Abstract
Objective
To investigate specific muscle pathologies of different kinds of myositis-specific autoantibodies (MSAs) in idiopathic inflammatory myopathy (IIM) patients.
Methods
One hundred eleven Chinese patients from Xiangya Hospital, Central South University diagnosed with IIMs according to European Neuromuscular Centre (ENMC) criteria were included. Clinical manifestation, myositis-specific autoantibodies, and histologic findings were evaluated to explore the pattern of necrosis, regeneration, and perifascicular atrophy, inflammatory cells in IIM patients with different MSAs.
Results
Anti-SRP group has the lowest muscle strength scores, the highest creatine kinase levels, the most severe degree of necrosis and regeneration (1.90[0.80–3.95], 1.00[0.30–1.71]), and the lowest positive rate of MHC-I staining (35.71%). The anti-MDA5 group demonstrates the mildest pathological changes, with the fewest necrotic and regenerated muscle fibers (0.00[0.00–0.50], 0.00[0.00–0.00]), and the fewest inflammatory cell infiltration, and the highest muscle strength scores. The anti-NXP2 group has the most frequent inflammatory infiltrates, especially CD4+ T cells (31.14[15.00–39.00]). The patients with anti-NXP2 and the anti-TIF1γ antibodies show higher frequency of punched-out fibers (1.50[0.00–3.70], 0.00[0.00–1.00]) and perifascicular atrophy (71.43%, 55.56%). As for anti-synthetase antibodies (ASAs), the anti-Jo-1 group shows the most frequent rate of perifascicular necrosis (60%), while other ASA groups do not show perifascicular necrosis.
Conclusions
Of the MSAs, the anti-SRP antibody leads to the most severe muscle involvement, while the anti-MAD5 antibody the mildest. The anti-NXP2 and anti-TIF1γ groups have the most typical “DM” pathology.
Key Points • Anti-SRP group shows severe muscle pathology while anti-MDA5 group shows the mildest. • Anti-NXP2 group has the most frequent inflammatory infiltrates. Pouch-out fibers and perifascicular atrophy are more prevalent in anti-NXP2 and anti-TIF1γ groups. • Anti-Jo-1 group is often accompanied by perifascicular necrosis, while other anti-synthetase antibody groups are not. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic inflammatory myopathy is a group of acquired myopathies characterized by proximal muscle weakness, skin rashes, and sometimes extramuscular manifestations, including fever, arthralgia, and interstitial lung disease. The 2004 ENMC criteria [1] are currently the most widely used criteria for the diagnosis of inflammatory myopathies. It relies on clinical manifestations and muscle pathology to classify subtypes of IIMs as polymyositis (PM), dermatomyositis (DM), non-specific myositis (NSM), immune-mediated necrotizing myopathy (IMNM), and inclusion body myositis (IBM). The exact immune mechanisms involved in the pathogenesis in idiopathic inflammatory myopathies are still elusive. Endomysial CD8+ T cells attacking MHC-I expressing muscles are typically seen in PM patients. In contrast to the T cell-mediated cytotoxicity in PM, DM is considered humoral mediated as B cells and CD4+ T helper cells comprise the majority of the infiltrating cells in DM, and a number of autoantibodies are found associated with DM. The active muscle necrosis and absence of prominent inflammation distinguish IMNM from PM and DM [2]. So far, IIM has been considered to be an autoimmune disease due to existence of autoantibodies, presence of T cells in muscle tissue and their response to immunotherapy, but how the underlying pathogenesis causes the disease manifestations is still elusive, and now, therapies are broadly immunosuppressive rather than targeting specific pathogenic pathways.
Over the 2 decades, with the discovery of an expanding repertoire of myositis-specific autoantibodies (MSAs), it is broadly accepted that each MSA has specific clinical pictures, and their importance in predicting disease prognosis is increasing [3,4,5]. In the most adopted criteria for inflammatory myopathy, i.e., ENMC, Peter and Bohan, et al., myopathology has significant weight in diagnostic strategy. However, the discrepancy of findings of multiple muscle biopsies from the same patient may lead to different diagnoses, as was shown by a recent study [6]. It is therefore reasonable to include serum autoantibody test in the diagnosis flowchart. Most studies so far have focused on the clinical aspects of patients with MSAs [7,8,9,10], while an in-depth study of the association between MSAs and pathological manifestations is lacking [11]. In this study, our aim was to analyze pathological features of different MSAs, more specifically, to explore the pattern of necrosis, regeneration, and perifascicular atrophy, with emphasis on the levels and distribution of inflammatory cells in muscle pathology for different MSAs. The findings of this study provide clues to the pathogenesis of each MSA and may aid the differentiation of subtypes of IIMs.
Participants and methods
Participants
We retrospectively studied 111 patients diagnosed as IIMs in the Department of Neurology, Xiangya Hospital, Central South University from January 1, 2017, to July 1, 2019, including 6 cases of PM, 56 cases of DM (including 54 adult DM and 2 juvenile DM), 34 cases of IMNM, and 15 cases of NSM. The diagnosis was based on the 2004 ENMC criteria [1]. All patients have signed the informed consent. This study was approved by the Ethics Committee of Xiangya Hospital.
Clinical data collection
Demographic data including sex, age of onset, and disease duration were collected. Modified Medical Research Council motor strength scores were adopted for evaluation of muscle strength and were performed by an experienced neurologist who specialized in neuromuscular disorders (HY). The tested muscles included cervical flexors and extensors, shoulder abductors, elbow flexors and extensors, wrist flexors and extensors, finger flexors and extensors, hip flexors and extensors, knee flexors and extensors, dorsal flexors, and digital flexors.
