Abstract
Objective
To evaluate whether anti-PL7 and anti-PL12 autoantibodies are associated with a greater extent of the fibrotic component of ILD in ASSD patients.
Methods
Patients with ILD-ASSD who were positive for one of the following autoantibodies: anti-Jo1, anti-PL7, anti-PL12, and anti-EJ were included. Clinical manifestations, CPK levels, pulmonary function tests, and HCRT assessments were prospectively collected according to the Goh index. The fibrotic, inflammatory, and overall extension of the Goh index and DLCO were assessed by multiple linear analyses and compared between ASSD antibody subgroups.
Results
Sixty-six patients were included; 17 were positive for anti-Jo1 (26%), 17 for anti-PL7 (26%), 20 for anti-PL12 (30%), and 9 (14%) for anti-EJ. Patients with anti-PL7 and anti-PL12 had a more extensive fibrotic component than anti-Jo1. Anti-PL7 patients had a 7.9% increase in the fibrotic extension (cβ = 7.9; 95% CI 1.863, 13.918), and the strength of the association was not modified after controlling for sex, age, and time of disease evolution (aβ = 7.9; 95% CI 0.677, 15.076) and also was associated with an increase in ILD severity after adjusting for the same variables, denoted by a lower DLCO (aβ = − 4.47; 95% CI − 8.919 to − 0.015).
Conclusions
Anti-PL7-positive ASSD patients had more extensive fibrosis and severe ILD than the anti-Jo1 subgroup. This information is clinically useful and has significant implications for managing these patients, suggesting the need for early consideration of concurrent immunosuppressive and antifibrotic therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Key Points • Patients with antisynthetase syndrome and positivity for anti-PL7 and PL-12 had a greater extension of the fibrotic component than anti-Jo1 patients. • Anti-PL7-positive patients had a greater extension of the fibrotic component and lower DLco, which could confer greater severity of interstitial disease. These suggest the need for prompt consideration of concurrent immunosuppressive and antifibrotic therapy. |
Introduction
Antisynthetase syndrome (ASSD) is a systemic autoimmune disease characterized by autoantibody positivity against aminoacyl-tRNA synthetase (anti-ARS), including anti-Jo1 (anti-histidyl), anti-PL7 (anti-threonyl), anti-PL12 (anti-alanyl), anti-EJ (anti-glycyl), anti-OJ (anti-isoleucyl) and less frequently anti-KS (anti-asparaginyl), anti-Zo (anti-phenylalanyl), anti-YRS/Ha (anti-tyrosyl), anti-SC (anti-lysil), and anti-JS (anti-glutaminyl), among other autoantibodies [1, 2]. Clinical manifestations vary from isolated interstitial lung disease (ILD) [3, 4] to systemic involvement, such as myositis, arthritis, fever, Raynaud’s phenomenon, and mechanic’s hands [4, 5]. ILD is the most frequent manifestation, affecting 69 to 100% of ASSD patients [6, 7], and is considered the main determinant of prognosis and mortality [8]. The most frequent ILD patterns in the ASSD are highly inflammatory [9], such as cellular non-specific interstitial pneumonia (NSIP) with or without organized pneumonia (OP), affecting about 80% of the patients [10]. Nevertheless, about 13% of ASSD patients have ILD patterns with a great extent of the fibrotic component, such as the usual interstitial pneumonia pattern (UIP) [10, 11]. Several studies have emphasized the critical role of antibody subtype in determining the clinical phenotype and survival of patients positive for anti-PL7 and anti-PL12 antibodies, who have shorter survival than those positive for anti-Jo1 antibodies [12, 13]. The exact pathophysiological mechanisms underlying this discrepancy in mortality and clinical manifestations remain unclear. However, the current hypothesis suggests that lung injury induced by environmental factors alters tolerance mechanisms, forming antigenic peptides such as HisRS. This alteration triggers systemic immune activation and the characteristic autoimmune-mediated organ damage, the lung being the organ mainly affected [13, 14]. The specific role of anti-PL7 and anti-PL12 antibodies in this process is not fully understood, highlighting the need to elucidate their involvement in profibrotic processes. So far, the cause of the increased mortality in these patients has not been explained. One possible explanation is a higher severity of ILD, with a higher extent of the fibrotic component. Although it has been described that anti-PL7 and anti-PL12 may have a higher degree of the fibrotic component of ILD [15, 16], a direct comparison of the extent of fibrosis between the different subtypes of anti-ARS has not been performed. With this background as a scenario, this study aims to evaluate whether anti-PL7 and anti-PL12 autoantibodies are associated with a greater extent of the fibrotic component of ILD in ASSD patients.
