Abstract
Objectives
Factors associated with disease activity of axial spondyloarthritis (axSpA) and switching of biologic disease-modifying anti-rheumatic drugs have not been clearly defined. We aimed to evaluate clinical characteristics of patients with axSpA, factors related to remission in treat to target era and predictive factors for biologic disease-modifying anti-rheumatic drug switching.
Method
A multicenter, observational cross-sectional study was performed between February 2019 and August 2019. We included all consecutive patients ≥ 18 years with axSpA. Demographic and clinical variables were prospectively recorded. Clinical tools included Ankylosing Spondylitis Disease Activity Score with C-reactive protein (ASDAS-CRP), Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), Bath Ankylosing Spondylitis Metrology Index (BASMI), and Maastricht Ankylosing Spondylitis Enthesitis Score (MASES).
Results
There were 969 patients with a mean age of 43.4 ± 10.8 years. There were 143 patients (14.8%) with remission and 223 (23.1%) patients with low disease activity. Male sex (p = 0.021), positive family history (p = 0.036), and human leukocyte antigen-B27 (p = 0.011) were predictors of remission by ASDAS-CRP. There were 654 patients (67.5%) who did not switch to another drug. The highest BASMI and MASES scores were calculated in patients with very high disease activity (p < 0.05). In patients with drug switching, the disease duration was significantly higher (p < 0.001) and the age at diagnosis was significantly lower (p = 0.016). There were significantly more patients with uveitis and higher scores of MASES and BASMI in patients who switch to another biologic disease-modifying anti-rheumatic drugs (p = 0.003, p = 0.009, and p = 0.004, respectively).
Conclusions
In patients with axSpA, male sex, younger age, and HLA-B27 positivity are associated with remission, while longer disease duration and accompanied uveitis appear to be related with drug switching.
Clinical trial registration number and date
NCT04139954/25.10.2019.
Key Points • Achievement of remission and/or low disease activity rates in patients with axSpA were assessed in a big registry from a real-life data. • Predictive factors for switching to another bDMARD were evaluated in axSpA patients. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Treatment of axial spondyloarthritis (axSpA) with two different dimensions, as radiographic and non-radiographic, has included several challenges concerning therapeutic options and their clinical responses [1, 2]. Biologic disease-modifying anti-rheumatic drugs (bDMARDs) have been used in patients with axSpA if they have clinically active disease or objective signs of inflammation unresponsive to the non-steroidal anti-inflammatory drugs (NSAIDs) [2, 3]. Their use has changed approaches for articular and extra-articular manifestations of rheumatic diseases such as uveitis, psoriasis, and inflammatory bowel disease [2, 4].
Clinical response to bDMARD treatment has been studied previously, focusing on disease activity and disease progression [2]. In these studies, several factors, including shorter disease duration, younger age, elevated C-reactive protein (CRP), male sex, and presence of human leukocyte antigen (HLA)-B27, are reported as the predictors of clinical response and remission [3, 4]. However, many controversial findings indicate none of these factors, alone or in combination, cannot be regarded as adequate to tailor the treatment [5].
Development of primary or secondary failure to bDMARDs and serious adverse effects may necessitate switching to another therapeutic option. No significant differences in patients with and without switching for failure or adverse events have been detected [6, 7]. So, the prediction of switchers remains a controversial issue for axSpA.
Evaluation of disease activity and management in patients with axSpA is quite complicated due to factors such as enthesitis, dactylitis, and extra-articular involvement such as uveitis or intestinal involvement [8]. The Ankylosing Spondylitis Disease Activity Score (ASDAS) blended with CRP covers multiple disease activity dimensions [2]. Besides, other clinical tools, including the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), the Bath Ankylosing Spondylitis Metrology Index (BASMI) for assessment of spinal mobility, and The Maastricht Ankylosing Spondylitis Enthesitis Score (MASES), for the assessment of enthesitis have also been used [9].
Treat to target (T2T) defined as a treatment strategy in which the patient achieved sufficiently aggressively treatment to obtain inactive disease. Minimal/low disease activity is another option in patients with long-term disease, comorbidities, and resistance to treatment. Periodic evaluation of disease activity and tight disease follow-up are expected to be associated with better outcomes for axSpA. Tight disease follow-up should be in accordance with acute phase reactants, patient reported outcomes, and composite scales [10].