Laboratory investigations
Clinical features and creatine levels were collected. Electromyography and nerve conduction were performed.
Muscle biopsies
For consistency reasons, biceps brachii were selected for patients demonstrating upper limb weakness with a modified MRC grading of 5–8. We have two patients with only lower limb weakness, gastrocnemius quadriceps was selected in these patients, and MRI was used for targeting muscles when necessary. Samples were immediately frozen in isopentane cooled with liquid nitrogen and preserved in − 80 °C. Sections of 8 μm thickness were cut in a cryostat (Leica, CM, 1950). Routine histological staining included hematoxylin and eosin (H&E), modified Gömöri trichrome (MGT), periodic acid Schiff (PAS), oil red O (ORO), NADH – TR, succinic dehydrogenase (SDH), cytochrome C oxidase (COX), acid phosphatase, and ATPase (PH = 4.1, 4.6, 11.0).
Immunohistochemistry
Immunohistochemical staining included MHC-I, CD4+ T cells, CD8+ T cells, CD20+ B cells, and CD68+ macrophages. Sections were fixed for 10 min in acetone at − 20 °C, incubated in 0.3% H2O2 solution (Sigma) in phosphate-buffered saline (PBS 0.01 M, pH 7.4, Sigma) for 10 min and subsequently blocked in 10% fetal bovine serum (Sigma) for 45 min. After the PBS wash, the samples were incubated with a primary antibody, and then treated with a secondary antibody. Finally, the sections were sealed in neutral balsam.
Light microscopy
The muscle biopsy results were evaluated by 5 professionals, including 2 biopsy specialists and 3 clinicians. Muscle fiber necrosis, regeneration, and punched-out fibers were counted in 10 random microscopic fields at 200 magnifications. The extent of connective tissue proliferation was classified as: normal, mild, moderate, and severe. The expression of MHC-I was classified as positive and negative. CD4+ T cells, CD8+ T cells, CD20+ B cells, and CD68+ macrophages were counted in 10 random fields at 200 magnifications, and the distribution of inflammatory cells was documented as endomysium, perimysium, and perivascular.
MSA detection
MSA antibodies were tested by using a commercial line blot assay (EUROLINE Myositis Antigen Profile 4, Euroimmun, Lübeck, Germany) including 12 myositis-specific antibodies: Mi -2α, Mi -2β, TIF1 γ, MDA5, NXP2, SAE1, Jo -1, SRP, PL-7, PL-12, EJ, OJ, and 4 myositis-associated antibodies (MAAs): Ku, PM-Scl100, PM-Scl75, and Ro-52.
Statistical analysis
The SPSS software was used for statistical analysis. Quantitative data were described as medians (first quartile and third quartile) or mean ± SD according to data distribution. Qualitative data were categorized into frequency and percentages. Nonparametric tests were used. The Kruskal-Wallis test was used for quantitative data. The chi-square test was used to analyze the frequency distribution of categorical variables, and the Fisher’s exact test was used for small sample sizes. The ranked data were tested by Kruskal-Wallis. P < 0.05 was considered statistically significant.
Results
Patients were divided into 12 groups according to types of MSA, including anti-SAE1, anti-Mi-2, anti-NXP2, anti-MDA5, anti-TIF1γ, anti-OJ, anti-PL-7, anti-EJ, anti-Jo-1, anti-SRP, double MSAs, and antibody-negative groups. Because of the rare cases in the anti-OJ and anti-SAE1 groups, these two groups were not included in the statistical analysis in case of skewing.
Distribution of clinical subtypes and MSAs in IIM patients
Our cohort consisted of 6 cases of PM (5.41%), 56 cases of DM (50.45%), 34 cases of IMNM (30.63%), and 15 cases of NSM (13.51%). The distribution of MSAs was showed in Table 1. Eighty-three patients were positive of single MSA, 6 patients were positive of double MSAs, and 22 patients were negative of MSA. Anti-SRP was the most frequent autoantibody (n = 28, 25.23%), while anti-OJ and anti-SAE1 were very rare, with only one patient respectively.
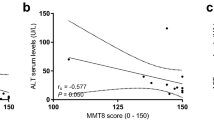
Clinical features of MSA groups
The demographic and clinical features were showed in Table 2. There was a female predominance (male: female = 1:2.36) and the numbers of females were more in all MSA groups except the anti-NXP2 group (male: female = 4:3). Patients in the anti-Mi-2 group showed the oldest onset ages than other groups (median age: 62.0), while the anti-MDA5 group the youngest (median age: 41.0, P = 0.05). The anti-EJ group had the longest disease duration (median 8.0 months), while the anti-NXP2 had the shortest disease duration (median 2.0 months, P = 0.697). Dysphagia was most frequent in the anti-SRP group (60.71%), while myalgia was most frequent in the anti-NXP2 group (71.43%). In terms of muscle strength (Online Resource 1), 93 IIM patients’ scores have been collected and the scores of cervical flexor and hip flexor are the lowest among these patients. Concerned to different IIM groups, the anti-SRP group has the lowest muscle strength scores, except the only one with anti-OJ has a lower muscle strength score. Due to small numbers in the anti-SAE1, anti-OJ, anti-PL-7, and anti-EJ groups, these four groups were not included in the statistical analysis of muscle strength. Of the 56 DM patients (Table 3), 89.29% showed cutaneous manifestations, among which all anti-Mi-2 and anti-TIF1γ patients had a classical rash. The anti-SRP group had significantly the highest CK value (median 4948.65 U/L) among all groups, while the anti-MDA5 group had the lowest CK value (median 92.20 U/L, P = 0.000). Interstitial lung disease (ILD) was more common in ASA groups (P = 0.00). Of the 28 ASS patients, 85.71% had concomitant ILD, with the highest proportion in the anti-EJ and the anti-PL-7 groups (both 100%), and the lowest in double antibodies group. There were 60.71% ASS patients having arthralgia and 42.86% having fever, with higher frequency in the anti-Jo-1 and non-anti-Jo-1 groups respectively.