Patients and methods
This single-center study was conducted at the Rheumatology clinic of the “Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas” (INER) in Mexico City from February 15 to December 21, 2023. This study was approved by the National Institute of Respiratory Diseases ethics and research committee on February 14, 2023, under code C06-23. Patients gave informed consent before enrolling in the study.
We included incident and prevalent consecutive patients 18 years or older, regardless of gender, with a confirmed ILD diagnosis of interstitial lung disease (ILD) by high-resolution computed tomography (HRCT) within 3 months before enrollment and positivity for one of the following autoantibodies: anti-Jo1, anti-PL7, anti-PL12, and anti-EJ. Patients with more than one positive antibody for ASSD were excluded to avoid the confounding factor of the presence of a second ARS antibody between the fibrotic extension and the ARS antibody. Patients were considered ineligible if they had a history of lung surgery, chronic obstructive pulmonary disease, previous radiotherapy, active tuberculosis, or any other condition that could affect the interpretation of pulmonary function tests and HRCT. A single rheumatologist (DR-G) evaluated all patients for relevant clinical manifestations (proximal muscle weakness, Raynaud’s phenomenon, sclerodactyly, mechanic’s hands, and hiker’s feet). Other epidemiological variables were also recorded, such as smoking history, time from the onset of respiratory symptoms to the diagnosis of IPAF and ILD, laboratory results, including creatinine phosphokinase (CPK), and pharmacological treatment. All patients were required to have undergone pulmonary function testing (PFTs) in the 3 months prior to study enrollment. In our institution, patients with ASSD-ILD are treated with the standard of care that includes prednisone (no more than 50 mg/day with tapering) in combination with methotrexate plus leflunomide [11]. In case of therapeutic failure, the treatment is replaced in a case-by-case analysis with rituximab or in combination with mycophenolate.
Measurement of autoantibodies
Anti-ARS antibody subtypes (anti-Jo1, anti-PL7, anti-PL12, and anti-EJ) were detected using immunoblot strips of the EUROLINE: Myositis Profile 3 panel manufactured by EUROIMMUN, based in Lübeck, Germany, following the instructions provided. This commercial strip-based immunoblot assay has been previously validated against the gold standard in a cohort of patients with inflammatory myopathy, showing a remarkable 100% specificity for anti-Jo1 [17]. Furthermore, for the PL7 antibody, this method has demonstrated both a high specificity of 97.2% and a positive likelihood ratio of 25 compared to immunoprecipitation [18].
Respiratory functional tests
All PFTs were performed in the INER’s specialized respiratory physiology laboratory. Each test measured weight and height in a standing position with a Seca model 206 and 769 digital scale. Spirometry was performed to determine FVC and DLCO, both single breathing, with commercial EasyOne Pro and EasyOne Pro Lab equipment (Ndd Medizintechnik AG). Data were expressed in absolute units and as percentages of predicted values. Predicted values for each subject were calculated according to sex, age, and height, and the US National Health and Nutrition Examination Survey (NHANESIII) equations were used (19). The PFTs met the ATS/ERS 2019 acceptability and reproducibility criteria) [19].
Tomographic assessment
HRCT was performed with 1.0-mm or 1.5-mm axial slices at 1-cm intervals and reconstructed using a high spatial frequency algorithm. Twenty to 25 HRCT images were acquired for each patient. This study was evaluated in a blinded manner by an expert (M-M), who has a high interobserver agreement (intraclass correlation coefficient 0.90, 95% CI 0.84–0.94) and who classified the images according to the Idiopathic Pulmonary Fibrosis (an Update) and Progressive Pulmonary Fibrosis in Adults An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline 2022 [20]. The fibrotic component, defined by reticular opacities, traction bronchiectasis, honeycombing, and inflammation, characterized by ground-glass opacities, was classified according to the scores described by Goh [21]
Statistical analysis
Categorical variables were reported with frequencies and percentages, while dimensional variables were reported with mean ± standard deviation (SD) or median and interquartile range (IQR) according to their distribution. The Shapiro-Wilks test was used to determine the distribution of the variables. The chi-square test was used to analyze the independence between the nominal variables. The Kruskal–Wallis test or ANOVA with Bonferroni correction (p = 0.0083) was used to compare the PFTs and the Gogh index between the subgroups according to their distribution; the corresponding post hoc tests were performed (Welch and Dunn’s test) as appropriate. To evaluate risk factors associated with fibrosis, inflammation, the global extent of the Goh index, and DLCO, a crude regression coefficient (cβ) was estimated through simple linear regression analysis. After adjusting for confounders (sex, age, time of disease evolution, and treatment), we used a multiple linear regression analysis to estimate adjusted regression coefficients (aβ). All analyses were two-tailed with a 95% confidence level, and statistical significance was set at p ≤ 0.05 unless required adjustment for multiple comparisons. Stata v. 14.2 was used to perform all statistical analyses.
