Abstract
Objective
To identify clinical characteristics and risk factors related to the progression of interstitial lung disease (ILD) in patients with primary Sjögren’s syndrome (pSS).
Methods
In this single-centered, retrospective study, a total of 83 identified pSS-ILD patients with relatively complete clinical data were finally enrolled. Clinical symptoms, laboratory data, high-resolution computed tomography (HRCT), and pulmonary function test (PFT) results were collected. A logistic regression analysis was performed to determine the independent risk factors for ILD progression, and a nomogram was plotted to construct a predictive model.
Results
The prevalence of pSS-ILD in our study was 18.89%. Among the 83 enrolled patients, 32 (38.6%) underwent ILD progression. The characteristic features associated with the progression of ILD included male sex, non-sicca onset, reticular pattern on HRCT, higher levels of baseline lactic dehydrogenase (LDH), and low baseline forced vital capacity (FVC). The results of multivariate logistic regression indicated that LDH (OR 1.008, p = 0.030) was an independent risk factor for ILD progression, while sicca onset (OR 0.254, p = 0.044) and FVC (OR 0.952, p = 0.003) were protective factors for ILD progression. A simple predictive model for ILD progression in pSS was developed and validated.
Conclusion
pSS patients with non-sicca onset, high baseline LDH level, and low baseline FVC were at higher risk of ILD progression.
Key Points • Male sex and reticular pattern in HRCT are more common in pSS patients with progressive ILD compared to those with stable ILD. • Non-sicca onset, high baseline LDH level, and low baseline FVC are independent risk factors of pSS-ILD progression. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary Sjögren’s syndrome (pSS) is the second most common autoimmune disease with a prevalence of 0.3–1‰. The pathological hallmarks of the disease are lymphocytic infiltration and structural destruction of the lacrimal and salivary glands, leading to the major clinical manifestations of dye eyes and dry mouth [1]. Extra-glandular involvements occur in a large majority of patients, including lung, kidney, liver, and nervous system [1, 2]. Interstitial lung disease (ILD) is a common form of lung involvement in pSS patients and the prevalence is between 3 and 60% depending on the methodology used to identify ILD [2, 3]. While the disease course of ILD may be benign and stable in some pSS patients, its progression and deterioration do happen in other cases, leading to impaired quality of life and higher rate of morbidity and mortality [4, 5]. Therefore, early screening of patients with high risk of ILD progression is of great significance for prompt intervention in order to improve prognosis.
Great endeavors have been made to unveil the factors associated with ILD development in pSS patients. To date, the following factors have been shown to be correlated with ILD occurrence: older age, male, high titer of anti-nuclear antibodies (ANA) or rheumatoid factor (RF), the presence of anti-Ro52 autoantibody, low circulating C3, increased C-reactive protein (CRP) level, etc. [2, 6,7,8,9]. However, there is a scarcity of data on ILD progression in pSS patients and the discrepancies do exist [10,11,12]. Thus, we conducted this single-centered, retrospective study, aiming to identify characteristic features and risk factors for ILD progression in pSS patients.
