already high response rate, significant sample size increases required to improve generalizability would necessitate increases in the number of young rheumatologists entering the workforce in Mexico. Despite the strong national representation of young rheumatologists in our sample, the nearly unanimous interest in learning MSUS impeded our ability to explore multivariable associations driving this interest. Further, this study did not explore attitudes and practices among older rheumatologists, as our focus was on understanding the next generation of clinicians and their needs as they relate to the future of MSUS in rheumatology in Mexico. Future work should investigate MSUS among both young and older rheumatologists in Mexico as well as in other global contexts. Notwithstanding these limitations, the alignment between our results and recent international work exploring ultrasound education supports the generalizability of our findings both nationally and in the global ultrasound education community.
Our proposal for evidence-based MSUS education
We propose a targeted intervention to overcome these limitations and barriers (Fig. 5). Initially, it is essential to reach a consensus on the topics to be integrated into an introductory ultrasound training during rheumatology specialization. This agreement would determine the breadth of training, whether it be basic, intermediate, and/or encompass advanced aspects. Subsequently, the development of a standardized curriculum is proposed to ensure the acquisition of essential knowledge by rheumatology residents, enabling them to identify normal sonoanatomy and common pathologies that require an ultrasound for diagnosis and distinguish them from their differential diagnoses. This knowledge base would provide rheumatologists with the ability to advance their ultrasound training, exploring more specialized topics through additional courses or certifications.
In addition to the curriculum during residency, the establishment of a regulatory body, such as an ultrasound school for rheumatologists, is proposed to certify the experience of the rheumatologist. Over a defined period, for example, 3 years, rheumatologists would have the opportunity to complete definitive certification in ultrasound. Flexibility in the certification period would be beneficial to adapt to students’ diverse circumstances, allowing options to accelerate or extend certification time according to individual needs. To avoid indefinite extensions, a time limit would be set. This regulatory body would consist not only of rheumatologist experts in ultrasound but also of radiologists with experience in MSUS, acting as tutors and verifying judges, each responsible for a specific group of students. Inclusion of experts in MSUS and radiologists in the planning and execution of the program would provide a valuable interdisciplinary perspective.
Interactions between students and teachers would be structured into in-person modules, such as clinical rotations or practical workshops, and online modules. Our study revealed that, after residency, rheumatologists face difficulties in pursuing an in-person curriculum, generating significant interest in hybrid learning. Therefore, the development of an online platform offering interactive modules and digital resources is crucial. A specific number of musculoskeletal and extra-articular ultrasound scans could be requested, divided into supervised and independent scans, all reviewed and approved by a tutor. This approach would provide rheumatologists with dual learning, combining residency with certification under the regulatory body, strengthening their skills, and offering the option to complete their ultrasound certification during or after their rheumatology specialization program. To ensure education quality, a final in-person exam, supervised by tutors, is proposed as a definitive complement to certification.
This idea could lay the foundation for establishing the “Mexican way” of teaching ultrasound in rheumatology and serve as an example to other healthcare systems worldwide, just as others have served as examples for writing this article.
To the best of our knowledge, this is the first evidence-based study to demonstrate the importance of barriers and limitations of MSUS use among young rheumatologists in Mexico, identify key drivers of its use, and propose an evidence-based model for advanced MSUS education and certification for the new generation of clinicians in a post-pandemic world.
Our study emphasizes a crucial inflection point in the evolution of MSUS in rheumatology. Moving beyond the initial excitement of the utility of MSUS and witnessing its impact, the focus now shifts towards standardization and formal integration into rheumatology education. We emphasize the need for a paradigm shift in MSUS education, moving beyond short and limited courses to a more comprehensive and standardized approach. In line with successful programs around the world, these results support the need for ultrasound education in rheumatology residency training programs in Mexico. Implementing such recommendations in Mexico and similar healthcare settings worldwide could lead to improved diagnostic accuracy and patient care and contribute to the advancement of rheumatological practice.
Conclusions
In conclusion, our study contributes valuable insights into the current state of MSUS education among young rheumatologists in Mexico. Most young rheumatologists recognize the necessity of MSUS in clinical practice, especially those with prior training, practice use, and access to expertise. Enhancing MSUS education, training opportunities, and rheumatologist-radiologist collaboration can address adoption barriers, ultimately improving patient care. By addressing identified barriers and leveraging international models, there is a clear opportunity to enhance MSUS knowledge, attitudes, and practices, empowering young rheumatologists with the skills necessary for effective use of MSUS ultimately benefiting patient care in rheumatological settings. The transformation from sporadic courses to standardized education represents a paradigm shift that holds the promise of reshaping rheumatological practice in the country and beyond, because the findings of this study are not only relevant to Mexico but also offer lessons for other healthcare systems striving to integrate MSUS into routine clinical practice. However, this shift can only be achieved by thorough collaboration.
In the bold pursuit of a brighter future in rheumatology, our study echoes the unwavering spirit of the young rheumatologists of Mexico. Their shared experiences, etched within these findings, propel us towards a future where standardized MSUS education becomes the beacon of progress. The power of us, as rheumatologists, lies in recognizing our strength founded in unity and cooperation, calling upon those with ultrasound expertise to join in this endeavor, for it is through our collective effort that we find progress. Together, we stand on the precipice of a new era, embracing the promise of enhanced patient care and innovation in the noble pursuit of excellence and health.
