Abstract
Objectives
The Turkish population is vaccinated with Bacille Calmette-Guérin (BCG), and the BCG vaccination decreases the specificity of the tuberculin skin test (TST). The purpose of this study was to investigate the incidence of active tuberculosis (TBC) among rheumatic patients who were screened only with the QuantiFERON®-TB Gold In-Tube (QFT-GIT) test for latent TBC prior to biological treatment.
Methods
The Hacettepe University Biological Database (HUR-BIO) was used for latent TBC assessment. Consecutive patients were evaluated from July 2015 to October 2016 by a questionnaire that included the patients’ demographic characteristics, treatment history, and symptoms of active TBC. A total of 664 patients were interviewed by physicians. TBC statuses of the 671 non-interviewed patients were checked from the Turkish National Tuberculosis Registry records. Mean TBC incidence per year was calculated for anti-tumor necrosis factor-alpha (TNF-α) agents.
Results
A total of 1335 (58.2% female) patients with the mean age of 44.2 ± 12.9 years were included. Of the patients, 836 (62.6%) had spondyloarthropathy, 432 (32.4%) had rheumatoid arthritis, and 67 (5%) had other rheumatologic diseases. The total biological drug exposure was 2292 patient-years (2043 patient-years for anti-TNF-α, 249 patient-years for non-TNF-α inhibitors). Positive and indeterminate QFT-GIT results were found in 258 (19.3%) and 23 (1.7%) patients, respectively. The median follow-up time after the onset of biological agent was 19.4 months (IQR = 29.5). Pulmonary TBC was found in 3 (0.2%) of the 1335 patients. The annual incidence of TBC was 147/100,000 patient-years for all TNF-α inhibitors (249/100,000 and 123/100,000 patient-years for QFT-GIT-positive and negative patients, respectively).
Conclusions
TBC incidence increased by nearly seven times the Turkish national TBC incidence. The QFT-GIT Test appears acceptable to determine latent TBC before biological agent use. Consequently, the QFT-GIT Test can be appropriately used in BCG-vaccinated countries.
Key Points • Our study contributes to filling the gap in the literature by reflecting real-life data about TBC frequency after QFT-GIT use in patients receiving biological agents. • The frequency of active TBC will remain within acceptable limits when only QFT-GIT is used in the screening of latent TBC prior to the use of biological agents in a population where the majority are vaccinated with BCG. • Using the QFT-GIT alone for latent TBC screening prior to biologic treatment in countries with high BCG vaccination rates reduces the number of patients needing isoniazid (INH) treatment. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Latent tuberculosis (TBC) reactivation is one of the important side effects observed after biological treatments, especially after the use of tumor necrosis factor-alpha (TNF-α) inhibitors [1]. Therefore, various guidelines have been published by national and international rheumatology associations to be followed in the screening of latent TBC before biological treatment. Some guidelines recommend the use of the tuberculin skin test (TST) alone, some recommend only the interferon-gamma release test (IGRT), and some recommend the use of both [2]. On the other hand, the American College of Rheumatology recommends the use of IGRT in patients with rheumatoid arthritis (RA) and those who are vaccinated with Bacille Calmette-Guérin (BCG) [3]. The TST is affected by BCG vaccination, but the IGRT is not [4].
Isoniazid (isonicotinylhydrazide (INH)) is recommended for patients at risk of reactivation of latent TBC before biological treatment [5]. In a multicenter study, it was shown that the number of patients who would receive this treatment could be decreased by half when IGRT is used instead of TST in the screening of latent TBC before biological treatment [6]. In countries where the BCG vaccination rate is high, such as Turkey, the number of patients who should receive antibiotic treatment will drop further if IGRT is used in screening of latent TBC.
The purpose of the present study was to investigate the incidence of active TBC infection among adult rheumatic patients who were screened with the QuantiFERON®-TB Gold In-Tube (QFT-GIT) test alone for latent TBC before biological treatment. Thus, we aimed it to share long-term real-life data and results of the use of QFT-GIT alone in screening of latent TBC before the use of biological agents in a rheumatologic patient group vaccinated with BCG.
