Abstract
Objectives
The aim of this study was to investigate the relation among atherosclerosis, antibodies against oxidized LDL (anti-oxLDL), and inflammation in rheumatoid arthritis (RA) patients treated with biological (b) disease-modifying anti-rheumatic drugs (DMARDs).
Methods
Fifty-nine patients who were receiving conventional synthetic DMARDs and were eligible for treatment with a biological agent were included in the study. Total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and IgG antibodies against oxidized LDL (anti-oxLDL) as well as carotid intima-media thickness (cIMT) were determined before and after 6 months of treatment. Thirty-one healthy individuals were used as a control group.
Results
At baseline, RA patients had lower TC and HDL-C levels and increased cIMT compared to controls. After a 6-month follow-up, the re-evaluation of carotids revealed a statistically important decrease of cIMT values. This observation was accompanied by a statistically important elevation of HDL-C levels and a reduction of the titer of anti-oxLDL antibodies regardless of the bDMARD that was administered. No statistically significant association was found between the cIMT and anti-oxLDL, HDL-C, CRP, or DAS28 score neither before nor 6 months after treatment using linear regression analyses adjusted for age and gender.
Conclusions
We provide evidence that atherogenic lipid profile and ongoing atherosclerosis which characterize RA patients appear to improve after biological therapy, and we also suggest a possible atherogenic effect of IgG anti-ox LDL antibodies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory disease which affects the synovial membrane causing joint damage and physical dysfunction [1]. Patients with RA suffer cardiovascular (CV) complications 1.5–2 fold than the general population [2]. Atherosclerosis constitutes an abnormal thickening of arterial walls as a result of endothelial layer dysfunction. Nowadays, it is considered a chronic inflammatory disease, as inflammation molecules and pathways play a significant role in all stages of the atherosclerotic process [3].
Oxidized LDL (oxLDL) plays a central role in the pathogenesis of atherosclerosis, promoting the activation of endothelial cells [4, 5]. Increased lipid oxidation has been described during inflammation, and oxLDL has been detected in the synovial membrane and synovial fluid of patients with RA [6,7,8,9]. Also, it has been reported that patients with RA and active disease had significantly increased serum oxLDL levels compared to patients without active disease [10]. Some studies have conflicting results questioning the pathogenic role of oxLDL in the development of CV disease in these patients, but most have confirmed that oxLDL is increased in RA [11, 12]. Many studies have tried to fill gaps in knowledge concerning the role of autoantigens and their associated autoantibodies in the development of atherosclerosis. In the case of autoantibodies against oxidized LDL (anti-oxLDL), data are ambiguous. Several studies have shown an atheroprotective effect of anti-oxLDL antibodies, while others are not in accordance with these results [13]. Indeed, various investigators assessed the association of IgM and IgG anti-oxLDL antibodies and cardiovascular events in subjects without CV disease. They found that IgM anti-oxLDL antibodies appear to have a protective effect for several CV events [14, 15], while the relationship of IgG anti-oxLDL is more complex and needs further investigation [13, 16].
In patients with RA, the association between lipid levels and CV events is less proportional than in the general population (lipid paradox in RA) [17]. In the present study, we investigated the impact of biological (b) disease-modifying anti-rheumatic drugs (DMARDs) on subclinical atherosclerosis in RA. Changes in the titer of anti-oxLDL antibodies after bDMARD initiation were also evaluated, and we tried to provide evidence regarding their general implication in the atherosclerotic process. An additional aim of our study was to determine possible relations among anti-oxLDL antibodies, inflammation, and atherosclerosis.
Methods
Study design and patients
This is a prospective controlled study conducted in a single University Centre between June 2016 and November 2020. During this time period, 753 RA patients visited the Rheumatology Department of the University Hospital of Ioannina, Greece. Among them, 70 patients met the inclusion criteria and were enrolled in the study.