Muscle pathology of MSAs
Pathological changes were presented in Table 4. Necrotic and regenerative muscle fibers were most prevalent in the anti-SRP group (necrosis: 1.90[0.80–3.95], regeneration: 1.00[0.30–1.71]), followed by the anti-Jo-1 group (necrosis: 1.70[0.43–2.55], regeneration: 0.40[0.10–0.63]), while the anti-MDA5 group had the mildest muscle pathology (necrosis: 0.00[0.00–0.50], regeneration: 0.00[0.00–0.00]). Punched-out fibers and perifascicular atrophy (Fig. 1a), the characteristics of DM, were most frequent in anti-NXP2 patients (punched-out fibers: 1.50[0.00–3.70], perifascicular atrophy: 71.43%). We also found that connective tissue proliferation was more severe in the anti-EJ group and the anti-Jo-1 group.
HE (a, b) and MHC-I immunostainings (c, d). Atrophy muscle fibers were clustered in perifascicular region in DM (a). Necrotic muscle fibers were clustered in perifascicular region in anti-Jo-1 patients (b). The MHC-I staining was positive in majority IIM patients (c) and a small number of patients were MHC-I negative (d). Magnification × 200
MHC-I staining was positive in 57.66% patients (Fig. 1c) with the highest rate in the anti-EJ and anti-NXP2 groups (100.00%, 85.71%), and the lowest in the anti-SRP group (35.71%). The difference was not statistically significant (P = 0.10). The distribution pattern of MHC-I staining was shown in Table 5. The majority of patients were sarcolemmal positive, except the anti-PL-7 group with more patients showing both sarcolemmal and sarcoplasmic MHC-I positivity. The difference of MHC-I staining distribution pattern among MSA groups was not significant (P = 0.13).
In terms of inflammatory cells (Fig. 2), CD4+ T cells (31.14[15.00–39.00]), CD8+ T cells (7.30[4.30–18.30]), and CD68+ macrophages (16.33[7.88–24.00]) were most frequent in the anti-NXP2 group, while CD20+ B cells (0.00[0.00–1.86]) were more frequent in the anti-EJ group (Table 5). Overall, the anti-MDA5 group had the least inflammatory cell infiltration (CD4: 1.00[0.06–5.60], CD8: 0.30[0.00–1.70], CD20: 0.00[0.00–0.00], CD68: 0.20[0.00–4.57]), followed by the anti-TIF1γ group. Overall, CD4+ T cells were more frequent compared with other types of inflammatory cells. Only 8 patients did not show CD4+ T cell infiltration (3 anti-TIF1γ, 2 anti-MDA5, 1 anti-SRP, 1 anti-Mi-2, and 1 seronegative). CD20+ B cells were the least frequent inflammatory cells, which could be observed in only 10 patients with anti-Mi-2, anti-NXP2, anti-EJ, anti-Jo-1, and anti-PL-7 antibodies, as well as seronegative patients. In terms of the distribution of inflammatory cells (Table 6), CD4+ T cells were predominantly endomysial in 63.1% patients, perimysial in 42.3%, and perivascular in 19.8%. CD4+ T cells were more frequent in perimysium in DM-specific antibody groups except for the anti-MDA5 group, while predominated in endomysium in ASA groups and the anti-SRP group. CD8+ T cells appeared more frequently at endomysium in almost all MSA groups except the anti-TIF1γ group. CD68+ macrophages also appeared more frequently in endomysium except in the anti-NXP2 group in which they were more perimysially located. CD20+ B cells could be found in endomysium, perimysium, and perivascular space, with no clearly preferential distribution.
Inflammatory marker immunostaining. Perimysial and endomysial infiltration of CD4+ T cells, CD8+ T cells, and CD68+ macrophages in the anti-NXP2 group (a, b, c). CD4+ T cells, CD8+ T cells, and CD68+ macrophages infiltration in necrotic muscle fibers in the anti-SRP group (d, e, f). Rare CD4+ T cells, CD8+ T cells, and CD68+ macrophages infiltration in the anti-MDA5 group (g, h, i). Magnification × 200
Pathological features in DM-specific antibodies
With regard to pathological features of 56 DM patients, 28.57% patients had punched-out fibers and 57.17% patients had perifascicular atrophy (Table 3). More specifically, 21.43% DM patients demonstrated both punched-out fibers and perifascicular atrophy, 42.86% had either punched-out fibers or perifascicular atrophy, and 35.71% showed neither changes. There was no obvious association between the occurrence of punched-out fibers and perifascicular atrophy (R2 = 0.175). The anti-NXP2 group had more frequent punched-out fibers (71.43%) and perifascicular atrophy (71.43%), while these two changes appeared least in the anti-MDA5 and anti-Mi-2 groups.