In this multicentered study, we aimed to evaluate the demographic and clinical characteristics of axSpA patients in association with disease severity and where we are in the T2T era. We also aimed to determine the predictive factors for switching to another bDMARD in the same patient group real-life data.
Materials and methods
Study
A multicenter, observational cross-sectional study evaluated the patients with axSpA between February 2019 and August 2019 using Biologic and targeted Synthetic anti-rheumatic drugs Registry (BioStaR) SpA. It was a multicenter, nationwide registry about biologic treatment on SpA. There were 14 centers from Turkey. The local ethical committee approved the study (Turkey Medicines and Medical Devices Agency, 66,175,679–514.99-E.6366, and Ankara Numune Training and Research Hospital Ethics Committee, E-182413). All procedures were in accordance with the Helsinki Declaration of 1964 and later versions. Written informed consent was taken from the participants or from the legally authorized representatives for the participants who were illiterate or vulnerable.
Patients
We included all consecutive patients ≥ 18 years with axSpA. All patients included in the study were evaluated and diagnosed by a rheumatologist or physical medicine and rehabilitation specialist. Patients met the Assessment of SpondyloArthritis international Society (ASAS) criteria and patients were evaluated as non-radiographic axSpA and radiographic axSpA [11, 12]. Cognitive disorders prevent the reply to the scales and the questionnaires; skin disorders other than psoriasis, chronic hepatic/renal diseases, coexisting rheumatic diseases, malignancy, pregnancy, breastfeeding, refusal to participate in the study, and missing data were the exclusion criteria.
Evaluation of disease activity
The disease activity was classified based on the ASDAS-CRP [10]. The disease activity groups were remission (< 1.3), low disease activity (1.3 to < 2.1), high disease activity (2.1–3.5), and very high disease activity (> 3.5) [13, 14].
Erythrocyte sedimentation rate (ESR) (mm/h) and CRP (mg/dL) were also measured as acute phase reactants.
Variables
Demographics, including age, sex, body mass index (BMI), educational and marital status, smoking, family history of SpA, and presence of comorbidities, were recorded using a prospective database. The educational status was classified as illiterate or primary, secondary or high school, and university or higher. The parameters related to SpA such as disease duration, symptom duration, age at the diagnosis, age at the initiation of the symptoms, type of AxSpA as radiographic and non-radiographic, HLA-B27 status, and the presence of extra-articular manifestations (uveitis, psoriasis, inflammatory bowel disease), enthesitis, and dactylitis were recorded.
Previous and current drugs used for axSpA including conventional and biological DMARDs and non-steroidal agents were noted. We analyzed the status of drug switching from a bDMARD to another bDMARD. The reasons for discontinuing drugs and switching patients to a different biologic drug were also classified into two major categories: inefficiency and adverse effects.
Outcome measures
At the inclusion of the study, data concerning the patient’s score reported outcomes were collected at a single time point. The clinical tools used in the study included BASDAI, MASES, BASMI, VAS global patient and VAS global physician, and tender and swollen joint counts.
The MASES considers tenderness on examining 13 enthesis sites, graded from 0 to 3 (0 = no pain; 1 = mild tenderness; 2 = moderate tenderness; 3 = wince or withdraw). The total range is from 0 to 39 [14]. The BASMI linear score (cervical rotation, tragus-wall distance, lateral lumbar flexion, modified Schober, intermalleolar distance measured) was used to assess mobility with a range of 0–10. Higher scores reflect worse mobility [14]. The patient’s global assessment has been developed to reflect the impact of the axSpA on the patient’s well-being. It consists of a single question: “How active was your spondylitis on average during the last week?” [15]. For peripheral joint assessment, tender (68 joints) and swollen (66 joints) joint counts were calculated separately.
Statistical analysis
All categorical variables were summarized with frequencies and percentages. In contrast, the numerical variables were summarized with mean and standard deviations (SD) or medians and interquartile ranges (Q1, Q3) according to their distributions in addition to minimum and maximum values. The numerical variables were analyzed across two groups with Mann–Whitney U test or t-test and three groups by Kruskal–Wallis test or ANOVA depending on their distribution. The assumption of normality was assessed with Shapiro–Wilk test in addition to visual inspection by Q-Q and PP plots. The homogeneity of variance was assessed using Levene’s test. The significant group comparisons for three or more groups were performed using the post hoc tests. Pairwise comparisons were conducted using the Mann–Whitney U test, and Benjamini–Hochberg adjusted p-values were evaluated. Odds ratios and corresponding 95% confidence intervals were calculated for the parameters associated with remission. A p-value smaller than 0.05 represents statistical significance. The R version 4.0.2 (2020–06-22) was employed for all analyses.
