Abstract
Introduction/objective
We aimed to establish sex-specific reference values of objective physical function tests among individuals with or at risk for knee osteoarthritis (KOA) across subsets of age, radiographic KOA severity, and body mass index (BMI).
Method
We included Osteoarthritis Initiative participants with data for objective physical function tests, sex, age, BMI, and radiographic KOA severity (Kellgren-Lawrence [KL] grade) at baseline. Objective physical function was quantified with 20-m walk speed, chair-stand speed, 400-m walk time, and knee extension and flexion strength. We created participant characteristic subsets for sex, age, KL grade, and BMI. Reference values were created as percentiles from minimum to maximum in 10% increments for each combination of participant characteristic subsets. Previously established clinically important differences for 20-m walk speed and knee extension strength were used to highlight clinically relevant differences.
Results
Objective physical function reference values tables and an interactive reference value table were created across all combinations of sex, age, KL grade, and BMI among 3860 individuals with or at risk for KOA. Clinically relevant differences exist for 20-m walk speed and knee extension strength between males and females across age groups, KL grades, and BMI categories.
Conclusions
Establishing an individual’s relative level of objective physical function by comparing their performance to individuals with similar sex, age, KL grade, or BMI may help improve interpretation of physical function performance. The interactive reference value table will provide clinicians and researchers a clinically accessible avenue to use these reference values.
Key Points • Since greater age, radiographic knee osteoarthritis severity, and body mass index are all associated with worse objective physical function, reference values should consider the complex inter-play among these patient characteristics. • This study provides objective physical function reference values among subsets of individuals across the spectrum of sex, age groups, radiographic knee osteoarthritis severity, and body mass index categories. • These reference values offer a more patient-centered approach for interpreting an individual’s relative level of objective physical function by comparing them to a more homogeneous group of individuals with similar participant characteristics. • We have provided a clinically accessible interactive table that will enable clinicians and researchers to input their patient’s data to quickly and efficiently determine a patient’s relative objective physical function compared to individual’s with similar characteristics. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the primary symptoms of knee osteoarthritis (KOA) is a decline in physical function leading to physical disability [1]. Performance-based measures of physical function quantify functional limitations by testing an individual’s performance on a variety of daily tasks (e.g., short/long walking, standing from a chair) [2, 3]. Additionally, declines in thigh muscle strength are an underlying physiological impairment that contributes to greater functional limitation [4, 5]. Both performance-based measures of physical function and muscle strength (collectively referred to as objective physical function tests) are considered clinically important outcome measures as worse performance is associated with poor quality of life, a decline in physical activity levels, and mortality in older adults and those with or at risk for KOA [5,6,7,8,9,10]. To better understand the natural history of objective physical function decline due to KOA, we first need to establish patient-specific reference values in a large cohort of individuals across multiple participant characteristics.
Objective physical function is thought to progressively decline as KOA severity increases [3], with a previous investigation highlighting that objective physical function is worse in individuals with greater radiographic evidence of tibiofemoral KOA compared to individuals with less severe disease [11]. However, other participant characteristics, in addition to KOA severity, are also involved in a decline in physical function. A recent population-based study found that symptomatic KOA was the strongest contributor to walking difficulty, but older age, female sex, and body mass index (BMI) were also significantly and independently associated with walking difficulty [12]. Adults present with fairly consistent performance on objective physical function tests until ~ 50 to 60 years of age after which they begin to experience a more accelerated decline in 20-m walk speed, chair stand performance, and 6-min walk distance [13, 14]. Obesity is another key risk factor of KOA development and progression [15], and obese individuals walk slower and perform worse during chair stand tests compared to individuals with normal BMI [16]. Additionally, females are at higher risk for KOA compared to males and perform worse than males on stair climbing, walking endurance, and quadriceps muscle strength tests in individuals with late-stage KOA [17]. Thus, objective physical function decline is a complex multi-dimensional construct dependent on multiple participant characteristics, including, KOA severity, age, sex, and BMI.
Since previous investigators have established that greater age, radiographic KOA severity, and BMI are all associated with worse objective physical function, reference values that consider the complex inter-play among these patient characteristics may help provide a personalized description of an individual’s physical function. Other investigators have provided sex-specific reference values for various objective physical function tests among healthy people in the general population across age groups [14, 18,19,20,21,22], but these analyses lack the sample size and age group granularity to provide more personalized results. Additionally, no studies have created reference values across the spectrum of BMI or radiographic KOA severity. Therefore, the purpose of this manuscript was to use a large community-based cohort of adults with or at risk for KOA to establish reference values of three performance-based measures of physical function and two thigh muscle strength tests across both sexes and a wide spectrum of age groups, radiographic KOA severity, and BMI categories. Creating patient-specific objective physical function reference values will enable researchers and clinicians to compare a patient to adults with similar participant characteristics and offer better interpretation of a patient’s relative level of objective physical function.
