Abstract
Background
Osteophyte formation is an important radiographic sign of osteoarthritis (OA) and limited joint motion in knee osteoarthritis patients. Some studies revealed relationships of osteophyte formation with a high bone mineral density and a high muscle mass, while others showed no correlations. The aim of this study was to identify relationships of osteophyte formation with bone mineral density and muscle mass.
Methods
A cross sectional study of knee osteoarthritis was conducted. Cases were classified as patients with osteophyte formation, while controls were those without osteophytes. All subjects underwent a knee x-ray and bone mineral density and body composition evaluation. General patient characteristics, covariates, and the results of biochemical analyses were also recorded. Statistical analysis was conducted using SPSS Version 22.0. Logistic regression and the chi-square test were utilized to analyze the relationships between the presence of knee osteophytes and the study variables.
Results
A total of 228 patients were enrolled, including 78 with osteophytes in the knee joint and 150 without. A total of 162/228 are females; knee OA is commonly explained among females. (p = 0.001). The mean age was 73.23 ± 11.10 years in the osteophyte group and 71.86 ± 12.23 in the no osteophyte group (p = 0.409). The mean body mass index was 24.15 ± 3.27 kg/m2 in the osteophyte group and 23.37 ± 3.48 kg/m2 in the no osteophyte group (p = 0.433). More patients in the osteophyte group had hypertension (p = 0.002), so the age group 73 years expected to have OA and hypertension along other metabolic diseases, and the femoral neck T score was higher in the osteophyte group (p = 0.044). Logistic regression analysis showed that the male gender was associated with less osteophyte formation (p = 0.001, odds ratio (OR) 0.11 (0.03–0.37)), and hypertension was associated with increased muscle loss (p = 0.005). Femoral neck T score was associated with the presence of osteophyte formation (p = 0.011, OR 1.98 (1.17–3.36)).
Conclusions
The results demonstrated an association of knee osteophyte formation with the femoral neck T score and hypertension, but no association with muscle mass. We speculated that in patients with osteophytosis and increased bone mass, metabolic factors such as hypertension should be considered. Further study of the molecular mechanisms regulating these processes is needed in the future.
Key Points • Associations of knee osteophyte formation with the femoral neck T score, but not with muscle mass. • Those with osteophytosis and an increased bone mass and metabolic factors such as hypertension need to be assessed. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Knee osteoarthritis (OA) is common and is becoming increasingly prevalent in the aging population. Conventional radiographic findings include joint space narrowing, sclerosis of the subchondral bone, subchondral cysts, and the formation of osteophytes, which are the key features in knee OA [1]. At present, the formation of osteophytes is regarded as an important radiographic sign of OA and is taken to indicate degeneration of the articular cartilage within the tibiofemoral joint [2].
It has been reported that osteophyte formation is associated with increased bone mineral density (BMD) at the lumbar spine femoral neck [3], and several studies have observed a stronger association between BMD and osteophyte formation than between BMD and joint space narrowing [4,5,6], suggesting that an increased BMD predisposes patients primarily to the bony features of OA. Other studies have suggested that BMD in the upper extremities is not associated with OA [7], and some studies have suggested that a decreased BMD is associated with radiographic OA of the hand [8], radius [9], and even the hip [10] and spine [11]. Therefore, the relationship between OA and osteoporosis remains controversial.
Sarcopenia, defined as age-related loss of muscle mass and low muscle function, may be the most prominent component of frailty, disability, and morbidity in older people [12]. In a German report, the prevalence of sarcopenia was significantly higher in participants with OA of the hip and lower limbs as compared with their nonarthritic peers [13]. In fact, lower limb muscle weakness favors OA progression [14]. Waters et al. reported that the habitual walking speed was significantly lower in patients with OA [15]; however, a review of OA and sarcopenia [16] illustrated that neither a direct effect of sarcopenia on OA development, nor the opposite relationship, can be concluded.
So, what are the relationships of osteophyte formation with BMD or sarcopenia? The aim of this study was to define the relationships of knee osteophyte formation with BMD and muscle mass. We aimed to determine whether the prevalence of radiographic knee osteophytes is increased with a high bone mass, or whether greater osteophyte formation is observed with a higher muscle mass.
Methods
A cross sectional study of the presence of knee osteophytes was conducted. The cases were defined as patients with osteophyte formation, and the controls were those without osteophyte formation.
