Abstract
Objective
Adult-onset Still’s disease (AOSD) is a systemic inflammatory disorder with clinical heterogeneity. Although tocilizumab (TCZ), an interleukin (IL)-6 receptor inhibitor, is an effective treatment for AOSD, the evidence regarding its efficacy on systemic or articular subtypes is conflicting. Furthermore, the predictors of therapeutic response are still elusive and worthy of exploration.
Methods
This two-center retrospective study analyzed the effectiveness and safety profile of TCZ treatment in 28 patients with refractory AOSD. The 28-joint disease activity score (DAS28) and systemic activity score were assessed before and during TCZ treatment period at weeks 12, 24, 36, and 48. Plasma levels of proinflammatory cytokines at baseline were determined using ELISA method.
Results
Among the systemic subtype patients, 10 (58.8%), 13 (76.5%), 14 (82.4%), and 15 (88.2%) patients achieved complete remission at week 12, 24, 36, and 48, respectively, in comparison to 2 (22.2%), 5 (55.6%), 6 (66.7%), and 7 (77.8%) who achieved disease remission (DAS28 < 2.6) at weeks 12, 24, 36, and 48, respectively, among articular subtype patients. The systemic activity scores and inflammatory parameters were significantly decreased after 12-week TCZ therapy, and TCZ could significantly reduce corticosteroid dose in AOSD patients. Multivariate analysis reveals that baseline IL-18 level is a significant predictor of poor therapeutic response at week 24 (odds ratio 7.86, p < 0.05).
Conclusion
AOSD patients refractory to high-dose corticosteroids and methotrexate may respond well to TCZ treatment with a steroid-sparing effect and an acceptable safety. A high baseline IL-18 level may be a predictor of poor therapeutic response.
Key Points • Tocilizumab may be effective and well-tolerated in refractory AOSD patients regardless of disease subtypes. • High plasma levels of IL-18 may predict poor response to tocilizumab in AOSD patients. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adult-onset Still’s disease (AOSD) is a systemic inflammatory disorder characterized by fever, rash, arthralgia or arthritis, liver dysfunction, lymphadenopathy, variable multi-systemic involvement, and increased acute phase reactant, with even life-threatening complications such as macrophage activation syndrome (MAS) [1,2,3]. With the lack of consensus or guidelines for treating AOSD currently, the mainstay treatment is corticosteroids and conventional synthetic disease-modifying anti-rheumatic drugs (csDMARDs) [4], notwithstanding that a significant proportion of patients had corticosteroid dependence or inadequate therapeutic response [5, 6].
AOSD is marked by elevated levels of proinflammatory cytokines including IL-1β, IL-6, IL-8, IL-17A, IL-18, and tumor necrosis factor (TNF)-α [7,8,9,10,11]. Increasing evidence indicates that IL-6 can enhance immune response and inflammatory reactions, which play a critical role in AOSD pathogenesis [11,12,13]. According to previous case reports and small retrospective case series, tocilizumab (TCZ), a humanized monoclonal antibody against IL-6 receptor, is effective and well-tolerated for AOSD patients [14,15,16,17,18,19,20,21,22]. A recent meta-analysis also suggests that TCZ is an effective and steroid-sparing treatment for AOSD [23]. Kaneko et al. conducted the first double-blind, randomized trial of TCZ treatment for 27 patients with refractory AOSD, revealing a significant improvement in the systemic symptoms in spite that the primary endpoint of the American College of Rheumatology (ACR)50 response (reflecting 50% improvement) was not met at week 4 [24].
The disease course of AOSD may vary considerably [25, 26] and can be divided into systemic subtype and chronic articular subtype. Based on cytokine profiles, the systemic subtype is characterized by high IL-1β and IL-18, and chronic articular subtype by high IL-8 and TNF-α, with increased IL-6 in both subtypes [12, 26]. Therefore, the therapeutic strategy for AOSD patients may be tailored according to this phenotypic dichotomy [26, 27].
In this study, we aimed to retrospectively assess the effectiveness and safety of TCZ treatment in refractory AOSD patients with either systemic or articular subtype. The effectiveness was shown in (1) the proportion of achieving complete remission, the time-course change in systemic activity scores, and corticosteroid dose during TCZ treatment in systemic subtype patients; (2) the time-course change of inflammatory parameters, including erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), ferritin, and neutrophil–lymphocyte ratio (NLR) during TCZ treatment in systemic subtype patients; and (3) the proportion of achieving disease remission and the time-course change of the 28-joint disease activity score (DAS28), swollen joint count, tender joint count, and corticosteroid dose during TCZ treatment in articular subtype patients. We also analyzed the baseline biomarkers for predicting the therapeutic response to TCZ.