Patients with no previous history of CV disease, eligible for the study, were those aged 18–65 years old, fulfilling the 2010 American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) classification criteria for RA [18]. They were receiving conventional synthetic (cs) DMARDs, such as methotrexate (MTX) or leflunomide (LFN). Biologic agents were administered in these patients after being carefully evaluated and screened appropriately [19, 20]. Exclusion criteria were the following: age above 65 years, established or familiar history of coronary artery disease, history of smoking, valvular heart defects, chronic infectious diseases, thyroid gland disorders, diabetes mellitus, neoplasms, chronic renal failure, hypertension, dyslipidemia of any type and metabolic syndrome, and patients that received any agent that can influence the lipid profile such as statins, diuretics, thyroid drugs, and others.
Thirty-one apparently healthy, non-smoking volunteers, with no previous history of CV disease, participated in the study and were used as a control group. These subjects were randomly selected during their routine medical check-up tests, the last 3 months of the patients’ selection period, and fulfilled the same exclusion criteria reported for the patient group. A written informed consent form was signed by all patients, and the study protocol was approved by the institutional ethics committee.
Clinical assessment
RA patients underwent a complete physical examination at baseline and after 6 months of bDMARD initiation. Age, gender, body mass index (BMI), disease activity score for 28-joint count indices based on C-reactive protein values (DAS28-CRP), and extra-articular manifestations of RA were recorded.
Laboratory monitoring
Blood samples were obtained at baseline and after 6 months of bDMARD initiation. Total cholesterol (TC), triglycerides (TG), and high-density lipoprotein cholesterol (HDL-C) were determined by a clinical chemistry analyzer. Low-density lipoprotein cholesterol (LDL-C) levels were calculated using the Friedewald formula, while CRP was measured by nephelometry. Erythrocyte sedimentation rate (ESR) was measured by an automatic analyzer. IgM rheumatoid factor (IgM RF) was measured by latex test. Concentrations of anti-citrullinated protein/peptide antibodies (ACPAs) were determined by immune enzyme analysis (ELISA).
Determination of antibody titer against oxLDL
ELISA sandwich
Serum of patients was incubated on ELISA plates containing immobilized antigen which in this case was oxidized LDL (oxLDL) after ultracentrifugation from pooled fresh plasma of normolipidemic volunteers. The unbound antibody was removed by multiple rinsing. Then, incubation was performed with HRP-conjugated rabbit anti-human IgG monoclonal antibody (Dako Cytomation) (diluted 1:1000, v/v). Excess of the secondary antibody was removed by successive rinsing, and the antigen complex with the antibodies remained immobilized on the ELISA plate—color development followed by the addition of hydrogen peroxide and chromophore (o-phenylene diamine) as substrates [21]. The previous reaction was stopped by the addition of hydrochloric acid. The results of anti-oxLDL titers are expressed as optical density (OD) values. All measurements were performed at 492 nm, in a multifunctional microplate reader (InfiniteM 200 Pro, Tecan, Italy), before and after 6 months of biological treatment initiation.
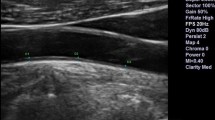
Subclinical atherosclerosis evaluation
For the evaluation of the carotid intima-media thickness (cIMT), we used a GE Healthcare LOGIQ E9 ultrasound machine, equipped with a GE 9L Linear Array Probe with a maximum frequency of 10 MHz. All the measurements were performed by a single observer unaware of the participants’ clinical or laboratory characteristics. Patients were examined in a supine position with the neck extended. The distance between the lumen-intima interface and the leading edge of the media-adventitia interface of the far wall corresponds with cIMT. The measurement of cIMT was always performed at the same location in the same common carotid artery, proximal to the carotid bifurcation, both at baseline and at 6 months. Values were expressed in millimeters [19].
Statistical analysis
Statistical analysis was performed using SPSS Statistics, version 21.0. Data are expressed as mean (SD) or median (IQR) as appropriate. Variable distribution was tested for normality. Comparisons between groups were made with the chi-square test for categorical variables and the independent sample t-test or the Mann–Whitney U test for continuous variables. Changes over time were analyzed with the paired sample t-test or the non-parametric alternative Wilcoxon signed-ranks test. All tests were 2-sided and the significance level was set at 0.05.
