Abstract
Introduction/objectives
MiRSNPs may interfere with mRNA stability through effects on microRNAs (miRNAs)-mRNA interactions via direct changes in miRNA binding site or effect on the secondary structure of this region and changes in accessibility of this region to miRNAs. Studies have confirmed that an elevated level of interleukin-15 receptor alpha (IL-15RA) has an important role in the pathogenesis of systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA). In the present study, for the first time, we aimed to evaluate the possible correlation between a miRSNP, rs2296135, in IL-15RA gene with the risk of SLE and RA.
Methods
In this case–control study, 100 SLE patients, 100 RA patients, and 110 healthy participants were enrolled to assess rs2296135 genotypes with real-time PCR high-resolution melting method.
Results
According to our findings, AA genotype and A allele of rs2296135 were considerably associated with enhanced risk of RA (for AA genotype, OR = 2.29; 95% CI [1.06–5.02]; for A allele, OR = 1.65; 95% CI [1.10–2.48]). However, this common variant was not significantly correlated with SLE risk in population under study. Stratification analysis in the RA group verified that patients with the A allele had considerably higher serum concentrations of C-reactive protein (CRP) (P < 0.001). In SLE subjects, the frequency of arthritis (P: 0.021) and renal involvement (P: 0.025) in patients with A allele was significantly higher than in other SLE individuals.
Conclusion
The current study proposes a substantial association between rs2296135 polymorphism in IL-15RA gene with augmented risk of RA and some clinical characteristics in RA and SLE patients.
Key Points • Based on a literature review and search on miRSNP databases, we found that rs2296135 could be associated with dysregulation of IL-15RA expression via interfere with mRNA stability through effects on miRNA-mRNA interactions. • The current study for the first time disclosed a significant association between rs2296135 polymorphism with RA risk and clinical characteristics of SLE and RA. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA) are two highly prevalent multisystem autoimmune disorders that share many clinical manifestations and serological characteristics [1, 2]. These common rheumatic autoimmune diseases have a wide range of symptoms, could lead to disability, and are classified from mild to life-threatening [3]. SLE and RA are considered multifactorial disorders with > 60% heritability [4, 5]. Over the last decades, several genes and loci with their mechanism of pathogenesis have been noticed to be implicated in the predisposition of these autoimmune disorders [6,7,8]. Recently, with advances in genotyping methods such as genome-wide association studies (GWAS), the number of genetic loci and single nucleotide polymorphisms (SNPs) associated with the risk of SLE and RA has meaningfully expanded. Most of these SNPs are located in genes that are involved in immune system function and inflammatory response; therefore, with the effect on the expression or functions of these genes, they might modulate the occurrence of autoimmune diseases such as SLE and RA [9, 10].
miR-SNPs are a novel collection of SNPs that are located in or near microRNAs (miRNAs) binding site and could considerably contribute to the risk and development of diseases by dysregulation of miRNA-mRNA interactions through disruption of predicted miRNA target sites or change in the secondary structure of mRNA and consequently dysregulation of the expression of the target gene [11, 12]. Considering the connection between miRSNPs and miRNAs, susceptibility to specific diseases can be emanated as these types of polymorphisms which are located in the 3′-untranslated region (3′-UTR) of a target gene could modulate the expression of specific genes via enhancement, creation, disruption, or elimination of the binding efficacy of miRNAs at these regions and finally changes in mRNA stability [13, 14].
One of the important genes that have been reported to have a critical role in the pathogenesis of various autoimmune diseases is interleukin (IL)-15 and their receptor (IL-15 receptor α gene; IL-15RA) [15, 16]. Existing evidence has revealed the higher expression of IL-15 and IL-15RA in different samples from patients with SLE and RA as well as their important role in the pathogenesis of these diseases [17,18,19,20,21,22].