Results
There were 969 patients with a mean age of 43.4 ± 10.8 years. The male-to-female ratio was 2.54. Secondary-high school was the most common educational status seen in 55.4% of the study group patients. Almost half of the patients (45.3%) were non-smoker. In 261 patients (27.0%), there was positive family history of SpA. The initial median level of ESR was 13 (6.0–26) mm/h, and the CRP level was 4 (2.1–10) mg/L. The demographic and clinical findings of the study are given in Table 1.
According to ASDAS-CRP, low disease activity was found in 223 (23.0%) patients and there were 143 patients (14.8%) with remission. The disease characteristics according to the different severity groupings are detailed in Table 1.
There were significant differences in sex, educational status, and family history of SpA between the different disease severity groups. The male-to-female ratio was higher in patients with remission and moderate disease activity than the other groups (p = 0.014). Positive family history of SpA was more frequently detected in patients with remission and moderate disease activity (p = 0.036). Other demographic and clinical findings were similar between the groups (p > 0.05).
In the overall study group, a total of 473 patients’ HLA-B27 results were obtained and the HLA-B27 positivity was detected in 174 (36.8%) patients. But there were significantly more HLAB-27-positive patients in the remission group (p = 0.005).
Analysis of the clinical tools with different disease severity groups revealed significant associations (Table 2). As the disease severity increased from moderate to very severe disease, the clinical tools’ score also significantly increased. The highest scores of the MASES, BASMI, VAS global patient, and VAS global physician were calculated in patients with very high disease activity (p < 0.05 for all). The lowest scores were detected in patients with remission. The BASMI scores for moderate, high, and very high disease activity were significantly higher than those in the remission group. The scores of the VAS global patient and VAS global physician had increasing trends from remission to very severe disease activity group. The median number of the tender joints was significantly higher in patients with high and very high disease activity (p < 0.001). There were more frequently swollen joints in patients with very severe disease compared to the patients’ remission (p = 0.013). There were no significant differences between the other groups. In the study group, there were 654 patients (67.5%) who did not switch to another drug. Remission rates were lower in the group that switched to another bDMARD treatment compared to non-switchers (9.2%; 17.4% respectively) (Table 2).
The median duration of the current bDMARD was higher in patients with remission and moderate disease activity than the other groups (p < 0.001). The use of concomitant NSAID was more frequently seen in patients with very high disease activity (p < 0.001) (Table 2).
Odds ratios were calculated for the parameters associated with remission. Male sex and HLA-B27 positivity were associated with remission (male sex: odds ratio 1.74 (95% CI: 1.12–2.70; p = 0.013); positive family history: odds ratio 1.24 (95% CI: 0.84–1.83; p = 0.263); HLA-B27 positivity: odds ratio 1.63 (95% CI: 1.05–1.52, p = 0.027)).
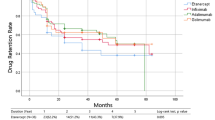
The list of all drugs and their distribution based on the drug switching status are given in Table 3. A total of 315 patients (32.5%) were in the drug switcher group; 236 patients (74.9% of the switchers) switched to a second bDMARD, and 79 patients (25.1% of the switchers) were treated with a third bDMARD. Among the cDMARDs, sulfasalazine was the most frequently used drug seen in 619 patients (63.9%). In 86 patients (8.9%), we detected the use of methotrexate. Adalimumab (43.1%), etanercept (40.4%), and golimumab (28.8%) were the most common bDMARDs used in the study group.
The disease characteristics according to the status of switching are summarized in Table 4. The median disease duration was 89 months in non-switcher patients. In patients with drug switching, the length of the disease duration was significantly higher than that of non-switcher patients (p < 0.001). The age of diagnosis was significantly higher in patients without drug switching (p = 0.016). Other clinical features except for uveitis were similar (p > 0.05). More patients with uveitis in both groups switch to the second and third bDMARD (p = 0.003).