Pathological features in the anti-synthetase antibody groups
There were 28 patients with ASAs, among which 6 had double MSAs. There were 28.57% patients (6 with anti-Jo-1 antibody and 2 with double MSAs) with necrotic fibers in perifascicular region (Fig. 1b). Among these 8 patients, one was diagnosed as IMNM, 3 as NSM, 4 DM. Double MSA patients in this study all had at least one ASA, two of them had two kinds of ASA antibodies, while the other had one ASA plus another MSA. The anti-Jo-1 group showed the highest frequency of perifascicular necrosis (60.0%). In particular, two of ASA positive patients demonstrated both perifascicular necrosis and perifascicular atrophy (Fig. 3).
Discussion
Since the discovery of anti-Mi-2 antibody in 1976 [12], MSAs hold an increasingly important role in the diagnostic algorithm of IIM. It is well recognized that each type of MSA accounts for a group of myositis patients with relatively homogenous clinical pictures. Nevertheless, the muscle pathology, especially the distribution pattern of inflammatory infiltrates, associated with each MSA, has not been investigated in detail. In the present study, we have systematically examined the myopathological features of IIM patients, with emphasis on muscle inflammatory characteristics. By conducting this study, we hope to identify the relationship between MSA and myopathology and shed light on the underlying pathogenesis. In our study, 111 patients diagnosed as IIM according to the 2004 ENMC criteria were included. DM patients account for the majority (50.45%), while PM patients are the rarest (5.41%). We proposed that the rarity of PM in our cohort is at least partially accounted by the more strict definition of PM in ENMC criteria than that of the Peter and Bohan’s (e.g., the non-necrotic fiber invasion). Single MSA is present in 74.77% patients, and double MSAs in 5.41%. Anti-SRP antibody is the most common MSA (25.23%) and is found in over 90% patients diagnosed as IMNM. This number is probably an overestimation as anti-HMGCR antibody immunoassay was not available in our center by the time of this study. Anti-MDA5 and anti-TIF1γ antibodies are the most common antibodies in DM patients, which is in accordance with a previous cohort study of Chinese patients [13]. Of note, patients with anti-TIF1γ and anti-Mi-2 antibodies have been reported as the most prevalent in European population [4, 5]. Muro [14] reported that anti-SAE1 is rare in Asian population as in agreement with our study with only one anti-SAE1 patient. Anti-Jo-1 is the most frequent anti-synthetase antibodies [15], accounting for more than one-third of ASAs. Anti-OJ autoantibody is rare myositis-specific autoantibodies, as the reactivity of anti-OJ autoantibodies is heterogeneous and targets several components of the MSC (multi-enzyme synthetase complex), and the precise target of anti-OJ remains elusive [16]. Anti-PL-12 is not present in our patients. Whether anti-synthetase syndrome should be classified as an independent syndrome rather than PM or DM is beyond the scope of this study [17]. The most common MAA in our study is anti-Ro-52, which usually concurs with a variety of different MSAs, including anti-EJ, anti-MDA5, and anti-Jo-1 antibodies [18, 19].
In our study, half of the patients complain of myalgia, especially in the anti-NXP2 group, and in DM patients, myalgia accounts for 53.33%, clinically amyopathic DM accounts for 46.67%, similar in anti-MDA5 group, with 44.44% amyopathic. Among DM-specific autoantibodies, anti-MDA5 antibody is the one most related with ILD, with more than half having concomitant ILD [20, 21]. The strong association between ILD and ASA and MDA5 antibodies raises the possibility that the lung may be the primary target of the autoimmune response [22]. One hypothesis that infection of the skin and lung epithelium by certain virus upregulates the expression of MDA5 in the infected tissues [23], which may account for high relevance with skin rash and ILD in anti-MDA5 patients. Anti-SRP patients are prone to have a lower MRC muscle strength scores, while anti-MDA5 and anti-TIF1γ patients with a higher score, which is consistent with a more severe muscle pathology in the anti-SRP group and a much milder pathology in the anti-MDA5 and anti-TIF1γ group. Autoantigen TIF1γ was reported to be upregulated in both skin and muscle in DM patients [24], which in line with all of anti-TIF1γ patients in our study suffer from skin rash. Notably, anti-TIF1γ autoantibody has been reported to be strongly linked with cancer, which is hypothesized to trigger the onset of DM. The alterations of TIF1γ in tumor activate anti-tumor response which is thought to cross-react with native TIF1γ, causing clinical manifestation of muscle and skin that also express TIF1γ antigen [25]. In a DM cohort by Oldroyd, breast cancer was the most common malignancy, followed by ovarian cancer [26]. Among 9 anti-TIF1γ patients in our study, one had breast cancer, two breast nodules (BI-RADS 2 and 3 respectively) and one cervical intraepithelial neoplasia (grade I). Given the relatively short recruitment period, further follow-up is needed to evaluate the incidence of malignancy in our anti-TIF1γ cases. Anti-Mi-2 patients are also closely linked to skin rash with all the anti-Mi-2 patients in our study presenting characteristic rash. Mi-2 is essential for the development and repair of the basal epidermis and is upregulated in response to ultraviolet damage, which may provide the antigen presentation required for the development and maintenance of the autoantibodies [27].
We have systematically analyzed the association between autoantibodies and muscle pathologies. We confirm that muscle necrosis and regeneration are the main myopathological features of patients with anti-SRP antibody [28], in which macrophages infiltration and aAb deposition play important roles [29]. Interestingly, the anti-NXP2 patients have even more CD68+ macrophages than the anti-SRP group. We do not find the increased atrophic fibers in anti-SRP patients as reported by Arouche-Delaperche [30]. Contrary to anti-SRP positive cases, anti-MDA5 patients show the mildest muscle pathology with the least amount of necrotic and regenerated muscle fibers as well as inflammatory cell infiltration.