Results
We included 63 patients with ILD and positive for anti-ARS antibodies; the mean age was 58 ± 10.5 years, and 48 (72.7%) were female. Eighteen (27.2%) patients had a smoking history with a tobacco smoking index of 1.65 (0.5–10.3). Anti-PL12 was the most frequent autoantibody (30.3%), followed by anti-PL7 and anti-Jo1 with 25.7% each. Nintedanib therapy was significantly more frequent in the anti-PL7 subgroup (29.4% vs. 4.35%, OR 9.16, 95% CI 1.24–102). The time from onset of respiratory symptoms to diagnosis of ILD was significantly longer in the anti-PL7 and anti-PL12 subgroups compared to anti-Jo1, with a median of 12 vs. 3 months (Table 1). Anti-Jo1-positive patients had more significant muscle weakness (47%, p = 0.029) than the other subgroups. In addition, significantly higher CPK levels were observed in anti-Jo1 (74.0 [59 to 116], p = 0.029, Table 1). In both anti-Jo1 and non-Jo1 groups of patients, NSIP and OP inflammatory patterns were the most frequent HCRT patterns (Table 2).
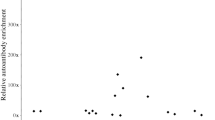
The extent of lung disease
We found a significant difference in the extent of fibrosis in HRCT according to the antibody subgroup (Fig. 1, Kruskal–Wallis, p = 0.026). Patients who were positive for anti-PL7 and anti-PL12 had more extensive fibrotic components than anti-Jo1 patients (Dunn’s test p = 0.0013 and p = 0.0254, respectively, Table 2). The greater extent for anti-PL7-positive patients compared to anti-Jo1 patients was confirmed after adjusting for confounding (age, sex, antibody subtype, and disease duration) using multivariable linear regression analysis: the anti-PL7 patients had aβ = 23.01 for the overall extent (95% IC 2.525 to 29.684) and aβ = 7.90 for the fibrotic component (95% IC 1.863 to 13.918). The multivariate linear regression analysis did not confirm this association between anti-PL12 and the extent of fibrosis (Table 3). Additionally, a third model was performed where treatment was considered a confounding variable, identifying an association between methotrexate and decreased fibrotic extension by Goh: aβ = − 10.89 (95% IC − 18.34 to − 3.4498). No statistically significant effect on the extension of the fibrotic component was observed when other treatment schedules were included.
The fibrotic component is according to the antibody subtype in antisynthetase syndrome. The boxplot’s lower side represents the first quartile; the line in the middle represents the median, and the box’s upper side represents the third quartile. The lower whisker shows the minimum data value, and the upper whisker shows the maximum. Statistically different concerning anti-Jo1 with a *p < 0.05 or **p < 0.01, by Kruskal–Wallis followed by Dunn’s test
Pulmonary function tests
A tendency for decreased lung function was observed in the non-Jo1 subgroups, especially in anti-PL7, which showed the most pronounced reduction in DLCO (Table 2). After adjusting (time from respiratory symptoms to ILD diagnosis, age, sex, and antibody subtype) in multivariable linear regression analysis, we found an association between anti-PL7 and lower DLCO: aβ = − 4.467 95% IC (− 8.919 to − 0.015) (Table 3).
Discussion
The main finding of this study was that anti-PL7-positive patients with ASSD have a greater fibrotic and global extent of ILD on HRCT assessment; this greater extent is mirrored in the severity of interstitial lung disease: anti-PL7 had lower DLCO than anti-Jo1 patients. These findings are clinically relevant in assessing and treating ASSD patients and may explain the previous observations that PL7 patients have worse prognoses when compared to anti-Jo1 patients.