In patients with remission, 79.7% of the cases were non-switcher. The measurement of ESR showed no difference between the drug groups (p = 0.179). CRP was significantly different between the groups (p < 0.001). There was a significant increasing trend from remission to very high disease activity group. The mean ASDAS-CRP score was significantly higher in the switcher patients to third bDMARD (p < 0.001). There were significantly higher scores of the MASES and BASMI in patients who switched to the third bDMARD than the other patients (p = 0.009 and p = 0.004). Other outcome measures showed similar results in patients with non-switcher and switchers (Table 5).
The reasons for switching of bDMARD are detailed in Table 6. The overall ineffectiveness (64.8%) and adverse effects (22.9%) were the most frequent reasons for drug switching in patients who switch to the second bDMARD.
Discussion
The concept of T2T has become a current issue also in the area of axSpA, with the assertive target of clinical remission [8]. Widespread confirmation of the real-life prevalence of remission and factors related with remission are still not enough. This study, presenting multicenter nationwide real-life data, showed that male sex and HLA-B27 were the predictors of remission in patients with axSpA and positive family history of axSpA was detected more frequently in remission. Moreover, there were significant associations between drug switching and disease duration, age at diagnosis, and uveitis in AxSpA patients.
Different parameter sets with variable factors, including ASDAS, ASAS, and BASDAI, have been used for predicting clinical response in axSpA patients [1, 3]. The ASAS partial remission criteria were the most widely used system for the definition of clinical remission [5]. It is a matter of debate because it is purely subjective and lacks objective indicators for disease activity. As a composite score, ASDAS-CRP has been considered a better index than the others [3,4,5]. CRP is an objective measure of inflammation and has validated cut-offs for various levels of disease activity. Combining the scores of clinical tools with CRP causes some improvement, which is the main advantage of ASDAS [16]. It can also differentiate between complete remission and low disease activity [5]. Therefore, consistent with others, we chose ASDAS-CRP as the sole predictor for remission in this study [5, 17].
In our cohort of the 969 patients treated with bDMARD, remission with ASDAS was noted in 143 (14.8%) patients and low disease activity was in 223 (23.1%) patients. The rates of remission and low disease activity were similar in the non-radiographic and radiographic groups; on the other hand, remission rates were lower in the group that switched to another bDMARD treatment compared to non-switchers (9.2%; 17.4% respectively). In the ABILITY-1 clinical trial with adalimumab versus placebo, 15% of 176 patients achieved ASDAS remission [18]. In the GO-RAISE study with golimumab, the percentage of patients classified as ASDAS remission after 24 weeks of treatment was 27.3% [19]. ASAS partial remission has been achieved in 20–40% of patients with SpA treated with tumor necrosis factor (TNF) inhibitor, while partial remission rates increase up to 60% ongoing regular treatment with a TNF inhibitor. After switching to a second TNFi, the chance of achieving the remission decreases again to 40.5% [20] and Monti et al. found 40.8% remission rate in their cohort with 218 patients [8]. It is known that ASDAS remission, together with the acute phase reactant, is less frequently achieved compared to more traditional indices, especially BASDAI, which is still shown as an alternative disease activity measure. Direct comparison with previous studies is difficult due to the lack of a unique definition of remission and a fine distinction between complete clinical remission and a state of low disease activity.
HLA-B27 has an essential role in axSpA classification and exists in nearly 6–8% of the general population and in 80–95% of AS patients in western European and North American populations. On the other hand, the prevalence of HLA-B27 in axSpA patients is found to be lower in Arab and Middle Eastern populations [21]. When we look at the prevalence of HLA-B27 in patients with axSpA, it was shown to be 41.1% in the Lebanese population and 45.3% in the Moroccan population, although it was found to be 78.4% in the COMOSPO database [21,22,23]. Although the prevalence of HLA-B27 was not investigated in our study, in which a real-life data was compiled, the frequency of HLA-B27 in our patients with axSpA was 36.8%. This frequency has been found to be lower than the European population and reflects the genetic background of our geographic region.
