Abstract
Purpose
To explore the 18F-fluoro-dexoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) imaging characteristics of adult-onset Still’s disease (AOSD) and its significance in differential diagnosis from other connective tissue diseases (CTDs).
Methods
FDG PET/CT images of 54 patients with AOSD and 66 with other CTD from patients suffering from fever of unknown origin (FUO) were retrospectively studied and compared with 40 healthy controls. Clinical and PET/CT characteristics of AOSD and other CTDs were compared, and SUVmax (maximum standardized uptake value) was used to analyze the differences of FDG uptake in the blood pool, liver, spleen, bone marrow, and hyperplastic lymph nodes between the AOSD and other CTDs. The SUVmax ratios of the spleen, bone marrow, and lymph nodes to the liver were used to establish the diagnostic criteria for differential diagnosis of AOSD, and its diagnostic efficiency was evaluated.
Results
Positive findings are presented in 53/54 (98.1%) AOSD patients and 61/66 (92.4%) other CTD patients in PET/CT imaging. AOSD manifested as diffusely increased FDG uptake in the spleen and bone marrow, and multiple reactive hyperplasia lymph nodes are symmetrically distributed mainly in the neck and axilla, while other organs were seldom involved. Although these abnormalities could be seen in other CTDs, its incidence and uptake value were both higher in AOSD. If two or more of the following three standard were met, the sensitivity, specificity, and accuracy of diagnosing AOSD could reach 90.7%, 92.4%, and 91.7%, respectively: ① spleen SUVmax/liver SUVmax ≥ 1.2 and/or bone marrow SUVmax/liver SUVmax ≥ 1.4; ②symmetrically distributed reactive hyperplastic lymph nodes mainly in the neck and axilla with a lymph node SUVmax/liver SUVmax ≥ 1.8; and ③ no other abnormal uptake found in other organs.
Conclusion
Characteristic manifestations in AOSD were found on FDG PET/CT. These findings could help to identify AOSD from the other CTDs, especially in cases of fever of unknown origin, where it can assist in identifying the cause.
Key Points • Image characteristics of FDG PET/CT in adult-onset Still’s disease were described. • FDG PET/CT helps in identifying adult-onset Still’s disease from the other connective tissue diseases. • FDG PET/CT imaging standard for diagnosing adult-onset Still’s disease were established. |
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Adult-onset Still’s disease (AOSD) is a multisystemic connective tissue disease (CTD), which mainly manifests as fever, rash, joint pain, and pharyngeal pain. Patients were often considered as fever of unknown origin (FUO) upon their first visits to the hospital. Although clinical diagnosis of AOSD is based on the current classification criteria [1, 2], ,early diagnosis is still challenging since patients are often lack of characteristic clinical manifestations. In recent years, more and more clinical attentions have been attracted to the use of 18F-fluoro-dexoxyglucose positron emission tomography/computed tomography (FDG PET/CT) in inflammatory diseases [3,4,5,6,7,8]. Relevant studies on the AOSD have also been reported [9,10,11,12]. For patients with FUO, FDG PET/CT is useful in detecting malignant tumors or infectious lesions with its advantages of high sensitivity and wide field imaging [13,14,15,16].. However, whether FDG PET/CT can help in diagnosing different types of CTD remains unknown. Since AOSD accounts for the most common cause in CTDs in FUO, it is of great significance to understand PET/CT characteristics in AOSD. In this study, we retrospectively investigated a group of patients with CTDs who presented as FUO and underwent FDG PET/CT, in order to explore the PET/CT imaging characteristics of AOSD and its significance in differential diagnosis among CTDs.
Patients and methods
Study subjects
From January 2013 to June 2018 in Peking University people’s hospital, FDG PET/CT examination was performed in 266 FUO patients for the determination of etiology. FUO was defined as an illness of more than 3 weeks in duration, temperature exceeding 38.3 °C on more than three occasions, and diagnosis uncertain despite appropriate investigations, after at least three outpatient visits or 3 days in the hospital [17]. Among the 266 FUO patients, 120 (45.1%) were eventually diagnosed as having CTDs, and 54 of the CTDs were AOSD. AOSD was diagnosed based on the Yamaguchi’s criteria [1]. Final clinical diagnosis of other CTDs was based on the patient’s medical history as well as laboratory, image, and histopathological examinations, which meet their respective clinical classification criteria. Table 1 listed the final clinical diagnosis for all of the 266 FUO patients. All patients were provided with laboratory examination data within 3 days before and after the PET/CT examination and the results of more than 1 year of clinical follow-up. The 54 patients with AOSD and 66 patients with other CTDs were studied and compared with the 40 cases with negative PET/CT findings that underwent PET/CT examination for the purpose of health examination. Table 2 shows the general information of the study subjects.