Study group
Two-hundred and twenty-eight patients with knee pain [162 women, 66 men; mean age 72 years (range, 44–87 years)] were randomly selected for study. The patients fulfilled Kellgren JH, Lawrence JS criteria for classification for knee osteoarthritis [17]. All patients gave their informed written consent, and the study was approved by the Ethics Committee of Kaohsiung Chang Gung Memorial Hospital.
Radiographic assessment
Both knees of each patient were radiographed in a weight-bearing position. All radiographs were read consecutively by a single trained observer. A knee was classified as having radiographic knee osteophytes if one or more were found in either the medial or lateral tibiofemoral compartment or the patellofemoral compartment [18].
Bone mineral density evaluation (DXA)
The bone mineral densities of the lumbar spine, femoral neck, and total femur, along with the appendicular muscle mass and total fat mass, were assessed via DXA analysis using dual-energy X-ray absorptiometry [19].
Body composition study
Body composition was assessed using whole-body DXA (Lunar iDXA, GE Healthcare, Tokyo, Japan). Whole-body scans enabled assessment of the total lean body mass and total fat mass.
General characteristics, covariates, and comorbidities
The general characteristics of the subjects were ascertained via questionnaire to assess the presence of diseases, medications being taken, and lifestyle variables. Participants were asked to list their medications and diseases on a questionnaire completed at home, and research assistants then checked the questionnaires for completeness and accuracy in the presence of the participants. Detailed interviews were conducted in order to confirm the presence of specific diseases (e.g., osteoporosis, coronary heart disease, diabetes mellitus, OA) listed by the participants in close cooperation with the participants. In cases of doubt, written indications attested by the responsible doctor were requested.
The biochemical parameters examined included hemoglobin, urea, creatinine, calcium, phosphorus, and HbA1c.
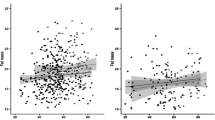
Statistical analysis
Continuous variables were compared between groups using t-tests, while associations between categorical variables were assessed using chi-squared tests. Logistic regression analyses were used to examine the associations between the presence of osteophytes and bone mineral density, muscle mass, and other parameters. A p value of less than 0.05 (two-tailed) or a 95% confidence interval (CI) not including the null point were regarded as indicating statistical significance. All statistical analyses were performed using SPSS Version 22.0 for Windows (Chicago, IL, USA).
Results
A total of 228 patients were enrolled, 78 of whom had osteophytes at the knee joint and 150 who did not. Female subjects were predominant in the osteophyte group (p = 0.001). The mean age was 73.23 ± 11.10 years in the osteophyte group and 71.86 ± 12.23 in the no osteophyte group (p = 0.409). The mean body mass index was 24.15 ± 3.27 kg/m2 in the osteophyte group and 23.37 ± 3.48 kg/m2 in the no osteophyte group (p = 0.433). More subjects in the osteophyte group had hypertension (p = 0.002), and the femoral neck T score was higher in the osteophyte group (p = 0.044). The characteristics of the patients are shown in Table 1. Using osteophytes as the outcome, logistic regression analysis showed that the male gender was associated with less osteophyte formation (p = 0.001, OR 0.11 (0.03–0.37)), and hypertension was associated with increased muscle loss (p = 0.005). So the age group 73 years expected to have OA and hypertension along other metabolic diseases, and the femoral neck T score was higher in the osteophyte group (p = 0.044). Femoral neck T score was associated with the presence of osteophyte formation (p = 0.011, OR 1.98 (1.17–3.36)) (Table 2). In this study, 43.2% had femoral neck T score < − 2.5.
Discussion
Our data showed that osteophyte formation was associated with a femoral neck T score, consistent with previous reports [3], and an increased BMD predisposes patients primarily to the bony features of OA. Hence, the relationship between OA and osteoporosis is consistent. Osteophyte formation was strongly associated with a femoral neck T score, as confirmed by pQCT study [20], and therefore, increased bone formation is a key feature in patients with a femoral neck T score. In addition, a literature review indicated that a bone mass is associated with significant comorbidities [21, 22]; therefore, the identification of comorbidities is important in patients with osteophyte formation.
A possible reason for a femoral neck BMD and osteophyte formation is altered joint loading secondary to an increased bone mass or as a result of an increased bone-formation response to a given load. These findings highlight that an altered bone response may contribute to the appearance of osteophytosis and increased bone mass. A high bone mass is associated with an increased risk of osteophytosis, which results in clinical end points of OA, such as joint replacement [21]. However, in this study, DXA was used to measure spine, total hip, and femoral neck, appendicular skeleton as distal radius, not knee, which differed from previous studies of the relationship between a high femoral BMD and hip osteophyte formation. Therefore, there may be a biological subtype of knee joint, and the biologic explanations of the increased bony proliferative response in these individuals include alterations in growth factor expressions [23], which are presumably related to genetic factors [24].
