Abstract
Background/objective
Recent studies observed an association between increased serum uric acid (SUA) levels and renal damage in lupus. However, the predictive value of UA for the development of long-term renal dysfunction in lupus nephritis (LN) is still unknown. The aim of this study was to evaluate if SUA may be a predictor of long-term renal outcome in LN.
Methods
Eighty biopsy-proven LN patients > 7 years of follow-up were selected. SUA levels were measured in sera stored at − 70 °C. All patients had serum stored from LN baseline, and 32 also had stored serum from 6 and 12 months after LN. Renal outcome was addressed after 7 years of follow-up to determine if SUA could be a predictor of long-term renal outcome. A good long-term renal outcome in 7 years was defined as a creatinine clearance (CrCl) ≥ 90.0 mL/min/1.73 m2, and poor if CrCl < 90 mL/min/1.73 m2. Patients were divided in two groups according to the renal outcome to assess whether SUA levels at different time points of follow-up could differentiate such groups. An ROC curve was plotted to assess accuracy.
Results
SUA levels at baseline and 6 months were not able to differentiate good from poor long-term renal outcomes in LN (respectively p = 0.37, p = 0.28), but at 12 months (p = 0.02), they could clearly differentiate the two groups. ROC curve (12 months) accuracy was 0.76. SUA cutoff was 6.05 mg/dL (sensitivity = 0.67, specificity = 0.89, positive predictive value = 0.85, negative predictive value = 0.73).
Conclusion
SUA levels < 6.05 mg/dL at 12 months of follow-up is a predictor of good long-term renal outcome in lupus nephritis.
Key Points
• Previous studies reported an association between increased serum uric acid level and short-term renal damage in lupus patients.
• The predictive value of serum uric acid for the development of long-term renal dysfunction in lupus nephritis was never assessed.
• At 12 months of follow-up serum uric acid clearly differentiated good from poor long-term renal outcome in lupus nephritis.
• SUA level < 6.05 mg/dL at 12 months of follow-up was a predictor of good long-term renal outcome in lupus nephritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hyperuricemia has been reported to be associated with chronic kidney disease (CKD) in several clinical conditions, and recent studies also observed an association between increased serum uric acid (SUA) levels and renal damage in lupus [1, 2]. Previous cross-sectional studies detected that higher levels of SUA in systemic lupus erythematosus (SLE) patients were closely related to renal involvement [3,4,5]. In fact, Liu et al. showed a higher prevalence of increased uric acid (UA) in lupus nephritis (LN) patients with CKD (stages 1–3) mostly due to renal under-excretion [3].
Lupus nephritis is a critical condition that affects up to 60% of SLE patients, and despite recent treatment improvements, 30% of patients still experience some degree of renal impairment in the long-term follow-up [2, 6]. Good predictors of long-term outcome are therefore needed to better assess the severity and provide an accurate treatment guidance [6]. In fact, the effectiveness of treat-to-target strategies in rheumatoid arthritis [7] and SLE [8] have driven the search for these prognostic parameters for other rheumatic diseases.
Until now, 24 h proteinuria (24 h PTU) has been considered the best single predictor of long-term (7 years) renal outcome in lupus patients [9, 10]. Recently, our group extended this observation demonstrating that 24 h PTU is also valid for an ethnically diverse group of SLE patients and for those with more severe LN [11]. Importantly, these studies also showed that the addition of other variables commonly used in LN response criteria, such as creatinine and hematuria, did not improve the predictive value of 24 h PTU [9,10,11].
Regarding SUA, one previous study in SLE patients reported an association between increased SUA levels and short-term renal damage [1], but there are no data concerning the predictive value of SUA for the development of long-term renal dysfunction in LN. Therefore, the aim of the present study was to evaluate if SUA levels could be considered a predictor of long-term renal outcome in patients with lupus nephritis.
Methods
Patient selection and study design
A total of 108 biopsy-proven LN patients with at least 7 years of available longitudinal follow-up data at the Rheumatology Division of our tertiary University Hospital were consecutively selected for this study. All enrolled patients had biopsy-proven LN and met ACR criteria for the diagnosis of SLE [12]. Data were obtained in a 3-month interval using a standardized electronic database protocol established in 2000 that included data on demographics, clinical and laboratory findings, and treatments. Serum UA at biopsy and follow-up was measured using a − 70 °C stored biorepository sera that was previously validated.