In DM patients, punched-out fibers are present in one-third of patients, and perifascicular atrophy in two-thirds of patients, both of which are most prevalent in the anti-NXP2 group. Comparing between the 33 DM-specific antibody-positive patients with the 11 ASA-positive patients in the DM group, we did not find significant clinical differences except that ASA-positive DM patients have higher CK levels and higher frequency of ILD, and that they also demonstrate more necrotic and regenerated fibers. There is no quantitative difference of inflammatory cells between these two groups. However, inflammatory cells of the DM-specific antibody group are predominantly located in perifascicular region, while the ASA DM group in endomysium.
Perifascicular necrosis is a characteristic in anti-synthetase syndrome [11, 31, 32]. Around 30% ASA-positive patients show perifascicular necrosis and two ASA-positive patients show both perifascicular necrosis and perifascicular atrophy, whereas no DM-specific antibody group patients with perifascicular atrophy have perifascicular necrosis, together with previous observations suggesting that perifascicular necrosis is specific for ASA-positive patients especially anti-Jo-1 patients [11]. None of our cases with ASAs other than anti-Jo-1 antibody demonstrated perifascicular necrosis, which is inconsistent with Uruha’s study concluding that perifascicular necrosis is a pathological feature associated with anti-Jo-1 and other anti-ARS antibodies [33]. Interestingly, contrast to increasement of antigen usually seen in other antibody groups, histidyl-tRNA synthetase (HARS) is present in the circulation of healthy individuals but undetectable in patients with anti-Jo-1 positive ASS [34].
MHC-I expression, which is undetectable immunohistochemically in normal muscle fibers, has been reported to be upregulated on the sarcolemma of IIM patients [35, 36]. Its expression can precede inflammatory infiltration and it is still detectable even after a short-term immunosuppressive treatment, which might be a strong marker of IIM. It has been reported that the combination of MHC-I and MHC-II staining results in a higher degree of specificity for the diagnosis of inflammatory myopathy [37]. MHC-I antigen has been reported along sarcolemma in non-necrotic fibers in PM and perifascicular pattern in DM [38, 39]. In our study, the anti-NXP2 group has the highest positive rate in MHC-I immunostaining while anti-SRP group the lowest. We only detect the expression of MHC-I and the distribution pattern of MHC-I is sarcolemmal in almost all groups, which is contrary to studies showing that MHC-I was upregulated in the cell membrane and cytoplasm of myofiber [40, 41]. Except for sarcolemmal or sarcoplasm distribution pattern, Englund reported that class I MHC expression was mainly confined to type II muscle fibers [42].
Pandya has shown that CD4+ CD28null and CD8+ CD28null T cells from PM patients can polarize perforin to muscle fibers and secrete IFNγ and granzyme B, leading to cell-mediated cytotoxicity towards muscle cells [43]. It is found that B cell levels and IL-4 producing CD4+ T cells are increased in flaring DM patients compared with patients in inactive stage [44]. In our study, CD4+ T cells predominate in almost all MSA groups, showing their importance in the activation of B cell and production of autoantibody. We find that CD4+ T cells can be widely distributed in perimysial, endomysial, and perivascular regions. CD4+ T cells are located more frequently at perimysium in DM-specific antibody groups including the anti-Mi-2, anti-NXP2, and anti-TIF1γ groups, and more frequently in endomysium of ASA groups. This suggests different primary inflammation-targeting regions in the two groups. In contrast, CD8+ T cells tend to be distributed at endomysium among almost all groups, while CD68+ macrophages at endomysium in the anti-SRP and ASAs groups and at endomysium and perimysium in DM-specific antibody groups. Anti-NXP2 is usually associated with cancer and calcinosis, whereas a large amount of inflammatory cell infiltrations like in our study has not been reported. Only sparse inflammatory cell infiltration in anti-SRP group was accepted. However, it has been reported that significant signs of inflammation and a complex immune response including classical complement activation are present in the skeletal muscle in anti-SRP patients [29], which aligns with our study.
Furthermore, we find that among the six patients with double-positive autoantibodies, all of them have at least one anti-synthetase antibody. These patients with one ASA plus another MSA usually have clinical symptoms in accordance with ASS, and either ASS or DM pathology.
Limitations
Firstly, the total number of patients is relatively small, which limits the power to test the difference among different antibody groups, and due to small cases in the anti-SAE1, anti-OJ groups, they are not statistically analyzed. Secondly, without profiling for anti-HMGCR autoantibody, the group of patients with this antibody remains unidentified and needs further investigation. Thirdly, serum antibodies were detected by line blot assays and the results are not verified by golden standard immunoprecipitation, but it is reported that line blot assay seems to be valid and useful to identify subgroups of IIM with specific clinical features [45]. Fourthly, lack of details of autoantibodies’ titer prevents us from studying the association between autoantibody levels and CK levels.
Conclusions
In the current study, we systematically analyzed myopathologies among different myositis-specific autoantibodies. We confirmed the severe muscle involvement in anti-SRP group and mild in anti-MDA5 and anti-TIF1γ groups. Unlike other ASAs, anti-Jo-1 group presents distinct perifascicular necrosis. Besides, we report for the first time CD4+ T cells as the most frequent inflammatory cells among MSA groups and abundant inflammatory infiltration in anti-NXP2.