FDG PET/CT imaging
All patients were fasted at least 6 h before PET imaging, and the blood glucose of the patients was controlled below 200 mg/dL. 18F-FDG (provided by Atom High-Tech Co., Ltd., Beijing, China) was injected intravenously at 5.55 MBq/kg (0.15 mCi/kg). Fifty minutes later, the patients lied in a supine position in the examination bed with both upper limbs placed at the sides of the body. Imaging ranging from the base of the skull to the middle of the tibia was acquired for each patient by using Discovery VCT PET/CT Scanner (GE Healthcare, Milwaukee, WI, USA). Images were reconstructed as three-dimensional PET, CT, and fusion images with a slice thickness of 3.3 mm. According to the patient’s situation, the range of image acquisition is appropriately increased from head to toe, sometimes an additional chest high resolution CT or local contrast CT is added.
Image analysis
More than three experienced nuclear medicine physicians read the images together by visual judgment, to determine whether there was abnormal FDG uptake and/or structural changes in the imaging field. Location, number, FDG uptake, and systemic distribution of abnormal lesions were recorded, and their natures were judged in combination with the clinical data. In addition, using the three-dimensional region of interest (3D ROI) technique, the maximum standardized uptake value (SUVmax) of the blood pool, liver, spleen and spine were measured and recorded by one fixed physician (Fig. 1). When an abnormal lymph node was found, its SUVmax was also measured and recorded.
Data analysis
Clinical features were compared between the patients with AOSD and other CTD. In image analysis, visual judgment was firstly used to analyze the image characteristics for AOSD patients and other CTD patients. Semi-quantitative parameter SUVmax was applied to compare the FDG uptake in referred organs in AOSD patients and other CTD patients. The ratios of SUVmax in the spleen, bone marrow, and lymph nodes to SUVmax in the liver were further used as diagnostic parameters, and the threshold for each parameter was determined by the receiver operating characteristic curve (ROC) analysis, respectively. Then the image diagnostic standard for AOSD was established based on the visual and quantitative parameters, and its diagnostic efficiency was evaluated.
Statistical analysis
Statistical analysis in this study was carried out by SPSS software (SPSS Inc. Released 2007). Among the different groups, the Student’s t-test was used to analyze the difference of ages; Chi-square test was used to analyze the nominal parameters, such as the clinical characteristics; the LSD t-test was used to analyze the differences in lesion uptake; ROC curve analysis was used to evaluate the diagnostic threshold of FDG uptake between AOSD and other CTDs group. Difference was considered statistically significant when P value was found less than 0.05.
Results
The clinical characteristics of AOSD and other CTDs were listed in Table 3. In this study, the average onset age of AOSD was younger than other CTDs, and AOSD was more likely to occur in women. In AOSD patients, the incidence of rash, arthralgia, sore throat, leukocytosis, elevated neutrophil, and abnormal liver function were significantly higher than in other CTD patients, while more autoantibodies were detected in other CTDs. No significant difference was found in the elevated serum level of C-reactive protein (CPR) and erythrocyte sedimentation rate (ESR) between the two groups.
On PET/CT examinations, positive findings were detected in 53/54 (98.1%) of patients with AOSD and 61/66 (92.4%) of patients with other CTD, showing diffuse or focal high uptake of FDG in various organs and tissues (Table 4).
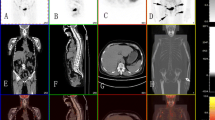
In patients with AOSD, PET/CT showed splenomegaly, diffusely increased FDG uptake in both the spleen and bone marrow, but no significant density or structural changes. Multiple and symmetrically distributed reactive hyperplastic lymph nodes with increased FDG uptake could be seen throughout the body; most of which were found in the neck and axilla. These lymph nodes were long oval in shape and maintained normal structure, with the maximum short diameter ≤ 1.2 cm. Besides, no involvement of other organs was found in most of the AOSD patients, with the exception of a few patients with articular synovitis and salivary gland inflammatory lesions (Fig. 2).