Our data also showed that osteophyte formation was not related to muscle mass. This differed from a previous German study, in which sarcopenia was found to be significantly more prevalent in participants with OA at the hip and lower limbs as compared with nonarthritic peers [13]. A definitive reason for a patient’s lower-limb weakness and predisposition to osteophyte formation were not found in our study. The results of a previous study indicating functional interaction of muscle and cartilage, and sharing of common pathological pathways by chondrocytes and skeletal muscle cells [25], were not observed in our study. Knee osteophyte formation may be independent of sarcopenia.
Our data showed that osteophyte formation was associated with hypertension.
This result was compatible with a Japanese study, in which hypertension as a metabolic factor was found to be associated with osteophyte formation [26]. In a Chinese cohort, metabolic factors including hypertension were found to be associated with knee osteophytes, but not with joint space narrowing [27]. In addition to a high prevalence of OA [18, 28, 29], Asian countries are seeing an increasing prevalence of metabolic syndrome due to changes in lifestyle over recent years [30]. Gandhi et al. [31] showed that the prevalence of metabolic syndrome in the Asian population was higher than in the white and black populations.
This was the first study to present evidence that hypertension is associated with radiographic knee osteophyte formation in a Taiwanese population. We speculate that the incidence and progression of hypertension and the presence of knee osteophytes are related to each other. This should be confirmed in further prospective cohort studies. In a previous study, knee osteoarthritis was found to be more frequent in obese women with cardiometabolic clustering than in those without [32]. If a patient is obese, insulin resistance and systemic inflammation might lead to fatigue and muscle weakness, which cause damage and affect repair mechanisms, resulting in the development of OA [33, 34]. In our study, there was no difference in BMI between the osteophyte group and the no osteophyte group. This may be due to the fact that osteophyte formation may precede other metabolic factors, or may occur via a different mechanism to other metabolic factors. Further study is needed for confirmation. Whatever the reason, the prevention of metabolic syndrome may be useful not only in reducing the risk of cardiovascular disease, but also in the prevention of knee OA, and may lead to a reduction in disability arising from joint disorders. In a review, hypertension in obese type 2 diabetes patients is associated with increases in insulin resistance and IL-6 cytokine levels [35]. While meta-analysis showed a relationship of common polymorphisms in IL-6, IL-1A, and IL-1B genes with susceptibility to osteoarthritis [36]. So these evidence may explain the reason of the risk for osteoarthritis.
In this study, osteophyte formation was observed to be more common in women, which has not been reported in previous literature. Lanyon et al. reported a decline in the hip joint space in women, but not in men; such changes may be related to sex differences in musculoskeletal aging, perhaps mediated through estrogen deficiency [37]. Estrogen is therefore an important factor related to osteophyte formation in the knee joint. These results have important implications for epidemiologic study, particularly in view of the major emphasis on osteophyte formation in the knee joint. Consideration should therefore be given to the development of sex-specific definitions of osteophyte formation.
There were some limitations of this study. The cross-sectional design precluded the drawing of causal correlations, and further prospective studies and intervention trials should therefore be undertaken to establish the causal associations between osteophyte formation and BMD, sarcopenia, and hypertension. In addition, the severity of osteophyte formation, knee deformities as valgus/Varus one, and hip-femur axis was not taken into account in this study, which may have limited expansion of the analysis in order to ascertain more realistic results and explanations. Furthermore, the sample size was relatively small, which may have limited its spread.