Patients and methods
HUR-BIO registry and latent TBC screening
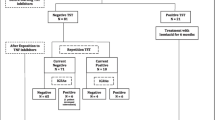
The Hacettepe University Biologic Registry (HUR-BIO) has been a single-center biologic registry since 2005 [7, 8]. In this registry, from 2005 to 2011, the TST was used to screen latent TBC before biological treatment. From May 2011, the QFT-GIT (Cellestis Limited, Carnegie, Victoria, Australia), which was available in Turkey at that time, began to be requested for screening. Positivity was defined as the TBC antigen minus Nil tube value ≥ 0.35 IU/mL and ≥ 25% of Nil value as recommended by the manufacturer [9]. Nine months of INH prophylaxis was initiated in patients with positive results.
Study population and study design
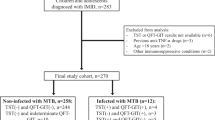
On August 1, 2015, there were 3155 patients registered in the HUR-BIO. Of these, 1606 patients had QFT-GIT results, and their records were examined in detail. Exclusion criteria for the study were as follows: patients whose biological treatment was initiated at an external center; patients who underwent TST and in whom prophylactic INH decision was made according to TST results (QFT-GIT was negative, TST ≥ 5 mm, and INH was initiated); patients with incomplete, inadequate, or conflicting data; patients on rituximab treatment without a history of switching between biological agents; and patients who received treatment for active TBC infection prior to biological treatment. Thus, patients who used biological agents other than rituximab and in whom INH prophylaxis decision was made according to QFT-GIT results were included in the study. Accordingly, 1335 patients were included in the analysis (Fig. 1).
This cross-sectional study aimed to reach 1335 patients from July 1, 2015 to October 1, 2016. The study questionnaire included information on the demographic and clinical characteristics of the patients; whether patients received prophylactic INH treatment and, if so, their compliance with INH treatment; BCG vaccination status; risk factors for TBC; and TBC symptoms. The presence of a BCG scar was evaluated by two trained research nurses. The patients who described the symptoms of active TBC were referred to the research physicians, and further examinations were then performed for TBC diagnosis. Written/verbal informed consent was obtained from the reached patients who were asked accepted to participate to the study. The study was approved by the Hacettepe University Non-Interventional Clinical Research Ethics Committee (date: 27.05.2015, Decision No: GO 15/301-08).
Screening of the national TBC records
Enhanced surveillance for TBC is being carried out in Turkey. A system, which includes not only recording and reporting of the disease but also follow-up results of its treatment, is applied. The Electronic Tuberculosis Management System (ETMS) established by the Ministry of Health was put into practice in Turkey in March 2012 [10]. In the present study, the patients who could not be contacted were checked for TBC registration on the ETMS on December 3–4, 2016. In addition, since the patients who were interviewed were likely to be diagnosed with TBC after the date of the survey, they were also checked from the ETMS to determine if they had any TBC records.
Statistical analysis
Statistical analysis was performed using the IBM SPSS Statistics for Windows, version 20.0 (IBM Corp., Armonk, NY, USA). The suitability of numerical variables for normal distribution was examined by visual (histogram and probability graphs) and analytical methods (Kolmogorov–Smirnov and Shapiro–Wilk tests). Descriptive analyses were expressed by mean ± standard deviation (SD) for normally distributed numerical variables and median and interquartile range (IQR) for non-normally distributed variables. However, although the duration of the disease was not normally distributed, the mean and median disease duration values were given together to show the difference. In independent groups, categorical data and rates were compared among groups using the eligibility criteria, Chi-square or Fisher tests, and normally distributed continuous data were compared using the Student’s t test. The Mann–Whitney U test was used to compare the median of non-normally distributed data of the independent groups. In cases where the p value was less than 0.05, results were accepted as statistically significant.