Twenty-seven patients were excluded: seven due to missing relevant data, six due to the development of early end-stage renal disease (ESRD) that required dialysis in the first year after the nephritis onset, and 14 due to lack of stored sera during nephritis flare. Patients who were diagnosed with ESRD at any time after the first year of follow-up were included. Eighty patients with biopsy-proven LN were enrolled for this study.
All persons gave their informed consent prior to their inclusion in the study. No patient data was included in this manuscript. The study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments and was approved by the Local Ethics committee.
Validation of stored serum UA
The serum UA analysis was performed using a biorepository serum stored at − 70 °C. Since samples were stored for several years, we performed a laboratorial validation analysis with five frozen samples that had SUA assessed at the same time of biorepository blood collection. A high correlation was observed between SUA results obtained at the time of blood collection and in − 70 °C stored sera (r = 0.99 p < 0.05), with a variation coefficient of 12% which allowed us to use these frozen samples in the present evaluation.
Definition of long-term renal outcome
A good long-term renal outcome was defined as a creatinine clearance (CrCl) ≥ 90 mL/min/1.73 m2, and conversely, a poor long-term renal outcome was defined as a CrCl < 90 mL/min/1.73 m2 in 7 years. Creatinine clearance was estimated using the Modification of Diet in Renal Disease (MDRD) index that defines normal renal function as a MDRD CrCl ≥ 90.0 mL/min/1.73 m2 and defines mild decrease of renal function as a MDRD CrCl between 60 and 89 mL/min/1.73 m2 [2, 13].
Statistical analysis
SUA and creatinine clearance were evaluated at baseline, after 6 months, 12 months, and at 7 years of follow-up. Anti-dsDNA antibodies, serum albumin and Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) score were assessed only at baseline. Renal flares were defined as significant increase in PTU levels (PTU > 500 mg/24 h if previously negative or PTU > 3 g if previously > 500 mg/24 h). Absolute values were used for PTU, CrCl, and albumin. Anti-dsDNA was considered only as present or absent. The ability of SUA at these different time points to predict a good long-term renal outcome (defined as CrCl ≥ 90 mL/min/1.73 m2) at 7 years was assessed. The same analysis was also performed with CrCl ≥ 60 mL/min/1.73 m2 cutoff. A multivariate analysis (multiple logistic regression) was also performed to understand the independence of variables (only variables with p < 0.05 were imported into the model).
The patients were divided in two groups according to the renal outcome: good outcome (CrCl ≥ 90.0 mL/min/1.73 m2 in 7 years) and poor outcome (CrCl < 90 mL/min/1.73 m2 in 7 years) to assess whether SUA levels at different time points of follow-up were able to differentiate such groups. Mann–Whitney, Student’s t test, and Fisher test were used for the comparisons. Correlations between SUA and CrCl at different set time points were calculated with Spearman test.
A receiver operating characteristic (ROC) curve of SUA was plotted to assess its accuracy (AUC), sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and confidence interval 95% (CI) in predicting long-term outcome. The SUA cutoff was defined using the Youden index.
All analyses were performed using SigmaStat software. Statistical significance was set as p < 0.05.
Results
Demographic, clinical, and histological features
Of the total LN patients (n = 80), 71 patients (88.75%) were women and 35 patients (43.75%) were non-Caucasian. The mean age was 29.85 ± 9.37 years old. At baseline, LN patients had a mean SCr of 1.75 ± 1.3 mg/dL, MDRD CrCl of 68.16 ± 43.4 mL/min/1.73 m2, PTU of 5.7 ± 4.7 g/24 h, albumin concentration of 2.4 ± 0.8 g/dL, and a mean SLEDAI of 9.5 ± 4.2. Almost two thirds had positive anti-dsDNA (n = 53, 66.25%), 58 SLE patients (72.50%) had CrCl < 90 mL/min/1.73 m2, and 38 SLE patients (47.50%) had CrCl < 60 mL/min/1.73 m2, inferring a severe subset of patients. The distribution of histological classes among studied patients was as follows: class II (6.25%), class III–IV (56.25%), and pure class V (36.25%) (Table 1).