Materials and methods
Study design and participant selection
We identified community-based individuals from the Osteoarthritis Initiative (OAI) [23]. The OAI is a longitudinal observational study of KOA involving 4 clinical sites in the USA: Memorial Hospital of Rhode Island, Ohio State University, the University of Maryland/Johns Hopkins University, and the University of Pittsburgh. Overall, 4796 participants enrolled between February 2004 and May 2006. The OAI recruited 3 groups of individuals: (1) individuals with symptomatic KOA (n = 1396); (2) individuals at risk for symptomatic KOA (n = 3278); and (3) individuals with no KOA and no risk factors for KOA (n = 122) [24]. An individual was considered at risk for KOA based on age-stratified criteria that incorporated several common risk factors for KOA. Detailed descriptions of the specific eligibility criteria as well as the OAI protocol are available at the OAI website [23]. Institutional review boards (IRB) at each OAI clinical site and the coordinating center (University of California, San Francisco, USA) approved the OAI study. Since data from the OAI is deidentified and publicly available, our institution’s IRB determined that, per federal guidance, our study does not constitute human subjects research.
For this analysis, we included any participant with data for each objective physical function test, age, BMI (> 18.5 kg/m2), and radiographic KOA severity (Kellgren-Lawrence [KL] grade) at the OAI baseline visit (Fig. 1).
Knee radiographs
We defined radiographic tibiofemoral KOA severity using baseline bilateral weight-bearing, fixed-flexion posteroanterior knee radiographs [25]. Central OAI readers scored the KL grade of each knee (KL0–KL4), with KL4 indicating the worst radiographic KOA severity. Good intra-rater agreement was observed for KL grade (weighted κ = 0.70). These KL grades are publicly accessible (files: KXR_SQ_BU-_SAS [versions 0.6, 1.6, 3.5, 5.5, and 6.3]).
Most affected knee
For unilateral measures, we defined the most affected knee as follows: (1) the knee with the worst KL grade; (2) if KL grade was equal between knees, then the knee with the worst WOMAC pain score; 3) if WOMAC pain was equal between knees, then the right knee was selected.
Objective physical function tests
The inclusion of objective physical function tests in this analysis was limited to tests included in the OAI protocol. Full description of the protocols for each test can be found in the operations manual on the OAI website [23]. To ensure standardization across the different clinical sites, each examiner was required to (1) study the operations manuals and specific quality assurance checklists for each test, (2) attend an OAI training session on each test, (3) practice on other staff or volunteers, and (4) pass a test protocol observed by an OAI quality control officer. Study staff provided reasons for an individual’s non-completion for each test based on pre-specified criteria included on the data collection sheet. We reviewed these notes to determine if an individual was unable to complete a test due to limitations in their physical function. In order to include individuals with potentially the greatest functional limitations into our final analysis, we assigned a value to individuals with missing data due to physical function limitations (the value is defined for each test below).
20-m walk speed
Participants performed two trials of a timed 20-m walk at their usual, comfortable walking speed to assess their habitual walking speed [23, 26]. The participants began each 20-m walk trial in a standing position and timing began when the participant took their first step and ended when they passed a cone positioned 20-m away. The time needed to complete the 20-m was converted to walking speed (meters/second [m/s]) and averaged across two trials. If needed, participants used a walking aid (i.e., cane; n = 44). Testing habitual walking speed in individuals with KOA has high reliability (intraclass correlation coefficients [ICC] > 0.93) [27]. Slower 20-m walk speed indicates worse functional limitations. Individuals with missing 20-m walk speed data due to functional limitations were assigned a 0 m/s speed [28].
Chair stand speed
Participants performed two trials of a chair stand test in which they stood up from a seated position five times as quickly as possible to assess their chair stand speed [28]. Prior to completing the repeated chair stand test, the participants completed a single chair stand to confirm they were able to stand up from a standard straight-back chair without using their arms or walking aids. If able to complete the single chair stand, the participants then completed the repeated chair stand test. The time needed to complete five chair stands was converted to a chair stand speed (chair stands/min) and averaged across two trials [28]. Testing chair stand speed in individuals with KOA has high reliability (ICC = 0.96) [29]. Slower chair stand speed indicates worse functional limitations. Individuals unable to complete the single or repeated chair stand test due to functional limitations were assigned a 0 chair stands/min speed [28].
