Abstract
Objective
We aimed to provide a better understanding of the secular trends in rheumatoid arthritis (RA) burden at the regional and national levels, contributing to identifying the areas with high burden needs and finding the potential areas requiring additional attention, which will facilitate the development of strategies tailored to RA burden.
Method
Data were obtained from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019 study. We presented the secular trends in the prevalence, incidence, and years lived with disability (YLDs) of RA needs by sex, age, sociodemographic index (SDI), region, country, and category between 1990 and 2019 using data from the GBD 2019 study. The age-standardized rates (ASR) and its estimated annual percentage changes (EAPCs) are employed to describe the secular trends in RA.
Results
Globally, there were an estimated 18.5 million [95% confidence interval (CI) 31.53 to 41.74)] prevalent cases of RA, with 1.07 million (95% CI 0.95 to 1.18) incident cases per year and almost 2.43 million YLDs (95% CI 1.68 to 3.28) in 2019. The age-standardized prevalence and incidence rates estimated for RA were 224.25 per 100,000 and 12.21 per 100,000 in 2019, with EAPCs of 0.37 (95% CI − 0.32, 0.42) and 0.30 (95% CI 0.25 to 0.34), respectively. The corresponding age-standardized YLDs estimated was 29.35 per 100,000 in 2019, with an EAPC of 0.38 (95% CI: 0.33, 0.43). During the study period, the ASR of RA was consistently higher in females than in males. Moreover, the age-standardized YLD rate of RA was associated with the sociodemographic index (SDI) in 2019 across all 204 countries and territories (R = 0.28). The projections indicate that the age-standardized incidence rates (ASIR) trend will continue to increase from 2019 to 2040, with a projected ASIR of 10.48 and 4.63/100,000 for females and males, respectively.
Conclusions
RA is prevalent and remains a significant global public health challenge. Globally, the burden of RA has increased over the past 30 years and will continue to increase. Prevention and early treatment of RA are pivotal to avoiding disease onset and alleviating the enormous burden.
Key Points • The burden of rheumatoid arthritis is increasing globally. • Global estimates indicate that the number of RA incident cases will increase 1.4-fold globally, from approximately 1.07 million at the end of 2019 to approximately 1.5 million by 2040. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is an inflammatory, autoimmune, chronic disease that primarily affects joints. Symmetrical inflammatory polyarthritis is the primary clinical manifestation, including the metacarpophalangeal and proximal interphalangeal joints of the hands and feet, gradually progressing to the large joints [1, 2]. Persistent inflammation leads to damage and deformity of the affected joint [3,4,5]. It has only been during the twenty-first century that remission, let alone cure, has been a regularly achievable target in RA. RA is a significant public health problem associated with a burden of resultant functional disability. Globally, the overall age-standardized prevalence and incidence rate of RA have increased [6]. However, the secular trend in RA burden by region and country has not been reported. Collectively, these findings point to a strong need to document the global burden caused by RA.
Clinically, the symptoms of early treated RA differ significantly from later undertreated symptoms. Early diagnosis and treatment of RA can block joint degeneration in 90% of patients [2]. However, insufficiently treated RA exhibits complex clinical symptoms accompanied by severe general manifestations [2]. RA could also involve some essential internal organs, such as the lungs, heart, kidneys, and digestive tract, and the whole process is ongoing and recurrent, which is a significant health problem worldwide, resulting in a huge psychological burden for patients and a substantial economic burden for society [7, 8]. Determining the global burden of RA, such as prevalence, incidence, and years lived with disability (YLDs), is essential because of the high rate of disability in RA. Collectively, these findings point to a strong need to document the global burden caused by RA.
Several national studies have reported, examined the prevalence and incidence of RA, and reported the burden of RA in regions or territories. The prevalence and incidence of RA varied significantly between studies due to differences in the definitions used, data sources, age categories, and sex distribution of the study population [9,10,11]. It is unclear whether this is due to inconsistencies in the defined population, changes in the methods used to identify people with RA, including data sources, sample size, date of data collection, or the criteria used to classify RA [12]. For instance, Sebbag et al. conducted an analysis utilizing the Global Burden of Disease (GBD) 2010 and reported the global and regional burdens of RA in terms of prevalence and disability-adjusted life years. However, national-level estimates were not provided [13]. Using GBD 2017, Safiri S et al. systematically examined RA burden at global, regional, and national levels, yet their estimates were based on 2017 data and no forecast for RA trends over the next 20 years [14]. However, the global trend in RA burden by region and country has never been reported. In addition, no study has investigated the annual percentage changes (EAPCs) in RA burden by category over a specific time interval. Hence, we aimed to understand better the secular trends in RA burden at the regional and national levels, providing evidence that healthcare decision-makers can make decisions and prioritize RA as a population-level health problem.