At the end of the 7 years follow-up, a total of 33 patients (41.25%) had a good long-term outcome of a CrCl ≥ 90 mL/min/1.73 m2, 31 patients (38.75%) had a CrCl < 60 mL/min/1.73 m2, 18 patients (22.5%) were on dialysis, and 7 patients (8.75%) died (primarily due to infections).
Baseline data and long-term renal outcome
To investigate if long-term renal outcome could be predicted by baseline data, LN patients were divided into two groups (CrCl at 7 years ≥ 90.0 mL/min/1.73 m2 and < 90 mL/min/1.73 m2). Most of the baseline data were comparable between groups: serum UA (7.25 ± 4.75 vs. 6.43 ± 2.92 mg/dL; p = 0.35), 24-h PTU (6.70 ± 5.7 vs. 5.06 ± 3.85; p = 0.13), serum albumin (2.23 ± 0.80 vs. 2.52 ± 0.92 g/dL; p = 0.13), complement C3 (78.44 ± 35.3 vs. 65.5 ± 26.2 mg/dL; p = 0.08), positive anti-dsDNA (66% vs. 66%; p = 0.94), and SLEDAI scores (9.06 ± 3.91 vs. 9.85 ± 5.39; p = 0.43). Only serum creatinine (1.29 ± 0.81 vs. 2.06 ± 1.60 mg/dL; p = 0.013) and ClCr (83.44 ± 47.26 vs. 57.42 ± 37.36 mg/min; p = 0.007) were statistically different at baseline among groups (Table 2).
Assessing renal flares
The analysis of renal flares revealed that both groups (CrCl at 7 years ≥ 90.0 and < 90 mL/min/1.73 m2) exhibited a similar number of flares during follow-up (1.60 ± 0.92 vs. 1.47 ± 0.61, p = 0.45).
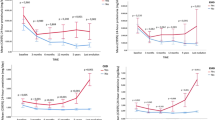
Performance of SUA levels at baseline, 6 months, and 12 months
SUA levels within the first year of follow-up were assessed in both groups (CrCl at 7 years ≥ 90.0 and < 90 mL/min/1.73 m2). Figure 1 shows that SUA levels were not able to differentiate long-term renal outcomes at baseline (7.25 ± 4.75 vs. 6.43 ± 2.92 mg/dL; p = 0.37), nor at 6 months (4.97 ± 2.12 vs. 5.86 ± 2.35 mg/dL; p = 0.28). However, at 12 months, SUA was able to differentiate good from poor long-term renal outcomes (4.66 ± 2.12 vs. 6.51 ± 2.45 mg/dL; p = 0.02).
The same analysis was performed using a less stringent CrCl cutoff at 7 years of ≥ 60.0 and < 60 mL/min/1.73 m2. Using this less stringent cutoff, SUA levels were not able to differentiate good from poor long-term renal outcomes at baseline (6.68 ± 4.22 vs. 6.88 ± 3.04 mg/dL; p = 0.82), nor at 6 months (5.21 ± 1.98 vs. 5.91 ± 2.72 mg/dL; p = 0.42). However, at 12 months, SUA was able to differentiate good from poor long-term renal outcomes (5.01 ± 2.19 vs. 6.83 ± 2.61 mg/dL; p = 0.03).
The multivariate analysis could not demonstrate independency of any variable pointed in the univariate analysis. Due to the sample size, the power of this analysis is low.
ROC curve at 12 months
The ROC curve with the higher AUC (the 12 months curve) demonstrated a good accuracy (AUC = 0.76, p < 0.05) in predicting long-term renal outcome, Fig. 2. The cutoff for SUA was 6.05 mg/dL, with a sensitivity of 0.67 (CI 95% = 0.44–0.84, p < 0.05), specificity of 0.89 (CI 95% = 0.68–0.97, p < 0.05), positive predictive value of 0.85, and negative predictive value of 0.73. The cutoff that maximized the sensitivity and specificity was 6.05 mg/dL.