References
Backhaus M et al (2001) Guidelines for musculoskeletal ultrasound in rheumatology. Ann Rheum Dis 60(7):641–9. https://doi.org/10.1136/ard.60.7.641
Koppikar S, Diaz P, Kaeley GS, Eder L (2023) Seeing is believing: smart use of musculoskeletal ultrasound in rheumatology practice. Best Pract Res: Clin Rheumatol 37(1):101850. https://doi.org/10.1016/j.berh.2023.101850
McAlindon T et al (2012) American College of Rheumatology Report on reasonable use of musculoskeletal ultrasonography in rheumatology clinical practice. Arthritis Care Res (Hoboken) 64(11):1625–40. https://doi.org/10.1002/acr.21836
Möller I et al (2017) The EULAR standardised procedures for ultrasound imaging in rheumatology. Ann Rheum Dis 76(12):2017. https://doi.org/10.1136/annrheumdis-2017-211585
Dejaco C et al (2022) EULAR points to consider for the use of imaging to guide interventional procedures in patients with rheumatic and musculoskeletal diseases (RMDs). Ann Rheum Dis 81(6):760. https://doi.org/10.1136/annrheumdis-2021-221261
G. Tamborrini, C. Dejaco, A. Bruyn, and A. Siegenthaler, Ultrasound and clinically guided Injection techniques on the musculoskeletal system. Books on Demand, 2019
Fukui S et al (2023) Current evidence and practical knowledge for ultrasound-guided procedures in rheumatology: joint aspiration, injection, and other applications. Best Pract Res Clin Rheumatol 37(1):101832. https://doi.org/10.1016/j.berh.2023.101832
Cipolletta E et al (2021) Ultrasound-guided procedures in rheumatology daily practice: feasibility, accuracy, and safety issues. J Clin Rheumatol 27(6):226–31. https://doi.org/10.1097/RHU.0000000000001298
Cazenave T, Pineda C, Reginato AM, Gutierrez M (2015) Ultrasound-guided procedures in rheumatology. What is the evidence? J Clin Rheumatol 21(4):201. https://doi.org/10.1097/RHU.0000000000000242
C. Dejaco et al., 2023 EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice: 2023 update Ann Rheum Dis https://doi.org/10.1136/ard-2023-224543
Jousse-Joulin S et al (2019) Video clip assessment of a salivary gland ultrasound scoring system in Sjögren’s syndrome using consensual definitions: an OMERACT ultrasound working group reliability exercise. Ann Rheum Dis 78(7):967. https://doi.org/10.1136/annrheumdis-2019-215024
Fana V, Dohn UM, Krabbe S, Terslev L (2021) Application of the OMERACT Grey-scale Ultrasound Scoring System for salivary glands in a single-centre cohort of patients with suspected Sjögren’s syndrome. RMD Open 7(2):e001516. https://doi.org/10.1136/rmdopen-2020-001516
Neubauer R, Recker F, Bauer CJ, Brossart P, Schäfer VS (2023) The current situation of musculoskeletal ultrasound education: a systematic literature review. Ultrasound Med Biol 49:6. https://doi.org/10.1016/j.ultrasmedbio.2023.02.008
Tamborrini G, Krebs A, Michel M, Michel BA, Ciurea A (2011) Web-based learning in musculoskeletal ultrasound. Z Rheumatol 70(2):154. https://doi.org/10.1007/s00393-010-0740-z
Global Burden of Disease Collaborative Network, “Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) results.,” Seattle, United States, 2019. Accessed: Jan. 23, 2024. [Online]. Available: https://vizhub.healthdata.org/gbd-results/
Álvarez-Hernández E et al (2023) Distribution and characteristics of the certification of rheumatologists in Mexico. Reumatol Clín (English Edition) 19(7):379–85. https://doi.org/10.1016/j.reumae.2023.04.002
Chávez-López M, Pineda C (2012) Musculoskeletal ultrasound in México 10 years after its inception. Reumatol Clin 8(6):304–5. https://doi.org/10.1016/j.reuma.2012.04.003
Pineda C et al (2008) Ultrasound in rheumatology. The Mexican experience. Clin Exp Rheumatol 26(5):929
Wu M et al (2021) Musculoskeletal ultrasound imaging training, use, and knowledge among rheumatologists in China. Clin Rheumatol 40(1):321–30. https://doi.org/10.1007/s10067-020-05175-4
R Core Team, “R Core Team 2022 R: a language and environment for statistical computing. R foundation for statistical computing. https://www.R-project.org/,” R Foundation for Statistical Computing, vol. 2, 2022.