Several studies have reported that patients with anti-PL7 and anti-PL12 have shorter survival and more severe lung disease than anti-Jo1 patients [12, 16, 22]. This observation is intriguing, partly because many patients with ASSD respond well to medical treatment [11, 23]. Two possible mechanisms may explain why this subgroup of patients with anti-PL7 and anti-PL12 has the worst survival: first, they have a lower prevalence of musculoskeletal involvement [16], which could delay diagnosis and medical management; secondly, it has been reported that they may have more fibrotic component of ILD [15, 22], and therefore a poor response to initial immunosuppressive therapy. The results of this study support the second hypothesis. After adjusting for possible confounders (age, sex, antibody subtype, treatment, and mainly time of evolution of the disease), the strength of the association between anti-PL7 and the extent of the fibrotic component was maintained.
From a biological perspective, it should be noted that patients with anti-PL7/PL12 antibodies may have distinct pathophysiological bases that differentiate them from those positive to anti-Jo1. Some research has revealed the relationship between the progression of ASSD-ILD and an elevated proinflammatory TH17 profile. In addition, evidence points to a predominant profile of proinflammatory M2 macrophages with high levels of soluble SCD163 protein [24, 25]. The next crucial step is investigating whether these proinflammatory and profibrotic pathways influence the increased fibrotic component observed in anti-PL7 and anti-PL12 antibody-positive patients.
Our study and others support that anti-PL7 and anti-PL12 are associated with a more fibrotic component of ILD when compared to anti-Jo1 ILD patients; for example, the ASSD-ILD cohort showed that fibrotic patterns were present in 20% of the anti-PL7 subgroup and 50% of the anti-PL12 subgroup at baseline. Remarkably, at the end of the follow-up period, 100% of these subgroups progressed to fibrotic patterns; in contrast, the anti-Jo1 subgroup was only 67.7% [26]. Our study differs concerning what was reported in the ASSD-ILD cohort. We did not find a difference in the prevalence of fibrotic patterns as UIP between antibody subtypes. Nevertheless, the difference was evident when we analyzed the overall extent and the fibrotic component of the Goh index. These data suggest that despite variations due to different methodologies, both studies agree that patients with anti-PL7 have a more extensive degree of pulmonary fibrosis.
Identifying patients with anti-PL7 autoantibodies and a greater extent of the fibrotic component, as demonstrated in our study, has significant clinical implications, especially given the irreversible nature of fibrosis and its poor response to immunosuppressive therapy. In the González-Pérez cohort, 24% of patients with ASSD-ILD developed progressive fibrosing phenotype (PFP), highlighting the importance of early recognition of these patients for timely treatment leading to reduced mortality [11]. The recent use of antifibrotic therapies, capable of reducing the annual rate of FVC decline [27], underscores the importance of our findings; timely administration of antifibrotic interventions is promising for this specific subgroup. However, controlled clinical trials are essential to standardize and validate this therapeutic approach.
Our study is not exempt from limitations. First, the sample size is relatively small, which may explain why we have not detected differences in certain variables of interest, such as patients with anti-PL12 and the fibrotic extension in our linear regression analysis. In addition, the small sample size restricted our ability to simultaneously include a larger number of variables in the multivariate models. Another significant limitation is that our institution is a nationwide referral center for patients with pulmonary conditions. Therefore, patients referred to our center may not necessarily represent the broader population of patients evaluated elsewhere. Despite these limitations, our results are of utmost importance, considering the low prevalence of the disease. A considerable number of non-Jo1 patients were recruited. Furthermore, these results may explain why PL7 patients have a worse prognosis than the other anti-ARS subgroups.
In conclusion, our study revealed that anti-PL7-positive ASSD patients had more extensive fibrosis and severe ILD than the anti-Jo1 subgroup. These findings have significant implications for managing these patients, suggesting the need for timely consideration of concurrent immunosuppressive and antifibrotic therapy.
Data availability
Data are available on reasonable request. The data supporting this study’s findings are available from the corresponding author upon reasonable request.
References
Galindo-Feria AS, Notarnicola A, Lundberg IE, Horuluoglu B (2022) Aminoacyl-tRNA synthetases: on anti-synthetase syndrome and beyond. Front Immunol 13. https://doi.org/10.3389/FIMMU.2022.866087
Ghirardello A, Doria A (2018) New insights in myositis-specific autoantibodies. Curr Opin Rheumatol 30:614–622. https://doi.org/10.1097/BOR.0000000000000548
Betteridge Z, Tansley S, Shaddick G, et al (2019) Frequency, mutual exclusivity and clinical associations of myositis autoantibodies in a combined European cohort of idiopathic inflammatory myopathy patients. J Autoimmun 101. https://doi.org/10.1016/j.jaut.2019.04.001.