Linear regression analyses adjusted for age and sex were performed to estimate the association between cIMT and anti-oxLDL, HDL-C, ESR, and CRP before and 6 months after the administration of biological agents and to calculate effect estimates (betas, 95% confidence intervals). Results were considered statistically significant if the p-value was < 0.05. Linear regression analyses were performed using Stata (version 13.1; StataCorp, College Station, TX, USA).
Results
Among the 70 RA patients who initially fulfilled the enrollment criteria, 11 were excluded. Five refused to receive any biological treatment, 3 had positive hepatitis B surface antigen, 2 had an abnormal chest x-ray, and one was positive for hepatitis C virus. Patient demographic data, baseline clinical characteristics, immunological profile, and their comparison with controls are presented in Table 1. The majority of patients were women, and mean age was 53.9 years with a mean disease duration of 2.8 years. The extra-articular manifestations included rheumatoid nodules in 6 patients, anemia of chronic disease in 5 patients, secondary Sjogren syndrome in 2 patients, and Raynaud phenomenon in 2 patients. All patients received csDMARDs, MTX 50 (84.6%), and LFN 9 (15.4%), while 35 received tumor necrosis factor a (TNFa) inhibitors, and 24 received non-anti-TNFa therapy. More specifically, among TNFa inhibitor users, 12 patients received adalimumab, 10 infliximab, 7 etanercept, and 6 golimumab. On the other hand, among non-anti-TNFa users, 15 patients received tocilizumab, an interleukin-6 receptor antagonist, while 9 were treated with abatacept, a T-cell modulatory agent. The choice of bDMARD therapy was based on a shared decision between patients and doctors, following the EULAR recommendations for RA management [22]. Patients presented with statistically significant lower TC and HDL-C levels and a statistically significant elevation of cIMT levels at baseline, compared with controls (Table 1).
After a six-month follow-up, the re-evaluation of carotids revealed a statistically important decrease of cIMT values. This observation was accompanied by a statistically significant elevation of HDL-C levels and a reduction of the titer of anti-oxLDL antibodies regardless of the bDMARD that was administered (Table 2). There was also a clinical improvement, and the reduction of the DAS28-CRP score reflects a low disease activity (Table 2). A comparative analysis of parameters and change of parameters was also performed between the anti-TNF group and the group of patients who did not receive anti-TNF at baseline and after 6 months of treatment, respectively. Based on the results in Table 3, the two groups did not show a statistically significant difference regarding the parameters at baseline and their change over a 6-month follow-up.
No statistically significant association was found between the cIMT and anti-oxLDL, HDL-C, CRP, or DAS28-CRP neither before nor 6 months after the administration of biological agents. Moreover, the change of cIMT within 6 months of the bDMARD administration was not correlated with the changes in anti-oxLDL, HDL-C, or CRP respectively (Table 4).
Discussion
In our study, RA patients who presented with significant subclinical atherosclerosis and high titer of anti-oxLDL antibodies at baseline ended up with favorable outcomes concerning their CV risk as there was a reduction of anti-oxLDL antibody titer and cIMT values after 6 months of bDMARD initiation. No statistically significant correlation was revealed between the cIMT and anti-oxLDL, HDL-C, or CRP neither before nor 6 months after the administration of biological agents.
Elevated HDL-C levels were also observed, even from the first 6 months of therapy. Several studies have focused on examining other CV risk factors and in particular HDL-C function. The increase in TC and LDL-C after suppression of inflammation was accompanied by a HDL-C increase, which protects from CV disease [23, 24]. In addition, there is evidence that anti-atherogenic properties of HDL-C appeared to improve when inflammation is reduced [25, 26]. Quantitative as well as qualitative lipid changes are important in the assessment of the atherosclerotic process. HDL-C particles contain, among others, apolipoprotein A1, whose main role is to prevent the oxidation of LDL-C and as a consequence to inhibit one of the first steps of atherosclerosis [25].