van Buuren S, Groothuis-Oudshoorn K (2011) Mice: multivariate imputation by chained equations in R. J Stat Softw 45(3):1–67. https://doi.org/10.18637/jss.v045.i03
Friedman J, Hastie T, Tibshirani R (2010) Regularization paths for generalized linear models via coordinate descent. J Stat Softw 33(1):1. https://doi.org/10.18637/jss.v033.i01
Recker F, Schäfer VS, Holzgreve W, Brossart P, Petzinna S (2023) Development and implementation of a comprehensive ultrasound curriculum for medical students: the Bonn internship point-of-care-ultrasound curriculum (BI-POCUS). Front Med (Lausanne) 10:1072326. https://doi.org/10.3389/fmed.2023.1072326
Russell FM, Zakeri B, Herbert A, Ferre RM, Leiser A, Wallach PM (2022) The state of point-of-care ultrasound training in undergraduate medical education: findings from a national survey. Acad Med 97(5):729–7. https://doi.org/10.1097/ACM.0000000000004512
Horowitz DL, Mandelin AM, Tabechian D, Ben-Artzi A (2024) Precision medicine in rheumatology: the promise of ultrasound-guided synovial biopsy, barriers to its implementation in the United States, and proposed solutions. Curr Rheumatol Rep 1–7. https://doi.org/10.1007/s11926-024-01138-9
Instituto Nacional de Rehabilitacion. Secretaría de Salud., “Convocatoria 2024–2025: Posgrado De Alta Especialidad En Medicina De ‘Ecografía En Reumatología,’” https://www.inr.gob.mx/Descargas/Ensena/2024-2025-CPAEM-EcografiaReumatologica.pdf.
EULAR, “EULAR catalog: live courses and meetings,” https://esor.eular.org/totara/catalog/index.php?catalog_cat_browse=75&orderbykey=time&itemstyle=narrow.
Sociedad Española de Reumatología, “Sociedad Española de Reumatología: Material de Escuela de Ecografía,” https://www.ser.es/escuela-de-ecografia/.
Molina Collada J, Mayordomo L (2022) Perceived quality of training in musculoskeletal ultrasound in Spanish rheumatology services. Reumatol Clín 18(6):349–54. https://doi.org/10.1016/j.reumae.2021.01.003
SIWF (Swiss Institute for Further Medical Education and Training), “SIWF FMH ISFM: specialist in rheumatology. Continuing education program.,” https://www.rheuma-net.ch/de/doc/weiterbildungsprogramm-rheumatologie/viewdocument/184.
SGUM SSUM, “SGUM SSUM: continuing education information. General information,” https://www.msus-schweiz.ch/en/continuing-education-information/general-information-42.html.
M. Powell et al., “Expert consensus recommendations for musculoskeletal ultrasound education in Canadian rheumatology residency training programs,” https://acrabstracts.org/abstract/expert-consensus-recommendations-for-musculoskeletal-ultrasound-education-in-canadian-rheumatology-residency-training-programs/.
Canadian Rheumatology Ultrasound Society, “Canadian Rheumatology Ultrasound Society: courses.,” https://crus-surc.ca/courses/
Ultrasound School of North American Rheumatologists, “Ultrasound School of North American Rheumatologists: training program.,” https://www.ussonar.org.
Cannella AC, Kissin EY, and Torralba KD, “2019 Rheumatologic Ultrasound (RhUS) curriculum supplement to the American College of Rheumatology 2015 Core Curriculum Outline,” https://assets.contentstack.io/v3/assets/bltee37abb6b278ab2c/blt457aaaf0d1d7e7a0/rheumatologic-ultrasound-curriculum-supplement.pdf.
American College of Rheumatology, “American College of Rheumatology: RhMSUS certification,” https://rheumatology.org/rhmsus-certification.
Acknowledgements
Profound gratitude is extended to the ReumaJoven network and the Mexican College of Rheumatology, as well as the esteemed Deshire Alpizar-Rodriguez MD-PhD and Panagiotis Ermeidis MD for their invaluable contributions that have significantly enriched the depth and scope of this work.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
Writing of manuscript: GPMR, AS.
Final approval of manuscript: GPMR, AS, MCJ, TG, DSME, SLK, GEMA.
Creation and/or compilation of images and tables: AS, GPMR.
Critical review of manuscript: GPMR, AS, MCJ, TG, DSME, SLK, GEMA.
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
Our study pioneers a comprehensive examination of musculoskeletal ultrasound (MSUS) adoption among young rheumatologists in Mexico, providing a holistic understanding of factors influencing its integration, from driving forces to obstacles.
The study elucidates key drivers linked to positive MSUS attitudes, such as learning from conferences and colleagues, in-person training, practice use, and collaboration with radiologists, offering actionable strategies for fostering a conducive MSUS environment.
By examining international MSUS education models, our research highlights the global drive for standardization, contributing to the discourse about adapting educational strategies to local contexts, ensuring international relevance.
We call for a paradigm shift in MSUS education, advocating for its standardized and formal integration into medical education, thus elevating MSUS from sporadic courses to a cornerstone of rheumatological practice, both in Mexico and comparable healthcare settings worldwide.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Garcia-Pompermayer, M.R., Ayton, S.G., Molina-Collada, J. et al. The power of us: breaking barriers and bridging the gap of ultrasound in rheumatology to empower a new generation. Clin Rheumatol 43, 2103–2116 (2024). https://doi.org/10.1007/s10067-024-06973-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-024-06973-w