Materials and methods
Subjects
This two-center retrospective study evaluates the therapeutic outcomes of TCZ, including its effectiveness and safety in 28 refractory AOSD patients at the China Medical University Hospital and Taichung Veterans General Hospital between June 2013 and May 2020. Each enrolled patient fulfilled the Yamaguchi criteria for AOSD [28], and those with infections, malignancies, or other rheumatic diseases were excluded. Refractory AOSD was defined as poor response to at least 8-week therapy with a high dose of corticosteroids (more than 0.5 mg/kg/day) and methotrexate (MTX) 10–15 mg weekly, with a poor response defined as the persistence of two or more clinical manifestations or laboratory abnormalities at enrollment. All patients received intravenous TCZ therapy at 4–8 mg/kg dose every 4 weeks and concomitant MTX at a stable weekly dose of 10–15 mg. Since IL-1 inhibitors were unavailable in Taiwan, none of our AOSD patients received this treatment. As in previous studies [27], patients were classified into two disease course subtypes: a systemic subtype, including monocyclic and polycyclic forms, and chronic articular subtype.
The systemic activity was assessed using a modified Pouchot score described by Rau et al. [29]. This systemic activity score (range 0–12) assigns one point to each of 12 manifestations: fever, evanescent rash, sore throat, arthralgia or arthritis, myalgia, pleuritis, pericarditis, pneumonitis, lymphadenopathy, hepatomegaly or abnormal liver function, elevated leukocyte count≧15,000/mm3, and serum ferritin levels > 3000 µg/L. Articular activity in chronic articular subtype patients was assessed with DAS28 [30]. Systemic activity score and DAS28 were assessed before TCZ treatment as a baseline and during the TCZ-treated period at weeks 12, 24, 36, and 48.
Patients’ demographics, medical history, the results of clinical and laboratory assessments, doses of concomitant corticosteroids, and the csDMARDs used at baseline and during the follow-up period were reviewed. Plasma cytokines levels at baseline were determined by the ELISA kits for IL-1β (RayBiotech Inc., Norcross, GA, USA), IL-6 (PeproTech Inc., Rocky Hill, NJ, USA), IL-17A (RayBiotech Inc., Norcross, GA, USA), IL-18 (Medical & Biology Laboratories Co, Ltd., Naka-Ku, Nagoya, Japan), and TNF-α (R&D Systems, Minneapolis, MN, USA) according to manufacturer’s instructions. The Institutional Review Board of both medical centers approved this study (TCVGH CE20304B, CMUH109-REC1-101), and the written consent was not needed because this is a retrospective analysis.
Determination of inflammatory parameters
Erythrocyte sedimentation rate (ESR) was determined using the Westergren method. Serum levels of ferritin were determined by chemiluminescent immunoassay sandwich method and CRP levels by nephelometry method (Dade Behring Inc. Newark, USA).
Outcome measurements
The therapeutic response (primary outcome) to TCZ treatment in systemic subtype patients was categorized into (1) complete remission if all the baseline clinical symptoms and laboratory abnormalities had resolved or (2) poor response if two or more baseline clinical manifestations or laboratory abnormalities persisted at the time of assessment during TCZ treatment [20, 27]. Regarding the therapeutic response to TCZ treatment in articular subtype patients, disease remission was defined as DAS28 ≦2.6 and poor response as DAS28 > 3.2 [31]. The secondary outcomes were the time-course change of corticosteroid dose and inflammatory parameters, including ESR, CRP, ferritin, and the NLR, in systemic subtype patients and swollen joint count plus tender joint count in articular subtype patients. The safety of TCZ treatment was reflected in the occurrence of treatment-related adverse events during the TCZ-treated period.
Statistical analysis
The results were presented as the mean ± standard deviation (SD) or median (interquartile range). The effectiveness was shown as the changes of the variables in clinical and laboratory assessments performed at baseline and weeks 12, 24, 36, and 48 of TCZ treatment, using a non-parametric Wilcoxon signed-rank test. We also constructed a multivariate regression model to identify the potential predictive factors for poor therapeutic response to TCZ treatment. We selected the variables in the multivariate model based on the statistical significance in the univariate model and the disease subtype, which reportedly predict the treatment response to TCZ. The safety analysis was performed on all patients who received at least one dose of TCZ. A probability of less than 0.05 (two-sided) was considered significant.