Abbreviations
- IIM:
-
Idiopathic inflammatory myopathy
- PM:
-
Polymyositis
- DM:
-
Dermatomyositis
- IMNM:
-
Immune-mediated necrotic myopathy
- NSM:
-
Non-specific myositis
- IBM:
-
Inclusion body myositis
- ASA:
-
Anti-synthetase antibody
- ASS:
-
Anti-synthetase antibody syndrome
- ARS:
-
tRNA synthetase
- MSA:
-
Myositis-specific autoantibody
- MAA:
-
Myositis-associated autoantibody
- ILD:
-
Interstitial lung disease
- CK:
-
Creatine kinase
- MHC:
-
Major histocompatibility complex
References
Hoogendijk JE, Amato AA, Lecky BR, Choy EH, Lundberg IE, Rose MR, Vencovsky J, de Visser M, Hughes RA (2004) 119th ENMC international workshop: trial design in adult idiopathic inflammatory myopathies, with the exception of inclusion body myositis, 10-12 October 2003, Naarden, The Netherlands. Neuromuscul Disord 14:337–345. https://doi.org/10.1016/j.nmd.2004.02.006
Luo YB, Mastaglia FL (2015) Dermatomyositis, polymyositis and immune-mediated necrotising myopathies. Biochim Biophys Acta 1852:622–632. https://doi.org/10.1016/j.bbadis.2014.05.034
Gunawardena H, Betteridge ZE, McHugh NJ (2009) Myositis-specific autoantibodies: their clinical and pathogenic significance in disease expression. Rheumatology (Oxford) 48:607–612. https://doi.org/10.1093/rheumatology/kep078
Bodoki L, Nagy-Vincze M, Griger Z, Betteridge Z, Szollosi L, Danko K (2014) Four dermatomyositis-specific autoantibodies-anti-TIF1gamma, anti-NXP2, anti-SAE and anti-MDA5-in adult and juvenile patients with idiopathic inflammatory myopathies in a Hungarian cohort. Autoimmun Rev 13:1211–1219. https://doi.org/10.1016/j.autrev.2014.08.011
Betteridge Z, Tansley S, Shaddick G, Chinoy H, Cooper RG, New RP, Lilleker JB, Vencovsky J, Chazarain L, Danko K, Nagy-Vincze M, Bodoki L, Dastmalchi M, Ekholm L, Lundberg IE, McHugh N, UKMyonet contributors (2019) Frequency, mutual exclusivity and clinical associations of myositis autoantibodies in a combined European cohort of idiopathic inflammatory myopathy patients. J Autoimmun 101:48–55. https://doi.org/10.1016/j.jaut.2019.04.001
Hou Y, Luo YB, Dai T, Shao K, Li W, Zhao Y, Lu JQ, Yan C (2018) Revisiting pathological classification criteria for adult idiopathic inflammatory myopathies: in-depth analysis of muscle biopsies and correlation between pathological diagnosis and clinical manifestations. J Neuropathol Exp Neurol 77:395–404. https://doi.org/10.1093/jnen/nly017
Rider LG, Shah M, Mamyrova G, Huber AM, Rice MM, Targoff IN, Miller FW, Childhood Myositis Heterogeneity Collaborative Study Group (2013) The myositis autoantibody phenotypes of the juvenile idiopathic inflammatory myopathies. Medicine (Baltimore) 92:223–243. https://doi.org/10.1097/MD.0b013e31829d08f9
Habers GE, Huber AM, Mamyrova G, Targoff IN, O'Hanlon TP, Adams S et al. (2016) Brief report: association of myositis autoantibodies, clinical features, and environmental exposures at illness onset with disease course in juvenile myositis. Arthritis Rheumatol 68:761–768. https://doi.org/10.1002/art.39466
Rider LG, Nistala K (2016) The juvenile idiopathic inflammatory myopathies: pathogenesis, clinical and autoantibody phenotypes, and outcomes. J Intern Med 280:24–38. https://doi.org/10.1111/joim.12444
Srivastava P, Dwivedi S, Misra R (2016) Myositis-specific and myositis-associated autoantibodies in Indian patients with inflammatory myositis. Rheumatol Int 36:935–943. https://doi.org/10.1007/s00296-016-3494-3
Mescam-Mancini L, Allenbach Y, Hervier B, Devilliers H, Mariampillay K, Dubourg O, Maisonobe T, Gherardi R, Mezin P, Preusse C, Stenzel W, Benveniste O (2015) Anti-Jo-1 antibody-positive patients show a characteristic necrotizing perifascicular myositis. Brain 138:2485–2492. https://doi.org/10.1093/brain/awv192
Reichlin M, Mattioli M (1976) Description of a serological reaction characteristic of polymyositis. Clin Immunol Immunopathol 5:12–20. https://doi.org/10.1016/0090-1229(76)90145-8
Yang H, Peng Q, Yin L, Li S, Shi J, Zhang Y, Lu X, Shu X, Zhang S, Wang G (2017) Identification of multiple cancer-associated myositis-specific autoantibodies in idiopathic inflammatory myopathies: a large longitudinal cohort study. Arthritis Res Ther 19:259. https://doi.org/10.1186/s13075-017-1469-8
Muro Y, Sugiura K, Akiyama M (2013) Low prevalence of anti-small ubiquitin-like modifier activating enzyme antibodies in dermatomyositis patients. Autoimmunity 46:279–284. https://doi.org/10.3109/08916934.2012.755958
Betteridge Z, McHugh N (2016) Myositis-specific autoantibodies: an important tool to support diagnosis of myositis. J Intern Med 280:8–23. https://doi.org/10.1111/joim.12451