FDG PET/CT images in a 32-year-old female who manifested clinically as FUO. PET/CT showed splenomegaly, diffusely increased FDG uptake in both the spleen and bone marrow, reactive hyperplastic lymph nodes symmetrically distributed in the bilateral neck and axilla, and no other positive findings were found throughout the body. Final clinical diagnosis for the patient was AOSD
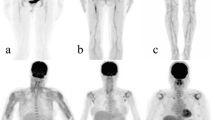
In patients with other CTD, although diffuse uptake in the spleen and bone marrow could also be seen, the incidence was significantly lower than in patients with AOSD (P < 0.001). Reactive hyperplastic lymph nodes were also found, but the distribution patterns as in the neck and axilla were less common. While the high uptake lesions in other tissues became the major positive findings on PET/CT, with or without structural changes. Various tissue involvements were observed, corresponding to disease characteristics, respectively, such as joints, blood vessels, muscles, lungs, and subcutaneous soft tissues (Fig. 3).
FDG PET/CT images in patients with other connective tissue diseases. A abnormal uptake of FDG in large and middle blood vessels in a patient with giant cell arteritis; B abnormal muscle uptake in a patient with idiopathic inflammatory myopathy; and C abnormal synovial uptake of multiple joints in a patient with rheumatoid arthritis
The results of semi-quantitative analysis showed that the average SUVmax of the spleen and bone marrow were significantly higher in both AOSD patients and other CTD patients comparing with the control group, and the SUVmax of the liver was significantly lower. Meantime, AOSD patients showed higher uptake of FDG in the spleen, bone marrow, and positive lymph nodes than other CTD patients (Table 5).
In our study, the following imaging findings were considered to be associated with the presence of AOSD: ① spleen SUVmax/liver SUVmax ≥ 1.2 and/or bone marrow SUVmax/liver SUVmax ≥ 1.4; ②symmetrically distributed reactive hyperplastic lymph nodes that mainly distributed in the neck and axilla, with a lymph node SUVmax/liver SUVmax ratio ≥ 1.8; and ③ no other abnormal uptake found in other organs. When two or more standards above were met, the diagnostic sensitivity, specificity, and accuracy for AOSD reached 90.7%, 92.4%, and 91.7%, respectively. According to this image diagnosis standard, there were 5 false positives and 5 false negatives. Three of the false negative patients had recently received glucocorticoid therapy. False positive patients were eventually diagnosed with undifferentiated CTD (2), idiopathic inflammatory myopathy (2), or systemic lupus erythematosus (1).
Discussion
AOSD is predisposed to middle-aged and young people [18], and its pathogenesis is not completely clear. It is generally believed that it is related to the immune mechanism triggered by inflammatory factors. Overexpression of macrophage colony-stimulating factors induces macrophage differentiation and promotes the expression of sequential pro-inflammatory factors, including IL-1b, IL-6, IL-8, IL-18, tumor necrosis factor-A (TNF-α), and interferon-y (IFN- γ) [19, 20]. Early diagnosis of AOSD is important because treatment in time can ameliorate patients’ prognosis efficiently [21]. Although Yamaguchi classification criteria could be used in the diagnosis of AOSD, malignances, infections, and other CTDs must be excluded first in the diagnostic process. It is well-known that FDG PET/CT plays an important role in detecting malignant tumors, and it is also promising in detecting infectious lesions [13, 14]. Therefore, during the diagnosis of AOSD, FDG PET/CT could help detect or exclude malignant tumors and infectious lesions and suggest reasonable biopsy site, thus further establish the diagnosis [9,10,11,12]. Some researchers demonstrated that the FDG uptake was correlated with disease activity and could also be used to evaluate the progress of disease and therapeutic effects [9, 12, 22].