Methods
Overview GBD
GBD 2019, conducted by the Institute of Health Metrics and Evaluation, covers 204 countries, 7 superregions, and 21 regions from 1990 to 2019. GBD 2019 enlarged its analysis of the burden of disease for all WHO Member States compared to GBD 2017, adding nine countries and territories to the GBD position hierarchy [15]. GBD 2019 assessed attributable mortality, years of life lost, years of life lived with disability, and disability-adjusted life years for 87 risk factors and combinations of risk factors at the worldwide level, regionally, for 204 countries and territories, comparing the 84 risk factors in GBD 2017 [14, 15]. A detailed description of the collection and processing of the data, the methodology for reporting the 2019 GBD results, and key advances compared to earlier series has been published elsewhere [15,16,17]. RA incidence, prevalence, and YLDs were evaluated using large-scale population-representative data sources identified in the literature retrieval and via research collaborations.
Case definition and data sources
The definition has been described in previous studies [14]. The reference case definitions for estimating RA prevalence in the GBD studies were from the American College of Rheumatology (ACR 2010) [18], which display seven diagnostic criteria. The GBD 2019 study includes raw data from 46 countries, as well as data based on modeling derived from other country regions, incidence, prevalence, and YLDs of RA in global, regional, and national populations by sex and age, and national socio-demographic index (SDI) value levels from 1990 to 2019.
Severity and years lived with disability
The International Classification of RA (M05-M06.9, M08.0-M08.89) uses ICD-10 codes with three sequelae (severity), each with a specific DW ranging from 0.11 to 0.58. These proportions were then used to divide the overall prevalence of RA into severity categories. Finally, prevalence estimations were multiplied by the disability weights (DWs) of reciprocally exclusive disease and injury sequelae to calculate YLDs.
Socio-demographic index
SDI is a generalized measure that assesses a location’s position on a development spectrum. A composite indicator of income, education, and fertility is a metric for measuring development. It allows comparisons of health outcomes and health system performance between countries to better understand world health in the future [17].
Statistical analysis
The International Classification of RA (M05-M06.9, M08.0-M08.89) uses ICD-10 codes with three sequelae (severity), each with a specific DW ranging from 0.11 to 0.58. These proportions were then used to divide the overall prevalence of RA into severity categories. Finally, prevalence estimations were multiplied by the disability weights (DWs) of reciprocally exclusive disease and injury sequelae to calculate YLDs. To assess long-term trends in RA, the estimated annual percentage change (EAPC) and obtain 95% confidence intervals (CIs), ASR in number and amplitude of fold change variations apply to all ages. The EAPC was identified to be 100 × (exp(β) − 1), and the corresponding 95% confidence interval (CI) was calculated using a linear regression model: y = α + βx + ε, where y = ln (ASR) and x = calendar year [19]. ASR showed a decreasing trend when the upper limit of both the EAPC estimate, and it's 95% CI were < 0. Conversely, when both the EAPC estimate and the lower limit of its 95% CI were > 0, ASR showed an increasing trend. In addition, ASR was stable over time. To explore the gender and age distribution patterns of RA prevalence, we obtained crude data and proportions of RA prevalence in 2019 and analyzed the gender-age patterns of male and female individuals according to RA patients grouped every five years. Based on the GBD 2019 estimates, we projected the incidence of RA in 2040 by running the Nordpred age-period-cohort (NAPC) analytically using the Nordpred package R. Considering the changing rates and the ongoing demographic changes, the model has been well demonstrated and endorsed in previous studies [20]. Furthermore, to facilitate comparison with the predicted results, we calculated the absolute number of events that would occur if the incidence remained stable (baseline reference), decreased by 1% per year (optimistic reference), and increased by 1% per year (pessimistic reference) based on the observed rates in 2019. All statistical analysis and visualizations were performed using Python 3.9.9 (Jupyter, US) and R version 3.5.2 (The R Project for Statistical Computing, Vienna, Austria).