We found that male sex, educational status of secondary-high school, positive family history of SpA, and positive HLA-B27 status were associated with remission. Besides, we also detected the increasing trends of the MASES and BASMI scores from remission to very severe disease activity. In previous studies, younger age, male sex, smoking, HLA-B27, lower BASDAI and BASMI scores, and shorter disease duration were the significant predictors for good clinical response and remission [3, 4, 24, 25]. There were controversial results about the association between these severity scores and the remission [3, 4]. Some authors reported that the patients with low disease activity were older than the others [26]. Based on the presence of great variations, the results should be interpreted with caution. Studies have heterogeneous features such as inclusion of radiographic or non-radiographic axSpA patients and different bDMARDs [1, 3, 4, 27, 28]. We believe that such differences may have a negative impact on the generalizability of the results.
Switching during the medical treatment of rheumatic diseases was a frequent event due to lack or loss of efficiency or development of side effects [4]. In our study, switching from one type of bDMARD to another drug occurred in 32.5% of the cases, consistent with previous outcomes [4]. Several demographic and baseline disease parameters such as female sex, methotrexate use, and higher BASFI and BASDAI scores have been defined as the relevant predictive factors for switching [29]. In enthesitis-related juvenile-type arthritis, shorter disease duration and HLA-B27 were more frequently seen in patients who were responsive to DMARD treatment [24]. But, Shimabuco et al. [4] found no factor in predicting remission in patients using tumor necrosis factor inhibitors. They identified that higher BASDAI reflecting a refractory disease might be a predictive factor for switching from the second anti-TNF agent to the third. In the present study, we found that the non-switcher patients have had a significantly shorter disease duration. We also showed that the age at the diagnosis was significantly higher in patients with remission. The differences in these studies were most probably originated because of the different study characteristics. So, prospective large-scale, multicenter studies with homogenous inclusion criteria are needed to resolve such controversial issues.
It is known that the prevalence of enthesitis is quite high in spondyloarthritis and it has been reported with a frequency ranging from 51 to 81% in spondyloarthritis [30, 31]. The MASES score is regarded as a reflection of the severity of enthesitis, which is also used to evaluate anti-tumor necrosis factor treatment response and therapeutic follow-up for biological treatments [30]. Enthesitis was also reported as a common feature of the patients who switched to TNF inhibitor treatment and it has also been shown that MASES scores reduce after bDMARD treatments in axSpA patients [32, 33]. However, there is no data about any association between the MASES score and switching one bDMARD to another. We found higher MASES scores in patients switching to the third bDMARD in our study. Higher MASES scores in the switcher patients might be due to the autoimmune or inflammatory mechanisms of axSpA that necessitates future studies. However, we think that higher MASES scores or other clinical variables indicating higher grades of enthesitis might be clinical evidences for unresponsiveness to the medical treatment in axSpA patients.
Uveitis is one of the common extra-articular manifestations of axSpA. Several studies have documented the efficacy of TNF inhibitors in reducing the uveitis attacks in patients with spondyloarthritis. On the other hand, some studies have mentioned that TNF inhibitors may induce new-onset uveitis as a paradoxical side effect [34]. In our study, comparison of with different switching status revealed that the incidence of uveitis was higher in the switcher patients. In addition, paradoxical uveitis was reported in 11 of 236 switcher to second biological patients. Although paradoxical uveitis does not seem to be one of the main reasons for drug switch, further analyses will be obtained with a larger number of patients and long-term follow-up of patients may be more beneficial in clarification of the complicated relationship between TNF inhibition and uveitis.
The inclusion of patients from different centers as a nationwide project was the primary strength of the study. This issue is an essential point for the generalization of the findings. Although we used objective measures to determine clinical remission, the patients’ open-label inclusion without any limit for each center may be necessary, leading to selection bias. Besides, some missing data can bias the results. On the other hand, 6-month regular visits of patients still continue to BioStaR registry and analyses with data on biological tapering in the assessment of disease outcomes will lead to more detailed results in the evaluation of biological treatments.
In conclusion, our findings demonstrated that ASDAS remission and low disease activity were noted in 366 (37.9%) patients. In this nationwide registry, male sex and presence of HLA-B27 consistently predicted remission of axSpA as measured by ASDAS-CRP.