400-m walk time
Among those who could complete the 20-m walk test, participants performed one timed 400-m walk trial, while being instructed to “pace themselves without overexertion” as a measure of walking endurance [30]. The participants walked 20-m to a cone, walked around the cone, then back 20-m to a starting cone. Completion of 10 laps resulted in a 400-m walk. Participants could rest during the 400-m walk trial, but the total test time could not exceed 15 min [23]. The time needed to complete the 400 m was recorded for the single trial. The 400-m walk has high reliability in healthy, middle-aged women (ICC = 0.95) [31]. Longer 400-m walk time indicates worse functional limitations. Individuals with missing 400-m walk time data due to functional limitations were assigned a time of 15 min, as this is the cutoff in the literature that defines inability to complete [32].
Knee extension and flexion strength
Participants performed three maximal isometric contraction trials in each leg for knee flexion and extension on the “Good Strength Chair” (Metitur Oy, Jyvaskyla, Finland), as part of the OAI strength assessment protocol [33, 34]. Participants were positioned with their knee at 60° with straps secured over their waist and thigh to stabilize their pelvis and lower limb. A force transducer was attached to a lever arm and secured around their leg at a consistent anatomical position at 2 cm proximal to the calcaneus [35]. After two warmup trials at 50% of maximal effort, the participants completed three maximal effort trials in which the participants pulled (knee extension) and pushed (knee flexion) against the pad secured around their leg. A complete description of the procedure can be found on the OAI website [36]. Since KOA represents a heterogenous population, and our cohort presents with a wide range of body mass, we have normalized the trial with the maximum force (N) to body mass (kg) to account for the variability in body dimensions between participants [33, 37]. Lower normalized strength indicates worse functional impairment. Individuals with missing knee extension and flexion strength due to functional limitations were assigned 0 N/kg.
Including individuals with missing objective physical function data
During data collection for the OAI, the trained study personnel recorded why a participant had missing data. We reviewed these reasons for missing data to determine if a participant failed to complete a test due to physical function limitations. This process allowed us to assign a new value as specified in the prior sections for each test. Hence, we could include these individuals in our main analysis. The following reasons for missing data were attributed to physical function limitations a priori: 20-m walk speed (n = 1, < 1%): “cannot do/attempted” or “cannot do/not attempted”; chair stand speed (n = 180, < 5%): “attempted, unable to complete,” “did not attempt, unable to complete,” or “used arms to complete”; 400-m walk time (n = 41, 1%): “began, but did not complete all 400-meter,” “did not feel safe walking 400-meter,” “could not complete 20-meter walk,” or “walker or three-/four-pronged cane use”; knee strength (extension: n = 9, < 1%; flexion: n = 11, < 1%): “did not complete due to knee pain” or “did not complete due to fatigue.”
Participant characteristic categories used to create subsets for patient-specific reference values
Since the OAI includes males and females across a wide spectrum of age, radiographic KOA severity, and BMI, we used the following categories to create subsets defined by all combinations of the participant characteristic categories to create patient-specific reference values.
Sex was separated into two categories: male, female. Based on age group classification standards used by the World Health Organization [38], age was separated into categories defined by 5-year intervals: 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, and 75–79 years. Radiographic KOA severity was separated into each KL grade [39]: KL0, KL1, KL2, KL3, and KL4. BMI was separated into four categories defined by the World Health Organization [40]: normal: 18.5–24.9 kg/m2, overweight: 25–29.9 kg/m2, moderately obese: 30–34.9 kg/m2, and severely/morbidly obese: > 35 kg/m2.
Due to smaller sample sizes when creating reference values across three/four participant characteristics, we combined levels of our grouping variables such that males and females were separated into three levels for age group (i.e., 45–59, 60–69, and 70–79 years), KL grade (i.e., KL0/1, KL2, KL3/4), and BMI category (i.e., 18.5–24.9 kg/m2, 25–29.9 kg/m2, and > 30 kg/m2).
Other demographic information
Additional demographic measures were acquired based on a standard protocol to describe the cohort [41]. We extracted baseline WOMAC pain, Physical Activity Scale for the Elderly (PASE), Short Form-12 Mental and Physical Components, history of a previous knee injury, and Charlson Comorbidity Index (i.e., yes or no indicating any presence of comorbidity) at the OAI baseline visit.
Statistical analysis
Sex-specific reference values for objective physical function tests across age, radiographic KOA severity, and BMI
To establish objective physical function test reference values, we created tables with percentile scores from minimum to maximum in 10% increments for each combination of sex, age, radiographic KOA severity, and BMI category. The 50th percentile in these tables is equivalent to the median. These reference tables will allow clinicians and researchers to determine a patient’s relative level of objective physical function test (i.e., an individual’s percentile among a subset of similar individuals defined by a combination of multiple participant characteristics).