Results
Global level
Based on the GBD estimates, the age-standardized prevalence and incidence rates estimated for RA were 224.25 per 100,000 persons (95% CI 20.94 to 245.99) and 12.21 per 100,000 persons (95% CI 11.83 to 14.27) in 2019, with EAPCs of 0.37 (95% CI − 0.32 to 0.42) and 0.30 (95% CI 0.25 to 0.34), respectively. The corresponding estimated age-standardized YLD rate was 29.35 per 100,000 person-years (95% CI 20.29 to 39.51) in 2019, with an EAPC of 0.38 (95% CI 0.33 to 0.43) (Table 1).
The present study estimated that the global number of incident cases of RA increased 0.89-fold from 1990, with 1.07 million (95% CI 0.95 to 1.18) in 2019 (Supplementary Figure S1). The ASIR increased from 1990 to 2019 (EAPC = 0.30, 95% CI 0.25 to 0.34), with values of 12.21 (95% CI 11.33 to 13.38) and 13.00 (95% CI 11.83 to 14.27), respectively. There were 18.5 million (95% CI 31.53 to 41.74) prevalent cases of RA in 2019, a 1.06-fold increase from 1990 (Supplementary Figure S1b). The age-standardized prevalence rates (ASPR) increased across the study period (EAPC = 0.37, 95% CI, 0.32 to 0.42), from 207.46 per 100,000 in 1990 to 224.25 per 100,000 in 2019 (Table 1).
In 2019, nearly 2.43 million (95% CI 1.68 to 3.28) YLDs increased 1.05-fold from 1990 due to RA. (Supplementary figure S1c). Moreover, the age-standardized rate of YLDs increased across the study period (EAPC = 0.38, 95% CI 0.33 to 0.43), from 27.10 per 100,000 in 1990 to 29.35 per 100,000 in 2019 (Table 1).
The prevalent cases, incident cases, and YLD cases increased in all five SDI regions from 1990 to 2019, with the most significant increase detected in the Low SDI regions. The absolute number of prevalent cases, incident cases, and YLD cases increased nearly 1.48-fold, 1.34-fold, and 1.49-fold, respectively (Table 1) Supplementary figure S2).
Regional level
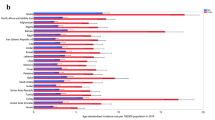
Based on the GBD estimates, the ASIR of RA was found to have the most significant increases in Andean Latin America (EAPC = 1.39, 95% CI, 1.32 to 1.45), followed by Southern Latin America (EAPC = 1.01, 95% CI, 0.92 to 1.10) and Central Asia (EAPC = 1.0, 95% CI, 0.90 to 1.10), whereas Oceania (EAPC = 0.13, 95% CI, 0.10 to 0.17), high-income Asia Pacific (EAPC = 0.11, 95% CI, 0.02 to 0.20), and Central Latin America (EAPC = 0.08, 95% CI, 0.05 to 0.11) showed the lowest increases. Only EAPC was stable in southern sub-Saharan Africa (EAPC = 0.03, 95% CI − 0.01 to 0.08) (Fig. 1A and Fig. 2A).
The global ASR trends of RA for both sexes in 204 countries and territories from 1990 to 2019. (A) The ASIR of RA in 2019. (B) The ASPR of RA in 2019. (C) The YLDs of RA in 2019. ASR, age-standardized rate; ASIR, age-standardized incidence rate; ASPR, age-standardized prevalence rate; YLDs, years lived with disability; RA, rheumatoid arthritis
In 2019, the highest number of incident cases (290,965) occurred in South Asia, followed by East Asia (229,076) (Table 1), whereas high-income North America had the highest ASIR at 21.46 per 100,000, followed by Central Latin America at 21.12 per 100,000 (Supplementary Table 2. Supplementary figure S3).
Based on the GBD estimates, the ASPR of RA was found to have the highest increase in Andean Latin America (EAPC = 1.49, 95% CI, 1.42 to 1.56), followed by Central Asia (EAPC = 1.07, 95% CI, 0.96 to 1.17) and Southern Latin America (EAPC = 1.03, 95% CI, 0.94 to 1.12). Oceania (EAPC = 0.14, 95% CI, 0.11 to 0.18) and Central Latin America (EAPC = 0.13, 95% CI, 0.10 to 0.16) showed the lowest and were stable only in Southern Sub-Saharan Africa (EAPC = 0.05, 95% CI − 0.01 to 0.11) (Fig. 1B and Fig. 2B).