Results
Baseline characteristics of AOSD patients
Before TCZ treatment, spiking fevers (≥ 39℃), evanescent rash, arthralgia or arthritis, sore throat, and lymphadenopathy were noted in 23 (82.1%), 22 (78.6%), 22 (78.6%), 15 (53.6%), and 14 (50.0%) patients, respectively, at baseline. Nineteen patients (67.9%) were classified as the systemic subtype and 9 (32.1%) as the articular subtype. A significantly higher proportion of fever, higher systemic activity scores, but lower baseline plasma TNF-α levels were observed in the systemic subtype than those in the articular subtype. However, there were no significant differences in the demographic data, laboratory data, or other clinical manifestations between the systemic subtype and articular subtype patients (Table 1).
The effectiveness of TCZ treatment and the time-course change of systemic activity scores and inflammatory parameters in systemic subtype patients
All the 28 enrolled patients received at least 3 months of TCZ treatment. In the fourth month, TCZ treatment was early terminated in two systemic subtype patients: one because of poor response and the other due to the emergence of pulmonary non-tuberculosis mycobacterial (NTM) infection. The remaining 26 patients (17 systemic subtype and nine articular subtype) were evaluated for TCZ effectiveness at week 12, week 24, week 36, and week 48.
Among the 17 systemic subtype patients, 10 (58.8%), 13 (76.5%), 14 (82.4%), and 15 (88.2%) patients achieved complete remission when assessed at weeks 12, 24, 36, and 48, respectively. As shown in Fig. 1a and Table 2, the systemic subtype patients had significantly decreased systemic activity scores assessed at week 12 (p < 0.005), which were decreased further after week 12 (p < 0.001, compared with baseline values). Similarly, inflammatory parameters, including ESR, CRP, and ferritin levels, were also rapidly and significantly decreased at week 12 (p < 0.05, p < 0.01, and p < 0.005, respectively, Fig. 1b, c, d). Interestingly, the NLR was also significantly reduced at week 24 compared with the baseline value (p < 0.001) (Fig. 1e).
The change in a systemic activity scores and inflammatory parameters including b ESR, c CRP, d ferritin, e NLR, and f corticosteroid dose in AOSD patients with systemic subtype. ESR, erythrocyte sedimentation rate; CRP, C-reactive protein; NLR, neutrophil/lymphocyte ratio. P values were determined by non-parametric Wilcoxon signed rank test
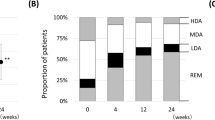
The effectiveness of TCZ treatment and the time-course change of DAS28, swollen joint count, and tender joint count in articular subtype patients
Among the nine articular subtype patients, 2 (22.2%), 5 (55.6%), 6 (66.7%), and 7 (77.8%) achieved disease remission (DAS28 < 2.6) when assessed at weeks 12, 24, 36, and 48, respectively. As illustrated in Fig. 2a–c and Table 2, the articular activity parameters, including DAS28, swollen joint count, and tender joint count, were significantly decreased at week 24 (p < 0.05, p < 0.05, and p < 0.01, respectively) and decreased further after week 24 (all p < 0.001, compared with baseline value).
The time-course change in corticosteroid dose in patients receiving TCZ treatment
TCZ treatment had a significant corticosteroid-sparing effect. As illustrated in Fig. 1f and Table 2, a significant decrease of daily corticosteroid dose at week 24 (p < 0.001) and a continuing decrease after week 24 (p < 0.001, compared with baseline value) were observed in systemic subtype patients. Similarly, the daily corticosteroid dose was significantly decreased at week 36 (p < 0.001) compared with the baseline value in articular subtype patients (Fig. 2d). Notably, our patients did not have any disease flare while receiving TCZ treatment with reduced dosage, or even discontinuation, of corticosteroids during the follow-up period. Only one patient had a disease flare 2 months after the discontinuation of both TCZ and corticosteroid therapy.
Multiple logistic regression analysis to predict therapeutic response to TCZ
A total of 9 patients were categorized as the poor responders to TCZ assessed at week 24. A multivariate regression analysis was performed to evaluate the simultaneous effects of demographic data, clinical manifestations, and baseline proinflammatory cytokines levels on the therapeutic response to TCZ. As shown in Table 3, the baseline IL-18 level was identified as a predictor of poor therapeutic response assessed at week 24 (odds ratio 7.86, 95% confidence interval 1.08–57.23, p < 0.05).