With regard to the importance of IL-15RA in the pathogenesis of SLE and RA, we searched the literature and miRSNPs databases to find a good candidate of miRSNP in this gene. One of these miRSNP, rs2296135, has been proposed as a possible modulator of interactions between miRNA and IL-15RA mRNA [23,24,25]. In the present case–control study, we aimed to estimate the possible relationship between rs2296135 polymorphism in the miRNA binding site of the IL-15RA gene with the risk of SLE and RA in the Iranian subjects. Furthermore, we assessed the correlation between this variant and the clinical parameters of these diseases including factors associated with disease activity and some clinical presentations.
Materials and methods
Criteria for selecting the polymorphism
Based on a literature review, we found that dysregulation of IL-15RA has a fundamental role in the pathogenesis of SLE and RA. Then, we carried out an extra literature review plus a thorough search on miRSNP database including miRNASNP-v3 (http://bioinfo.life.hust.edu.cn/miRNASNP#!/) [26] and miRdSNP (http://mirdsnp.ccr.buffalo.edu/) databases [27]. Next, using data from the 1000 Genomes project, we selected polymorphism with minor allele frequency (MAF) more than or equal to 0.05 (MAF ≥ 0.05). Subsequently, considering these basic principles, we nominated a polymorphism named rs2296135 (A > C) which is situated in miRNA target seed sites or in the near multiple predicted miRNA response elements (MREs) such as miR-2276, miR-4766, miR-2276, miR-509, miR-217, miR-488, miR-4766, and miR-4724. Finally, we hypothesize that rs2296135 may affect the ability of miRNAs to bind 3′UTR of IL-15RA mRNA and lead to dysregulation of this gene and consequently change the risk of SLE and RA diseases.
Subjects and blood sample collection
We included 100 patients with SLE, 100 patients with RA, and 110 healthy participants who were referred to the rheumatology division of Al-Zahra Hospital, Isfahan, Iran. Total cases had Iranian nation and met the American College of Rheumatology (ACR) (2019) and the European League Against Rheumatism (EULAR) diagnostic criteria [28]. Healthy controls, which had no signs and symptoms of these disorders, with no personal and/or family histories of immunological and autoimmune diseases were recruited in parallel from the same population. This study was approved by the ethics committee of Islamic Azad University, Tehran North Branch (ethical approval code: IR.IAU.TNB.REC.1400.099), and all subjects provided written informed consent before blood sample collection. We obtained all demographic, clinical features, and laboratory characteristics of all participants in this study using a structured questionnaire listed in Tables 1 and 2. Then, we obtained 3–5 ml of the venous blood samples from all volunteers and transferred them to EDTA anticoagulant tubes, and stored them at − 20 °C until further processing.
rs2296135 genotyping and statistics
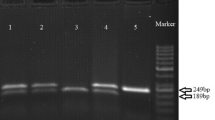
Genomic DNA was isolated from blood samples via the GeNet Bio DNA extraction Kit (Korea) according to the manufacturer’s protocol. We assessed the suitability of the extracted DNA for genotyping using spectrophotometric measurements and electrophoresis.
The real‑time polymerase chain reaction high‑resolution melting (HRM) method was used to determine rs2296135 polymorphism genotypes. This method was performed using HOT FIREPol EvaGreen HRM Mix (no ROX) HRM PCR kit, and HRM methodologies used for genotyping in the current study were performed as previously described [29, 30]. The HRM method was performed to amplify a fragment (173 bp) around rs2296135 under the following conditions: 5 min at 95 °C for initial denaturation for the first cycle, followed by 35 cycles of denaturation at 95 °C for the 20 s, annealing at 60 °C for 30 s, and extension at 72 °C for 20 s. Then, melting data was acquired on the LightCycler during a temperature ramp from 60 to 95 °C using 0.1 °C intervals.