In 2019, the highest number of prevalent cases (4,439,149) occurred in East Asia, followed by South Asia (3,954,265) and Western Europe (1,818,229) (Table 1), whereas Central Latin America had the highest ASPR was 366.08 per 100,000, followed by Australasia was 331.81 per 100,000 in 2019 (Supplementary table 2 and supplementary figure S4).
Based on the GBD estimates, the most of RA YLDs cases in 2019 were documented in East Asia (587,559), followed by South Asia (510,513). However, Central Latin America had the highest YLDs of age-standardized rate was 47.99 per 100,000, followed by high-income North America at 44.03 per 100,000 in 2019 (Supplementary table 2 and supplementary figure S5). Meanwhile, the RA YLDs of the age-standardized rate increased fastest in Andean Latin America (EAPC = 1.48, 95% CI 1.41 to 1.56), followed by Central Asia (EAPC = 1.06, 95% CI 0.96 to 1.16) and Southern Latin America (EAPC = 1.02, 95% CI 0.94 to 1.11). Moreover, the RA YLDs of the age-standardized rate were only stable in western sub-Saharan Africa (EAPC = -0.02, 95% CI -0.05 to 0.08) (Fig. 1C and Fig. 2C).
Age and sex patterns
Globally, both the incidence rate and prevalent cases of RA were higher in females. The global ASIR is higher in females and increases with age, peaking in 2019 in the 70–74 and 75–79 age cohorts for females and males, respectively. The number of prevalent cases increased with age, peaking at 60–64 years for both males and females, with a decreasing trend after this age (Fig. 3A).
In 2019, global ASPR was also higher in females and increased with population aging, peaking in the 60–64 and 65–69 age groups for females and males, respectively. The number of incident cases after that the trend starts to decline, with the fastest decline for males and females from 70–74 to 80–84, after which the decline slows down (Fig. 3B). The rate of YLDs was higher in women and increased with age, peaking in 2019 in females and males in the age group 70–74 years. The number of YLD cases increased with age and was highest in both sexes in the age group 60–64 years, after which the trend declined (Fig. 3C).
Burden of RA according to SDI
The smoothing splines model suggests an overall correlation between age-standardized YLDs due to RA and SDI at the global and regional levels in 2019 (R = 0.28, p < 0.001). When SDI is 0.25, YLDs is estimated to be the lowest; it shows an overall elevation trend of YLDs with SDI improvement, especially when SDI is > 0.75, which significantly increases. As shown in Fig. 4, high-income North America, Andean Latin America, Eastern Sub-Saharan Africa, Australasia, Central Latin America, and southern Latin America had a much higher than expected burden in almost all measurement periods. However, high-income Asia Pacific, Southeast Asia, Oceania, North Africa, and the Middle East had a lower-than-expected burden of RA during this period. Moreover, in Central Europe, Eastern Europe, the burden caused by RA in different regions shows diversity.
Global predictions of RA incidence
Based on the GBD estimates, we forecast that the global incidence of RA will continue to increase, especially among females (Fig. 5A–C). As shown in Fig. 5B and C, the trend in female incidence is somewhat similar to that of males, but the incidence is substantially higher than that of males. Our study shows that the ASIR trend will continue to increase from 2019 to 2040, with a projected ASIR of 10.48 and 4.63/100,000 for females and males, respectively.
Global trends in RA incidence rates by sex: observed (solid lines) and predicted rates (dashed lines). (A) Global incidence trends by 2040. (B) Global female incidence trends by 2040. (C) Global male incidence trends by 2040. (D) Shades indicate whether the rate remained stable (baseline reference), decreased by 1% per year (optimistic reference, lower limit), or increased by 1% per year (pessimistic reference, upper limit) based on the observed rate in 2019
With the increased incidence of RA, the number of new cases globally is expected to increase over the next 20 years due to population growth. The shading in Fig. 5 indicates a 1% increase or decrease per year, with a corresponding substantial variation in the number of newly diagnosed cases. The forecast results were somewhat higher than the pessimistic reference; with a 1% increased rate annually, incident cases would increase from 1,074,391 in 2019 to 1,496,358 in 2040. Among females, the number of incident cases is expected to increase from 743,930 in 2019 to 1,033,887 in 2040. In addition, the number of incident cases in males would increase from 330,460 in 2019 to 467,282 in 2040 (Fig. 5D).