When FDG is used for inflammatory imaging, the lesion uptake of FDG is correlated with capillary dilatation and inflammatory cell infiltration [23, 24]. Previous studies suggested that patients with AOSD mainly showed multiple enlarged lymph nodes on FDG PET/CT, as well as increased diffuse FDG uptake in the spleen and bone marrow [9,10,11]. On the other hand, Dr. Yamashita et al. reported additional abnormal uptake in the joints, salivary glands, pericardium, and pleura in AOSD [12]. However, these studies did not clarify the morphological and distribution characteristics of lymph nodes, nor did they compare the abnormal uptake of AOSD patients with other CTD patients. Our study showed that the reported PET/CT manifestations in AOSD could also be seen in other CTDs. But AOSD usually has the following features: diffuse uptake of FDG in the spleen and bone marrow is more common and higher than other CTDs, suggesting the inflammatory responses in the above-mentioned organs were more active [25, 26]. Multiple reactive hyperplastic lymph nodes are symmetrically distributed in various lymph node regions of the body but mainly in the neck and axilla; and other organs seldomly involved. When these imaging features were used in the diagnosis of AOSD, a satisfactory diagnostic efficiency could be obtained. In fact, combining the imaging findings with the patients’ clinical manifestations (such as fever, rash, sore throat, leukocytosis, elevated neutrophils, and liver dysfunction) would yield a more confident diagnosis.
The etiology of FUO includes infections, CTDs, malignances, and some miscellaneous diseases. When PET/CT is introduced to the diagnosis process, it appears to be easy for nuclear medicine physicians to detect or exclude malignances, since malignant tumors often showed occupying effect of malignant growth and higher FDG uptake compared with benign lesions [7]. The value of PET/CT in detecting infectious lesions has also been recognized [13, 15]. However, in CTDs, although PET/CT is positive in most of the cases, some non-focal uptake were often overlooked, or regarded as “non-specific uptake” with no diagnostic significance [27,28,29,30,31], such as diffuse high uptake on spleen and bone marrow. Therefore, it remains controversial whether PET/CT can be helpful for the classification of CTDs in FUO patients. Although the use of FDG PET/CT in various CTDs have been reported, such as vasculitis [8], idiopathic inflammatory myopathy [5], rheumatoid arthritis, and systemic lupus erythematous [6], cohort studies on image characteristics and its diagnostic significance are still rare. Considering that the 32.4% of FUO patients are caused by CTDs, AOSD is the most common disease within the CTDs [7]. we investigated the significance of FDG PET/CT in early differential diagnosis of AOSD from other CTDs. Results of our study suggested that FDG PET/CT is an effective technique for early diagnosing of AOSD, and the distribution status of inflammatory lesions could provide a basis for CTDs classification. Of course, PET/CT image characteristics in other CTDs still require to be confirmed.
For AOSD patients, differential diagnosis with lymphoma should be considered. It was thought by some scholars that the radiologic findings of AOSD on FDG PET/CT were similar to lymphoma [11, 12]. However, it has been suggested from our current study that AOSD image features displayed on FDG PET/CT can be used not only to differentiate other CTDs but also to differentiate lymphoma, although the relevant analysis data was not included in the study. Based on our clinical experience, enlarged lymph nodes with different morphologic findings from reactive hyperplasia were usually found in lymphoma. In our opinion, if a FUO patient who met the Yamaguchi criteria and manifested multiple, symmetrically distributed lymph nodes with increased FDG uptake and normal structure on PET/CT, especially when a reactive hyperplasia lymph node was demonstrated by biopsy, lymphoma should be excluded. Otherwise, it might delay the proper treatment and waste medical resources.