Materials and methods
Patients
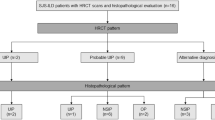
This retrospective study started with identification of pSS-ILD patients by searching the electronic medical records. In the first electronic search, patients diagnosed as pSS at the First Affiliated Hospital of Zhengzhou University from January of 2015 to December of 2019 were screened. All patients met the 2002 revised classification criteria proposed by American-European Consensus Group (AECG) for pSS [13]. A second search was then conducted to identify those who exhibited ILD in pSS patients (pSS-ILD). pSS patients who met any 3 of the 5 following items were diagnosed as pSS-ILD: (1) cough or shortness of breath in rest and/or after activity; (2) the presence of Velcro crackles in auscultation; (3) imaging features supporting ILD in HRCT (e.g., ground-glass opacity, consolidation, reticulation, nodules, traction bronchiectasis, honeycombing, cysts); (4) abnormal PFT results: FVC or diffusing capacity for carbon monoxide (DLCO) < 80% predicted value; (5) lung biopsy confirmed pathological patterns of ILD. Patients with any of the following conditions were excluded: younger than 18 years, concomitant with tumors, other pulmonary diseases, and/or other autoimmune diseases. Altogether 1382 pSS patients were screened in this study, and 261 had pSS-ILD. Among these pSS-ILD patients, 68 patients were missed during follow-ups (could not be contacted or did not finish subsequent visits), 41 patients were excluded due to above mentioned conditions, and 69 patients were further excluded for the lack of vital baseline data (mainly for the lack of baseline HRCT images, PFT results, and/or too many missing data on laboratory tests). Finally, 83 patients with relatively complete clinical data and at least one follow-up were enrolled and divided into two groups depending on their ILD status (Fig. 1). In order to exclude the possibility of major selection bias, the study cohort of the 83 patients was compared to all available baseline data of the 68 excluded patients for the reason of missed follow-up and the results are shown in Table S1.
A flow chart of this study. A total of 1382 pSS patients were screened and 261 of them were identified as pSS-ILD. Among the 261 patients, 68 patients were missed, 41 patients were excluded because of different reasons, and 69 patients were further excluded for the lack of vital baseline data. Finally, 83 patients with relatively complete clinical data and at least one follow-up were enrolled and divided into two groups depending on their clinical course of ILD
Data collection
The following demographic and clinical data were collected: age, gender, disease duration, hospital stays, and treatment strategies. Clinical features associated with pSS and systemic involvement were fully recorded as well. In addition, the laboratory data were collected, including complete blood count, biochemical profile, antinuclear antibody (ANA) spectrum, Krebs von den Lungen-6 (KL-6), complement 3 (C3), complement 4 (C4), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and rheumatoid factor (RF).
For HRCT abnormalities, ground-glass opacities, reticular pattern, and honeycombing were analyzed for their high prevalence and/or potential clinical significance based on previous studies [14, 15] and clinical experience. HRCT patterns of ILD were determined by two experienced radiologists and one rheumatologist according to the 2011 American Thoracic Society (ATS) and the European Respiratory Society (ERS) modified classification [16, 17]. For the PFTs, the results of FVC and DLCO were collected. In this study, progressive ILD was defined when any of the following results were presented during follow-up period: (1) a relative decline in FVC from baseline of ≥ 10% or in DLCO of ≥ 15%; (2) a relative decline in FVC of 5–9% plus increased extent of fibrosis on HRCT; (3) a relative decline in FVC of 5–9% plus worsening of respiratory symptoms; (4) worsened respiratory symptoms plus increased extent of fibrosis on HRCT. Accordingly, patients without abovementioned results were designated as stable ILD.
Statistics
Continuous variables were presented as mean ± standard deviation (SD) for normally distributed data and the median (range) for non-normally distributed data. Categorical variables were presented as the percentages. Intergroup comparisons were conducted using Student’s t test or Mann–Whitney U test for continuous variables, while categorical data were compared using chi-square test. Univariate and multivariate logistic regression analyses were performed to identify the independent risk factors for ILD progression in pSS patients. Multi-collinearity diagnostic tests were carried out before determining the final model. A nomogram was plotted to construct the predictive model for ILD progression in pSS patients based on the results of multivariate analysis. A calibration curve was performed to evaluate the accuracy of the predictive model. Receiver operating characteristic (ROC) curve was used to compare the obtained nomogram with each single factor based on area under the curve (AUC). p < 0.05 was considered to be statistically significant. SPSS 21.0 (SPSS Inc., Chicago, IL, USA) and R software (version 3.6.1) were used for the analysis.