Discussion
In this paper, using data derived from GBD 2019, we provide updated and comprehensive estimates of age-standardized prevalence, incidence rates, and YLDs for RA in 204 countries and territories in 2019. We present the first analysis of long-term trends in prevalence, incidence, and YLDs from 1990 to 2019. Prevalent cases, incident cases, YLDs cases, and ASR of RA increased globally and revealed female predominance and showed geographical diversity and location differences by comparing across regions and over periods. Moreover, the forecasts up to 2040 suggest that the increasing incidence will continue.
In 2019, Safiri S et al. first reported the incidence, prevalence, ASR, and DALYs of RA at the national level in GBD 2017. Furthermore, they examined the age and gender patterns of RA and assessed the relation between the DALY rate and SDI. The updated data sources and improved methodologies in our study provide an advantage over the previous two studies. Our data are from GBD 2019 and are updated compared to GBD 2017. In addition, we have projected the disease burden for the next 20 years. Therefore, obtaining the latest global RA and the trend of the coming diseases is essential to provide basic information for policymakers to implement measures. However, due to GBD 2019 data differences, our estimates need to be compared with previous findings with caution. This discrepancy may be partly explained by additional data sources and new methods applied in GBD 2019. In addition, previous studies did not include predicting the incidence of RA in 2040 globally and did not involve the EAPC.
The age-standardized prevalence and incidence of RA increased from 1990 to 2019, which is consistent with previous studies [14, 21]. However, we found that the EAPC of RA was > 0 in 204 countries and territories worldwide. GBD modeling allows us to compare across regions and over time periods, showing geographical diversity and site disparity of RA burden. In addition, GBD 2019 showed that the ASPR was higher among females and increased with age, peaking at 70–74 and 75–79 in the female and male age groups, respectively. The ASIR was higher in females and increased with age, peaking in the 60–64 and 65–69 age groups for females and males, respectively. The age-standardized YLDs rates among females were higher and increased with age, peaking at 70–74 for both sexes. The prevalence of RA by age group has also been investigated in previous studies and has been reported to be higher in females than males [11, 14, 22]. However, the prevalence was higher in people aged 50–69 years in previous studies [22], which was not similar to the GBD 2019 findings. This may be the result of different sources of databases and geographical diversity and site disparity.
Previous findings confirm the notion of an increasing burden of RA observed in previous studies [11, 14, 21, 23]. A nationwide study of older RA patients reported that nearly 5% of the patients developed interstitial lung disease (ILD) due to RA [24]. A systematic review examined the prevalence, costs, and work activity associated with the incidence of RA [23]. The mean all-cause direct cost for RA varies from $12,509 ($13,800) [25] to $20,919 ($24,255) [26] per patient annually. This is only for the US and does not provide a comprehensive assessment. Globally, of the 369 diseases and injuries studied in the 2019 GBD, RA had a prevalent case load of 18.5 million in 2019, indicating a substantial disease burden. Additionally, regarding the public health significance, the present study shows an increasing trend in the prevalence, incidence and YLDs of RA globally from 1990 to 2019. These results show a substantial disease burden.
The present study indicated that YLDs is an overall correlation with socioeconomic development level (R = 0.28, p < 0.001), which is not consistent with the previously reported trend of RA and SDI [14]. Although our results show an overall correlation, the association between SDI level and YLDs shows a complex association. Indeed, the RA burden was not confined to developed or less developed countries, and countries with diverse SDIs reported an overall higher RA burden. Especially in Central Europe and Eastern Europe, the burden caused by RA in different SDI regions shows diversity. We analyze the burden of RA in various regions and countries, allowing for better comparisons between countries to facilitate response strategies based on the corresponding health situation.