Anti-oxLDL antibodies are associated with atherosclerosis in the general population and have been reported in several autoimmune diseases. In a previous study, their concentrations were measured in the serum of 140 patients with RA. The analysis revealed a positive correlation with CRP and a negative correlation with HDL-C. An independent positive correlation was also found with cIMT [7]. In another study, their titer was found to be high in patients with early RA, and a reduction was observed after csDMARD administration and subsequent control of inflammation [27]. In the present study, no correlation was found between cIMT and anti-oxLDL. These contradictory findings suggest that the role of the humoral immune response to oxLDL is unclear, and the antibody formation may serve a different purpose through the various stages of atherosclerosis.
The mechanism by which anti-oxLDL antibodies participate in the pathogenesis of atherosclerosis is not certain. A logical theory is that the reduction of their titer reflects the reduction of their substrate, oxLDL, which plays a central role in the whole atherogenic process. However, there is another theory that potentially places oxLDL among the most potent epitopes. The term oxLDL refers to a set of heterogeneous oxidative changes in LDL-C subunits and ApoB (apolipoprotein B). These changes include reorganization of the phospholipid shell upon exposure of phosphorylcholine (PC) and binding of aldehydes, such as malondialdehyde (MDA), to ApoB. Oxidized phospholipids derived from oxLDL and LDL-C can promote inflammatory activation of macrophages, vascular smooth muscle cells, and other cells, acting as damage-associated molecular patterns (DAMPs). DAMPs are endogenous molecules released by cells that are damaged or shed and activate the immune system [28, 29].
Measurement of titer of anti-oxLDL antibodies may also contribute to stratification of CV risk. Nevertheless, the role of anti-oxLDL antibodies in the atherosclerotic process remains controversial. A systematic review by van den Berg et al. has highlighted that IgM anti-oxLDL antibodies appear to be protective against severe coronary artery disease and cardiovascular events, while the relationship with IgG anti-oxLDL antibodies is complex enough and difficult to elucidate [13]. More specifically, a study by Tsimikas et al. found higher serum levels of IgM oxLDL antibodies which were associated with a lower risk of developing CV endpoints [14]. van den Berg et al. also found a strong protective effect of IgM anti-MDA-LDL antibodies on future CV disease development [15]. However, other studies did not discover a significant association between IgM anti-MDA-LDL antibodies and future CV events [30, 31]. Another study by Khamis et al. found a protective association between IgG anti-oxLDL antibodies and cardiovascular endpoints with cases having lower levels of IgG anti-oxLDL than controls [16]. However, the IgG class of autoantibodies is mostly pathogenic in many autoimmune rheumatic diseases like systemic lupus erythematosus, antiphospholipid syndrome, and others [32, 33]. Despite the paucity of studies that lack definite conclusive data as regards the role of oxLDL antibodies and CV events, it seems that IgM anti-oxLDL antibodies have a protective effect for severe CV events, while the relationship of IgG-oxLDL is more complex and needs further investigation [13].
The biological role of these autoantibodies requires further evaluation, as new evidence supports the notion that they constitute not only a simple biomarker of atherosclerosis but also a key component of the innate immune system. IgM anti-oxLDL antibodies perform homeostatic functions, maintaining the equilibrium of atherosclerosis development. Perhaps in the presence of overwhelming stimuli, such as traditional CV risk factors or other inflammatory triggers, a maladaptive immune response occurs with immunoglobulin class switching to IgG and leading to accelerated atheroma deposition or plaque rupture [28, 34, 35].
Our study provides evidence concerning the implication of IgG anti-oxLDL antibodies in atherosclerosis of RA patients treated with bDMARDs. The results of the present study suggest their potential atherogenic action as the reduction of their titer after treatment was accompanied by reduced cIMT values, even if no correlation was revealed between them, probably due to a type II error. Imaging modalities and especially non-invasive carotid ultrasound are very useful in depicting atherosclerotic plaques [36]. Carotid plaques and cIMT have been reported in several studies as markers of coronary artery disease [37,38,39,40,41].
Furthermore, no statistically important difference was found between anti-TNF and non-anti-TNF users as regards the parameters and their change over time. This observation emphasizes the necessity of suppression and control of inflammation, in an attempt of managing the CV risk in RA patients [16, 17]. Indeed, it is reported that the use of anti-TNF in these patients is associated with the reduction of insulin resistance [41].