The frequency of TBC was calculated as years of exposure to biological agents and 100,000 patient-years according from the first to the last dose dates of biological agents [11]. Accordingly, 1 patient-year indicated the patients on medication for 1 year. For periods less than 1 year, the period of medication use was calculated on a monthly basis. Cumulative and annual average incidences were calculated by the following formulas:
Results
Study design and demographic and clinical features
Out of 1606 patients, 271 (16.9%) patients who had QFT-GIT results were excluded from the study (Fig. 1). Of the remaining 1335 patients, 664 (49.7%) could be interviewed (Fig. 1). There was no difference between the QFT-GIT results of the interviewed and non-interviewed patients (p = 0.522). Of 1335 patients, 777 (58.2%) were female. The mean age of all patients was 44.2 ± 12.9 years. The median disease duration of the patients was 5.9 years (IQR = 6; min = 1.8 years, max = 43 years). The median follow-up period was 19.4 months (IQR = 29.5; min: 0 month, max: 66.5 months). Of 1335 patients, 836 (62.6%) had spondyloarthropathy (SpA), 432 (32.4%) had RA, and 67 (5%) were followed up for other rheumatologic diseases (Table 1). The biological agents used and the exposure times of the patients are shown in Table 2. According to the most recent medication histories of the patients, 1140 (85.4%) patients had received one of the TNF-α inhibitors. A total of 1218 (91.2%) patients had previously received at least one TNF-α inhibitor. Overall, 399 (29.9%) of the patients had a history of switching among biological agents.
BCG vaccination, QFT-GIT results, and INH prophylaxis
Among the 1335 patients, BCG statuses of 1235 patients were known, and 1163 (94.2%) of them had had BCG vaccination. The presence of a BCG scar could only be assessed in the interviewed patients (642/664), and a BCG scar was detected in 578 of 642 (90.0%) patients.
The QFT-GIT results of 281 (21%) patients were positive or indeterminate. In 308 (23.0%) patients, 9 months of INH prophylaxis had been prescribed. Moreover, 38 (3.9%) of the patients who had negative QFT-GIT results had also prescribed to have INH prophylaxis for 9 months. Compliance with the INH treatment could only be assessed in the patients who were interviewed, and 152 of the interviewed patients (22.9%) had been treated with INH prophylaxis for 9 months. While 120 (78.9%) patients stated that they had regularly used INH treatment for 9 months, 32 patients (21.1%) stated that they had not fully complied with INH treatment. A total of 16/152 (10.5%) patients voluntarily discontinued their INH treatment before the 9-month period was completed; 10/152 (6.6%) patients used their drugs irregularly due to neglect and/or forgetting; and 6/152 (4.0%) patients discontinued their drugs upon physician advice because of increased liver function tests.
Patients with active TBC and the incidence of TBC
Screening on the ETMS revealed the TBC records of 3/1335 (0.2%) patients. In the HUR-BIO database, it was recorded that these three patients had active TBC. No additional active TBC patients were detected by the ETMS screening. The demographic and clinical characteristics of these patients diagnosed with TBC are given in Supplementary Table 1. The QFT-GIT result was positive in one patient (patient 3) and negative in two patients. At the time of diagnosis, only one of the three patients (patient 1) had had a QFT-GIT Test, and the result was negative. The other two patients had not been recommended for QFT-GIT at the time of diagnosis (see Supplementary Table 1). INH treatment was not planned for patient 1, while INH prophylaxis was planned for patients 2 and 3 for 9 months prior to biological treatment. The median time to TBC diagnosis was 28.5 months (min: 21.7 months, max: 40.5 months) after the initiation of biological agents.
The cumulative incidence of TBC in the patients receiving TNF-α inhibitor was 246/100,000. The mean annual incidence was 147/100,000 patient-years for all TNF-α inhibitors, 154/100,000 patient-years for adalimumab, 163/100000 patient-years for etanercept, and 237/100000 patient-years for infliximab. The incidence of active TBC development was calculated according to the QFT-GIT results over anti-TNF-α exposure. Total anti-TNF-α exposure of the QFT-GIT-positive patients was 401.5 patient-years, whereas anti-TNF-α exposure of those with negative results was 1625 patient-years. The incidence of TBC in the QFT-GIT-positive patients was 249/100,000 patient-years, whereas the incidence of TBC in the QFT-GIT-negative patients was 123/100,000 patient-years (Table 3).