Receiver operating characteristic curve of uric acid at 12 months of follow-up. ROC receiver operating characteristic curve. Area under the curve (AUC) = 0.76, sensitivity = 0.67 (confidence interval 95% = 0.44–0.84, p < 0.05), specificity = 0.89 (confidence interval 95% = 0.68–0.97, p < 0.05), positive predictive value (PPV) = 0.85, and negative predictive value (NPV) = 0.73
Correlations between SUA and current CrCl
The SUA is inversely correlated with the current CrCl at 12 months of follow-up (r = − 0.46, p = 0.004). However, the same analysis did not show correlation between SUA and CrCl at baseline (r = − 0.19, p = 0.23) and 6 months of follow-up (r = − 0.19, p = 0.90).
Using the SUA cutoff of 6.05 mg/dL
Dividing the patients into two groups using the SUA cutoff of 6.05 mg/dL at 12 months, it was possible to differentiate in a long term (7 years of follow-up): the creatinine levels (1.24 ± 2.20 vs. 4.48 ± 3.88 mg/dL, p = 0.007), the CrCl (117.10 ± 55.95 vs. 41.63 ± 41.65 mL/min/1.73 m2, p = 0.00004), the creatinine increase (delta − 0.08 ± 2.41 vs. 2.94 ± 4.20, p = 0.02), and SLICC damage index (1.28 ± 1.27 vs. 2.46 ± 1.45, p = 0.02) at the end of follow-up.
As SUA was moderately correlated with the CrCl at 12 months of follow-up, we performed a separated analysis excluding patients with moderate/severe CrCl reduction (MDRD CrCl < 60 mL/min/1.73 m2) to understand if this elevated SUA was not only predicting patients who were already in CKD at 12 months. In this separated analysis, SUA at 12 months remained a good predictor of long-term CrCl (120.16 ± 55.2 vs. 75.65 ± 34.60 mL/min/1.73 m2, p = 0.02) in the subgroup of patients with normal/mild decrease in MDRD.
Discussion
This is the first study to demonstrate that serum uric acid at 12 months of follow-up can predict long-term renal outcome in lupus nephritis.
In the present study, biopsy-proven LN was an inclusion criterion allowing a more accurate definition of renal involvement related to disease and not to other conditions [14], which were not considered in previous reports [1,2,3]. In addition, a long-term follow-up is required to define predictors of CKD [9, 15] since short-term assessment is not reliable to define renal survival, as demonstrated in the original National Institute of Health trial [16].
The balanced representation of severe and non-severe nephritis histological classes was important to assure a more precise calculation of predictive values. In fact, previous reports have demonstrated that proliferative classes had worse outcome [9, 15, 17]. Of note, the possible influence of nephritis flares during follow-up on renal outcome [18] was minimized herein by the fact that patients with poor and good outcomes exhibited comparable number of nephritic flares.
The results of our study indicate that uric acid is stable after years of storage at − 70 °C, with a high correlation between SUA results obtained at the time of blood collection and in stored sera (r = 0.99; p < 0.05). Validation was essential since some previous studies [19, 20] demonstrated that serum uric acid concentrations were unstable after 48 h of storage at − 4 °C, whereas others observed a minor decrease in uric acid concentration over time which was neither statistically nor clinically significant [21].
We confirmed previous report that baseline estimate of glomerular filtration rate is an important parameter associated with long-term renal survival in lupus [22, 23]. However, in the present study, baseline SUA and 6 months SUA was not associated with long-term renal outcome nor current MDRD CrCl, despite the known association of SUA levels and renal function [24, 25]. This discrepancy may be explained by the fact that several SUA interferences may be present during the induction treatment such as hypertension, weight gain, and some drugs such as diuretics, antiproteinuric, and immunosuppressive drugs.
The novel demonstration that SUA levels at 12 months is a long-term predictor of renal outcome in SLE is in line with the reported association between increased SUA levels and progression of chronic kidney disease in non-CKD individuals [26,27,28]. In fact, a recent study in SLE has also detected an association between increased baseline SUA levels and higher scores of renal damage in a short-term follow-up (3 years) [1].
Experimental data have demonstrated that increased uric acid levels can both be a marker and cause/accelerate renal disease [29]. Whether elevated SUA is only a marker of subclinical chronic kidney disease or also a risk factor for renal dysfunction requires further studies. Notwithstanding that, persistence of hyperuricemia seems to be more relevant in the long run than in the initial presentation, suggesting that irreversible subclinical renal damage may underlie hyperuricemia at 1-year follow-up.