References
Deodhar A, Gensler LS, Kay J, Maksymowych WP, Haroon N, Landewé R, Rudwaleit M, Hall S, Bauer L, Hoepken B, de Peyrecave N, Kilgallen B, van der Heijde D (2019) A fifty-two-week, randomized, placebo-controlled trial of certolizumab pegol in nonradiographic axial spondyloarthritis. Arthritis Rheumatol. 71:1101-1111.: https://doi.org/10.1002/art.40866
Rodrigues-Manica S, Silva J, Cruz-Machado R, Coelho C, Duarte J, Vieira-Sousa E, Tavares-Costa J, Pimentel-Santos FM (2021) Biologic disease-modifying anti-rheumatic drugs and patient-reported outcomes in axial SpA: a systematic review and a call for action. Clin Rheumatol 40:33–41. https://doi.org/10.1007/s10067-020-05209-x
Sieper J, Landewé R, Magrey M, Anderson JK, Zhong S, Wang X, Lertratanakul A (2019) Predictors of remission in patients with non-radiographic axial spondyloarthritis receiving open-label adalimumab in the ABILITY-3 study. RMD Open. 7;5:e000917.: https://doi.org/10.1136/rmdopen-2019-000917
Shimabuco AY, Gonçalves CR, Moraes JCB, Waisberg MG, Ribeiro ACM, Sampaio-Barros PD, Goldenstein-Schainberg C, Bonfa E, Saad CGS (2018) Factors associated with ASDAS remission in a long-term study of ankylosing spondylitis patients under tumor necrosis factor inhibitors. Adv Rheumatol. 4;58:40.: https://doi.org/10.1186/s42358-018-0040-x
Chen X, Zhang T, Wang W, Xue J (2018) Analysis of relapse rates and risk factors of tapering or stopping pharmacologic therapies in axial spondyloarthritis patients with sustained remission. Clin Rheumatol 37:1625–1632. https://doi.org/10.1007/s10067-018-4084-4
Pradeep DJ, Keat AC, Gaffney K, Brooksby A, Leeder J, Harris C (2008) Switching anti-TNF therapy in ankylosing spondylitis. Rheumatology (Oxford) 47:1726–1727. https://doi.org/10.1093/rheumatology/ken334
Haberhauer G, Strehblow C, Fasching P (2010) Observational study of switching anti-TNF agents in ankylosing spondylitis and psoriatic arthritis versus rheumatoid arthritis. Wien Med Wochenschr 160:220–4. https://doi.org/10.1007/s10354-010-0795-0
Monti S, Todoerti M, Codullo V, Favalli EG, Biggioggero M, Becciolini A, Montecucco C, Caporali R (2018) Prevalence of Ankylosing Spondylitis Disease Activity Score (ASDAS) inactive disease in a cohort of patients treated with TNF-alpha inhibitors. Mod Rheumatol 28:542–549. https://doi.org/10.1080/14397595.2017.1367076
Landewé R, van Tubergen A (2015) Clinical tools to assess and monitor spondyloarthritis. Curr Rheumatol Rep. 17:47.:https://doi.org/10.1007/s11926-015-0522-3
Machado PM, Deodhar A (2019). Treat-to-target in axial spondyloarthritis: gold standard or fools’ gold? Curr Opin Rheumatol. 31:344–348.:https://doi.org/10.1097/BOR.0000000000000625
Deodhar A, Reveille JD, van den Bosch F, Braun J, Burgos-Vargas R, Caplan L, Clegg DO, Colbert RA, Gensler LS, van der Heijde D, van der Horst-Bruinsma IE, Inman RD, Maksymowych WP, Mease PJ, Raychaudhuri S, Reimold A, Rudwaleit M, Sieper J, Weisman MH, Landewé RB (2014) The concept of axial spondyloarthritis: joint statement of the spondyloarthritis research and treatment network and the Assessment of SpondyloArthritis international Society in response to the US Food and Drug Administration’s comments and concerns. Arthritis Rheumatol. 66:2649–2656.:https://doi.org/10.1002/art.38776