For brevity, the results focused on the two-way reference values between sex and the other characteristics for the 20-m walk speed and knee extension strength to highlight the need for these reference values across sex, age, radiographic KOA severity, and BMI. We selected these two tests because they are clinically relevant tests that reflect different constructs of physical function. We used established clinically important differences in individuals with or at risk for KOA for 20-m walk speed (i.e., 0.07 m/s [42]) and normalized knee extension strength (i.e., 5.2% [male] or 5.8% [female] strength per body mass [43]) to highlight within each reference value table (Supplementary File) if (1) the median of a subset with greater age, radiographic KOA severity, or BMI exceeded a clinically important difference compared to the median of the first subset (i.e., age 45–49 years, KL0, or normal BMI) separately for males and females and (2) the median of females exceeded a clinically important difference compared to the median of males at each patient characteristic category level. The previous walking speed study used a combination of distribution-based and anchor-based methods to establish that a walking speed change between 0.07 and 0.12 m per second is clinically important [42]. The threshold of 0.07 m/s for defining clinically important change in people with and at risk for KOA is similar to a substantial change in self-selected walking speed among sedentary adults aged 70 to 89 years [44]. In our Supplementary Files, we decided to highlight a difference of 0.07 m/s as potential clinically important differences in walking speed.
Results
Demographics
Table 1 describes the demographics and physical function performance of the 3860 included participants, as well as the available demographics for the OAI participants excluded from our analyses (n = 936).
Patient-specific reference values for objective physical function tests
The Supplemental File includes reference value tables across all combinations of sex, age, radiographic KOA severity, and BMI (Supplemental File: Tables 2–16). To use these reference value tables for determining a patient’s relative level of objective physical function, (1) select a reference value table based on your availability of patient characteristics, (2) within the table, find the objective physical function test of interest and the patient’s specific subset based on any combination of sex, age, KL grade, or BMI, and (3) find where the patient’s objective physical function is located within the percentiles from minimum to maximum in 10% intervals. An individual’s percentile will provide an easy, intuitive interpretation of an individual’s relative level of objective physical function compared to individuals with similar characteristics.
Interactive reference value table to determine an individual’s relative objective physical function across all patient characteristics
To facilitate the clinical accessibility of the reference value tables, we created an interactive table (Supplemental File: Table 1) that synthesizes the reference values from each reference value table across all two-, three-, and four-way combination of sex, age, radiographic KOA severity, and BMI (Supplemental File: Tables 2–16). This interactive table will allow a clinician or researcher to enter in a patient’s characteristics and objective physical function performance to determine an individual’s relative objective physical function (i.e., percentile) when compared to individuals with any combination of similar sex, age, radiographic KOA severity, or BMI.
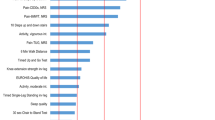
Sex-specific differences across age
Supplementary File: Table 2 provides the reference values across sex and age, as well as highlighting the clinically meaningful differences in medians for 20-m walk speed (i.e., 0.07 m/s [42]) and knee extension strength (i.e., 5.2% [males] or 5.8% [females] strength per body mass [43]) between sexes and across the age groups. While the two male subsets > 70 years of age walked slower than the youngest males, the three oldest female subsets > 65 years of age walked slower than the youngest female subset. Females 50–54, 65–69, and 75–79 years old walked slower than their male counterparts of similar age.
For knee extension strength, every male age group (> 50 years) is weaker than the youngest male subset. However, for females, the age groups greater than 55 years of age had weaker knee extension strength compared to the youngest female subset. Even with strength normalized to body mass, the females at every age group are weaker in knee extension strength compared to males of similar age.
Sex-specific differences across radiographic KOA severity
Supplementary File: Table 3 provides the reference values across sex and radiographic KOA severity, as well as highlighting the clinically meaningful differences in medians for 20-m walk speed and knee extension strength between sexes and across KL grades. There are no clinically meaningful differences in 20-m walk speed across the subsets of males with increasing radiographic severity of KOA when compared to males with no radiographic evidence of KOA. However, female subsets with KL3 and KL4 walked slower compared to females with KL0. Similarly, females with KL3 and KL4 walked clinically meaningfully slower compared to males with similar radiographic KOA severity.
For knee extension strength, both male and female subsets with radiographic KOA severity of KL2 or greater are weaker than their respective subset with no radiographic evidence of KOA. The females at every KL grade present with weaker knee extension strength compared to males with similar radiographic KOA severity.