Reinforcing this possibility, a retrospective study analyzing 177 renal biopsy-proven LN showed that the hyperuricemic group had higher pathological kidney scores (including activity, chronicity, and tubulointerstitial impairment) than those without hyperuricemia [30]. Accordingly, in vitro and experimental studies have demonstrated that SUA can lead to tubular injury, endothelial dysfunction, oxidative stress, and intrarenal inflammation [31].
The retrospective study design is a limitation and may have hampered the accurate evaluation of some confounding factors such as diet, alcoholism, weight, drugs, and clinical conditions (hypertension, diabetes, and dyslipidemia) that may interfere in SUA levels [32]. The small sample size also precluded us from having a definitive conclusion whether SUA is independently related to the long-term renal outcome in LN patients or it is a reflex of underlying renal damages. Hyperuricemia is a known a risk factor for CKD, and these findings may be not only specific for LN patients but also useful for the management of their condition. Independent of the cause, persistent elevation of SUA seems to be relevant for long-term renal survival.
In conclusion, SUA level < 6.05 mg/dL at 12 months is a predictor of good long-term renal outcome in lupus nephritis. Whether elevated SUA is only a marker of subclinical chronic kidney disease or also an additional risk factor for renal dysfunction in lupus patients that will require intervention to decrease its levels remains to be determined.
References
Reátegui-Sokolova C, Ugarte-Gil MF, Gamboa-Cárdenas RV, Zevallos F, Cucho-Venegas JM, Alfaro-Lozano JL, Medina M, Rodriguez-Bellido Z, Pastor-Asurza CA, Alarcón GS, Perich-Campos RA, Lam MF, Chan TM (2017) Serum uric acid levels contribute to new renal damage in systemic lupus erythematosus patients. Clin Rheumatol 36(4):845–852. https://doi.org/10.1007/s10067-017-3538-4
Yap DY, Tang CS, Ma MK, Lam MF, Chan TM (2012) Survival analysis and causes of mortality in patients with lupus nephritis. Nephrol Dial Transplant 27(8):3248–3254. https://doi.org/10.1093/ndt/gfs073
Liu S, Gong Y, Ren H, Zhang W, Chen X, Zhou T, Li X, Chen N (2017) The prevalence, subtypes and associated factors of hyperuricemia in lupus nephritis patients at chronic kidney disease stages 1-3. Oncotarget. 8(34):57099–57108. https://doi.org/10.18632/oncotarget.19051.eCollection2017
Calich AL, Borba EF, Ugolini-Lopes MR, da Rocha LF, Bonfá E, Fuller R (2018) Serum uric acid levels are associated with lupus nephritis in patients with normal renal function. Clin Rheumatol 37(5):1223–1228. https://doi.org/10.1007/s10067-018-3991-8
Liu H, Cai X, Dai L, Ma J, Mo Y (2018) Elevated uric acid levels in premenopausal female systemic lupus erythematosus patients: association with potential or existing renal damage. Eur J Inflamm 16:1–6. sagepub.com/journals-permissions. journals.sagepub.com/home/eji. https://doi.org/10.1177/2058739218802442
Bomback AS, Appel GB (2010) Updates on the treatment of lupus nephritis. J Am Soc Nephrol 21:2028–2035. https://doi.org/10.1681/ASN.2010050472
Majdan M (2015) Treat-to-target in rheumatology. Wiad Lek 68:259–264
Van Vollenhoven RF, Mosca M, Bertsias G, van Vollenhoven RF, Mosca M, Bertsias G, Isenberg D, Kuhn A, Lerstrøm K, Aringer M, Bootsma H, Boumpas D, Bruce IN, Cervera R, Clarke A, Costedoat-Chalumeau N, Czirják L, Derksen R, Dörner T, Gordon C, Graninger W, Houssiau F, Inanc M, Jacobsen S, Jayne D, Jedryka-Goral A, Levitsky A, Levy R, Mariette X, Morand E, Navarra S, Neumann I, Rahman A, Rovensky J, Smolen J, Vasconcelos C, Voskuyl A, Voss A, Zakharova H, Zoma A, Schneider M (2014) Treat-to-target in systemic lupus erythematosus: recommendations from an international task force. Ann Rheum Dis 73:958–967. https://doi.org/10.1136/annrheumdis-2013-205139