Discussion
From the HUR-BIO registry, 1335 patients with approximately 2300 exposure years who used biological agents other than rituximab and in whom INH prophylaxis decision was made according to the QFT-GIT results were included in the study. The cumulative incidence of TBC in the patients receiving TNF-α inhibitor was 246/100,000. The mean annual incidence of TBC was 147/100,000 patient-years for all TNF-α inhibitors. In France and Spain, the incidence rates of TBC in patients using anti-TNF-α have been reported to be 12 and 7 times the incidence of TBC in the general population, respectively [5, 12]. In our study, it was found to be 7 times the incidence of TBC in the general population, which was compatible with the literature. This suggests that the incidence of active TBC would remain within acceptable limits when only QFT-GIT is used in the screening of latent TBC prior to the initiation of biological treatment.
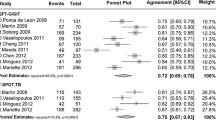
Many studies documented in the literature investigated the use of the IGRT and TST for screening of latent TBC before biological treatment in patients with rheumatic diseases [13,14,15,16]. However, most of these studies were performed in countries with low BCG vaccination. In Turkey, BCG vaccination is mandatory, and BCG scars were detected in 90% of our interviewed patients. In our real-life results, only QFT-GIT was used before the biological treatment, and the patients for whom a decision was made to administer INH prophylaxis according to the QFT-GIT results were included. To the best of our knowledge, this is the first study to investigate the incidence of active TBC with QFT-GIT use alone in the screening of latent TBC before biological treatment in a country with a high BCG vaccination rate and a low-to-moderate incidence of TBC (17–20/100,000 [11, 17, 18]). In the study by Lee et al. [19], 342 patients with arthritis who had undergone both TST and QFT-GIT before the biological treatment were examined. In that study, the decision to administer latent TBC prophylaxis was made only on the basis of QFT-GIT results, and TST results were used to measure the concordance of both tests. The study was performed in Korea where BCG vaccine was routinely administered and the frequency of TBC was moderate (70–90/100,000). The QFT-GIT positivity rate was 30.1%, and prophylaxis was started in all patients who were positive. At the end of the median follow-up period of 41.7 months, 5 (1.5%) patients developed active TBC infection, of whom 4 had negative QFT-GIT results. The incidence of TBC after anti-TNF-α exposure was reported to be about 5–6 times the incidence of TBC in the country [19]. In our study, the QFT-GIT was negative prior to biological treatment in 2 of the 3 patients who developed TBC. One had a positive QFT-GIT result and developed active TBC despite prophylactic antibiotic use. In the Korean study [19] and in our study, the increase in the incidence of TBC was similar compared with the general population (5–6 times vs. 7 times). The literature review about the incidence of active TBC infection in a “normal population” with a positive QFT-GIT Test is limited. In a prospective cohort study about the prognostic value of IFN-γ release assays and the TST in predicting the development of active TBC in high-risk groups (i.e., people in recent contact with active TBC cases and from high-burden countries), annual incidence in participants who tested positive with the QuantiFERON-TB Gold In-Tube and were not treated for latent TBC was 10.1 per 1000 person-years (7.4–13.4) [20].