Sex-specific differences across BMI
Supplementary File: Table 4 provides the reference values across sex and BMI, as well as highlighting the clinically meaningful differences in medians for 20-m walk speed and knee extension strength between sexes and across BMI categories. Severely/morbidly obese males (BMI > 35 kg/m2) walk slower than males with a normal BMI. For females, individuals who are considered at least moderately obese (BMI > 30 kg/m2) walk slower than females with a normal BMI. The median 20-m walk speed for females with BMI greater than 35 is clinically meaningfully slower than males within the similar BMI category.
For knee extension strength, every BMI category from overweight to obese presents with weaker knee extension strength compared to the normal BMI category for both males and females. The females at every BMI category present with weaker knee extension strength compared to males within the same BMI category.
Discussion
This novel study provides objective physical function reference values among subsets of individuals across the spectrum of sex, age, radiographic KOA severity, and BMI. Since individuals with or at risk for KOA represent a highly heterogeneous cohort, these reference values offer a patient-centered approach for interpreting a person’s relative level of objective physical function by comparing them to a group of individuals with similar participant characteristics. Additionally, we have provided a clinically accessible interactive table that will enable clinicians and researchers to input their patient’s data on one screen to determine a patient’s relative level of objective physical function. Therefore, these patient-specific reference values embedded within a clinically accessible interactive table help determine a patient’s relative level of objective physical function, which may help develop more personalized guidance regarding the maintenance of objective physical function in individuals with or at risk for KOA.
Previous studies have provided reference values for various objective physical function tests across age group [14, 18,19,20,21,22]. However, the results of this study using a large cohort of community-based individuals with or at risk for KOA help to provide a more granular patient-centered approach to monitoring objective physical function. For instance, we used age group increments of 5 years instead of 10 [14, 21] or 40 [19] years used in previous studies. Our results indicate that females older than 65 years and males older than 70 years present with slower walking speed than a sex-specific group between 45 and 49 years of age. Even when normalizing knee extension strength to body mass, the female participants are weaker than males across every 5-year age range. These reference values with 5-year age ranges offer a more granular perspective to compare patients to a more similar group of individuals, which will allow for a more accurate reflection of that patient’s relative functional limitations when compared to reference values based on a broader age range.
Previous studies [11, 15] have demonstrated that higher BMI and KL grade are associated with worse objective physical function. However, no previous studies have created objective physical function reference values across radiographic KOA severity and BMI categories. Among females, 20-m walk speed is slower in women with greater radiographic KOA severity. Specifically, females with KL grades 3 and 4 present with clinically important differences compared to females with KL0. Conversely, there were no clinically important differences in 20-m walk speed among males across radiographic KOA severity. These highlight the need for sex-specific analyses since walking speed in females may be more adversely affected by radiographic KOA severity compared to males. When comparing 20-m walk speed across BMI categories, females with an obese BMI walk slower than males in a similar BMI category. For knee extension strength, females are weaker than males at every stage of radiographic KOA severity, as well as all BMI categories. Since we know that worse radiographic KOA severity and greater BMI contribute to worse objective physical function, our reference value tables that couple BMI and KL grade to age and sex may provide a more holistic reflection of an individual’s relative physical function by comparing a patient to individuals with multiple similar characteristics.
There may be logistical issues using the 15 different tables of patient-specific reference values based on the various combinations of sex, age, KL grade, and BMI (Supplemental File 1: Tables 2–16). Therefore, we created the interactive table (Supplemental File 1: Table 1) as an initial attempt to create a clinically accessible alternative for clinicians/researchers to input a patient’s data to obtain their relative objective physical function across all combinations of sex, age, KL grade, and BMI. We foresee this tool being used to improve participant selection in clinical trials by specifically selecting people based on a patient-specific cutoff of relative objective physical function. Additionally, this could be used within the clinic to help clinicians interpret and monitor a patient’s relative level of physical function by comparing them to other individuals with similar characteristics. Future studies are needed to determine the optimal range of relative objective physical function that should be used for inclusion within clinical trials to optimize the treatment response, as well as if this interactive table can help clinicians interpret the results of objective physical function tests to better improve physical function in their patients.