All statistical analyses were accomplished by SPSS 25.0 (IBM SPSS Statistics 25 software (Armonk, NY: IBM Corp.)). Logistic regression analysis was achieved to examine the association among alleles and genotypes in cases and controls and compute specific odds ratios (ORs), 95% confidential intervals (CIs), and P values. For demographic, clinical, and laboratory characteristics, the univariate analysis was done via three independent tests, Mann–Whitney U-test, Pearson χ2 test, and Fischer Exact test wherever appropriate, and the significance level was set at P < 0.05.
Results
Characteristics of individuals
Subjects in the current study consisted of 22 males and 78 females in a group of patients with SLE, 27 males and 73 females in the RA group, and 32 males and 78 females in the control group. The mean age of participants at sampling was 43.18 ± 13.57 years for SLE, 47.56 ± 10.53 years for RA, and 45.25 ± 12.76 years for healthy control groups. There was no substantial variance among the patients (SLE and RA) and control groups in terms of age at sampling time (P Controls vs SLE: 0.255, P Controls vs RA: 0.154) and sex (P Controls vs SLE: 0.27, P Controls vs RA: 0.761), representing that for these parameters, matching was satisfactory. Between the patients (SLE and RA) and controls, there was a notable difference in terms of body mass index (BMI) (P < 0.001). Besides, SLE subjects had higher systolic blood pressure (SBP) (P: 0.014) and diastolic blood pressure (DBP) (P < 0.001) than controls. Data about the clinical manifestation of patients, especially in SLE groups, are presented in Table 1. Based on our laboratory findings, SLE patients compared with subjects in the control group had higher C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), creatinine, blood urea nitrogen (BUN), and anti‑dsDNA antibody level (P < 0.05), while the mean concentration of hemoglobin, platelet (PLT), complement component 3 (C3), and complement component 3 (C4) levels was meaningfully higher in the control group compared with the SLE patients (P < 0.05). In the RA group, serum concentrations of CRP, ESR, creatinine, and white blood cell count were significantly higher compared with RA-free subjects (P < 0.05). However, hemoglobin in RA patients was lower compared with controls (P < 0.001). The details of the laboratory factors of patients and control groups are documented in Table 2.
Correlation between rs2296135 with RA and SLE risk
In the RA cases, the frequency of the CC, AC, and AA was 29%, 39%, and 32%, respectively. In the control group, the frequency of the rs2296135 genotype was 41.8% for CC, 38.2% for AC, and 20% for AA. Moreover, the frequencies of C and A alleles were 48.5% and 51.5% in patients and 60.91% and 39.09% in controls, respectively. Statistical analysis established an important association between the rs2296135 variant and RA susceptibility. In detail, our findings showed that the AA genotype and A allele statistically increased the risk of RA (P < 0.05), while combined genotype analysis demonstrated that there is no obvious difference between individuals with AA and AC genotypes (AA + AC) with subjects with CC genotype in RA and healthy control group (P: 0.061). On the other hand, genotype and allele distribution in SLE subjects had no significant difference compared with controls (P > 0.05). The frequency of CC, AC, and AA genotypes in SLE patients was 42%, 37%, and 21%, respectively. Similarly, considering the combined genotypes, our findings confirmed that AC + AA genotypes did not affect the risk of RA pathogenesis compared to the CC genotype (P: 0.999). The genotype distribution and allele frequencies in subjects are shown in detail in Table 3.
Genotype stratification analysis
Stratification analysis in the RA group verified that patients with the A allele (AC + AA) had considerably higher serum concentrations of CRP (P < 0.001). Among RA patients, CRP level in individuals with risk allele (A) was 19.02 ± 15.34, while in RA participants with C allele (CC genotype) was 10.21 ± 6.14. However, there was no significant difference in genotype stratification in terms of age of onset, ESR, creatinine, hemoglobin, and BMI (P > 0.05).
In SLE subjects, the frequency of arthritis (P: 0.021) and renal involvement (P: 0.025) in patients with A allele (AC + AA) was significantly higher than subjects with CC genotype, while there was not any difference based on genotype stratification and other laboratory parameters and clinical manifestations in the SLE group (P > 0.05). The detailed findings of stratification analysis for the rs2296135 polymorphism in the RA and SLE groups are provided in Table 4.