Results
Demographic features and laboratory metrics
The prevalence of pSS-ILD in our study was 18.89%. Among the 83 finally enrolled patients, 72 (86.7%) were females, 8 (9.6%) had a history of smoking, and 32 (38.6%) had progressive ILD. The mean age at baseline was 54.13 ± 9.35 years old. All patients were followed up for 2–67 months (median follow-up period: 23 months). As for the ANA spectrum, the positivity for different autoantibodies was as follows: 72 (86.7%) for ANA, 2 (2.4%) for centromere, 15 (18.1%) for SSB, 65 (78.3%) for Ro52, 34 (41.0%) for Ro60, and 4 (4.8%) for nRNP/Sm. Compared to ILD stable group, the LDH levels and proportion of male patients were significantly higher in patients with progressive ILD (Table 1).
PFT results and HRCT features
For baseline HRCT abnormalities, the percentages of different patterns were as follows: 56 patients with ground-glass opacities (67.5%), 47 with reticular pattern (56.6%), and 9 with honeycombing (10.8%). Nonspecific interstitial pneumonia (NSIP) was identified in 42 (50.6%) patients, usual interstitial pneumonia (UIP) in 22 (26.5%) patients, and lymphocytic interstitial pneumonia (LIP) in 3 (3.6%) patients. The proportion of patients with reticular pattern was significantly higher in progressive ILD than that in stable ILD. Besides, patients with progressive ILD showed significantly lower baseline FVC than those with stable ILD (Table 1).
Clinical features and treatments
The initial symptoms were highly heterogeneous in these patients and the percentages were as follows: 23 with xerostomia (27.7%), 17 with xerophthalmia (20.5%), 7 with decayed tooth (8.4%), 5 with parotitis (6.0%), 6 with arthralgia (7.2%), 46 with cough or shortness of breathing (55.4%), 5 with Raynaud phenomenon (6.0%), 1 with numbness of hands and feet (1.2%), and 1 with lower limb edema (1.2%). The proportion of patients with abovementioned initial symptoms in each group is shown in Fig. 2. Sicca onset was defined as the initial manifestation being xerostomia and/or xerophthalmia in their first visit. The proportion of the patients with sicca onset was significantly lower in ILD-progression group than in ILD stable group (Table 1).
Systemic involvements were found in 33 patients (39.8%), including 16 with arthritis (19.3%), 5 with complicated involvement of peripheral nervous system (6.0%), and 9 with digestive system involvement (10.8%). Among patients with digestive system involvements, 1 with primary biliary cholangitis and 8 with chronic gastritis. No significant differences were found between the two groups on these systemic involvements (data not shown).
The treatments of these 83 pSS-ILD patients are summarized in Table 2. Almost all patients (95.18%) were treated with different dosage of glucocorticoid (GC). None of these patients received pulse GC therapy. Only 6 (7.23%) patients were treated with GC alone, while others in combination of immunosuppressant or other agents (e.g., hydroxychloroquine, total glucosides of paeonia, acetylcysteine). Antifibrotic agent pirfenidone was used in 7 (8.43%) patients and 1 patient received intravenous immunoglobulin (IVIG) therapy due to acute exacerbation.
Risk factors for ILD progression and predictive model
The results of univariate and multivariate logistic regression analyses of ILD progression are shown in Table 3. In univariate logistic regression analysis, sex, sicca onset, LDH, FVC, and reticular pattern on HRCT were statistically significant variables for ILD progression. Before conducting the multivariate logistic regression, multi-collinearity diagnostic tests were carried out by variance inflation factor (VIF) using SPSS and no multi-collinearity was found (VIF < 10). Finally, the results from multivariate logistic regression analysis showed that sicca onset, LDH, and FVC were independently associated with ILD progression in pSS patients.
A nomogram was plotted to construct the predictive model (Fig. 3a). A calibration curve was constructed to evaluate the accuracy of the model (Fig. 3b). The sufficient agreement between the predicted ILD-progression rate by this model and the actual ILD-progression rate in pSS patients indicated a favorable accuracy of the model. In addition, ROC curve was used to compare this model with each single risk factor (sicca onset, LDH, and FVC) obtained from multivariate logistic regression (Fig. 3c). The AUC of our nomogram model was 0.798, and 0.612 for sicca onset, 0.668 for LDH, and 0.726 for FVC.