In conclusion, our results indicated associations of knee osteophyte formation with the femoral neck T score and hypertension, but not with muscle mass. We speculate that in patients with osteophytosis and an increased bone mass, metabolic factors such as hypertension need to be assessed. Further new insights into the molecular mechanisms regulating these processes are needed in the future.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- OA:
-
Osteoarthritis
- BMD:
-
Bone mineral density
- ACR:
-
American College of Rheumatology
- DXA:
-
Dual-energy X-ray absorptiometry
References
Kijowski R, Blankenbaker DG, Stanton PT, Fine JP, De Smet AA (2006) Radiographic findings of osteoarthritis versus arthroscopic findings of articular cartilage degeneration in the tibiofemoral joint. Radiology 239(3):818–824
van der Kraan PM, van den Berg WB (2007) Osteophytes: relevance and biology. Osteoarthritis Cartilage 15(3):237–244
Burger H, van Daele PL, Odding E, Valkenburg HA, Hofman A, Grobbee DE et al (1996) Association of radiographically evident osteoarthritis with higher bone mineral density and increased bone loss with age. Rotterdam Study Arthritis Rheum 39(1):81–86
Nevitt MC, Lane NE, Scott JC, Hochberg MC, Pressman AR, Genant HK, et al. (1995) Radiographic osteoarthritis of the hip and bone mineral density. The Study of Osteoporotic Fractures Research Group. Arthritis Rheum 38(7):907–16
Hannan MT, Anderson JJ, Zhang Y, Levy D, Felson DT (1993) Bone mineral density and knee osteoarthritis in elderly men and women. Framingham Study Arthritis Rheum 36(12):1671–1680
Hochberg MC (2004) Do risk factors for incident hip osteoarthritis (OA) differ from those for progression of hip OA? J Rheumatol Suppl 70:6–9
Dequeker J, Boonen S, Aerssens J, Westhovens R (1996) Inverse relationship osteoarthritis-osteoporosis: what is the evidence? What are the consequences? Br J Rheumatol 35(9):813–818
El-Sherif HE, Kamal R, Moawyah O (2008) Hand osteoarthritis and bone mineral density in postmenopausal women; clinical relevance to hand function, pain and disability. Osteoarthr Cartil 16(1):12–17
Hochberg MC, Lethbridge-Cejku M, Tobin JD (2004) Bone mineral density and osteoarthritis: data from the Baltimore Longitudinal Study of Aging. Osteoarthr Cartil 12 Suppl A:S45–8.
Schneider DL, Barrett-Connor E, Morton DJ, Weisman M (2002) Bone mineral density and clinical hand osteoarthritis in elderly men and women: the Rancho Bernardo study. J Rheumatol 29(7):1467–1472
Zoli A, Lizzio MM, Capuano A, Massafra U, Barini A, Ferraccioli G (2006) Osteoporosis and bone metabolism in postmenopausal women with osteoarthritis of the hand. Menopause 13(3):462–466
Milte R, Crotty M (2014) Musculoskeletal health, frailty and functional decline. Best Pract Res Clin Rheumatol 28(3):395–410
Kemmler W, Teschler M, Goisser S, Bebenek M, von Stengel S, Bollheimer LC et al (2015) Prevalence of sarcopenia in Germany and the corresponding effect of osteoarthritis in females 70 years and older living in the community: results of the FORMoSA study. Clin Interv Aging 10:1565–1573
Conroy MB, Kwoh CK, Krishnan E, Nevitt MC, Boudreau R, Carbone LD et al (2012) Muscle strength, mass, and quality in older men and women with knee osteoarthritis. Arthritis Care Res (Hoboken) 64(1):15–21
Waters RL, Campbell J, Perry J (1987) Energy cost of three-point crutch ambulation in fracture patients. J Orthop Trauma 1(2):170–173
Papalia R, Zampogna B, Torre G, Lanotte A, Vasta S, Albo E et al (2014) Sarcopenia and its relationship with osteoarthritis: risk factor or direct consequence? Musculoskelet Surg 98(1):9–14
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Ho-Pham LT, Lai TQ, Mai LD, Doan MC, Pham HN, Nguyen TV (2014) Prevalence of radiographic osteoarthritis of the knee and its relationship to self-reported pain. PLoS One 9(4):e94563
Celi M, Rao C, Scialdoni A, Tempesta V, Gasbarra E, Pistillo P et al (2013) Bone mineral density evaluation in osteoporosis: why yes and why not? Aging Clin Exp Res 25(Suppl 1):S47–S49
Gregson CL, Sayers A, Lazar V, Steel S, Dennison EM, Cooper C et al (2013) The high bone mass phenotype is characterised by a combined cortical and trabecular bone phenotype: findings from a pQCT case-control study. Bone 52(1):380–388
Hardcastle SA, Gregson CL, Deere KC, Davey Smith G, Dieppe P, Tobias JH (2013) High bone mass is associated with an increased prevalence of joint replacement: a case-control study. Rheumatology (Oxford) 52(6):1042–1051