Neither the TST nor IGRT is a gold standard test for latent TBC diagnosis [21]. They have advantages and disadvantages compared with each other—the TST is less expensive, and the IGRT is more specific. Owing to the similarity between the TST and BCG strains, the TST is affected by BCG vaccine while the IGRT is not [21]. In the meta-analysis by Pai et al. [22] in 2008, the sensitivities of the QFT-GIT, T-Spot test, and TST were reported to be 70%, 90%, and 77%, respectively. QFT-GIT specificity was 96% in the BCG-vaccinated populations, and 99% in the BCG-unvaccinated populations. While the TST specificity was high (97%) in the BCG-unvaccinated groups, the TST specificity was significantly reduced in the BCG-vaccinated populations (59%) [23]. When using the TST in BCG-vaccinated populations for screening latent TBC before biological treatment, the rates of positivity would be high; thus, the number of patients who need to receive INH prophylaxis would increase. For example, in the study by Cagatay et al. [24] from Turkey, 702 patients diagnosed with autoimmune-autoinflammatory disease and treated with anti-TNF-α inhibitors were examined. The patients underwent TST for the screening of latent TBC prior to the initiation of biological agent, and the positive limit was accepted as 5 mm. The TST was positive in 61.8% of the patients, and INH prophylaxis was started in 83% of the patients [24]. In a study published in France in 2012, 492 patients with RA, SpA, or Crohn’s disease, who were the candidates for anti-TNF-α, were examined [6]. It was shown that, when only QFT-GIT was used instead of the TST for screening of latent TBC, the number of patients requiring antibiotics would be halved [6]. In our study, the rate of patients who received INH prophylaxis was 23%. In other words, if only QFT-GIT is used before biological treatment, the rate of patients who should start prophylaxis would be reduced by 3–4 times. Side effects of latent TBC treatment, such as liver toxicity and neuropathy, have been acknowledged for a long time [25]. It has been shown that disease modifying antirheumatic drugs (DMARDs) and biological agents used in patients with rheumatologic diagnosis may contribute to liver toxicity caused by INH [26, 27]. In addition, the risk of severe hepatitis in patients receiving INH for treatment of latent TBC is 0.5–1.0%, while 0.05–0.1% of severe hepatitis cases result in death [25, 28,29,30,31]. Therefore, with INH treatment, we can protect patients from TBC incidence by approximately 0.02% annually in Turkey. Nevertheless, we expose the same patients to 0.5–1.0% of total hepatitis risk. Thus, reducing the number of patients needing INH treatment will also reduce the number of patients exposed to severe hepatitis risk.
Almost all of the patients who were positive for QFT-GIT received prophylactic antibiotics, whereas the majority of patients who were negative for QFT-GIT did not receive INH prophylaxis. However, the frequency of TBC was found to be approximately twice that of QFT-GIT-negative patients (249 vs. 123/100,000 patient-years). Calculating the predictive values of QFT-GIT at this point will not reflect reality, since one group received treatment, and the other group did not. However, it was found that the frequency of TBC was higher in those who tested positive. This suggests that QFT-GIT is not a gold standard test for latent TBC, but that it is a reliable screening test. Active TBC may still develop in the later stages, even in patients who have received prophylaxis and who have been screened with QFT-GIT for the diagnosis of latent TBC. For this reason, physicians should question patients receiving biological agents for signs of TBC symptoms and risk factors.
There are some limitations of this study. First, our study was a single-center study. Second, a registration system was used. Possible errors in the recording system may be reflected in the study data. However, since the records of the patients included in the study were confirmed once more from the hospital system, this effect was possibly minimized. Third, only QFT-GIT data were used; therefore, our study does not reflect the results of screening with other IGRTs. Moreover, approximately half of the patients were interviewed through a questionnaire. The follow-up periods of the patients who could not be interviewed were much shorter than those of the patients interviewed. However, the effects of this difference in follow-up time were possibly minimized based on drug last dose dates for biological agent exposure. Furthermore, patients who had previously received TBC treatment were excluded from the study. These patients had the highest risk of developing TBC after the use of biologic DMARDs. Therefore, it should be kept in mind that the results do not reflect the data of these patients. Some patients might have been followed up in external centers, and if these patients developed TBC, they would not have been known to us. The National Tuberculosis Registry System was screened to eliminate this possibility. However, the records of patients who developed TBC might not have been reported to the National Tuberculosis Registry System as of the date of screening in our study.
In conclusion, patients screened with QFT-GIT alone for latent TB prior to biologic treatment were included in the study. If only QFT-GIT is used before biological treatment, the rate of patients who should start prophylaxis will be reduced in countries with high BCG vaccination rates. This will prevent the unnecessary use of INH and reduce costs as well as prevent side effects from INH. Our study reflects a valuable experience of using QFT-GIT in a developing country with high BCG vaccination rates. Further studies will be needed to assess the country-specific cost-effectiveness of screening tests. The present study also offers valuable contributions to the literature in terms of future experiences and the use of QTF-GIT in routine practice.