This study predicts the ASIR for females and males in 2040, and our study shows that the ASIR trend will continue to increase from 2019 to 2040, with a projected ASIR of 10.48 and 4.63/100,000 for females and males, respectively. The projections indicate that the number of RA incident cases will increase 1.4-fold globally, from approximately 1.07 million at the end of 2019 to approximately 1.5 million by 2040. Thus, decreasing the global burden of RA is an urgent issue globally. Thus, this highlights the importance of health promotion to raise public awareness about RA disease onset, consequences, and treatment strategies, perhaps through health education interventions. The focus should be on the risk factors and the middle-aged female population of RA when developing these programs and interventions. In the current study, the global incidence of RA is predicted to increase over the next 20 years, considering the tremendous and increasing disease burden of RA. This further highlights the importance of RA prevention and treatment. Along with these previously emphasized aspects aimed at modifying risk factors, such as refraining from smoking, hormones, stress, obesity, infections, gut bacteria, and dietary factors [27], we also advocate for early recognition and early treatment of RA disease progression. Early diagnosis is critical to optimal treatment success, and combination therapy can prevent joint damage progression in approximately 90% of patients with early RA [2, 28]. The burden of RA on society is likely to rise. Government and policymakers should direct efforts, and strategies to improve prevention and treatment for RA need to be proposed to curb the increasing incidence of RA and reduce the burden of RA.
Several limitations of our study should be noted, including previously recognized flaws in the GBD research methodology [15]. Data from individual studies in the GBD model were labeled covariates in these changing methods during the modeling process, allowing DisMod-MR 2.1 to adjust the data points to the level predicted when the study measured the reference diagnosis. However, while this modeling provides for data comparisons across regions over time, differences in the way RAs are defined are a limitation that prevents truly valid comparisons between regions. However, there are reports that the incidence rate is decreasing in developed countries, and there is uncertainty in the results that it is increasing. Different countries have different access to medical care, diagnostic techniques, and treatments, making it difficult to lump them together. Therefore, this is a speculative calculation, and some estimates may be substantially uncertain and should be interpreted with caution. The disadvantage of our model is that there is no exact range of how much of the increased incidence is caused by cases of RA or by changes in practice detection. Moreover, we investigated ASR-related factors. The SDI was used to measure the quality and availability of health care, while health systems were not evaluated.
Conclusions
RA is prevalent and remains a significant global public health challenge. The age-standardized prevalence, annual incidence, and YLDs vary significantly across countries and territories. The change is most apparent, especially in Andean Latin America. The global burden of RA has increased over the past 30 years and will continue to grow over the next 20 years. Our findings emphasize the need for public policy interventions through disease prevention projects. Public awareness of modifiable risk factors, prevention, and early treatment is pivotal to avoiding the onset and alleviating the enormous burden of RA.
Data availability
These data can be found in a public, open-access repository. The datasets used for the analyses can be found at http://ghdx.healthdata. org/gbd- results- tool.
References
Smolen JS, Aletaha D, Barton A et al (2018) Rheumatoid arthritis. Nat Rev Dis Primers 4:18001
Aletaha D, Smolen JS (2018) Diagnosis and management of rheumatoid arthritis: a review. JAMA 320:1360–1372
Semb AG, Ikdahl E, Wibetoe G, Crowson C, Rollefstad S (2020) Atherosclerotic cardiovascular disease prevention in rheumatoid arthritis. Nat Rev Rheumatol 16:361–379
Lillegraven S, van der Heijde D, Uhlig T, Kvien TK, Haavardsholm EA (2012) What is the clinical relevance of erosions and joint space narrowing in RA? Nat Rev Rheumatol 8:117–120
Scott DL, Wolfe F, Huizinga TW (2010) Rheumatoid arthritis. Lancet 376:1094–1108
Myasoedova E, Davis J, Matteson EL, Crowson CS (2020) Is the epidemiology of rheumatoid arthritis changing? Results from a population-based incidence study, 1985–2014. Ann Rheum Dis 79:440–444
Papakonstantinou D (2021) Work disability and rheumatoid arthritis: predictive factors. Work 69:1293–1304
Hsieh PH, Wu O, Geue C et al (2020) Economic burden of rheumatoid arthritis: a systematic review of literature in biologic era. Ann Rheum Dis 79:771–777