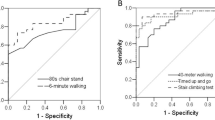
Oftentimes studies create thresholds for physical function tests using a heterogeneous cohort with a large spectrum of patient characteristics. However, a threshold created from a heterogeneous group will likely represent varying degrees of physical function limitations depending on a patient’s characteristics. Figure 2 illustrates how a common walking speed threshold of 1.22 m/s reflects different relative levels of objective physical function (determined by our reference value tables) that considers each combination of sex with age, radiographic KOA severity, and BMI [30, 45]. For example, a female with a walking speed of 1.22 m/s represents the 34th percentile when compared to all females within our cohort, indicating they walk faster than 34% of the females in the cohort. However, when a female walking at 1.22 m/s is compared to females within her 5-year age range, a 59-year-old female represents the 26th percentile, but a 75-year-old female would represent the 60th percentile of her age-specific cohort with that walking speed. Rather than relying on a single threshold for all adults with or at risk for KOA, our reference values highlight that future analyses may consider creating patient-specific physical function thresholds within clinically relevant subsets.
Sex-specific percentile of an individual walking at 1.22 m/s* varies based on KL grade, age, and BMI. *1.22 m/s is often used as a threshold for a “functional” walking speed, as this is the minimum speed needed to cross a timed crosswalk. This figure uses the patient-specific reference values to determine an individual’s percentile if walking at 1.22 m/s within each of the subsets separated by sex across each category of KL grade, age, and body mass index (BMI). For example, a female walking at 1.22 m/s represents the 34th percentile when compared to all females within our cohort, indicating they walk faster than 34% of the other females in the cohort. However, when compared to females within a similar age range, a 59-year-old female walking at 1.22 m/s represents the 26th percentile, but a 75-year-old female walking at the same speed represents the 60th percentile her age-specific cohort. Therefore, patient-specific physical function thresholds that are based on an individual’s demographics may help to provide a more accurate definition of an individual’s relative level of physical function
While this manuscript provides important insight into objective physical function reference values, there are some limitations that must be discussed. One limitation of the study is that some individuals in the OAI were excluded due to missing data. However, one of the strengths of our study is that we completed a thorough evaluation of the explanations for missing data that are included within the OAI database. This allowed us to reclaim and recode some of this subset to include individuals with potentially the most severe physical function limitations. However, we were unable to include missing data that was randomly occurring (e.g., equipment failure) or if the reason for missing data was not provided. While the sample size within this study is large, the OAI eligibility criterion was limited to individuals with or at risk for symptomatic KOA and may not be representative of the entire US population. Therefore, we have provided the complete age-specific eligibility criteria of the OAI within Supplemental File: Table 17 to help ensure these reference values are applied to the intended individuals [23]. Similar to KOA clinical trials, we selected an index knee for this study based on KL grade and pain. However, walking speed and chair stand tests are person-level outcomes that are likely influenced by both knees and disease in other joints. Therefore, future studies are needed to better understand how bilateral KOA status contributes to a decline in objective physical function.
In conclusion, this investigation provides an unprecedented insight into reference values of objective physical function tests within homogeneous subsets across both sexes and a wide spectrum of age, radiographic KOA severity, and BMI categories. The interactive table may provide a clinically accessible means for clinicians and researchers to incorporate these patient-specific reference values into practice.
References
Kauppila AM, Kyllonen E, Mikkonen P, Ohtonen P, Laine V, Siira P et al (2009) Disability in end-stage knee osteoarthritis. Disabil Rehabil 31(5):370–380
Edwards MH, van der Pas S, Denkinger MD, Parsons C, Jameson KA, Schaap L et al (2014) Relationships between physical performance and knee and hip osteoarthritis: findings from the European Project on Osteoarthritis (EPOSA). Age Ageing 43(6):806–813