The adverse events reported during the TCZ-treated period
The severity of adverse events was assessed using common toxicity criteria [32]. During the 48-week follow-up period, three (10.7%) patients developed infections. One patient developed pulmonary NTM infection after 2 months of TCZ therapy and needed permanent termination of TCZ. Another had parvovirus B19 infection with the emergence of MAS at week 28 but continued TCZ treatment after recovering from MAS with IVIG infusion and cyclosporine treatment. The third patient had a suspicious viral infection with MAS development 2 months after disease remission and then discontinued both TCZ and corticosteroid (Table 4). One patient had transitory neutropenia, and another had a mild infusion reaction and a minimal-degree itching rash. Nevertheless, TCZ treatment did not result in death or malignancies during the follow-up period.
Discussion
In this two-center observational study, we revealed a high rate of complete remission (88.2%) in the systemic subtype and disease remission (up to 77.8%) in the articular subtype among refractory AOSD patients assessed at week 48 of TCZ treatment. A meta-analysis similarly observed a 77.9% pooled complete remission rate [23], a retrospective study reported an 82.4% response rate [27], and another showed an 81.8% EULAR remission rate at week 48 of TCZ therapy [33]. As reported previously, the systemic activity scores and inflammatory parameters were markedly decreased after 12-week TCZ therapy [20, 21, 24, 34, 35], and the corticosteroid dose could be considerably reduced in our AOSD patients [19,20,21, 24, 27]. The multivariate analysis reveals that a high baseline level of IL-18 is a significant predictor of poor therapeutic response assessed at week 24. Similar to other studies [15, 19,20,21, 24, 27, 33], TCZ treatment is well-tolerated in our refractory AOSD patients. These observations indicate that TCZ treatment is effective and well-tolerated in treating refractory AOSD patients.
Considering the crucial role of IL-6 in AOSD pathogenesis [12, 13] and the experiences with TCZ treatment [14,15,16,17,18,19,20,21,22,23,24, 26, 27], we used TCZ to treat 28 AOSD patients who were refractory to corticosteroid and MTX treatment. The good response of systemic features to TCZ treatment, reflected in significant decreases of systemic activity scores and inflammatory parameters at week 12, was consistent with previous reports showing clinical and laboratory improvement after 3–6 months of TCZ treatment [21, 24, 35]. The clinical and laboratory parameters further improved after more than 12 weeks of TCZ treatment in our AOSD patients. With the NLR serving as a marker of a systemic inflammatory response, Seo et al. demonstrated that the NLR could help to diagnose and predict relapse in AOSD [36]. Resonating with the previous findings [37], the NLR in our systemic subtype patients was significantly decreased after 24-week TCZ therapy.
Regarding the TCZ effectiveness in the chronic articular phenotype, 55.6% and 77.8% of our patients achieved disease remission (DAS28 < 2.6) at week 24 and week 48, respectively, consistent with previous reports that TCZ-treated patients had a 57% disease remission rate at week 24 [14] and 81.8% EULAR remission rate at week 48 [33]. Similarly, the DAS28 scores, swollen joint count, and tender joint count assessed at week 24 were significantly decreased. In agreement with an evidence-based review which showed that TNF-α inhibitors were less effective in refractory AOSD treatment, with an overall response rate of 12.6% compared with 76.1% for IL-6 inhibitors (TCZ) [38], four of our patients were switched from TNF-α inhibitors due to poor response. These TNF-α-refractory patients still achieved disease remission after 48-week TCZ treatment.
Based on the differential pathogenic cytokine profiles, IL-1 inhibitors could achieve superior response in the systemic subtype, whereas IL-6 inhibitors are more effective for the articular subtype compared with systemic subtype [27, 39, 40]. These observations were analogous to rheumatoid arthritis patients, who also had a good response to TCZ treatment. However, Kaneko et al. and Maria et al. revealed that TCZ might be more effective in treating systemic features than chronic arthritis in refractory AOSD patients [24, 26]. As seen in a previous study that reported different cytokine profiles between the systemic subtype and articular subtype [41], our systemic subtype patients had higher IL-18 and lower TNF-α levels at baseline compared with the articular subtype patients. However, we revealed similar effectiveness of TCZ therapy in patients with either subtype (remission rate 88.2% vs. 77.8%), which was in agreement with the findings of a recent review [40]. The results remain to be validated in future prospective studies comparing the effectiveness of TCZ in AOSD patients with dichotomous phenotypes.