A simple predictive model for ILD progression in pSS patients. a The nomogram to predict ILD progression in pSS patients. b A calibration curve to evaluate the accuracy of the model. c ROC curve to compare this model with each single factor. The AUC for sicca onset, LDH, FVC, and model were 0.612, 0.668, 0.726, and 0.798, respectively. Sicca onset: patients presenting sicca symptoms (xerostomia and/or xerophthalmia) in the first visit are defined as sicca onset; LDH, lactic dehydrogenase; FVC, forced vital capacity; ROC, receiver operating characteristic
Discussion
ILD is a common form of systemic involvements in pSS patients. Although the clinical course of pSS-ILD is usually mild and stable compared to other connective tissue disease-associated ILD (CTD-ILD) and idiopathic pulmonary fibrosis (IPF), its progression and deterioration do occur in some patients, resulting in increased morbidity and mortality [8, 18]. A previous report demonstrates that the 5-year survival rate of pSS-ILD is about 89.8% and the 10-year survival rate about 79.0% [11]. Therefore, it is imperative to identify the clinical characteristics and risk factors for ILD progression in pSS patients. To the best of our knowledge, the present study is the largest retrospective study focused on risk factors for ILD progression in pSS patients. Several clinical characteristics associated with ILD progression have been identified, including male sex, non-sicca onset, reticular pattern in HRCT, higher levels of baseline LDH, and low baseline FVC. The results of multivariate logistic regression indicate that LDH is an independent risk factor for ILD progression, while sicca onset and FVC are protective factors for ILD progression. A simple predictive model for ILD progression in pSS patients has been developed and validated. Our results may help clinicians to stay vigilant to these risk factors responsible for ILD progression for early and effective intervention, which may then improve treatment outcomes and prognosis of pSS-ILD patients.
Previous studies have demonstrated that the prevalence of pSS-ILD is about 20% [8, 19]. Consistently, our study shows that 261 out of 1382 pSS patients developed ILD and the prevalence was 18.89%. To date, few studies focus on the progression of ILD in pSS patients. Zhang et al. reported that about 20.4% pSS patients developed progressive phenotype of ILD [12]. Roca et al. showed that 36.8% of pSS-ILD patients experienced ILD deterioration as evidenced by impaired pulmonary functions during the 24 months of follow-up [10]. While our study showed that 38.6% of pSS-ILD patients developed progressive ILD, cautions should be taken when interpreting the results because of the possibility of the selection bias and retrospective nature of this study. Previous studies have demonstrated that male sex is a risk factor for increased mortality due to progressive systemic sclerosis-associated ILD (SSc-ILD) and correlated with rheumatoid arthritis (RA)-related ILD (RA-ILD) [20, 21]. Accordantly, we have revealed a male predominance in the progressive ILD group compared to ILD stable group. These observations suggest that regardless of different types of CTDs, male patients with CTD-ILD are more likely to have poor prognosis, warranting more frequent evaluation of pulmonary conditions for prompt intervention.
HRCT has demonstrated that pSS-ILD have different presentations [2, 22]. We focused on ground-glass opacities, reticular pattern, and honeycombing for their high prevalence and potential clinical significance, and found significant differences on reticular pattern between the two groups. Enomoto et al. also reported that reticular abnormality on HRCT was a prognosis factor in pSS-ILD [15]. Our results are consistent with widely accepted notion that NSIP is the most common in pSS patients when examined with HRCT. Zhang et al. reported that UIP was a potential predictor for pSS-ILD progression [12], whereas Enomoto et al. did not find significant difference on survival rate between NSIP and UIP groups [15]. In our study, no significant difference on UIP pattern was found between progressive ILD and stable ILD group patients.