Discussion
Until now, several GWAS studies reported hundreds of SNPs in many genes which are associated with susceptibility to autoimmune diseases, especially SLE and RA [8, 31,32,33]. SNPs, as the most abundant form of allelic variations in the human genome with appreciable frequency (> 1%), could be associated with disorders especially multifactorial autoimmune diseases [9, 34, 35]. SNPs in the 3′-UTR region of mRNA molecules may interfere with mRNA stability through effects on miRNA-mRNA interactions via direct changes in the miRNA binding site or effect on the secondary structure of this region and changes in accessibility of this region to miRNAs [11, 13, 14].
Multiple pieces of evidence demonstrated that IL-15RA along with IL-15 are increased in several autoimmune diseases and have an important role in their pathogenesis [15, 36]. IL15 is an unfavorable inflammatory cytokine that prompts the production of TNFα, IL-1ß, and some inflammatory chemokines. This cytokine regulates the activation and proliferation of T and natural killer cell and could inhibit self-tolerance by the mediation of IL-2 [15, 37]. Binding to the high specificity IL-15 receptor chain, interleukin-15 receptor α (IL-15Rα), is critical for IL-15 signaling function. In this way, previous experiments suggested the suppression of IL-15Rα as a therapeutic approach for the treatment of autoimmune diseases [37,38,39]. Previous studies showed an increased level of IL-15RA in leukocytes [40] and serum samples [18] of patients with SLE and similarly in synovial fluid of patients with RA [17].
Given the importance of the expression of IL-15RA in the pathogenesis of SLE and RA, we intended to evaluate the association of a miRSNP, rs2296135, in the 3′-UTR region of this gene with the risk of incidence of SLE and RA and some clinical characteristics of these disorders. Our findings confirmed a significant association between AA genotype and A allele in this variant with increased risk of RA in the population under study (ORfor AA genotype = 2.29; 95% CI [1.06–5.02], ORfor A allele = 1.65; 95% CI [1.10–2.48]). However, our results indicated that rs2296135 was not correlated with the modulation of SLE risk (Table 3). On the other hand, genotype stratification analysis in patient groups demonstrated that the A allele is correlated with an increased level of CRP in RA cases and also is correlated with higher frequencies of arthritis and renal involvement in SLE subjects (Table 4).
Despite data from miRSNP databases about the possible effect of rs2296135 on several predicted miRNA binding capacities and the role of IL-15RA in the pathogenesis of SLE and RA, this is the first report on the association of this common variant with SLE and RA. However, in some studies, the association of this polymorphism with irrelevant situations with autoimmune diseases such as metabolic syndrome and estrogen receptor-positive breast cancers has been demonstrated [41, 42].
Finally, the current study for the first time disclosed a significant association between rs2296135 polymorphism with RA risk in the Iranian population. Moreover, our findings showed that this variant is correlated with increased production of CRP, which is an indicator of disease activity in RA. Also, rs2296135 was meaningfully correlated with some clinical manifestations such as renal enrolments in SLE, which may represent higher disease severity in SLE patients. In this work, probably, some possible limitations in the statistical validity of our results such as small population size exist, so further association studies in larger sample size also would help to confirm the suggested correlations. Furthermore, in order to confirm the role of rs2296135 on the expression of IL15RA, it will be better to evaluate the effect of this variant on the expression level of IL15RA in patients and cell lines.