A limitation of the present study is the relatively small number of patients included as a consequence of strict inclusion criteria and the short period of follow-up; nevertheless, a pure sample was selected. To our knowledge, there are a small number of studies investigating the role of these specific autoantibodies, and this number gets smaller when we focus on RA patients and bDMARDs. We conclude that biological therapy in RA patients is accompanied by a decrease of cIMT values, followed by the reduction of anti-oxLDL. Thus, there is growing evidence that these autoantibodies may constitute an independent biomarker of CV risk prediction, but further evaluation is needed to clarify their complicated mechanism of action.
References
Venetsanopoulou AI, Alamanos Y, Voulgari PV, Drosos AA (2022) Epidemiology of rheumatoid arthritis: genetic and environmental influences. Expert Rev Clin Immunol 18(9):923–931
Blum A, Adawi M (2019) Rheumatoid arthritis (RA) and cardiovascular disease. Autoimmun Rev 18(7):679–690
Libby P, Ridker PM, Hansson GK (2011) Progress and challenges in translating the biology of atherosclerosis. Nature 473(7347):317–325
Björkbacka H, Fredrikson GN, Nilsson J (2013) Emerging biomarkers and intervention targets for immune-modulation of atherosclerosis - a review of the experimental evidence. Atherosclerosis 227:9–17
Delporte C, Van Antwerpen P, Vanhamme L, Roumeguère T, Zouaoui Boudjeltia K (2013) Low-density lipoprotein modified by myeloperoxidase in inflammatory pathways and clinical studies. Mediators Inflamm 2013:971579
Mayr M, Kiechl S, Tsimikas S, Miller E, Sheldon J, Willeit J, Witztum JL, Xu Q (2006) Oxidized low-density lipoprotein autoantibodies, chronic infections, and carotid atherosclerosis in a population-based study. J Am Coll Cardiol 47:2436–2443
Peters MJ, van Halm VP, Nurmohamed MT, Damoiseaux J, Tervaert JW, Twisk JW, Dijkmans BA, Voskuyl AE (2008) Relations between autoantibodies against oxidized low-density lipoprotein, inflammation, subclinical atherosclerosis, and cardiovascular disease in rheumatoid arthritis. J Rheumatol 35:1495–1499
Winyard PG, Tatzber F, Esterbauer H, Kus ML, Blake DR, Morris CJ (1993) Presence of foam cells containing oxidised low density lipoprotein in the synovial membrane from patients with rheumatoid arthritis. Ann Rheum Dis 52:677–680
Dai L, Lamb DJ, Leake DS, Kus ML, Jones HW, Morris CJ, Winyard PG (2000) Evidence for oxidised low density lipoprotein in synovial fluid from rheumatoid arthritis patients. Free Radic Res 32:479–486
Kim SH, Lee CK, Lee EY, Park SY, Cho YS, Yoo B, Moon HB (2004) Serum oxidized low-density lipoproteins in rheumatoid arthritis. Rheumatol Int 24:230–233
Vuilleumier N, Bratt J, Alizadeh R, Jogestrand T, Hafström I, Frostegård J (2010) Anti-apoA-1 IgG and oxidized LDL are raised in rheumatoid arthritis (RA): potential associations with cardiovascular disease and RA disease activity. Scand J Rheumatol 39:447–453
Ajeganova S, de Faire U, Jogestrand T, Frostegård J, Hafström I (2012) Carotid atherosclerosis, disease measures, oxidized low-density lipoproteins, and atheroprotective natural antibodies for cardiovascular disease in early rheumatoid arthritis -- an inception cohort study. J Rheumatol 39:1146–1154
van den Berg VJ, Vroegindewey MM, Kardys I, Boersma E, Haskard D, Hartley A, Khamis R (2019) Anti-oxidized LDL antibodies and coronary artery disease: a systematic review. Antioxidants 8(10):484
Tsimikas S, Willeit P, Willeit J et al (2012) Oxidation-specific biomarkers, prospective 15-year cardiovascular and stroke outcomes, and net reclassification of cardiovascular events. J Am Coll Cardiol 60(21):2218–2229