To date, there is no standard definition of progressive fibrosing ILD and several criteria have been used to define ILD-progression, most of which are based on PFT results. A decrease of ≥ 10% in FVC and/or ≥ 15% in DLCO are the most commonly used criteria in clinical trials [10, 23, 24]. Of note, PFT alone may not be sufficient to evaluate the ILD condition as PFT results are not always correlated with radiological abnormalities and clinical manifestations [2, 25]. Recently, a large double-blind, placebo-controlled trial, the INBUILD study, took use of the compound criteria including lung function, HRCT, and clinical symptoms to define ILD progression [26]. Somewhat similarly, the definition of ILD progression in our present study was determined by the combination of the PFT results, HRCT findings, and clinical symptoms. However, a standardized and updated criterion is needed to better evaluate the course of ILD.
FVC is a significant parameter in evaluating the development and progression of ILD. It has been identified as a risk factor in various types of ILD such as progressive SSc-ILD, anti-melanoma differentiation-associated gene 5-positive dermatomyositis (MDA5+-DM)-associated ILD, and RA-ILD [20, 21, 27]. Kamiya Y et al. studied the prognostic factors for pSS-ILD in a relatively large number of patients and found that low %FVC was significantly correlated with long-term mortality [11]. Similarly, our present study indicated that a low baseline FVC was an independent risk factor for ILD progression in pSS patients. It seems that FVC is a defining factor to predict the prognosis of pSS-ILD, though more large-scale studies may be needed to better validate this concept. Apart from baseline FVC, particular attention should be paid to the changes of FVC in certain time periods in clinical practice. While a 5% change in FVC is previously thought to have no clinical significance as it is within normal test variability, du Bois et al. demonstrated that a decline in %FVC as small as 5% at 6 months was correlated with a more than twofold increase in the mortality over the following 12 months in IPF patients [28]. More studies are needed to improve our understanding of the significance of the FVC per se and its changes during disease courses. No significant difference on DLCO was found between the two groups in our study, indicating that the clinical significance of FVC and DLCO is not exactly the same. It seems that DLCO is highly sensitive to the development of ILD, whereas FVC more useful in assessing disease extent [29].
Several lines of evidence suggest a correlation between LDH and ILD. One study shows that high serum level of LDH is correlated with the progression of lung injury in IPF [30]. Another report demonstrates that elevated LDH levels are closely correlated to the development of RA-ILD [31]. A meta-analysis shows that LDH is a prognostic factor of acute exacerbation (AE) of IPF [32]. Dong et al. reported that elevated LDH levels were associated with ILD development in pSS patients [14]. Our study confirms the LDH is an independent risk factor for ILD progression in pSS patients.
OF note, we demonstrate that sicca onset is a protective factor for ILD progression in pSS patients. It is plausible to postulate that patients with non-sicca onset are at higher risk for ILD progression through a yet-unknown mechanism. Andreina et al. reported that nearly half of pSS-ILD patients were non-sicca onset, leading to delayed diagnosis of pSS in this group of patients [33]. GAO et al. conducted a large-scale case–control study and further explored the characteristics of non-sicca onset pSS patients. They found that 51% of pSS-ILD patients were non-sicca onset. The positivity for SSA autoantibody, elevated RF titer, and hyperglobulinemia were less predominant in non-sicca patients, while pulmonary complications were more progressive and severe compared with sicca-onset pSS patients [34]. More studies are needed to elucidate the pathognomics of ILD progression in pSS patients with different onsets.
The 6-min walk test (6MWT)/6-min walk distance (6MWD) is a simple, non-invasive, and highly reproducible test. It is commonly used to assess the functional exercise capacity of patients with heart and/or lung diseases, including several types of ILDs. du Bois et al. conducted a large-scale study with well-defined population of IPF patients to validate the relation between 6MWT and prognosis of IPF, and the results showed that both 6MWD and change in 6MWD were independent predictors of mortality in patients with IPF [35]. Previous studies have demonstrated controversial results of 6MWD in SSc patients [36, 37]. A recent report showed that a lower 6MWD in SSc patients was correlated with PFT test results, and it can be used as an independent predictor for the SSc-related mortality [38]. To date, the studies to explore the usefulness of 6MWD in pSS-ILD patients are rare. It was not included in our present study due to the unanticipated missing data, while prospective studies are needed to test its feasibility and reliability.