Given the rarity of AOSD and limited consensus in treatment, data addressing the predictors of therapeutic response is scarce. Our multivariate analysis revealed a high baseline IL-18 level could well predict poor therapeutic response to TCZ at week 24. Given that IL-18 could be an indicator of AOSD severity [8], higher baseline systemic disease activity, as reflected in a higher IL-18 level, is probably a feature of AOSD that is less likely to remit. Our results support the findings that the IL-18 dominant group among AOSD patients required a higher mean corticosteroid dose [42], and high IL-18 levels were associated with steroid dependence [43]. However, a large patient cohort will be needed to confirm the predictive capacity of baseline IL-18 level.
Considering the importance of corticosteroids in the treatment of AOSD [4,5,6], the reduction of corticosteroid use during the follow-up period frequently induces flares [1, 2, 6]. However, none of the TCZ-treated patients had a disease flare while tapering or even after discontinuing corticosteroids in the present study. Other previous studies also showed the benefit of TCZ treatment to minimize corticosteroid exposure and the related adverse events [16,17,18,19, 23, 24, 34] or revealed that 91.9% of AOSD patients could taper corticosteroids without relapse while receiving biologic therapy [38]. Hence, TCZ treatment had a significant corticosteroid-sparing effect and could successfully prevent disease flares while reducing corticosteroid dose, supporting the usefulness of TCZ therapy in the management of refractory AOSD patients.
Interestingly, there were two episodes of MAS in our TCZ-treated patients during the follow-up period. MAS was defined as a condition meeting the following criteria: symptoms of systemic inflammatory response syndrome, cytopenia of more than two blood cell series, and hyperferritinemia. The emergence of MAS in one patient might be triggered by parvovirus B19. After recovering from MAS with IVIG infusion and cyclosporine treatment, she continued TCZ treatment and finally achieved disease remission. The other patient developed MAS 2 months after disease remission and discontinuation of both TCZ and corticosteroid. Although using TCZ to treat AOSD complicated with MAS remains controversial [44,45,46,47], the MAS resolved after this patient resumed treatment with TCZ and corticosteroid. The emergence of MAS in this patient may indicate a disease flare, supporting the findings that MAS onset frequently correlates with an active status of AOSD [3, 48].
With infections accounting for most of the adverse events in TCZ-treated patients [34], three of our patients were diagnosed with infections during the 48 weeks of TCZ treatment. Pulmonary NTM infection occurred in one patient at week 12 of TCZ therapy, resulting in its permanent termination. Another patient suffered from parvovirus B19 infection complicated with MAS at week 28 of TCZ treatment, and the other had a suspicious viral infection. These patients recovered from NTM infection or viral infections during the follow-up period.
There were, however, some limitations in this study. The retrospective nature of our study did not allow for obtaining complete information from the enrolled patients, such as data related to the calculation of ACR 20, ACR50, and ACR70 in patients with articular subtype. The lack of a significant difference to support the superiority of TCZ effectiveness in the systemic subtype compared with the articular subtype might be due to the small sample size in each subtype, a limitation inherent to the rarity of this disease. Therefore, a multicentric, prospective, and large cohort study should be conducted to further explore the effectiveness and safety of TCZ treatment in AOSD.
In conclusion, TCZ therapy may be effective and well-tolerated in treating refractory AOSD patients regardless of the subtypes. TCZ treatment is beneficial for AOSD patients refractory to high-dose corticosteroid and MTX, leading to a steroid-sparing effect and an acceptable safety profile. A high baseline IL-18 level may serve as a predictor of poor therapeutic response to TCZ treatment.