References
Gomez-Reino JJ, Carmona L, Valverde VR et al (2003) Treatment of rheumatoid arthritis with tumor necrosis factor inhibitors may predispose to significant increase in tuberculosis risk: a multicenter active-surveillance report. Arthritis Rheum 48(8):2122–2127. https://doi.org/10.1002/art.11137
Denkinger CM, Dheda K, Pai M (2100) Guidelines on interferon-gamma release assays for tuberculosis infection: concordance, discordance or confusion? Clin Microbiol Infect 17(6):806–814. https://doi.org/10.1111/j.1469-0691.2011.03555.x
Singh JA, Furst DE, Bharat A, Curtis JR, Kavanaugh AF, Kremer JM, Moreland LW, O’Dell J, Winthrop KL, Beukelman T, Bridges SL Jr, Chatham WW, Paulus HE, Suarez-almazor M, Bombardier C, Dougados M, Khanna D, King CM, Leong AL, Matteson EL, Schousboe JT, Moynihan E, Kolba KS, Jain A, Volkmann ER, Agrawal H, Bae S, Mudano AS, Patkar NM, Saag KG (2012) 2012 update of the 2008 American College of Rheumatology recommendations for the use of disease-modifying antirheumatic drugs and biologic agents in the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken) 64(5):625–639. https://doi.org/10.1002/acr.21641
Vassilopoulos D, Tsikrika S, Hatzara C, Podia V, Kandili A, Stamoulis N, Hadziyannis E (2011) Comparison of two gamma interferon release assays and tuberculin skin testing for tuberculosis screening in a cohort of patients with rheumatic diseases starting anti-tumor necrosis factor therapy. Clin Vaccine Immunol 18(12):2102–2108. https://doi.org/10.1128/CVI.05299-11
Gomez-Reino JJ, Carmona L, Angel Descalzo M et al (2007) Risk of tuberculosis in patients treated with tumor necrosis factor antagonists due to incomplete prevention of reactivation of latent infection. Arthritis Rheum 57(5):756–761. https://doi.org/10.1002/art.22768
Mariette X, Baron G, Tubach F, Lioté F, Combe B, Miceli-Richard C, Flipo RM, Goupille P, Allez M, Salmon D, Emilie D, Carcelain G, Ravaud P (2012) Influence of replacing tuberculin skin test with ex vivo interferon gamma release assays on decision to administer prophylactic antituberculosis antibiotics before anti-TNF therapy. Ann Rheum Dis 71(11):1783–1790. https://doi.org/10.1136/annrheumdis-2011-200408
Kilic L, Erden A, Sari A et al (2016) AB0350 rituximab seems outstanding biological option in late onset rheumatoid arthritis: Hur-Bio real life results: BMJ. Publishing Group Ltd, London
Armagan B, Sari A, Erden A et al (2018) Starting of biological disease modifying antirheumatic drugs may be postponed in rheumatoid arthritis patients with multimorbidity: single center real life results. Medicine 97(13):e9930. https://doi.org/10.1097/md.0000000000009930 [published Online First: 2018/03/30]
QuantiFERON®-TB Gold (QFT®) ELISA Package Insert. http://www.quantiferon.com/wp-content/uploads/2017/04/English_QFT_ELISA_R04_082016.pdf. Accessed August 2016