There are some limitations in our study. Firstly, it is a single-centered, retrospective study and the number of patients enrolled is relatively small. Secondly, we did not perform a further stratified analysis based on different treatment strategies. Thirdly, our predictive model was not validated externally in another validation cohort due to the limited number of cases.
Conclusions
ILD is not rare in pSS patients and the risk of ILD progression should not be underestimated. Our study showed that 38.6% of pSS-ILD patients developed progressive ILD during follow-up periods, and more extensive studies are needed to validate our results. In terms of clinical features, pSS patients with progressive ILD were characterized by male predominance and non-sicca complaints at initial referral. Low baseline FVC, high baseline LDH, and more reticular pattern on chest HRCT were also identified when compared to those with stable ILD. No significant difference was found on the ANA spectrum between these two groups. We further explored the relevant features of ILD progression in pSS patients and identified that baseline LDH was an independent risk factor for ILD progression, while sicca onset and preserved baseline FVC were shown protective. pSS-ILD patients with abovementioned characteristics should be monitored more frequently, assessed more carefully, and, if necessary, be treated more aggressively. Based on these findings, a simple predictive nomogram model for ILD progression in pSS patients has been developed and validated for better evaluation of pSS-ILD patients in daily clinical practice.
References
Mariette X, Criswell LA (2018) Primary Sjogren’s syndrome. N Engl J Med 378:931–939. https://doi.org/10.1056/NEJMcp1702514
Flament T, Bigot A, Chaigne B, Henique H, Diot E, Marchand-Adam S (2016) Pulmonary manifestations of Sjogren’s syndrome. Eur Respir Rev 25:110–123. https://doi.org/10.1183/16000617.0011-2016
Peredo RA, Beegle S (2021) Sjogren’s syndrome and pulmonary disease. Adv Exp Med Biol 1303:193–207. https://doi.org/10.1007/978-3-030-63046-1_12
Reina D, Roig Vilaseca D, Torrente-Segarra V et al (2016) Sjogren’s syndrome-associated interstitial lung disease: a multicenter study. Reumatol Clin 12:201–205. https://doi.org/10.1016/j.reuma.2015.09.003
Zhao R, Wang Y, Zhou W et al (2020) Associated factors with interstitial lung disease and health-related quality of life in Chinese patients with primary Sjogren’s syndrome. Clin Rheumatol 39:483–489. https://doi.org/10.1007/s10067-019-04753-5
Gao H, Zhang XW, He J et al (2018) Prevalence, risk factors, and prognosis of interstitial lung disease in a large cohort of Chinese primary Sjogren syndrome patients: a case-control study. Medicine (Baltimore) 97:e11003. https://doi.org/10.1097/MD.0000000000011003
Buvry C, Cassagnes L, Tekath M et al (2020) Anti-Ro52 antibodies are a risk factor for interstitial lung disease in primary Sjogren syndrome. Respir Med 163:105895. https://doi.org/10.1016/j.rmed.2020.105895
Luppi F, Sebastiani M, Silva M et al (2020) Interstitial lung disease in Sjogren’s syndrome: a clinical review. Clin Exp Rheumatol 38(Suppl 126):291–300
Li X, Xu B, Ma Y et al (2015) Clinical and laboratory profiles of primary Sjogren’s syndrome in a Chinese population: a retrospective analysis of 315 patients. Int J Rheum Dis 18:439–446. https://doi.org/10.1111/1756-185X.12583
Roca F, Dominique S, Schmidt J et al (2017) Interstitial lung disease in primary Sjogren’s syndrome. Autoimmun Rev 16:48–54. https://doi.org/10.1016/j.autrev.2016.09.017