References
Ohta A, Yamaguchi M, Kaneoka H, Nagayoshi T, Hiida M (1987) Adult Still’s disease: review of 228 cases from the literature. J Rheumatol 14(6):1139–1146
Kadavath S, Efthimiou P (2015) Adult-onset Still’s disease-pathogenesis, clinical manifestations, and new treatment options. Ann Med 47(1):6–14. https://doi.org/10.3109/07853890.2014.971052
Lenert A, Yao Q (2016) Macrophage activation syndrome complicating adult onset Still’s disease: a single center case series and comparison with literature. Semin Arthritis Rheum 45(6):711–716. https://doi.org/10.1016/j.semarthrit.2015.11.002
Yoo DH (2017) Treatment of adult-onset Still’s disease: up to date. Expert Rev Clin Immunol 13(9):849–866. https://doi.org/10.1080/1744666X.2017.1332994
Castaneda S, Blanco R, Gonzalez-Gay MA (2016) Adult-onset Still’s disease: advances in the treatment. Best Pract Res Clin Rheumatol 30(2):222–238. https://doi.org/10.1016/j.berh.2016.08.003
Kalyoncu U, Solmaz D, Emmungil H et al (2016) Response rate of initial conventional treatments, disease course, and related factors of patients with adult-onset Still’s disease: data from a large multicenter cohort. J Autoimmun 69:59–63. https://doi.org/10.1016/j.jaut.2016.02.010
Choi JH, Suh CH, Lee YM et al (2003) Serum cytokine profiles in patients with adult onset Still’s disease. J Rheumatol 30(11):2422–2427
Kawaguchi Y, Terajima H, Harigai M, Hara M, Kamatani N (2001) Interleukin-18 as a novel diagnostic marker and indicator of disease severity in adult-onset Still’s disease. Arthritis Rheum 44(7):1716–1717. https://doi.org/10.1002/1529-0131(200107)44:7%3c1716::AID-ART298%3e3.0.CO;2-I
Chen DY, Chen YM, Lan JL, Lin CC, Chen HH, Hsieh CW (2010) Potential role of Th17 cells in the pathogenesis of adult-onset Still’s disease. Rheumatology (Oxford) 49(12):2305–2312. https://doi.org/10.1093/rheumatology/keq284
Hsieh CW, Chen YM, Lin CC et al (2017) Elevated expression of the NLRP3 inflammasome and its correlation with disease activity in adult-onset Still disease. J Rheumatol 44(8):1142–1150. https://doi.org/10.3899/jrheum.161354
Feist E, Mitrovic S, Fautrel B (2018) Mechanisms, biomarkers and targets for adult-onset Still’s disease. Nat Rev Rheumatol 14(10):603–618. https://doi.org/10.1038/s41584-018-0081-x
Inoue N, Shimizu M, Tsunoda S, Kawano M, Matsumura M, Yachie A (2016) Cytokine profile in adult-onset Still’s disease: comparison with systemic juvenile idiopathic arthritis. Clin Immunol 169:8–13. https://doi.org/10.1016/j.clim.2016.05.010
Sfriso P, Bindoli S, Galozzi P (2018) Adult-onset Still’s disease: molecular pathophysiology and therapeutic advances. Drugs 78(12):1187–1195. https://doi.org/10.1007/s40265-018-0956-9
Puechal X, DeBandt M, Berthelot JM et al (2011) Tocilizumab in refractory adult Still’s disease. Arthritis Care Res (Hoboken) 63(1):155–159. https://doi.org/10.1002/acr.20319
de Boysson H, Fevrier J, Nicolle A, Auzary C, Geffray L (2013) Tocilizumab in the treatment of the adult-onset Still’s disease: current clinical evidence. Clin Rheumatol 32(1):141–147. https://doi.org/10.1007/s10067-012-2105-2
Ortiz-Sanjuan F, Blanco R, Calvo-Rio V et al (2014) Efficacy of tocilizumab in conventional treatment-refractory adult-onset Still’s disease: multicenter retrospective open-label study of thirty-four patients. Arthritis Rheumatol 66(6):1659–1665. https://doi.org/10.1002/art.38398
Nishina N, Kaneko Y, Kameda H, Takeuchi T (2015) The effect of tocilizumab on preventing relapses in adult-onset Still’s disease: a retrospective, single-center study. Mod Rheumatol 25(3):401–404. https://doi.org/10.3109/14397595.2014.973659
Bannai E, Yamashita H, Kaneko S et al (2016) Successful tocilizumab therapy in seven patients with refractory adult-onset Still’s disease. Mod Rheumatol 26(2):297–301. https://doi.org/10.3109/14397595.2014.899178
Song ST, Kim JJ, Lee S et al (2016) Efficacy of tocilizumab therapy in Korean patients with adult-onset Still’s disease: a multicentre retrospective study of 22 cases. Clin Exp Rheumatol 34(6 Suppl 102):S64–S71