Tamirou F, Lauwerys BR, Dall'Era M, Mackay M, Rovin B, Cervera R, Houssiau FA, Nephritis Trial Investigators MAINTAIN (2015) A proteinuria cut-off level of 0.7 g/day after 12 months of treatment best predicts long-term renal outcome in lupus nephritis: data from the MAINTAIN Nephritis Trial. Lupus Sci Med 2(1):e000123. https://doi.org/10.1136/lupus-2015-000123 eCollection 2015
Dall'Era M, Cisternas MG, Smilek DE, Straub L, Houssiau FA, Cervera R, Rovin BH, Mackay M (2015) Predictors of long-term renal outcome in lupus nephritis trials: lessons learned from the Euro-Lupus Nephritis cohort. Arthritis Rheum 67:1305–1313. https://doi.org/10.1002/art.39026
Ugolini-Lopes MR, Seguro LPC, Castro MXF, Daffre D, Lopes AC, Borba EF, Bonfá E (2017) Early proteinuria response: a valid real-life situation predictor of long-term lupus renal outcome in an ethnically diverse group with severe biopsy-proven nephritis? Lupus Sci Med 4(1):e000213. https://doi.org/10.1136/lupus-2017-000213 . eCollection 2017
Petri M, Orbai AM, Alarcón GS, Gordon C, Merrill JT, Fortin PR, Bruce IN, Isenberg D, Wallace DJ, Nived O, Sturfelt G, Ramsey-Goldman R, Bae SC, Hanly JG, Sánchez-Guerrero J, Clarke A, Aranow C, Manzi S, Urowitz M, Gladman D, Kalunian K, Costner M, Werth VP, Zoma A, Bernatsky S, Ruiz-Irastorza G, Khamashta MA, Jacobsen S, Buyon JP, Maddison P, Dooley MA, van Vollenhoven RF, Ginzler E, Stoll T, Peschken C, Jorizzo JL, Callen JP, Lim SS, Fessler BJ, Inanc M, Kamen DL, Rahman A, Steinsson K, Franks AG Jr, Sigler L, Hameed S, Fang H, Pham N, Brey R, Weisman MH, McGwin G Jr, Magder LS (2012) Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum 64(8):2677–2686. https://doi.org/10.1002/art.34473
Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoyan G, National Kidney Foundation (2003) National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med 139:137–147
Giannico G, Fogo AB (2013) Lupus nephritis: is the kidney biopsy currently necessary in the management of lupus nephritis? Clin J Am Soc Nephrol 8(1):138–145. https://doi.org/10.2215/CJN.03400412
Houssiau FA, Vasconcelos C, D'Cruz D, Sebastiani GD, Garrido Ed Ede R, Danieli MG, Abramovicz D, Blockmans D, Mathieu A, Direskeneli H, Galeazzi M, Gül A, Levy Y, Petera P, Popovic R, Petrovic R, Sinico RA, Cattaneo R, Font J, Depresseux G, Cosyns JP, Cervera R (2002) Immunosuppressive therapy in lupus nephritis: the Euro-Lupus Nephritis Trial, a randomized trial of low-dose versus high-dose intravenous cyclophosphamide. Arthritis Rheum 46:2121–2131. https://doi.org/10.1002/art.10461
Boumpas DT, Austin HA 3rd, Vaughn EM, Klippel JH, Steinberg AD, Yarboro CH, Balow JE (1992) Controlled trial of pulse methylprednisolone versus two regimens of pulse cyclophosphamide in severe lupus nephritis. Lancet. 340(8822):741–745
Appel GB, Cohen DJ, Pirani CL, Meltzer JI, Estes D (1987) Long-term follow-up of patients with lupus nephritis. A study based on the classification of the World Health Organization. Am J Med 83:877–885
Moroni G, Quaglini S, Maccario M, Banfi G, Ponticelli C (1996) "Nephritic flares" are predictors of bad long-term renal outcome in lupus nephritis. Kidney Int 50(6):2047–2053