Gregson CL, Paggiosi MA, Crabtree N, Steel SA, McCloskey E, Duncan EL et al (2013) Analysis of body composition in individuals with high bone mass reveals a marked increase in fat mass in women but not men. J Clin Endocrinol Metab 98(2):818–828
Felson DT, Neogi T (2004) Osteoarthritis: is it a disease of cartilage or of bone? Arthritis Rheum 50(2):341–344
Rogers J, Shepstone L, Dieppe P (1997) Bone formers: osteophyte and enthesophyte formation are positively associated. Ann Rheum Dis 56(2):85–90
De Ceuninck F, Fradin A, Pastoureau P (2014) Bearing arms against osteoarthritis and sarcopenia: when cartilage and skeletal muscle find common interest in talking together. Drug Discov Today 19(3):305–311
Yoshimura N, Muraki S, Oka H, Kawaguchi H, Nakamura K, Akune T (2011) Association of knee osteoarthritis with the accumulation of metabolic risk factors such as overweight, hypertension, dyslipidemia, and impaired glucose tolerance in Japanese men and women: the ROAD study. J Rheumatol 38(5):921–930
Xie DX, Wei J, Zeng C, Yang T, Li H, Wang YL et al (2017) Association between metabolic syndrome and knee osteoarthritis: a cross-sectional study. BMC Musculoskelet Disord 18(1):533
Kang X, Fransen M, Zhang Y, Li H, Ke Y, Lu M et al (2009) The high prevalence of knee osteoarthritis in a rural Chinese population: the Wuchuan osteoarthritis study. Arthritis Rheum 61(5):641–647
Salve H, Gupta V, Palanivel C, Yadav K, Singh B (2010) Prevalence of knee osteoarthritis amongst perimenopausal women in an urban resettlement colony in South Delhi. Indian J Public Health 54(3):155–157
Nestel P, Lyu R, Low LP, Sheu WH, Nitiyanant W, Saito I et al (2007) Metabolic syndrome: recent prevalence in East and Southeast Asian populations. Asia Pac J Clin Nutr 16(2):362–367
Gandhi R, Razak F, Tso P, Davey JR, Mahomed NN (2010) Asian ethnicity and the prevalence of metabolic syndrome in the osteoarthritic total knee arthroplasty population. J Arthroplasty 25(3):416–419
Sowers M, Karvonen-Gutierrez CA, Palmieri-Smith R, Jacobson JA, Jiang Y, Ashton-Miller JA (2009) Knee osteoarthritis in obese women with cardiometabolic clustering. Arthritis Rheum 61(10):1328–1336
Kornaat PR, Sharma R, van der Geest RJ, Lamb HJ, Kloppenburg M, Hellio le Graverand MP, et al. (2009) Positive association between increased popliteal artery vessel wall thickness and generalized osteoarthritis: is OA also part of the metabolic syndrome? Skeletal Radiol 38(12):1147–51
Rojas-Rodriguez J, Escobar-Linares LE, Garcia-Carrasco M, Escarcega RO, Fuentes-Alexandro S, Zamora-Ustaran A (2007) The relationship between the metabolic syndrome and energy-utilization deficit in the pathogenesis of obesity-induced osteoarthritis. Med Hypotheses 69(4):860–868
Cai H, Sun HJ, Wang YH, Zhang Z (2015) Relationships of common polymorphisms in IL-6, IL-1A, and IL-1B genes with susceptibility to osteoarthritis: a meta-analysis. Clin Rheumatol 34(8):1443–1453
Lukic L, Lalic NM, Rajkovic N, Jotic A, Lalic K, Milicic T et al (2014) Hypertension in obese type 2 diabetes patients is associated with increases in insulin resistance and IL-6 cytokine levels: potential targets for an efficient preventive intervention. Int J Environ Res Public Health 11(4):3586–3598
Lanyon P, Muir K, Doherty S, Doherty M (2003) Age and sex differences in hip joint space among asymptomatic subjects without structural change: implications for epidemiologic studies. Arthritis Rheum 48(4):1041–1046
Funding
This study was supported by Chang Gung Memorial Hospital and Chang Gung University College of Medicine (CMRPG8H0521). The funders had no role in study design, data collection and analysis, decision to publish, nor preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
KTW: study design, data collection, statistical analysis, and writing the paper; TTC: data collection; RWW, CCH: study design and writing the paper; YCC: corresponding author, study design, and writing the paper. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and with approval by the Institutional Review Board of Chang Gung Memorial Hospital, IRB No.: 201800414A3. Informed consent was obtained from the individuals who had joined the study.
Consent for publication
Informed written consent was provided by every participant.
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, KT., Wang, YW., Wu, RW. et al. Association of a femoral neck T score with knee joint osteophyte formation but not with skeletal muscle mass. Clin Rheumatol 42, 917–922 (2023). https://doi.org/10.1007/s10067-022-06410-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-022-06410-w