Oiestad BE, White DK, Booton R, Niu J, Zhang Y, Torner J et al (2016) Longitudinal course of physical function in people with symptomatic knee osteoarthritis: data from the Multicenter Osteoarthritis Study and the Osteoarthritis Initiative. Arthritis Care Res 68(3):325–331
Liikavainio T, Lyytinen T, Tyrvainen E, Sipila S, Arokoski JP (2008) Physical function and properties of quadriceps femoris muscle in men with knee osteoarthritis. Arch Phys Med Rehabil 89(11):2185–2194
Hairi NN, Cumming RG, Naganathan V, Handelsman DJ, Le Couteur DG, Creasey H et al (2010) Loss of muscle strength, mass (sarcopenia), and quality (specific force) and its relationship with functional limitation and physical disability: the Concord Health and Ageing in Men Project. J Am Geriatr Soc 58(11):2055–2062
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49(2):M85–M94
Dunlop DD, Song J, Semanik PA, Sharma L, Chang RW (2011) Physical activity levels and functional performance in the osteoarthritis initiative: a graded relationship. Arthritis Rheum 63(1):127–136
Ruhdorfer A, Wirth W, Eckstein F (2016) Longitudinal change in thigh muscle strength prior to and concurrent with minimum clinically important worsening or improvement in knee function: data from the osteoarthritis initiative. Arthritis Rheum 68(4):826–836
Newman AB, Simonsick EM, Naydeck BL, Boudreau RM, Kritchevsky SB, Nevitt MC et al (2006) Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. 295(17):2018–2026
Master H, Neogi T, Lavalley M, Thoma LM, Christansen M, Voiner D, et al. (2019) Optimal threshold of walking speed predictive of mortality risk over 9 years in knee osteoarthritis: data from Osteoarthritis Initiative. American College of Rheumatology Annual Meeting. Atlanta, GA: Arthritis and Rheumatology 71(S10):4978–9
van Leeuwen DM, van de Bunt F, de Ruiter CJ, van Schoor NM, Deeg DJH, Emanuel KS (2017) Functioning without cartilage: older people with radiographic knee osteoarthritis who self-report no functional limitations do score lower on a performance battery. J Aging Phys Act 1–19
King LK, Kendzerska T, Waugh EJ, Hawker GA (2018) Impact of osteoarthritis on difficulty walking: a population-based study. Arthritis Care Res 70(1):71–79
Himann JE, Cunningham DA, Rechnitzer PA, Paterson DH (1988) Age-related changes in speed of walking. Med Sci Sports Exerc 20(2):161–166
Tveter AT, Dagfinrud H, Moseng T, Holm I (2014) Health-related physical fitness measures: reference values and reference equations for use in clinical practice. Arch Phys Med Rehabil 95(7):1366–1373
Zheng H, Chen C (2015) Body mass index and risk of knee osteoarthritis: systematic review and meta-analysis of prospective studies. BMJ Open 5(12):e007568
Batsis JA, Zbehlik AJ, Barre LK, Bynum JP, Pidgeon D, Bartels SJ (2015) Impact of obesity on disability, function, and physical activity: data from the Osteoarthritis Initiative. Scand J Rheumatol 44(6):495–502
Petterson SC, Raisis L, Bodenstab A, Snyder-Mackler L (2007) Disease-specific gender differences among total knee arthroplasty candidates. J Bone Joint Surg Am 89(11):2327–2333
Landi F, Calvani R, Tosato M, Martone AM, Fusco D, Sisto A et al (2017) Age-related variations of muscle mass, strength, and physical performance in community-dwellers: results from the Milan EXPO Survey. J Am Med Dir Assoc 18(1):88 e17–88 e24
McKay MJ, Baldwin JN, Ferreira P, Simic M, Vanicek N, Burns J et al (2017) Reference values for developing responsive functional outcome measures across the lifespan. Neurology. 88(16):1512–1519
Salbach NM, O'Brien KK, Brooks D, Irvin E, Martino R, Takhar P, Chan S, Howe JA (2015) Reference values for standardized tests of walking speed and distance: a systematic review. Gait Posture 41(2):341–360
Bohannon RW, Williams AA (2011) Normal walking speed: a descriptive meta-analysis. Physiotherapy. 97(3):182–189
Cooper R, Hardy R, Aihie Sayer A, Ben-Shlomo Y, Birnie K, Cooper C, Craig L, Deary IJ, Demakakos P, Gallacher J, McNeill G, Martin RM, Starr JM, Steptoe A, Kuh D, HALCyon study team (2011) Age and gender differences in physical capability levels from mid-life onwards: the harmonisation and meta-analysis of data from eight UK cohort studies. PLoS One 6(11):e27899
The Osteoarthritis Initiative. Available at: https://oai.nih.gov. Accessed 7 Jul 2018
Osteoarthritis Initiative Website. The Osteoarthritis Initiative: protocol for the cohort study. 2006. Available at: https://oai.epi-ucsf.org/datarelease/docs/StudyDesignProtocol.pdf
Driban JB, Stout AC, Lo GH, Eaton CB, Price LL, Lu B et al (2016) Best performing definition of accelerated knee osteoarthritis: data from the Osteoarthritis Initiative. Ther Adv Musculoskelet Dis 8(5):165–171
White DK, Niu J, Zhang Y (2013) Is symptomatic knee osteoarthritis a risk factor for a trajectory of fast decline in gait speed? Results from a longitudinal cohort study. Arthritis Care Res 65(2):187–194