Cavagna L, Trallero-Araguás E, Meloni F, et al (2019) Influence of antisynthetase antibodies specificities on antisynthetase syndrome clinical spectrum time course. J Clin Med 8: https://doi.org/10.3390/JCM8112013
Opinc AH, Makowska JS (2021) Antisynthetase syndrome – much more than just a myopathy. Semin Arthritis Rheum 51:72–83. https://doi.org/10.1016/J.SEMARTHRIT.2020.09.020
Marco JL, Collins BF (2020) Clinical manifestations and treatment of antisynthetase syndrome. Best Pract Res Clin Rheumatol 34:101503. https://doi.org/10.1016/J.BERH.2020.101503
Lilleker JB, Vencovsky J, Wang G et al (2018) Extended report: the EuroMyositis registry: an international collaborative tool to facilitate myositis research. Ann Rheum Dis 77:30. https://doi.org/10.1136/ANNRHEUMDIS-2017-211868
Sawal N, Mukhopadhyay S, Rayancha S et al (2021) A narrative review of interstitial lung disease in anti-synthetase syndrome: a clinical approach. J Thorac Dis 13:5556–5571. https://doi.org/10.21037/JTD-20-3328
Mima M, Sato S, Shinya T et al (2024) Characteristics of chest high-resolution computed tomography in patients with anti-aminoacyl-tRNA synthetase antibody-positive interstitial lung disease. Sarcoidosis Vasc Diffuse Lung Dis 41:2024005. https://doi.org/10.36141/svdld.v41i1.14144
Maturu VN, Lakshman A, Bal A, et al (2016) Antisynthetase syndrome: an under-recognized cause of interstitial lung disease. Lung India 33. https://doi.org/10.4103/0970-2113.173055
González-Pérez MI, Mejía-Hurtado JG, Pérez-Román DI et al (2020) Evolution of pulmonary function in a cohort of patients with interstitial lung disease and positive for antisynthetase antibodies. J Rheumatol 47:415–423. https://doi.org/10.3899/JRHEUM.181141
Aggarwal R, Cassidy E, Fertig N et al (2014) Patients with non-Jo-1 anti-tRNA-synthetase autoantibodies have worse survival than Jo-1 positive patients. Ann Rheum Dis 73:227. https://doi.org/10.1136/ANNRHEUMDIS-2012-201800
Fu H, Zheng Z, Zhang Z et al (2023) Prediction of progressive pulmonary fibrosis in patients with anti-synthetase syndrome-associated interstitial lung disease. Clin Rheumatol 3:1917–1929. https://doi.org/10.1007/s10067-023-06570-3
Gallay L, Gayed C, Hervier B (2018) Antisynthetase syndrome pathogenesis: knowledge and uncertainties. Curr Opin Rheumatol 2018; 30(6). https://doi.org/10.1097/BOR.0000000000000555
Marie I, Josse S, Decaux O, et al (2012) Comparison of long-term outcome between anti-Jo1- and anti-PL7/PL12 positive patients with antisynthetase syndrome. Autoimmun Rev. 2012;11(10). https://doi.org/10.1016/j.autrev.2012.01.006
Pinal-Fernandez I, Casal-Dominguez M, Huapaya JA et al (2017) A longitudinal cohort study of the anti-synthetase syndrome: increased severity of interstitial lung disease in black patients and patients with anti-PL7 and anti-PL12 autoantibodies Rheumatology key messages. Rheumatology 56:999–1007. https://doi.org/10.1093/rheumatology/kex021
Ghirardello A, Rampudda M, Ekholm L et al (2010) Diagnostic performance and validation of autoantibody testing in myositis by a commercial line blot assay. Rheumatology (Oxford) 49:2370–2374. https://doi.org/10.1093/RHEUMATOLOGY/KEQ281
Loganathan A, Zanframundo G, Faghihi-Kashani S, et al (2024) Agreement between local and central anti-synthetase antibodies detection: results from the classification criteria of anti-synthetase syndrome project biobank. Clin Exp Rheumatol. https://doi.org/10.55563/clinexprheumatol/s14zq8
Graham BL, Steenbruggen I, Barjaktarevic IZ et al (2019) (2019) Standardization of spirometry 2019 update. An official American Thoracic Society and European Respiratory Society technical statement. Am J Respir Crit Care Med 200(8):E70–E88. https://doi.org/10.1164/rccm.201908-1590st
Rodriguez K, Ashby CL, Varela VR, Sharma A (2022) High-resolution computed tomography of fibrotic interstitial lung disease. Semin Respir Crit Care Med 43:764–779. https://doi.org/10.1055/s-0042-1755563