References
Pabón-Porras MA, Molina-Ríos S, Flórez-Suárez JB, Coral-Alvarado PX, Méndez-Patarroyo P, Quintana-López G (2019) Rheumatoid arthritis and systemic lupus erythematosus: pathophysiological mechanisms related to innate immune system. SAGE Open Med 7:2050312119876146. https://doi.org/10.1177/2050312119876146
Frade-Sosa B, Narváez J, Salman-Monte TC, Castellanos-Moreira R, Ortiz-Santamaria V, Torrente-Segarra V, Castellvi I, Magallares B, Reina D, Minguez S (2020) A comparative study on clinical and serological characteristics between patients with rhupus and those with systemic lupus erythematosus and rheumatoid arthritis. Lupus 29(10):1216–1226
Icen M, Nicola PJ, Maradit-Kremers H, Crowson CS, Therneau TM, Matteson EL, Gabriel SE (2009) Systemic lupus erythematosus features in rheumatoid arthritis and their effect on overall mortality. J Rheumatol 36(1):50–57. https://doi.org/10.3899/jrheum.080091
Moser KL, Kelly JA, Lessard CJ, Harley JB (2009) Recent insights into the genetic basis of systemic lupus erythematosus. Genes Immun 10(5):373–379
Okada Y, Eyre S, Suzuki A, Kochi Y, Yamamoto K (2019) Genetics of rheumatoid arthritis: 2018 status. Ann Rheum Dis 78(4):446–453
Seldin MF (2015) The genetics of human autoimmune disease: a perspective on progress in the field and future directions. J Autoimmun 64:1–12. https://doi.org/10.1016/j.jaut.2015.08.015
Zeinalzadeh S, Kheradmand N, Rasouli G, Esmaeilzadeh E, Pakzad B, Behroozi J, Chamanara M, Zoshk MY, Ehtesham N, Sabet MN (2022) Association of a miRNA-binding site polymorphism in IL-16 gene with disease risk and clinical characteristics of rheumatoid arthritis and systemic lupus erythematosus. Clin Rheumatol 41:2189–2196
Kwon Y-C, Chun S, Kim K, Mak A (2019) Update on the genetics of systemic lupus erythematosus: genome-wide association studies and beyond. Cells 8(10):1180
Ye J, Gillespie KM, Rodriguez S (2018) Unravelling the roles of susceptibility loci for autoimmune diseases in the post-GWAS era. Genes (Basel) 9(8):377. https://doi.org/10.3390/genes9080377
Suzuki A, Guerrini MM, Yamamoto K (2021) Functional genomics of autoimmune diseases. Ann Rheum Dis 80(6):689–697
Karimzadeh MR, Zarin M, Ehtesham N, Khosravi S, Soosanabadi M, Mosallaei M, Pourdavoud P (2020) MicroRNA binding site polymorphism in inflammatory genes associated with colorectal cancer: literature review and bioinformatics analysis. Cancer Gene Ther 27(10):739–753
Liu C, Zhang F, Li T, Lu M, Wang L, Yue W, Zhang D (2012) MirSNP, a database of polymorphisms altering miRNA target sites, identifies miRNA-related SNPs in GWAS SNPs and eQTLs. BMC Genom 13(1):661. https://doi.org/10.1186/1471-2164-13-661
Hu Z, Bruno AE (2011) The influence of 3′ UTRs on MicroRNA function inferred from human SNP data. Comp Funct Genom 9p:1–9
Yuan Y, Weidhaas JB (2019) Functional micro RNA binding site variants. Mol Oncol 13(1):4–8
Allard-Chamard H, Mishra HK, Nandi M, Mayhue M, Menendez A, Ilangumaran S, Ramanathan S (2020) Interleukin-15 in autoimmunity. Cytokine 136:155258. https://doi.org/10.1016/j.cyto.2020.155258
Waldmann TA (2004) Targeting the interleukin-15/interleukin-15 receptor system in inflammatory autoimmune diseases. Arthritis Res Ther 6(4):174–177. https://doi.org/10.1186/ar1202