Li T, Gu L, Wang X et al (2017) A pilot study on tocilizumab for treating refractory adult-onset Still’s disease. Sci Rep 7(1):13477. https://doi.org/10.1038/s41598-017-13639-y
Wang CY, Guo SH, Wang LP, Shen HL (2019) Refractory adult-onset Still disease treated by tocilizumab combined with methotrexate: a STROBE-compliant article. Medicine (Baltimore) 98(32):e16682. https://doi.org/10.1097/MD.0000000000016682
Castaneda S, Martinez-Quintanilla D, Martin-Varillas JL, Garcia-Castaneda N, Atienza-Mateo B, Gonzalez-Gay MA (2019) Tocilizumab for the treatment of adult-onset Still’s disease. Expert Opin Biol Ther 19(4):273–286. https://doi.org/10.1080/14712598.2019.1590334
Ma Y, Wu M, Zhang X et al (2018) Efficacy and safety of tocilizumab with inhibition of interleukin-6 in adult-onset Still’s disease: a meta-analysis. Mod Rheumatol 28(5):849–857. https://doi.org/10.1080/14397595.2017.1416924
Kaneko Y, Kameda H, Ikeda K et al (2018) Tocilizumab in patients with adult-onset Still’s disease refractory to glucocorticoid treatment: a randomised, double-blind, placebo-controlled phase III trial. Ann Rheum Dis 77(12):1720–1729. https://doi.org/10.1136/annrheumdis-2018-213920
Franchini S, Dagna L, Salvo F, Aiello P, Baldissera E, Sabbadini MG (2010) Efficacy of traditional and biologic agents in different clinical phenotypes of adult-onset Still’s disease. Arthritis Rheum 62(8):2530–2535. https://doi.org/10.1002/art.27532
Maria AT, Le Quellec A, Jorgensen C, Touitou I, Riviere S, Guilpain P (2014) Adult onset Still’s disease (AOSD) in the era of biologic therapies: dichotomous view for cytokine and clinical expressions. Autoimmun Rev 13(11):1149–1159. https://doi.org/10.1016/j.autrev.2014.08.032
Vercruysse F, Barnetche T, Lazaro E et al (2019) Adult-onset Still’s disease biological treatment strategy may depend on the phenotypic dichotomy. Arthritis Res Ther 21(1):53. https://doi.org/10.1186/s13075-019-1838-6
Yamaguchi M, Ohta A, Tsunematsu T et al (1992) Preliminary criteria for classification of adult Still’s disease. J Rheumatol 19(3):424–430
Rau M, Schiller M, Krienke S, Heyder P, Lorenz H, Blank N (2010) Clinical manifestations but not cytokine profiles differentiate adult-onset Still’s disease and sepsis. J Rheumatol 37(11):2369–2376. https://doi.org/10.3899/jrheum.100247
Prevoo ML, van ’t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL (1995) Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 38(1):44–48. https://doi.org/10.1002/art.1780380107
Smolen JS, Aletaha D, Bijlsma JW et al (2010) Treating rheumatoid arthritis to target: recommendations of an international task force. Ann Rheum Dis 69(4):631–637. https://doi.org/10.1136/ard.2009.123919
CTEP cancer therapy evaluation program (2017) Common Terminology Criteria for Adverse Events (CTCAE) versions 5.0. National Cancer Institute. https://ctep.cancer.gov/protocoldevelopment/electronic_applications/ctc.htm#ctc_50. Accessed 17 August 2021
Cipriani P, Ruscitti P, Carubbi F et al (2014) Tocilizumab for the treatment of adult-onset Still’s disease: results from a case series. Clin Rheumatol 33(1):49–55. https://doi.org/10.1007/s10067-013-2381-5
Yoshida Y, Sakamoto M, Yokota K, Sato K, Mimura T (2011) Tocilizumab improved both clinical and laboratory manifestations except for interleukin-18 in a case of multiple drug-resistant adult-onset Still’s disease. Intern Med 50(16):1757–1760. https://doi.org/10.2169/internalmedicine.50.4771
Kir S, Ozgen M, Zontul S (2021) Adult-onset Still’s disease and treatment results with tocilizumab. Int J Clin Pract 75(3):e13936. https://doi.org/10.1111/ijcp.13936
Mercan R, Bitik B, Tufan A et al (2016) The association between neutrophil/lymphocyte ratio and disease activity in rheumatoid arthritis and ankylosing spondylitis. J Clin Lab Anal 30(5):597–601. https://doi.org/10.1002/jcla.21908
Seo JY, Suh CH, Jung JY, Kim AR, Yang JW, Kim HA (2017) The neutrophil-to-lymphocyte ratio could be a good diagnostic marker and predictor of relapse in patients with adult-onset Still’s disease: a STROBE-compliant retrospective observational analysis. Medicine (Baltimore) 96(29):e7546. https://doi.org/10.1097/MD.0000000000007546