Ns G Sr, D, S V, et al (2008) Interstitial lung disease in systemic sclerosis: a simple staging system. Am J Respir Crit Care Med 177:57–59. https://doi.org/10.1164/RCCM.200706-877OC
Hervier B, Devilliers H, Stanciu R, et al (2012) Hierarchical cluster and survival analyses of antisynthetase syndrome: phenotype and outcome are correlated with anti-tRNA synthetase antibody specificity. Autoimmun Rev. 2012;12(2). https://doi.org/10.1016/j.autrev.2012.06.006
Trallero-Araguás E, Grau-Junyent JM, Labirua-Iturburu A et al (2016) Clinical manifestations and long-term outcome of anti-Jo1 antisynthetase patients in a large cohort of Spanish patients from the GEAS-IIM group. Semin Arthritis Rheum 46:225–231. https://doi.org/10.1016/J.SEMARTHRIT.2016.03.011
Ramos-Martinez E, Falfán-Valencia R, Pérez-Rubio G, et al (2020) Anti-aminoacyl transfer-rna-synthetases (anti-trna) autoantibodies associated with interstitial lung disease: pulmonary disease progression has a persistent elevation of the th17 cytokine profile. J Clin Med 9. https://doi.org/10.3390/jcm9051356
Ramos-Martínez E, Falfán-Valencia R, Pérez-Rubio G et al (2022) Interstitial lung disease progression in patients with anti-aminoacyl transfer-RNA-synthetase autoantibodies is characterized by higher levels of sCD163. Immunol Lett 248:56–61. https://doi.org/10.1016/J.IMLET.2022.06.007
Wu W, Collins BF, Gardner GC et al (2023) Antisynthetase syndrome-related interstitial lung disease (ASyS-ILD): longitudinal imaging findings. Eur Radiol 33:4746–4757. https://doi.org/10.1007/S00330-023-09439-W
Wells AU, Flaherty KR, Brown KK, et al (2020) Nintedanib in patients with progressive fibrosing interstitial lung diseases—subgroup analyses by interstitial lung disease diagnosis in the INBUILD trial: a randomised, double-blind, placebo-controlled, parallel-group trial. Lancet Respir Med 8. https://doi.org/10.1016/S2213-2600(20)30036-9
Acknowledgements
All authors acknowledge the Instituto Nacional de Enfermedades Respiratorias (INER) clinical laboratory in Mexico City for the immunoblot assays and laboratory analysis. We also thank all the patients in the study and all the research assistants who collaborated in patient recruitment.
Author information
Authors and Affiliations
Contributions
J.R-S and D.R-G designed this study. They later participated in patient recruitment, conceptualization, methodology, validation, formal analysis, research, writing, and original draft preparation. M. M participated in conceptualization, drafting-revising, final approval of the final version, methodology, and validation. H.I.R-G, J.C.H-C, R.F-V, and E. R-M participated in study conceptualization, design, methodology, drafting-revising, and editing of the final version. H.N.M-T, M.F.C-L, Y.K.R-T, and V.L-B participated in the data acquisition, drafting the word, research, and resources. J.R-S participated in conceptualization, methodology, writing revision, editing and supervision, and project management. All authors reviewed, edited, and approved the manuscript in its final form and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethical approval
This study involved human subjects and was approved by the National Institute of Respiratory Diseases ethics and research committee on February 14, 2023, with code C06-23. Patients gave informed consent before enrolling in the study.
Disclosures
None.
Additional information
Published congress abstract
Preliminary results of the research were presented at the GCOM Congress of Myopathies in March 2024 https://doi.org/10.55563/clinexprheumatol/byxxv1.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rivero-Gallegos, D., Mejía, M., Rocha-González, H.I. et al. Association between anti-PL7 antibodies and increased fibrotic component in patients with antisynthetase syndrome and interstitial lung disease: a cross-sectional study. Clin Rheumatol 43, 1971–1978 (2024). https://doi.org/10.1007/s10067-024-06965-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-024-06965-w