Fransen M, Crosbie J, Edmonds J (1997) Reliability of gait measurements in people with osteoarthritis of the knee. Phys Ther 77(9):944–953
Sharma L, Cahue S, Song J, Hayes K, Pai YC, Dunlop D (2003) Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum 48(12):3359–3370
Lin YC, Davey RC, Cochrane T (2001) Tests for physical function of the elderly with knee and hip osteoarthritis. Scand J Med Sci Sports 11(5):280–286
Master H, Thoma LM, Christiansen MB, Polakowski E, Schmitt LA, White DK (2018) Minimum performance on clinical tests of physical function to predict walking 6,000 steps/day in knee osteoarthritis: an observational study. Arthritis Care Res 70(7):1005–1011
Pettee Gabriel KK, Rankin RL, Lee C, Charlton ME, Swan PD, Ainsworth BE (2010) Test-retest reliability and validity of the 400-meter walk test in healthy, middle-aged women. J Phys Act Health 7(5):649–657
Investigators LS, Pahor M, Blair SN, Espeland M, Fielding R, Gill TM et al (2006) Effects of a physical activity intervention on measures of physical performance: results of the lifestyle interventions and independence for Elders Pilot (LIFE-P) study. J Gerontol A Biol Sci Med Sci 61(11):1157–1165
Eckstein F, Hitzl W, Duryea J, Kent Kwoh C, Wirth W, Investigators OAI (2013) Baseline and longitudinal change in isometric muscle strength prior to radiographic progression in osteoarthritic and pre-osteoarthritic knees—data from the Osteoarthritis Initiative. Osteoarthr Cartil 21(5):682–690
Berger MJ, Kean CO, Goela A, Doherty TJ (2012) Disease severity and knee extensor force in knee osteoarthritis: data from the Osteoarthritis Initiative. Arthritis Care Res 64(5):729–734
Ruhdorfer A, Wirth W, Eckstein F (2017) Association of knee pain with a reduction in thigh muscle strength—a cross-sectional analysis including 4553 osteoarthritis initiative participants. Osteoarthr Cartil 25(5):658–666
Osteoarthritis Initiative Website. Isometric Strength OAI Operations Manual 2008. Available at: http://oai.epi-ucsf.org/datarelease/operationsManuals/isometric_strengthv1_2p.pdf
Hall M, Hinman RS, Wrigley TV, Kasza J, Lim BW, Bennell KL (2018) Knee extensor strength gains mediate symptom improvement in knee osteoarthritis: secondary analysis of a randomised controlled trial. Osteoarthr Cartil 26(4):495–500
Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M (2001) Age standardization of rates: a new WHO standard. Available at: https://www.who.int/healthinfo/paper31.pdf
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Changulani M, Kalairajah Y, Peel T, Field RE (2008) The relationship between obesity and the age at which hip and knee replacement is undertaken. J Bone Joint Surg (Br) 90(3):360–363
Osteoarthritis Initiative Website. Overview of enrollment visit. 2006. Available at: https://oai.epi-ucsf.org/datarelease/operationsManuals/Overview_of_Enrollment_Visit1_0p.pdf
Song J, Cella D, Gilbert A, Chang RW, Dunlop D (2019) What is an important difference in gait speed in adults with knee osteoarthritis? American College of Rheumatology Annual Meeting. Atlanta, GA: Arthritis & Rheumatology 71(S10):3850–1
Ruhdorfer A, Wirth W, Eckstein F (2015) Relationship between isometric thigh muscle strength and minimum clinically important differences in knee function in osteoarthritis: data from the osteoarthritis initiative. Arthritis Care Res 67(4):509–518
Kwon S, Perera S, Pahor M, Katula JA, King AC, Groessl EJ et al (2009) What is a meaningful change in physical performance? Findings from a clinical trial in older adults (the LIFE-P study). J Nutr Health Aging 13(6):538–544
Langlois JA, Keyl PM, Guralnik JM, Foley DJ, Marottoli RA, Wallace RB (1997) Characteristics of older pedestrians who have difficulty crossing the street. Am J Public Health 87(3):393–397
Funding
MSH was supported by the National Institutes of Health (grant no. 5 TL1 TR 1454-3). These data were financially supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health (grant no. R01 AR065977). The OAI is a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners. This research was based upon work supported by the U.S. Department of Agriculture, under agreement no. 58-1950-4-003. Any opinions, findings, conclusion, or recommendations expressed in this publication are those of the author(s) and do not necessarily reflect the view of the U.S. Department of Agriculture.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(XLSX 906 kb)
Rights and permissions
About this article
Cite this article
Harkey, M.S., Price, L.L., Reid, K.F. et al. Patient-specific reference values for objective physical function tests: data from the Osteoarthritis Initiative. Clin Rheumatol 39, 1961–1970 (2020). https://doi.org/10.1007/s10067-020-04972-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-04972-1