Zhou S, Qiao J, Bai J, Wu Y, Fang H (2018) Biological therapy of traditional therapy-resistant adult-onset Still’s disease: an evidence-based review. Ther Clin Risk Manag 14:167–171. https://doi.org/10.2147/TCRM.S155488
Ortiz-Sanjuan F, Blanco R, Riancho-Zarrabeitia L et al (2015) Efficacy of anakinra in refractory adult-onset Still’s disease: multicenter study of 41 patients and literature review. Medicine (Baltimore) 94(39):e1554. https://doi.org/10.1097/MD.0000000000001554
Yoo DH (2019) Biologics for the treatment of adult-onset Still’s disease. Expert Opin Biol Ther 19(11):1173–1190. https://doi.org/10.1080/14712598.2019.1652591
Ichida H, Kawaguchi Y, Sugiura T et al (2014) Clinical manifestations of adult-onset Still’s disease presenting with erosive arthritis: association with low levels of ferritin and interleukin-18. Arthritis Care Res (Hoboken) 66(4):642–646. https://doi.org/10.1002/acr.22194
Nam SW, Kang SM, Lee JH, Yoo DH (2021) Different features of interleukin-37 and interleukin-18 as disease activity markers of adult-onset Still’s disease. J Clin Med 10(5):910. https://doi.org/10.3390/jcm10050910
Jung KH, Kim JJ, Lee JS et al (2014) Interleukin-18 as an efficient marker for remission and follow-up in patients with inactive adult-onset Still’s disease. Scand J Rheumatol 43(2):162–169. https://doi.org/10.3109/03009742.2013.824023
Tsuchida Y, Sumitomo S, Shoda H, Kubo K, Fujio K, Yamamoto K (2017) Macrophage activation syndrome associated with tocilizumab treatment in adult-onset Still’s disease. Mod Rheumatol 27(3):556–557. https://doi.org/10.1080/14397595.2016.1221875
Kobayashi M, Takahashi Y, Yamashita H, Kaneko H, Mimori A (2011) Benefit and a possible risk of tocilizumab therapy for adult-onset Still’s disease accompanied by macrophage-activation syndrome. Mod Rheumatol 21(1):92–96. https://doi.org/10.1007/s10165-010-0348-9
Wang R, Li T, Ye S et al (2020) Macrophage activation syndrome associated with adult-onset Still’s disease: a multicenter retrospective analysis. Clin Rheumatol 39(8):2379–2386. https://doi.org/10.1007/s10067-020-04949-0
Yamabe T, Ohmura SI, Uehara K, Naniwa T (2021) Macrophage activation syndrome in patients with adult-onset Still’s disease under tocilizumab treatment: a single-center observational study. Mod Rheumatol:1–8. https://doi.org/10.1080/14397595.2021.1899565
Ruscitti P, Iacono D, Ciccia F et al (2018) Macrophage activation syndrome in patients affected by adult-onset Still disease: analysis of survival rates and predictive factors in the Gruppo Italiano di Ricerca in Reumatologia Clinica e Sperimentale Cohort. J Rheumatol 45(6):864–872. https://doi.org/10.3899/jrheum.170955
Acknowledgements
The authors thank Shiow-Jiuan Wey, MD, of the Chung Shan Medical University Hospital, Taiwan, for manuscript editing. The authors also thank the Biostatistics Task Force of Taichung Veterans General Hospital, Taichung, Taiwan.
Author information
Authors and Affiliations
Contributions
K-TT and C-WH contributed equally on this work, conceived the study, acquired the clinical data, performed the data analysis, and drafted and revised the manuscript. Both Y-MC, S-HC, and H-HC performed the clinical assessment as well as data acquisition and statistical analysis. P-HH and J-LL performed the clinical assessments on study subjects and conducted the analysis of data. D-YC conceived and designed the study, generated the original hypothesis, acquired the clinical data, performed the data analysis, and also revised the manuscript.
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tang, KT., Hsieh, CW., Chen, HH. et al. The effectiveness of tocilizumab in treating refractory adult-onset Still’s disease with dichotomous phenotypes: IL-18 is a potential predictor of therapeutic response. Clin Rheumatol 41, 557–566 (2022). https://doi.org/10.1007/s10067-021-05921-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-021-05921-2