Machado Diaz AC, Capote AC, Arrieta Aguero CA, Alvarez YR, del Barco Herrera DG, Del Toro ME, Guillen Nieto GE, Savio AS (2012) Proinflammatory soluble interleukin-15 receptor alpha is increased in rheumatoid arthritis. Arthritis 943156:1–6
Aringer M, Stummvoll G, Steiner G, Köller M, Steiner C, Höfler E, Hiesberger H, Smolen J, Graninger W (2001) Serum interleukin-15 is elevated in systemic lupus erythematosus. Rheumatol 40(8):876–881
Baranda L, De La Fuente H, Layseca-Espinosa E, Portales-Perez D, Nino-Moreno P, Valencia-Pacheco G, Abud-Mendoza C, Alcocer-Varela J, Gonzalez-Amaro R (2005) IL-15 and IL-15R in leucocytes from patients with systemic lupus erythematosus. Rheumatol 44(12):1507–1513
Lin S-J, Kuo M-L, Hsiao H-S, Lee P-T, Lee W-I, Chen J-Y, Huang J-L (2019) Cytotoxic function and cytokine production of natural killer cells and natural killer T-like cells in systemic lupus erythematosis regulation with interleukin-15. Mediat Inflamm 8:1–12
Oppenheimer-Marks N, Brezinschek RI, Mohamadzadeh M, Vita R, Lipsky PE (1998) Interleukin 15 is produced by endothelial cells and increases the transendothelial migration of T cells In vitro and in the SCID mouse-human rheumatoid arthritis model In vivo. J Clin Investig 101(6):1261–1272
Park YB, Kim DS, Lee WK, Suh CH, Lee SK (1999) Elevated serum interleukin-15 levels in systemic lupus erythematosus. Yonsei Med J 40(4):343–348. https://doi.org/10.3349/ymj.1999.40.4.343
Wu D, Yang G, Zhang L, Xue J, Wen Z, Li M (2014) Genome-wide association study combined with biological context can reveal more disease-related SNPs altering microRNA target seed sites. BMC Genomics 15(1):1–13
Bruno AE, Li L, Kalabus JL, Pan Y, Yu A, Hu Z (2012) miRdSNP: a database of disease-associated SNPs and microRNA target sites on 3’UTRs of human genes. BMC Genomics 13(1):44. https://doi.org/10.1186/1471-2164-13-44
Liu C, Zhang F, Li T, Lu M, Wang L, Yue W, Zhang D (2012) MirSNP, a database of polymorphisms altering miRNA target sites, identifies miRNA-related SNPs in GWAS SNPs and eQTLs. BMC Genomics 13(1):1–10
Liu C-J, Fu X, Xia M, Zhang Q, Gu Z, Guo A-Y (2021) miRNASNP-v3: a comprehensive database for SNPs and disease-related variations in miRNAs and miRNA targets. Nucleic Acids Res 49(D1):D1276–D1281
Bruno AE, Li L, Kalabus JL, Pan Y, Yu A, Hu Z (2012) miRdSNP: a database of disease-associated SNPs and microRNA target sites on 3′UTRs of human genes. BMC Genomics 13(1):1–7
Aringer M, Costenbader K, Daikh D, Brinks R, Mosca M, Ramsey-Goldman R, Smolen JS, Wofsy D, Boumpas DT, Kamen DL (2019) 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Arthritis & Rheumatol 71(9):1400–1412
Hassani M, Dehani M, Rafie MZ, Esmaeilzadeh E, Davar S, Pakzad B, Mosallaei M, Hoseini SM, Bayat H, Soosanabadi M (2021) Investigation of rs531564 polymorphism in the primary microRNA-124 gene in patients with systemic lupus erythematosus and rheumatoid arthritis: association with disease susceptibility and clinical characteristics. Iranian J Allergy Asthma Immunol 20(3):303–313
Ehtesham N, Zare Rafie M, Esmaeilzadeh E, Dehani M, Davar S, Mosallaei M, Pakzad B, Ghorashi T, Darvish H, Soosanabadi M (2021) Three functional variants in the NLRP3 gene are associated with susceptibility and clinical characteristics of systemic lupus erythematosus. Lupus 30(8):1273–1282