Won S, Cho SK, Kim D et al (2018) Update on the prevalence and incidence of rheumatoid arthritis in Korea and an analysis of medical care and drug utilization. Rheumatol Int 38:649–656
Vergne-Salle P, Pouplin S, Trouvin AP et al (2020) The burden of pain in rheumatoid arthritis: impact of disease activity and psychological factors. Eur J Pain 24:1979–1989
Almutairi KB, Nossent JC, Preen DB, Keen HI, Inderjeeth CA (2021) The prevalence of rheumatoid arthritis: a systematic review of population-based studies. J Rheumatol 48:669–676
Shapira Y, Agmon-Levin N, Shoenfeld Y (2010) Geoepidemiology of autoimmune rheumatic diseases. Nat Rev Rheumatol 6:468–476
Sebbag E, Felten R, Sagez F et al (2019) The world-wide burden of musculoskeletal diseases: a systematic analysis of the World Health Organization Burden of Diseases Database. Ann Rheum Dis 78:844–848
Safiri S, Kolahi AA, Hoy D et al (2019) Global, regional and national burden of rheumatoid arthritis 1990–2017: a systematic analysis of the Global Burden of Disease study 2017. Ann Rheum Dis 78:1463–1471
GBD 2019 Risk Factors Collaborators (2020) Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258):1223–1249
Global age-sex-specific fertility (2020) mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 396:1160–1203
GBD 2019 Diseases and Injuries Collaborators (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396(10258):1204–1222
Aletaha D, Neogi T, Silman AJ et al (2010) 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 62:2569–2581
Ming Y, Linghui Z, Anping L, Suxia L, Kongming W (2020) Global burden and trend of acute lymphoblastic leukemia from 1990 to 2017. Aging (Albany NY) 12(22):22869–22891
Møller B, Fekjaer H, Hakulinen T et al (2003) Prediction of cancer incidence in the Nordic countries: empirical comparison of different approaches. Stat Med 22:2751–2766
Cross M, Smith E, Hoy D et al (2014) The global burden of rheumatoid arthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis 73:1316–1322
Castillo-Cañón JC, Trujillo-Cáceres SJ, Bautista-Molano W et al (2021) Rheumatoid arthritis in Colombia: a clinical profile and prevalence from a national registry. Clin Rheumatol 40:3565–3573
Lo J, Chan L, Flynn S (2021) A systematic review of the incidence, prevalence, costs, and activity and work limitations of amputation, osteoarthritis, rheumatoid arthritis, back pain, multiple sclerosis, spinal cord injury, stroke, and traumatic brain injury in the United States: A 2019 Update. Arch Phys Med Rehabil 102:115–131
Sparks JA, Jin Y, Cho SK et al (2021) Prevalence, incidence and cause-specific mortality of rheumatoid arthritis-associated interstitial lung disease among older rheumatoid arthritis patients. Rheumatology (Oxford) 60:3689–3698
Hresko A, Lin TC, Solomon DH (2018) Medical care costs associated with rheumatoid arthritis in the US: A systematic literature review and meta-analysis. Arthritis Care Res (Hoboken) 70:1431–1438
Chen CI, Wang L, Wei W, Yuce H, Phillips K (2018) Burden of rheumatoid arthritis among US Medicare population: co-morbidities, health-care resource utilization and costs. Rheumatol Adv Pract 2:rky005
van der Woude D, van der Helm-van MAHM (2018) Update on the epidemiology, risk factors, and disease outcomes of rheumatoid arthritis. Best Pract Res Clin Rheumatol 32:174–187
Smolen JS, Aletaha D, McInnes IB (2016) Rheumatoid arthritis. Lancet 388:2023–2038
Acknowledgements
We would like to thank the staff and collaborators of the Institute for Health Metrics and Evaluation for making these publicly available data possible.
Author information
Authors and Affiliations
Contributions
GS, XL, and ZL designed the study. GS, XL, ZL, WL, and XL analyzed the data and performed the statistical analyses. GS, XL, and ZL drafted the initial manuscript. HRZ and XYC reviewed the key elements of the drafted manuscript. All authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval
This study is based on a public database; therefore, ethical approval is not needed.
Patient and public involvement
Researchers did not involve patients or the public in the design, conduct, reporting, or dissemination of the study.
Patient consent for publication
Not required.
Disclosures
None.
Provenance and peer review
The study was not commissioned; it was peer-reviewed.
Disclaimer
The study is based on publicly available information and only represents the views of its authors and not those of the Institute for Health Metrics and Evaluation.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shi, G., Liao, X., Lin, Z. et al. Estimation of the global prevalence, incidence, years lived with disability of rheumatoid arthritis in 2019 and forecasted incidence in 2040: results from the Global Burden of Disease Study 2019. Clin Rheumatol 42, 2297–2309 (2023). https://doi.org/10.1007/s10067-023-06628-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-023-06628-2