Vulsteke JB, Satoh M, Malyavantham K, Bossuyt X, De Langhe E, Mahler M (2019) Anti-OJ autoantibodies: rare or underdetected? Autoimmun Rev 18:658–664. https://doi.org/10.1016/j.autrev.2019.05.002
Benveniste O, Stenzel W, Allenbach Y (2016) Advances in serological diagnostics of inflammatory myopathies. Curr Opin Neurol 29:662–673. https://doi.org/10.1097/WCO.0000000000000376
Marie I, Hatron PY, Dominique S, Cherin P, Mouthon L, Menard JF, Levesque H, Jouen F (2012) Short-term and long-term outcome of anti-Jo1-positive patients with anti-Ro52 antibody. Semin Arthritis Rheum 41:890–899. https://doi.org/10.1016/j.semarthrit.2011.09.008
Stanciu R, Guiguet M, Musset L, Touitou D, Beigelman C, Rigolet A et al (2012) Antisynthetase syndrome with anti-Jo1 antibodies in 48 patients: pulmonary involvement predicts disease-modifying antirheumatic drug use. J Rheumatol 39:1835–1839. https://doi.org/10.3899/jrheum.111604
Fiorentino D, Chung L, Zwerner J, Rosen A, Casciola-Rosen L (2011) The mucocutaneous and systemic phenotype of dermatomyositis patients with antibodies to MDA5 (CADM-140): a retrospective study. J Am Acad Dermatol 65:25–34. https://doi.org/10.1016/j.jaad.2010.09.016
Chen F, Wang D, Shu X, Nakashima R, Wang G (2012) Anti-MDA5 antibody is associated with A/SIP and decreased T cells in peripheral blood and predicts poor prognosis of ILD in Chinese patients with dermatomyositis. Rheumatol Int 32:3909–3915. https://doi.org/10.1007/s00296-011-2323-y
Danoff SK, Casciola-Rosen L (2011) The lung as a possible target for the immune reaction in myositis. Arthritis Res Ther 13:230. https://doi.org/10.1186/ar3347
Sato S, Hoshino K, Satoh T, Fujita T, Kawakami Y, Fujita T, Kuwana M. (2009) RNA helicase encoded by melanoma differentiation-associated gene 5 is a major autoantigen in patients with clinically amyopathic dermatomyositis: association with rapidly progressive interstitial lung disease. Arthritis Rheum 60:2193–2200. https://doi.org/10.1002/art.24621
Scholtissek B, Ferring-Schmitt S, Maier J, Wenzel J (2017) Expression of the autoantigen TRIM33/TIF1gamma in skin and muscle of patients with dermatomyositis is upregulated, together with markers of cellular stress. Clin Exp Dermatol 42:659–662. https://doi.org/10.1111/ced.13180
De Vooght J, Vulsteke JB, De Haes P, Bossuyt X, Lories R, De Langhe E (2019) Anti-TIF1-gamma autoantibodies: warning lights of a tumour autoantigen. Rheumatology (Oxford) 59:469–477. https://doi.org/10.1093/rheumatology/kez572
Oldroyd A, Sergeant JC, New P, McHugh NJ, Betteridge Z, Lamb JA et al (2019) The temporal relationship between cancer and adult onset anti-transcriptional intermediary factor 1 antibody-positive dermatomyositis. Rheumatology (Oxford) 58:650–655. https://doi.org/10.1093/rheumatology/key357
Love LA, Weinberg CR, McConnaughey DR, Oddis CV, Medsger TA Jr, Reveille JD et al (2009) Ultraviolet radiation intensity predicts the relative distribution of dermatomyositis and anti-Mi-2 autoantibodies in women. Arthritis Rheum 60:2499–2504. https://doi.org/10.1002/art.24702
Watanabe Y, Uruha A, Suzuki S, Nakahara J, Hamanaka K, Takayama K, Suzuki N, Nishino I (2016) Clinical features and prognosis in anti-SRP and anti-HMGCR necrotising myopathy. J Neurol Neurosurg Psychiatry 87:1038–1044. https://doi.org/10.1136/jnnp-2016-313166
Allenbach Y, Arouche-Delaperche L, Preusse C, Radbruch H, Butler-Browne G, Champtiaux N, Mariampillai K, Rigolet A, Hufnagl P, Zerbe N, Amelin D, Maisonobe T, Louis-Leonard S, Duyckaerts C, Eymard B, Goebel HH, Bergua C, Drouot L, Boyer O, Benveniste O, Stenzel W (2018) Necrosis in anti-SRP(+) and anti-HMGCR(+)myopathies: role of autoantibodies and complement. Neurology 90:e507–e517. https://doi.org/10.1212/WNL.0000000000004923
Arouche-Delaperche L, Allenbach Y, Amelin D, Preusse C, Mouly V, Mauhin W, Tchoupou GD, Drouot L, Boyer O, Stenzel W, Butler-Browne G, Benveniste O (2017) Pathogenic role of anti-signal recognition protein and anti-3-Hydroxy-3-methylglutaryl-CoA reductase antibodies in necrotizing myopathies: myofiber atrophy and impairment of muscle regeneration in necrotizing autoimmune myopathies. Ann Neurol 81:538–548. https://doi.org/10.1002/ana.24902
Tateyama M, Shibuya S, Sato H, Fujihara K, Aoki M (2016) Pseudo-perifascicular atrophy in the healing phase of Jo-1 antisynthetase syndrome. Neuromuscul Disord 26:521–522. https://doi.org/10.1016/j.nmd.2016.06.003
Noguchi E, Uruha A, Suzuki S, Hamanaka K, Ohnuki Y, Tsugawa J, Watanabe Y, Nakahara J, Shiina T, Suzuki N, Nishino I (2017) Skeletal muscle involvement in antisynthetase syndrome. JAMA Neurol 74:992–999. https://doi.org/10.1001/jamaneurol.2017.0934