van den Berg VJ, Haskard DO, Fedorowski A et al (2018) IgM anti-malondialdehyde low density lipoprotein antibody levels indicate coronary heart disease and necrotic core characteristics in the Nordic Diltiazem (NORDIL) study and the integrated imaging and biomarker study 3 (IBIS-3). EBioMedicine 36:63–72
Khamis RY, Hughes AD, Caga-Anan M et al (2016) High serum immunoglobulin G and M levels predict freedom from adverse cardiovascular events in hypertension: a nested case-control substudy of the Anglo-Scandinavian cardiac outcomes trial. EBioMedicine 9:372–380
Venetsanopoulou AI, Pelechas E, Voulgari PV, Drosos AA (2020) The lipid paradox in rheumatoid arthritis: the dark horse of the augmented cardiovascular risk. Rheumatol Int 40(8):1181–1191
Neogi T, Aletaha D, Silman AJ et al (2010) The 2010 American College of Rheumatology/European League Against Rheumatism classification criteria for rheumatoid arthritis: phase 2 methodological report. Arthritis Rheum 62(9):2582–2591
Georgiadis AN, Voulgari PV, Argyropoulou MI et al (2008) Early treatment reduces the cardiovascular risk factors in newly diagnosed rheumatoid arthritis patients. Semin Arthritis Rheum 38:13
Papamichail GV, Markatseli TE, Georgiadis AN, Xydis VG, Milionis H, Drosos AA, Voulgari PV (2022) The effects of biologic agents on cardiovascular risk factors and atherosclerosis in rheumatoid arthritis patients: a prospective observational study. Heart Vessels 37(12):2128–2136
Tsouli SG, Kiortsis DN, Lourida ES, Xydis V, Tsironis LD, Argyropoulou MI, Elisaf M, Tselepis AD (2006) Autoantibody titers against OxLDL are correlated with Achilles tendon thickness in patients with familial hypercholesterolemia. J Lipid Res 47(10):2208–2214
Smolen JS, Landewé RBM, Bergstra SA et al (2023) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2022 update. Ann Rheum Dis 82(1):3–18
Charles-Schoeman C, Wang X, Lee YY et al (2016) Association of triple therapy with improvement in cholesterol profiles over two-year followup in the treatment of early aggressive rheumatoid arthritis trial. Arthritis Rheumatol 68:577–586
Liao KP, Playford MP, Frits M et al (2015) The association between reduction in inflammation and changes in lipoprotein levels and HDL cholesterol efflux capacity in rheumatoid arthritis. J Am Heart Assoc 4:e001588
McMahon M, Grossman J, FitzGerald J et al (2006) Proinflammatory high-density lipoprotein as a biomarker for atherosclerosis in patients with systemic lupus erythematosus and rheumatoid arthritis. Arthritis Rheum 54:2541
Ormseth MJ, Yancey PG, Solus JF et al (2016) Effect of drug therapy on net cholesterol efflux capacity of high-density lipoprotein-enriched serum in rheumatoid arthritis. Arthritis Rheumatol 68:2099
Lourida ES, Georgiadis AN, Papavasiliou EC et al (2007) Patients with early rheumatoid arthritis exhibit elevated autoantibody titers against mildly oxidized low-density lipoprotein and exhibit decreased activity of the lipoprotein-associated phospholipase A2. Arthritis Res Ther 9(1):R19
Hartley A, Haskard D, Khamis R (2019) Oxidized LDL and anti-oxidized LDL antibodies in atherosclerosis - novel insights and future directions in diagnosis and therapy. Trends Cardiovasc Med 29(1):22–26
Denning N-L, Aziz M, Gurien SD, Wang P (2019) DAMPs and NETs in sepsis. Front Immunol 10:2536
Prasad A, Clopton P, Ayers C et al (2017) Relationship of autoantibodies to MDA-LDL and ApoB-immune complexes to sex, ethnicity, subclinical atherosclerosis, and cardiovascular events. Arterioscler Thromb Vasc Biol 37(6):1213–1221
Ravandi A, Boekholdt SM, Mallat Z et al (2011) Relationship of IgG and IgM autoantibodies and immune complexes to oxidized LDL with markers of oxidation and inflammation and cardiovascular events: results from the EPIC-Norfolk Study. J Lipid Res 52(10):1829–1836