Cuhadar S, Atay A, Koseoglu M, Dirican A, Hur A (2012) Stability studies of common biochemical analytes in serum separator tubes with or without gel barrier subjected to various storage conditions. Biochem Med (Zagreb) 22(2):202–214
Cuhadar S, Koseoglu M, Atay A, Dirican A (2013) The effect of storage time and freeze-thaw cycles on the stability of serum samples. Biochem Med (Zagreb) 23(1):70–77
Kachhawa K, Kachhawa P, Varma M, Behera R, Agrawal D, Kumar S (2017) Study of the stability of various biochemical analytes in samples stored at different predefined storage conditions at an accredited laboratory of India. J Lab Physicians 9(1):11–15. https://doi.org/10.4103/0974-2727.187928
Martínez-Martínez MU, Borjas-García JA, Magaña-Aquino M, Cuevas-Orta E, Llamazares-Azuara L, Abud-Mendoza C (2012) Renal function assessment in patients with systemic lupus erythematosus. Rheumatol Int 32(8):2293–2299. https://doi.org/10.1007/s00296-011-1940-9
Collaborative Study Group, Korbet SM, Whittier WL, Lewis EJ (2016) The impact of baseline serum creatinine on complete remission rate and long-term outcome in patients with severe lupus nephritis. Nephron Extra 6(2):12–21. https://doi.org/10.1159/000448487
McQuarrie EP, Traynor JP, Taylor AH, Freel EM, Fox JG, Jardine AG, Mark PB (2014) Association between urinary sodium, creatinine, albumin, and long-term survival in chronic kidney disease. Hypertension. 64(1):111–117. https://doi.org/10.1161/HYPERTENSIONAHA.113.03093
Feig DI (2014) Serum uric acid and the risk of hypertension and chronic kidney disease. Curr Opin Rheumatol 26(2):176–185. https://doi.org/10.1097/BOR.0000000000000033
Li L, Yang C, Zhao Y, Zeng X, Liu F, Fu P (2014) Is hyperuricemia an independent risk factor for new-onset chronic kidney disease?: a systematic review and meta-analysis based on observational cohort studies. BMC Nephrol 15:122. https://doi.org/10.1186/1471-2369-15-122
Hsieh YP, Chang CC, Yang Y, Wen YK, Chiu PF, Lin CC (2017) The role of uric acid in chronic kidney disease patients. Nephrology (Carlton) 22(6):441–448. https://doi.org/10.1111/nep.12679
Kang DH, Nakagawa T, Feng L, Watanabe S, Han L, Mazzali M, Truong L, Harris R, Johnson RJ (2002) A role for uric acid in the progression of renal disease. J Am Soc Nephrol 13(12):2888–2897
Kang DH, Nakagawa T (2005) Uric acid and chronic renal disease: possible implication of hyperuricemia on progression of renal disease. Semin Nephrol 25(1):43–49
Xie T, Chen M, Tang X, Yin H, Wang X, Li G, Li J, Zuo X, Zhang W (2016) Hyperuricemia is an independent risk factor for renal pathological damage and poor prognosis in lupus nephritis patients. Zhong Nan Da Xue Xue Bao Yi Xue Ban 41(10):1052–1057. https://doi.org/10.11817/j.issn.1672-7347.2016.10.007. Access Sept 2018
Kanellis J, Kang DH (2005) Uric acid as a mediator of endothelial dysfunction, inflammation, and vascular disease. Semin Nephrol 25(1):39–42
Feig DI, Kang DH, Johnson RJ (2008) Uric acid and cardiovascular risk. N Engl J Med 359(17):1811–1821. https://doi.org/10.1056/NEJMra0800885
Funding
This study was supported by grants from Conselho Nacional de Desenvolvimento Científico e Tecnológico (#305068/2014-8 to EB and #307226/2014-0 to EFB).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments and was approved by the Local Ethics committee.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ugolini-Lopes, M.R., Gavinier, S.S., Leon, E. et al. Is serum uric acid a predictor of long-term renal outcome in lupus nephritis?. Clin Rheumatol 38, 2777–2783 (2019). https://doi.org/10.1007/s10067-019-04620-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-019-04620-3