TC Sağlık Bakanlığı Halk Sağlığı Genel Müdürlüğü. Tüberküloz Tanı Rehberi (TC Ministry of Health Tuberculosis Diagnosis Guide), 2. Baskı. (2019). Artı6 Medya Tanıtım Matbaa Ltd. Şti. https://hsgm.saglik.gov.tr/depo/birimler/tuberkuloz_db/haberler/Tuberkuloz_Tani_Ve_Tedavi_Rehberi_/Tuberkuloz_Tani_ve_Tedavi_Rehberi.pdf. Ankara. Accessed May 2019
TC Sağlık Bakanlığı Anti-TNF Kullanan Hastalarda Tüberküloz Rehberi (TC Ministry of Health Tuberculosis Guide in Patients Using Anti-TNF) (2016). http://www.romatoloji.org/Dokumanlar/Site/ATKHTR.pdf. Ankara 2016
Tubach F, Salmon D, Ravaud P, Allanore Y, Goupille P, Bréban M, Pallot-Prades B, Pouplin S, Sacchi A, Chichemanian RM, Bretagne S, Emilie D, Lemann M, Lorthololary O, Mariette X, Research Axed on Tolerance of Biotherapies Group (2009) Risk of tuberculosis is higher with anti-tumor necrosis factor monoclonal antibody therapy than with soluble tumor necrosis factor receptor therapy: the three-year prospective French research axed on tolerance of biotherapies registry. Arthritis Rheum 60(7):1884–1894. https://doi.org/10.1002/art.24632
Hsia EC, Schluger N, Cush JJ, Chaisson RE, Matteson EL, Xu S, Beutler A, Doyle MK, Hsu B, Rahman MU (2012) Interferon-gamma release assay versus tuberculin skin test prior to treatment with golimumab, a human anti-tumor necrosis factor antibody, in patients with rheumatoid arthritis, psoriatic arthritis, or ankylosing spondylitis. Arthritis Rheum 64(7):2068–2077. https://doi.org/10.1002/art.34382
Soborg B, Ruhwald M, Hetland ML et al (2009) Comparison of screening procedures for Mycobacterium tuberculosis infection among patients with inflammatory diseases. J Rheumatol 36(9):1876–1884. https://doi.org/10.3899/jrheum.081292
Martin J, Walsh C, Gibbs A, McDonnell T, Fearon U, Keane J, Codd MB, Dodd J, Veale D, FitzGerald O, Bresnihan B (2010) Comparison of interferon {gamma} release assays and conventional screening tests before tumour necrosis factor {alpha} blockade in patients with inflammatory arthritis. Ann Rheum Dis 69(1):181–185. https://doi.org/10.1136/ard.2008.101857
Smith R, Cattamanchi A, Steingart KR, Denkinger C, Dheda K, Winthrop KL, Pai M (2011) Interferon-gamma release assays for diagnosis of latent tuberculosis infection: evidence in immune-mediated inflammatory disorders. Curr Opin Rheumatol 23(4):377–384. https://doi.org/10.1097/BOR.0b013e3283474d62
TC Sağlık Bakanlığı (2015) Türkiye’de Verem Savaşı Raporu (TC Ministry of Health 2015 Tuberculosis Control Report in Turkey), Yayın No: 1059 (2016). Ankara. https://hsgm.saglik.gov.tr/depo/birimler/tuberkuloz_db/dosya/raporlar/Turkiyede_Verem_Savasi_2015_Raporu.pdf?type=file. Accessed 25 March 2017
WHO (2014) World Health Organization Global tuberculosis report. Geneva. Accessed 25 March 2017.