Lessard CJ, Ice JA, Adrianto I, Wiley GB, Kelly JA, Gaffney PM, Montgomery CG, Moser KL (2012) The genomics of autoimmune disease in the era of genome-wide association studies and beyond. Autoimmun Rev 11(4):267–275
Caliskan M, Brown CD, Maranville JC (2021) A catalog of GWAS fine-mapping efforts in autoimmune disease. Am J Hum Genet 108(4):549–563
Karami J, Aslani S, Jamshidi A, Garshasbi M, Mahmoudi M (2019) Genetic implications in the pathogenesis of rheumatoid arthritis; an updated review. Gene 702:8–16
Gualtierotti R, Biggioggero M, Penatti A, Meroni P (2010) Updating on the pathogenesis of systemic lupus erythematosus. Autoimmun Rev 10(1):3–7
Mosallaei M, Simonian M, Ahangari F, Miraghajani M, Mortazavi D, Salehi AR, Khosravi S, Salehi R (2018) Single nucleotide polymorphism rs4648298 in miRNAs hsa-miR21 and hsa-miR590 binding site of COX gene is a strong colorectal cancer determinant. J Gastrointest Oncol 9(3):448–457
Zhao L, Hu B, Zhang Y, Song Y, Lin D, Liu Y, Mei Y, Sandikin D, Sun W, Zhuang M, Liu H (2016) An activation-induced IL-15 isoform is a natural antagonist for IL-15 function. Sci Rep 6(1):25822. https://doi.org/10.1038/srep25822
Waldmann TA (2004) Targeting the interleukin-15/interleukin-15 receptor system in inflammatory autoimmune diseases. Arthritis Res Ther 6(4):1–4
Baranda L, de la Fuente H, Layseca-Espinosa E, Portales-Pérez D, Niño-Moreno P, Valencia-Pacheco G, Abud-Mendoza C, Alcocer-Varela J, González-Amaro R (2005) IL-15 and IL-15R in leucocytes from patients with systemic lupus erythematosus. Rheumatol (Oxford) 44(12):1507–1513. https://doi.org/10.1093/rheumatology/kei083
Ruchatz H, Leung BP, Wei X-q, McInnes IB, Liew FY (1998) Soluble IL-15 receptor α-chain administration prevents murine collagen-induced arthritis: a role for IL-15 in development of antigen-induced immunopathology. J Immunol 160(11):5654–5660
Baranda L, de la Fuente H, Layseca-Espinosa E, Portales-Pérez D, Niño-Moreno P, Valencia-Pacheco G, Abud-Mendoza C, Alcocer-Varela J, González-Amaro R (2005) IL-15 and IL-15R in leucocytes from patients with systemic lupus erythematosus. Rheumatol 44(12):1507–1513. https://doi.org/10.1093/rheumatology/kei083
Pistilli EE, Devaney JM, Gordish-Dressman H, Bradbury MK, Seip RL, Thompson PD, Angelopoulos TJ, Clarkson PM, Moyna NM, Pescatello LS (2008) Interleukin-15 and interleukin-15Rα SNPs and associations with muscle, bone, and predictors of the metabolic syndrome. Cytokine 43(1):45–53
Quan L, Gong Z, Yao S, Bandera EV, Zirpoli G, Hwang H, Roberts M, Ciupak G, Davis W, Sucheston L (2014) Cytokine and cytokine receptor genes of the adaptive immune response are differentially associated with breast cancer risk in American women of African and European ancestry. Int J Cancer 134(6):1408–1421
Acknowledgements
We thank all subjects who participated in this study also We would like to appreciate any support provided by Islamic Azad University, Tehran North Branch.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jadidi, ., Alesaeidi, ., Arab, . et al. miRNA-binding site polymorphism in IL-15RA gene in rheumatoid arthritis and systemic lupus erythematosus: correlation with disease risk and clinical characteristics. Clin Rheumatol 41, 3487–3494 (2022). https://doi.org/10.1007/s10067-022-06298-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-022-06298-6