References
Yamaguchi M, Ohta A, Tsunematsu T, Kasukawa R, Mizushima Y, Kashiwagi H, Kashiwazaki S, Tanimoto K, Matsumoto Y, Ota T (1992) Preliminary criteria for classification of adult Still's disease. J Rheumatol 19:424–430
Cush JJ, Medsger TA Jr, Christy WC, Herbert DC, Cooperstein LA (1987) Adult-onset Still's disease. Clinical course and outcome. Arthritis Rheum 30:186–194
Wenter V, Muller JP, Albert NL, Lehner S, Fendler WP, Bartenstein P et al (2016) The diagnostic value of [(18)F]FDG PET for the detection of chronic osteomyelitis and implant-associated infection. Eur J Nucl Med Mol Imaging 43:749–761. https://doi.org/10.1007/s00259-015-3221-4
Kubota K, Yamashita H, Mimori A (2017) Clinical value of FDG-PET/CT for the evaluation of rheumatic diseases: rheumatoid arthritis, polymyalgia rheumatica, and relapsing polychondritis. Semin Nucl Med 47:408–424. https://doi.org/10.1053/j.semnuclmed.2017.02.005
Li Y, Zhou Y, Wang Q (2017) Multiple values of (18)F-FDG PET/CT in idiopathic inflammatory myopathy. Clin Rheumatol 36:2297–2305. https://doi.org/10.1007/s10067-017-3794-3
Curiel R, Akin EA, Beaulieu G, DePalma L, Hashefi M (2011) PET/CT imaging in systemic lupus erythematosus. Ann N Y Acad Sci 1228:71–80. https://doi.org/10.1111/j.1749-6632.2011.06076.x
Wang Q, Li YM, Li Y, Hua FC, Wang QS, Zhang XL, Cheng C, Wu H, Yao ZM, Zhang WF, Hou QY, Miao WB, Wang XM (2019) (18)F-FDGPET/CT in fever of unknown origin and inflammation of unknown origin: a Chinese multi-center study. Eur J Nucl Med Mol Imaging 46:159–165. https://doi.org/10.1007/s00259-018-4121-1
Andrews J, Al-Nahhas A, Pennell DJ, Hossain MS, Davies KA, Haskard DO et al (2004) Non-invasive imaging in the diagnosis and management of Takayasu's arteritis. Ann Rheum Dis 63:995–1000. https://doi.org/10.1136/ard.2003.015701
Choe JY, Chung DS, Park SH, Kwon HH, Kim SK (2010) Clinical significance of (1)(8)F-fluoro-dexoxyglucose positron emission tomography in patients with adult-onset Still's disease: report of two cases and review of literatures. Rheumatol Int 30:1673–1676. https://doi.org/10.1007/s00296-009-1137-7
Dong MJ, Wang CQ, Zhao K, Wang GL, Sun ML, Liu ZF, Xu L (2015) 18F-FDG PET/CT in patients with adult-onset Still's disease. Clin Rheumatol 34:2047–2056. https://doi.org/10.1007/s10067-015-2901-6
Jiang L, Xiu Y, Gu T, Dong C, Wu B, Shi H (2017) Imaging characteristics of adult onset Still's disease demonstrated with 18F-FDG PET/CT. Mol Med Rep 16:3680–3686. https://doi.org/10.3892/mmr.2017.7022
Yamashita H, Kubota K, Takahashi Y, Minamimoto R, Morooka M, Kaneko H et al (2014) Clinical value of (1)(8)F-fluoro-dexoxyglucose positron emission tomography/computed tomography in patients with adult-onset Still's disease: a seven-case series and review of the literature. Mod Rheumatol 24:645–650. https://doi.org/10.3109/14397595.2013.850998
Bleeker-Rovers CP, de Kleijn EMHA, Corstens FHM, van der Meer JWM, Oyen WJG (2004) Clinical value of FDG PET in patients with fever of unknown origin and patients suspected of focal infection or inflammation. Eur J Nucl Med Mol Imaging 31:29–37. https://doi.org/10.1007/s00259-003-1338-3
Gallamini A, Zwarthoed C, Borra A (2014) Positron emission tomography (PET) in oncology. Cancers. 6:1821–1889. https://doi.org/10.3390/cancers6041821
Treglia G, Pascale M, Lazzeri E, van der Bruggen W, Delgado Bolton RC, Glaudemans AWJM (2019) Diagnostic performance of (18)F-FDG PET/CT in patients with spinal infection: a systematic review and a bivariate meta-analysis. Eur J Nucl Med Mol Imaging. https://doi.org/10.1007/s00259-019-04571-6