Lee H, Park HY, Jeon K, Jeong BH, Hwang JW, Lee J, Cha HS, Koh EM, Kang ES, Koh WJ (2015) QuantiFERON-TB Gold In-Tube assay for screening arthritis patients for latent tuberculosis infection before starting anti-tumor necrosis factor treatment. PLoS One 10(3):e0119260. https://doi.org/10.1371/journal.pone.0119260
Abubakar I, Drobniewski F, Southern J, Sitch AJ, Jackson C, Lipman M, Deeks JJ, Griffiths C, Bothamley G, Lynn W, Burgess H, Mann B, Imran A, Sridhar S, Tsou CY, Nikolayevskyy V, Rees-Roberts M, Whitworth H, Kon OM, Haldar P, Kunst H, Anderson S, Hayward A, Watson JM, Milburn H, Lalvani A, Adeboyeku D, Bari N, Barker J, Booth H, Chua F, Creer D, Darmalingam M, Davidson RN, Dedicoat M, Dunleavy A, Figueroa J, Haseldean M, Johnson N, Losewicz S, Lord J, Moore-Gillon J, Packe G, Pareek M, Tiberi S, Pozniak A, Sanderson F (2018) Prognostic value of interferon-γ release assays and tuberculin skin test in predicting the development of active tuberculosis (UK PREDICT TB): a prospective cohort study. Lancet Infect Dis 18(10):1077–1087
Matteelli A, Sulis G, Capone S, D’Ambrosio L, Migliori GB, Getahun H (2017) Tuberculosis elimination and the challenge of latent tuberculosis. Presse Med 46(2):e13–e21. https://doi.org/10.1016/j.lpm.2017.01.015
Pai M, Denkinger CM, Kik SV, Rangaka MX, Zwerling A, Oxlade O, Metcalfe JZ, Cattamanchi A, Dowdy DW, Dheda K, Banaei N (2014) Gamma interferon release assays for detection of Mycobacterium tuberculosis infection. Clin Microbiol Rev 27(1):3–20. https://doi.org/10.1128/CMR.00034-13
Pai M, Zwerling A, Menzies D (2008) Systematic review: T-cell-based assays for the diagnosis of latent tuberculosis infection: an update. Ann Intern Med 149(3):177–184
Cagatay T, Aydin M, Sunmez S et al (2010) Follow-up results of 702 patients receiving tumor necrosis factor-alpha antagonists and evaluation of risk of tuberculosis. Rheumatol Int 30(11):1459–1463. https://doi.org/10.1007/s00296-009-1170-6
Saukkonen JJ, Cohn DL, Jasmer RM, Schenker S, Jereb JA, Nolan CM, Peloquin CA, Gordin FM, Nunes D, Strader DB, Bernardo J, Venkataramanan R, Sterling TR, ATS (American Thoracic Society) Hepatotoxicity of Antituberculosis Therapy Subcommittee (2006) An official ATS statement: hepatotoxicity of antituberculosis therapy. Am J Respir Crit Care Med 174(8):935–952. https://doi.org/10.1164/rccm.200510-1666ST
Bray MG, Poulain C, Dougados M, Gossec L (2010) Frequency and tolerance of antituberculosis treatment according to national guidelines for prevention of risk of tuberculosis due to tumor necrosis factor blocker treatment. Joint Bone Spine 77(2):135–141. https://doi.org/10.1016/j.jbspin.2009.10.012
Bourre-Tessier J, Arino-Torregrosa M, Choquette D (2014) Increased incidence of liver enzymes abnormalities in patients treated with isoniazid in combination with disease modifying and/or biologic agents. Clin Rheumatol 33(8):1049–1053. https://doi.org/10.1007/s10067-014-2528-z
Hayashi PH, Fontana RJ, Chalasani NP et al (2015) Under-reporting and poor adherence to monitoring guidelines for severe cases of isoniazid hepatotoxicity. Clin Gastroenterol Hepatol 13(9):1676–1682.e1
LoBue PA, Moser KS (2003) Use of isoniazid for latent tuberculosis infection in a public health clinic. Am J Respir Crit Care Med 168(4):443–447
Control CfD, Prevention (2010) Severe isoniazid-associated liver injuries among persons being treated for latent tuberculosis infection-United States, 2004–2008. MMWR Morb Mortal Wkly Rep 59(8):224
Chalasani N, Bonkovsky HL, Fontana R et al (2015) Features and outcomes of 899 patients with drug-induced liver injury: the DILIN prospective study. Gastroenterol 148(7):1340–1352.e7
Acknowledgments
We want to thank our research nurses M. Baykal and S. Ak.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Seyhoglu, E., Uyaroğlu, O.A., Erden, A. et al. QuantiFERON®-TB Gold In-Tube test can be used for screening latent tuberculosis before biological treatment in a Bacille Calmette-Guérin (BCG)-vaccinated country: the HUR-BIO single-center real-life results. Clin Rheumatol 40, 2027–2035 (2021). https://doi.org/10.1007/s10067-020-05443-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05443-3