Cozzani E, Drosera M, Gasparini G, Parodi A (2014) Serology of lupus erythematosus: correlation between immunopathological features and clinical aspects. Autoimmune Dis 2014:321359
Robbins A, Hentzien M, Toquet S, Didier K, Servettaz A, Pham BN, Giusti D (2019) Diagnostic utility of separate anti-Ro60 and anti-Ro52/TRIM21 antibody detection in autoimmune diseases. Front Immunol 10:444
Steinberg D, Witztum JL (2010) Oxidized low-density lipoprotein and atherosclerosis. Arterioscler Thromb Vasc Biol 30(12):2311–2316
Tsiantoulas D, Diehl CJ, Witztum JL, Binder CJ (2014) B cells and humoral immunity in atherosclerosis. Circ Res 114(11):1743–1756
Fent GJ, Greenwood JP, Plein S, Buch MH (2017) The role of non-invasive cardiovascular imaging in the assessment of cardiovascular risk in rheumatoid arthritis: where we are and where we need to be. Ann Rheum Dis 76(7):1169
Polak JF, Pencina MJ, Pencina KM, O’Donnell CJ, Wolf PA, D’Agostino RB Sr (2011) Carotid-wall intima-media thickness and cardiovascular events. N Engl J Med 365(3):213–221
Lorenz MW, Sitzer M, Markus HS, Bots ML, Rosvall M (2007) Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis response. Circulation 116(9):318
Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, Najjar SS, Rembold CM, Post WS (2008) Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr 21(2):93–111
Johri AM, Nambi V, Naqvi TZ, Feinstein SB, Kim ES, Park MM, Becher H, Sillesen H (2020) Recommendations for the assessment of carotid arterial plaque by ultrasound for the characterization of atherosclerosis and evaluation of cardiovascular risk: from the American Society of Echocardiography. J Am Soc Echocardiogr 33:917–933
Kiortsis DN, Mavridis AK, Vasakos S, Nikas SN, Drosos AA (2005) Effects of infliximab treatment on insulin resistance in patients with rheumatoid arthritis and ankylosing spondylitis. Ann Rheum Dis 64(5):765–776
Acknowledgements
The authors would like to thank the patients who participated in the study.
Author information
Authors and Affiliations
Contributions
G. V. Papamichail: conceptualization, methodology, data collection, investigation, and writing—original draft preparation; A. N. Georgiadis: data collection and investigation; C. C. Tellis: investigation; I. Rapti: statistical analysis; T. E. Markatseli: statistical analysis; V. G. Xydis: investigation; A. D. Tselepis: investigation and critical review; A. A. Drosos: methodology, supervision, and critical review and editing; P. V. Voulgari: conceptualization, methodology, supervision, and critical review.
Corresponding author
Ethics declarations
Ethics approval
All procedures were in accordance with ethical standards and the Helsinki Declaration of 1964 and its later amendments. The study protocol was approved by the institutional ethics committee.
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
•RA patients with active disease, receiving csDMARDs may develop ongoing atherosclerosis.
•TC and HDL-C were elevated, while cIMT and anti-oxLDL were reduced after 6 months of treatment, regardless of the bDMARD that was administered.
•No statistically significant association was found between the cIMT and anti-oxLDL, HDL-C, CRP, or DAS28 neither before nor 6 months after the administration of biological agents.
•IgG anti-oxLDL may contribute to atherosclerosis in active RA.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Papamichail, G.V., Georgiadis, A.N., Tellis, C.C. et al. Antibodies against oxidized LDL and atherosclerosis in rheumatoid arthritis patients treated with biological agents: a prospective controlled study. Clin Rheumatol 43, 481–488 (2024). https://doi.org/10.1007/s10067-023-06744-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-023-06744-z