Kamiya Y, Fujisawa T, Kono M et al (2019) Prognostic factors for primary Sjogren’s syndrome-associated interstitial lung diseases. Respir Med 159:105811. https://doi.org/10.1016/j.rmed.2019.105811
Zhang T, Yuan F, Xu L, Sun W, Liu L, Xue J (2020) Characteristics of patients with primary Sjogren’s syndrome associated interstitial lung disease and relevant features of disease progression. Clin Rheumatol 39:1561–1568. https://doi.org/10.1007/s10067-019-04906-6
Vitali C, Bombardieri S, Jonsson R et al (2002) Classification criteria for Sjogren’s syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis 61:554–558. https://doi.org/10.1136/ard.61.6.554
Dong X, Zhou J, Guo X et al (2018) A retrospective analysis of distinguishing features of chest HRCT and clinical manifestation in primary Sjogren’s syndrome-related interstitial lung disease in a Chinese population. Clin Rheumatol 37:2981–2988. https://doi.org/10.1007/s10067-018-4289-6
Enomoto Y, Takemura T, Hagiwara E et al (2013) Prognostic factors in interstitial lung disease associated with primary Sjogren’s syndrome: a retrospective analysis of 33 pathologically-proven cases. PLoS ONE 8:e73774. https://doi.org/10.1371/journal.pone.0073774
Travis WD, Hunninghake G, King TE Jr et al (2008) Idiopathic nonspecific interstitial pneumonia: report of an American Thoracic Society project. Am J Respir Crit Care Med 177:1338–1347. https://doi.org/10.1164/rccm.200611-1685OC
Raghu G, Collard HR, Egan JJ et al (2011) An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 183:788–824. https://doi.org/10.1164/rccm.2009-040GL
Gupta S, Ferrada MA, Hasni SA (2019) Pulmonary manifestations of primary Sjogren’s syndrome: underlying immunological mechanisms, clinical presentation, and management. Front Immunol 10:1327. https://doi.org/10.3389/fimmu.2019.01327
Sambataro G, Ferro F, Orlandi M et al (2020) Clinical, morphological features and prognostic factors associated with interstitial lung disease in primary Sjgren’s syndrome: a systematic review from the Italian Society of Rheumatology. Autoimmun Rev 19:102447. https://doi.org/10.1016/j.autrev.2019.102447
Spagnolo P, Lee JS, Sverzellati N, Rossi G, Cottin V (2018) The lung in rheumatoid arthritis: focus on interstitial lung disease. Arthritis Rheumatol 70:1544–1554. https://doi.org/10.1002/art.40574
Khanna D, Tashkin DP, Denton CP, Renzoni EA, Desai SR, Varga J (2020) Etiology, risk factors, and biomarkers in systemic sclerosis with interstitial lung disease. Am J Respir Crit Care Med 201:650–660. https://doi.org/10.1164/rccm.201903-0563CI
Chung A, Wilgus ML, Fishbein G, Lynch JP 3rd (2019) Pulmonary and bronchiolar involvement in Sjogren’s syndrome. Semin Respir Crit Care Med 40:235–254. https://doi.org/10.1055/s-0039-1688448
Fu Q, Wang L, Li L, Li Y, Liu R, Zheng Y (2019) Risk factors for progression and prognosis of rheumatoid arthritis-associated interstitial lung disease: single center study with a large sample of Chinese population. Clin Rheumatol 38:1109–1116. https://doi.org/10.1007/s10067-018-4382-x
Khanna D, Mittoo S, Aggarwal R et al (2015) Connective tissue disease-associated interstitial lung diseases (CTD-ILD) - report from OMERACT CTD-ILD Working Group. J Rheumatol 42:2168–2171. https://doi.org/10.3899/jrheum.141182
Uffmann M, Kiener HP, Bankier AA, Baldt MM, Zontsich T, Herold CJ (2001) Lung manifestation in asymptomatic patients with primary Sjogren syndrome: assessment with high resolution CT and pulmonary function tests. J Thorac Imaging 16:282–289. https://doi.org/10.1097/00005382-200110000-00009
Flaherty KR, Wells AU, Cottin V et al (2019) Nintedanib in progressive fibrosing interstitial lung diseases. N Engl J Med 381:1718–1727. https://doi.org/10.1056/NEJMoa1908681