Kouijzer IJE, Mulders-Manders CM, Bleeker-Rovers CP, Oyen WJG (2018) Fever of unknown origin: the value of FDG-PET/CT. Semin Nucl Med 48(2):100–107. https://doi.org/10.1053/j.semnuclmed.2017.11.004
Knockaert DC, Vanderschueren S, Blockmans D (2003) Fever of unknown origin in adults: 40 years on. J Intern Med 253:263–275
Liu Z, Lv X, Tang G (2015) Clinical features and prognosis of adult-onset Still's disease: 75 cases from China. Int J Clin Exp Med 8:16634–16639
Der-Yuan C, Joung-Liang L, Fang-Ju L, Tsu-Yi HJJR (2004) Proinflammatory cytokine profiles in sera and pathological tissues of patients with active untreated adult onset Still's disease. 31:2189–2198
Fitzgerald AA, Leclercq SA, Alexander Y, Homik JE, Dinarello CA (2014) Rapid responses to anakinra in patients with refractory adult-onset Still's disease. Arthritis Rheum 52:1794–1803
Gerfaud-Valentin M, Jamilloux Y, Iwaz J, Seve P (2014) Adult-onset Still's disease. Autoimmun Rev 13:708–722. https://doi.org/10.1016/j.autrev.2014.01.058
An YS (2017) The role of (18)F-fluorodeoxyglucose positron emission tomography in the assessment of disease activity of adult-onset Still’s disease. 32:1082–1089. https://doi.org/10.3904/kjim.2015.322
Forstrom LA, Dunn WL, Mullan BP, Hung JC, Lowe VJ, Thorson LM (2002) Biodistribution and dosimetry of [(18)F]fluorodeoxyglucose labelled leukocytes in normal human subjects. Nucl Med Commun 23:721–725
Pak K, Kim SJ, Kim IJ, Kim DU, Kim K, Kim H (2013) Impact of cytokines on diffuse splenic 18F-fluorodeoxyglucose uptake during positron emission tomography/computed tomography. Nucl Med Commun 34:64–70. https://doi.org/10.1097/MNM.0b013e3283595cac
Rosario C, Zandman-Goddard G, Meyron-Holtz EG, D'Cruz DP, Shoenfeld Y (2013) The hyperferritinemic syndrome: macrophage activation syndrome, Still's disease, septic shock and catastrophic antiphospholipid syndrome. BMC Med 11:185. https://doi.org/10.1186/1741-7015-11-185
Uppal SS, Al-Mutairi M, Hayat S, Abraham M, Malaviya A (2007) Ten years of clinical experience with adult onset Still's disease: is the outcome improving? Clin Rheumatol 26:1055–1060. https://doi.org/10.1007/s10067-006-0440-x
Keidar Z, Gurman-Balbir A, Gaitini D, Israel O (2008) Fever of unknown origin: the role of 18F-FDG PET/CT. J Nucl Med 49(12):1980–1985. https://doi.org/10.2967/jnumed.108.054692
Ergül N, Halac M, Cermik TF, Ozaras R, Sager S, Onsel C, Uslu I (2011) The diagnostic role of FDG PET/CT in patients with fever of unknown origin. Mol Imaging Radionucl Ther 20:19–25. https://doi.org/10.4274/MIRT.20.04
Tokmak H, Ergonul O, Demirkol O, Cetiner M, Ferhanoglu B (2014) Diagnostic contribution of (18)F-FDG-PET/CT in fever of unknown origin. Int J Infect Dis 19:53–58. https://doi.org/10.1016/j.ijid.2013.10.009
Gafter-Gvili A, Raibman S, Grossman A, Avni T, Paul M, Leibovici L, Tadmor B, Groshar D, Bernstine H (2015) [18F]FDG-PET/CT for the diagnosis of patients with fever of unknown origin. QJM 108:289–298. https://doi.org/10.1093/qjmed/hcu193
Schönau V, Vogel K, Englbrecht M et al (2018) The value of 18F-FDG PET/CT in identifying the cause of fever of unknown origin (FUO) and inflammation of unknown origin (IUO): data from a prospective study. Ann Rheum Dis 77(1):70–77. https://doi.org/10.1136/annrheumdis-2017-211687
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent does not apply as this is a review manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, X., Li, Y. & Wang, Q. FDG PET/CT used in identifying adult-onset Still’s disease in connective tissue diseases. Clin Rheumatol 39, 2735–2742 (2020). https://doi.org/10.1007/s10067-020-05041-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05041-3