Poddubnyy D, Gensler LS (2014) Spontaneous, drug-induced, and drug-free remission in peripheral and axial spondyloarthritis. Best Pract Res Clin Rheumatol 28:807–818. https://doi.org/10.1016/j.berh.2014.10.005
Hernández-Breijo B, Plasencia-Rodríguez C, Navarro-Compán V, Martínez-Feito A, Jochems A, Kneepkens EL, Wolbink GJ, Rispens T, Diego C, Pascual-Salcedo D, Balsa A (2019) Association between concomitant csDMARDs and clinical response to TNF inhibitors in overweight patients with axial spondyloarthritis. Arthritis Res Ther. 211:66.:https://doi.org/10.1186/s13075-019-1849-3
Carvalho PD, Ruyssen-Witrand A, Fonseca J, Marreiros A, Machado PM (2020) Determining factors related to impaired spinal and hip mobility in patients with axial spondyloarthritis: longitudinal results from the DESIR cohort. RMD Open. 6:e001356.:https://doi.org/10.1136/rmdopen-2020-001356
Akgul O, Bodur H, Ataman S, Yurdakul FG, Capkin E, Gurer G, Sezer I, Duruoz MT, Melikoglu MA, Cay HF, Rezvani A, Yagci I, Gogus F, Kamanli A, Cevik R (2020) Clinical performance of ASAS Health Index in patients with ankylosing spondylitis and non-radiographic axial spondyloarthritis: real-world evidence from Multicenter Nationwide Registry. Rheumatol Int. 40:1793–1801.:https://doi.org/10.1007/s00296-020-04680-8
Landewé RB, van der Heijde D, Dougados M, Baraliakos X, Van den Bosch FE, Gaffney K, Bauer L, Hoepken B, Davies OR, de Peyrecave N, Thomas K, Gensler LS (2020) Maintenance of clinical remission in early axial spondyloarthritis following certolizumab pegol dose reduction. Ann Rheum Dis. 79:920–928.:https://doi.org/10.1136/annrheumdis-2019-216839
Landewé R, van der Heijde D, Dougados M, Baraliakos X, Van den Bosch F, Gaffney K, Bauer L, Hoepken B, de Peyrecave N, Thomas K, Gensler LS (2020) Induction of sustained clinical remission in early axial spondyloarthritis following certolizumabpegol treatment: 48-week outcomes from C-OPTIMISE. Rheumatol Ther. 7:581–599.: https://doi.org/10.1007/s40744-020-00214-7.
Lubrano E, Perrotta FM, Marchesoni A, D’Angelo S, Ramonda R, Addimanda O et al (2015) Remission in nonradiographic axial spondyloarthritis treated with anti-tumor necrosis factor-a drugs: an Italian multicenter study. J Rheumatol 42:258–263
van der Heijde D, Deodhar A, Braun J, Mack M, Hsu B, Gathany TA et al (2014) The effect of golimumab therapy on disease activity and health-related quality of life in patients with ankylosing spondylitis: 2-year results of the GO-RAISE trial. J Rheumatol 41:1095–1103
Zochling J, Braun J (2006) Remission in ankylosing spondylitis. Clin Exp Rheumatol. 24:S-88–92.
Ziade N, Abi Karam G, Merheb G, Mallak I, Irani L, Alam E, Messaykeh J, Menassa J, Mroue’ K, Uthman I, Masri AF, Ghorra P, Witte T, Baraliakos X (2019) HLA-B27 prevalence in axial spondyloarthritis patients and in blood donors in a Lebanese population: Results from a nationwide study. Int J Rheum Dis. 22:708–714.:https://doi.org/10.1111/1756-185X.13487.