Uruha A, Suzuki S, Suzuki N, Nishino I (2016) Perifascicular necrosis in anti-synthetase syndrome beyond anti-Jo-1. Brain 139:e50. https://doi.org/10.1093/brain/aww125
Adams RA, Fernandes-Cerqueira C, Notarnicola A, Mertsching E, Xu Z, Lo WS, Ogilvie K, Chiang KP, Ampudia J, Rosengren S, Cubitt A, King DJ, Mendlein JD, Yang XL, Nangle LA, Lundberg IE, Jakobsson PJ, Schimmel P (2019) Serum-circulating His-tRNA synthetase inhibits organ-targeted immune responses. Cell Mol Immunol. https://doi.org/10.1038/s41423-019-0331-0
Karpati G, Pouliot Y, Carpenter S (1988) Expression of immunoreactive major histocompatibility complex products in human skeletal muscles. Ann Neurol 23:64–72. https://doi.org/10.1002/ana.410230111
Dalakas MC (1991) Polymyositis, dermatomyositis and inclusion-body myositis. N Engl J Med 325:1487–1498. https://doi.org/10.1056/NEJM199111213252107
Rodriguez Cruz PM, Luo YB, Miller J, Junckerstorff RC, Mastaglia FL, Fabian V (2014) An analysis of the sensitivity and specificity of MHC-I and MHC-II immunohistochemical staining in muscle biopsies for the diagnosis of inflammatory myopathies. Neuromuscul Disord 24:1025–1035. https://doi.org/10.1016/j.nmd.2014.06.436
Das L, Blumbergs PC, Manavis J, Limaye VS (2013) Major histocompatibility complex class I and II expression in idiopathic inflammatory myopathy. Appl Immunohistochem Mol Morphol 21:539–542. https://doi.org/10.1097/PAI.0b013e31827d7f16
Sundaram C, Uppin MS, Meena AK (2008) Major histocompatibility complex class I expression can be used as a diagnostic tool to differentiate idiopathic inflammatory myopathies from dystrophies. Neurol India 56:363–367. https://doi.org/10.4103/0028-3886.43457
Huang K, Li QX, Bi FF, Duan HQ, Mastaglia F, Luo YB, Yang H (2018) Comparative immunoprofiling of polymyositis and dermatomyositis muscles. Int J Clin Exp Pathol 11:3984–3993
Xiao Y, Zhu H, Li L, Gao S, Liu D, Dai B, Li Q, Duan H, Yang H, Li Q, Zhang H, Luo H, Zuo X (2019) Global analysis of protein expression in muscle tissues of dermatomyositis/polymyosisits patients demonstrated an association between dysferlin and human leucocyte antigen a. Rheumatology (Oxford) 58:1474–1484. https://doi.org/10.1093/rheumatology/kez085
Englund P, Nennesmo I, Klareskog L, Lundberg IE (2002) Interleukin-1alpha expression in capillaries and major histocompatibility complex class I expression in type II muscle fibers from polymyositis and dermatomyositis patients: important pathogenic features independent of inflammatory cell clusters in muscle tissue. Arthritis Rheum 46:1044–1055. https://doi.org/10.1002/art.10140
Pandya JM, Venalis P, Al-Khalili L, Shahadat Hossain M, Stache V, Lundberg IE et al. (2016) CD4+ and CD8+ CD28(null) T cells are cytotoxic to autologous muscle cells in patients with polymyositis. Arthritis Rheumatol 68:2016–2026. https://doi.org/10.1002/art.39650
Wienke J, Deakin CT, Wedderburn LR, van Wijk F, van Royen-Kerkhof A (2018) Systemic and tissue inflammation in juvenile dermatomyositis: from pathogenesis to the quest for monitoring tools. Front Immunol 9:2951. https://doi.org/10.3389/fimmu.2018.02951
Espinosa-Ortega F, Holmqvist M, Alexanderson H, Storfors H, Mimori T, Lundberg IE, Rönnelid J (2019) Comparison of autoantibody specificities tested by a line blot assay and immunoprecipitation-based algorithm in patients with idiopathic inflammatory myopathies. Ann Rheum Dis 78:858–860. https://doi.org/10.1136/annrheumdis-2018-214690
Funding
This work was supported by the National Natural Science Foundation of China (grant no. 81601094).
Author information
Authors and Affiliations
Contributions
Yue-Bei Luo and Huan Yang designed this study. Qiu Xu and Yue-Bei Luo collected the data and wrote the manuscript. Huan Yang revised this manuscript. Qiu-Xiang Li, Fang Fang Bi, and Hui Qian Duan contributed to the muscle pathological evaluation.
Corresponding authors
Ethics declarations
All participants or their legal guardians provided written informed consent prior to its inclusion in the present study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 217 kb)
Supplementary Table 1-6
(PDF 303 kb)
Rights and permissions
About this article
Cite this article
Xu, Q., Li, QX., Bi, FF. et al. The association between myositis-specific autoantibodies and muscle pathologies in idiopathic inflammatory myopathies. Clin Rheumatol 40, 613–624 (2021). https://doi.org/10.1007/s10067-020-05274-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05274-2