Wu W, Guo L, Fu Y et al (2021) Interstitial lung disease in Anti-MDA5 positive dermatomyositis. Clin Rev Allergy Immunol 60:293–304. https://doi.org/10.1007/s12016-020-08822-5
du Bois RM, Weycker D, Albera C et al (2011) Ascertainment of individual risk of mortality for patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 184:459–466. https://doi.org/10.1164/rccm.201011-1790OC
Ciancio N, Pavone M, Torrisi SE et al (2019) Contribution of pulmonary function tests (PFTs) to the diagnosis and follow up of connective tissue diseases. Multidiscip Respir Med 14:17. https://doi.org/10.1186/s40248-019-0179-2
Kusume K (1991) Lung injury in idiopathic pulmonary fibrosis and measurement of immunoreactive neutrophil elastase and alpha 1-protease inhibitor in blood. Nihon Kyobu Shikkan Gakkai Zasshi 29:1254–1260
Li L, Liu R, Zhang Y et al (2020) A retrospective study on the predictive implications of clinical characteristics and therapeutic management in patients with rheumatoid arthritis-associated interstitial lung disease. Clin Rheumatol 39:1457–1470. https://doi.org/10.1007/s10067-019-04846-1
Kamiya H, Panlaqui OM (2020) Systematic review and meta-analysis of prognostic factors of acute exacerbation of idiopathic pulmonary fibrosis. BMJ Open 10:e035420. https://doi.org/10.1136/bmjopen-2019-035420
Manfredi A, Sebastiani M, Cerri S et al (2017) Prevalence and characterization of non-sicca onset primary Sjogren syndrome with interstitial lung involvement. Clin Rheumatol 36:1261–1268. https://doi.org/10.1007/s10067-017-3601-1
Gao H, Zou YD, Zhang XW et al (2018) Interstitial lung disease in non-sicca onset primary Sjogren’s syndrome: a large-scale case-control study. Int J Rheum Dis 21:1423–1429. https://doi.org/10.1111/1756-185X.13334
du Bois RM, Albera C, Bradford WZ et al (2014) 6-Minute walk distance is an independent predictor of mortality in patients with idiopathic pulmonary fibrosis. Eur Respir J 43:1421–1429. https://doi.org/10.1183/09031936.00131813
Vandecasteele E, De Pauw M, De Keyser F et al (2016) Six-minute walk test in systemic sclerosis: a systematic review and meta-analysis. Int J Cardiol 212:265–273. https://doi.org/10.1016/j.ijcard.2016.03.084
Santus P, Radovanovic D, Frassanito F, Cristiano A, Rizzi M (2017) Is the six-minute walk test useful or useless in systemic sclerosis? Eur J Intern Med 43:e37–e39. https://doi.org/10.1016/j.ejim.2017.05.018
Pugnet G, Marjanovic Z, Deligny C et al (2018) Reproducibility and utility of the 6-minute walk test in systemic sclerosis. J Rheumatol 45:1273–1280. https://doi.org/10.3899/jrheum.170994
Funding
This study was supported by the grants from the National Natural Science Foundation (U1704177 and 8187811).
Author information
Authors and Affiliations
Contributions
TFL contributed to the study conception and design. YJH and XL contributed to the acquisition of data. SHH, KJG, and SSL analyzed the data. SHH drafted the manuscript. YJH and TFL revised the manuscript. All authors approved the final version of the manuscript to be published.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Ethics Committee of the First Affiliated Hospital of Zhengzhou University. Written informed consent was not required owing to the retrospective nature of the study.
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
He, SH., He, YJ., Guo, KJ. et al. Risk factors for progression of interstitial lung disease in Sjögren’s syndrome: a single-centered, retrospective study. Clin Rheumatol 41, 1153–1161 (2022). https://doi.org/10.1007/s10067-021-05984-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-021-05984-1