Akassou A, Yacoubi H, Jamil A, Dakka N, Amzazi S, Sadki K, Niamane R, Elhassani S, Bakri Y (2015) Prevalence of HLA-B27 in Moroccan healthy subjects and patients with ankylosing spondylitis and mapping construction of several factors influencing AS diagnosis by using multiple correspondence analysis. Rheumatol Int 35:1889–94. https://doi.org/10.1007/s00296-015-3342-x
Arévalo M, López-Medina C, Moreno Martinez-Losa M, Moltó A, Font P, Collantes-Estevez E, Gratacós J (2020) Role of HLA-B27 in the comorbidities observed in axial spondyloarthritis: data from COMOSPA. Joint Bone Spine 87:445–448. https://doi.org/10.1016/j.jbspin.2020.03.012
Kısaarslan AP, Sözeri B, Gündüz Z, Zararsız G, Poyrazoğlu H, Düşünsel R (2019) Evaluation of factors affecting the duration of disease-modifying anti-rheumatic drugs application in patients with enthesitis-related arthritis. Eur J Rheumatol 6:130–35. https://doi.org/10.5152/eurjrheum.2019.18180
Soubrier M, Pereira B, Fan A, Frayssac T, Couderc M, Malochet-Guinamand S, Mathieu S, Tatar Z, Tournadre A, Dubost JJ (2018) Retention rates of adalimumab, etanercept, and infliximab as first- or second-line biotherapies for spondyloarthritis patients in daily practice in Auvergne (France). Int J Rheum Dis 21:1986–1992. https://doi.org/10.1111/1756-185X.13375
Sebastian A, Wojtala P, Lubiński Ł, Mimier M, Chlebicki A, Wiland P (2017) Disease activity in axial spondyloarthritis after discontinuation of TNF inhibitors therapy. Reumatologia 55:157–162. https://doi.org/10.5114/reum.2017.69775
Landewé R, Sieper J, Mease P, Inman RD, Lambert RG, Deodhar A, Marzo-Ortega H, Magrey M, Kiltz U, Wang X, Li M, Zhong S, Mostafa NM, Lertratanakul A, Pangan AL, Anderson JK (2018) Efficacy and safety of continuing versus withdrawing adalimumab therapy in maintaining remission in patients with non-radiographic axial spondyloarthritis (ABILITY-3): a multicentre, randomised, double-blind study. Lancet. 392:134–144.: https://doi.org/10.1016/S0140-6736(18)31362-X.
Deodhar A, Sandoval D, Holdsworth E, Booth N, Hunter T (2020) Use and switching of biologic therapy in patients with non-radiographic axial spondyloarthritis: a patient and provider survey in the United States. Rheumatol Ther 7:415–423. https://doi.org/10.1007/s40744-020-00208-5
Glintborg B, Østergaard M, Krogh NS, Tarp U, Manilo N, Loft AG, Hansen A, Schlemmer A, Fana V, Lindegaard HM, Nordin H, Rasmussen C, Ejstrup L, Jensen DV, Petersen PM, Hetland ML (2013) Clinical response, drug survival and predictors thereof in 432 ankylosing spondylitis patients after switching tumour necrosis factor α inhibitor therapy: results from the Danish nationwide DANBIO registry. Ann Rheum Dis 72:1149–1155. https://doi.org/10.1136/annrheumdis-2012-201933
Hartung W, Nigg A, Strunk J, Wolff B (2018) Clinical assessment and ultrasonography in the follow-up of enthesitis in patients with spondyloarthritis: a multicenter ultrasound study in daily clinical practice Open Access. Rheumatol 10(161):169. https://doi.org/10.2147/OARRR.S179472
Palominos PE, de Campos APB, Ribeiro SLE, Xavier RM, Xavier JW, de Oliveira FB, Guerra B, Saldanha C, Mancuso ACB, Kohem CL, Gasparin AA, Sampaio-Barros PD (2019) Correlation of enthesitis indices with disease activity and function in axial and peripheral spondyloarthritis: a cross-sectional study comparing MASES, SPARCC and LEI. Adv Rheumatol. 59:23.:https://doi.org/10.1186/s42358-019-0066-8.
Berg KH, Rohde G, Pripp A, Prøven A, Pirelli Benestad EE, Østensen M, Haugeberg G (2021) Increased proportion of comorbidities but no deterioration of sexual QOL during a 5-year follow-up in patients with axSpA in the biologic treatment era. Rheumatology (Oxford). 7: keaa887.:https://doi.org/10.1093/rheumatology/keaa887
Deodhar A, Yu D (2017) Switching tumor necrosis factor inhibitors in the treatment of axial spondyloarthritis. Semin Arthritis Rheum 47:343–350. https://doi.org/10.1016/j.semarthrit.2017.04.005
Lee S, Park YJ, Lee JY (2019) The effect of tumor necrosis factor-alpha inhibitors on uveitis in patients with ankylosing spondylitis. J Korean Med Sci. 4:e278.:https://doi.org/10.3346/jkms.2019.34.e278.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bodur, H., Yurdakul, F.G., Ataman, S. et al. Where we are in treat to target era? Predictive factors for remission and drug switching in patients with axial spondyloarthritis: a real-life evidence from BioStaR nationwide registry. Clin Rheumatol 41, 2053–2063 (2022). https://doi.org/10.1007/s10067-022-06145-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-022-06145-8