Abstract
Objective
To evaluate the diagnostic performance of bacterial identification by broad-range polymerase chain reaction (PCR) of ribosomal DNA (rDNA) 16 s (16S rDNA PCR) for the diagnosis of septic arthritis on native joints.
Methods
Patients with acute mono or oligoarthritis who underwent synovial fluid puncture and prospective follow-up allowing definitive diagnosis (septic arthritis, crystal related disease, chronic inflammatory arthritis, undifferentiated arthritis) were recruited in this single-center study. Systematic analysis of synovial fluid included leukocytes count, search for urate and pyrophosphate crystals with polarized light microscopy, direct bacteriological examination (gram staining), bacteriological culture, and 16S rDNA PCR.
Results
Ninety-five patients were included, 34 of which (35.8%) had septic arthritis. Nineteen (20.0%) patients had received probabilistic antibiotic therapy prior to joint puncture. Gram + cocci infection accounted for 79.4% of septic arthritis, of which nearly half (47.1%) was caused by Staphylococcus aureus. Eight (23.5%) septic arthritis patients had a 16S rDNA PCR positive in the synovial fluid with an AUC of 0.618 (95% CI, 0.493–0.742), a sensitivity of 0.24 (95% CI, 0.12–0.40), and a specificity of 1.00 (95% CI 0.94–1.00). The diagnostic performance of 16S rDNA PCR was lower than that of direct examination (AUC at 0.691, CI 95%, 0.570–0.812), blood cultures (AUC at 0.727, CI 95%, 0.610–0.844), and culture (0.925, CI 95%, 0.856–0.994) for the diagnosis of septic arthritis. There was no difference in the positivity of 16S rDNA PCR according to previous exposure to antibiotics.
Conclusions
16 s rDNA PCR in the synovial fluid does not improve the diagnostic performance of septic arthritis on native adult joints, particularly for Gram-positive cocci infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Septic arthritis is a diagnostic and therapeutic medical emergency due to excess mortality (2% at 1 month, approximately 10% at 1 year) and the frequency of joint functional sequelae (approximately 50%), requiring antibiotic therapy adapted to the microorganism involved [1,2,3]. The incidence of septic arthritis in native joints is increasing, particularly in subjects over 75 years of age [4], a population also exposed to crystal related arthritis, its main differential diagnosis [5].
Microbiological culture of joint fluid is considered the reference technique for bacterial identification. However, the sensitivity of this method varies from 67 to 87% for bacterial identification in septic arthritis cases [6,7,8]. The failure of conventional microbiological diagnosis techniques could be explained by the initiation of prior antibiotic therapy and the presence of slow-growing or non-cultivable bacteria on usual media [9].
Since the late 2000s, numerous publications [10,11,12,13,14,15] have reported the use of a new molecular biology technique, the broad-range polymerase chain reaction (PCR) targeting genes encoding 16 s ribosomal DNA (16 s rDNA). This technique makes it possible to detect a large number of bacterial species in a sample without first knowing whether the bacterium is cultivable or not in vitro. This diagnostic tool has proved interesting in various infections such as infectious endocarditis with negative blood cultures [10, 11], meningitis [12], or bacteremia during febrile neutropenia induced by chemotherapy [13].
Some studies suggest an interest of this technique for the diagnosis of bone and joint infections, particularly in difficult diagnostic situations corresponding to germs difficult to cultivate spontaneously or because of prior antibiotic therapy [14,15,16,17]. However, the heterogeneity of the results observed and the techniques used do not make it possible to generalize the use of this costly technique in clinical practice. In addition, new bacteriological techniques for rapid diagnosis are being evaluated in septic arthritis [18, 19]. These PCR techniques use primers specific to several genes of bacterial species (Multiplex PCR) [18] or genes of resistance to certain antibiotics (GeneXpert Cepheid PCR) [19]. Available in specialized bacteriology laboratories, they are not yet used in daily clinical practice.
The objective of this study was to establish the diagnostic performance of 16 s universal rDNA PCR in synovial fluid for the microbiological diagnosis of native joint septic arthritis in clinical practice.
Patients and methods
Inclusion criteria
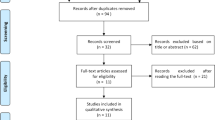
Adults (≥ 18 years old) referred for acute monoarthritis or oligoarthritis (progression < 6 weeks) on native joint and who received a diagnostic joint fluid puncture were included in this cross-sectional single-center study conducted at the Rennes university hospital rheumatology department with prospective recruitment from May 2000 to October 2016.
Parameters studied in synovial fluid
In the bacteriology laboratory, a cytological examination was carried out including a count of the elements (leukocytes, red blood cells) in single-use cells (Kova-Slide®, CML, Nemours, France) and the determination of the formula of the elements on a cytocentrifugation tablet (Cytospin®) after rapid staining (May-Grünwald-Giemsa) if ≥ 10 elements/mm3, and a direct examination after Gram staining on a cytocentrifugation tablet (qualitative and semi-quantitative evaluation with evaluation of the density and morphology of each bacterial species). A sample of each sample (10 μL) was then sown and incubated at 37 °C on the following media (AES France):
-
(i)
an enrichment medium (trypticase soy broth,) incubated in an aerobic atmosphere for 10 days,
-
(ii)
a 48-h incubated trypticase soy agar in an aerobic atmosphere,
-
(iii)
a cooked blood agar incubated under C02 (5%) for 48 h, and
-
(iv)
Schaedler broth and blood agar incubated anaerobically for 10 days and 3 days, respectively.
A sample of each synovial fluid was frozen at − 80 °C for the subsequent realization of the 16 s rDNA PCR (Technique described in Supplementary data).
Synovial fluid crystal analysis was performed with a compensated polarized light microscopy in the fresh state and after staining with May-Grünwald-Giemsa.
Other parameters studied
The following clinical variables were collected prospectively: patient’s age, sex, number of joints affected and their location, fever, comorbidities classically associated with septic arthritis, the presence of known chronic inflammatory or crystal arthritis, antibiotic intake prior to joint puncture, and its bacteriological analysis. The following biological variables were collected: CRP (mg/L) and synovial leukocytes counts (/mm3).
Diagnosis/definition of septic arthritis
The diagnosis of septic arthritis was made by the clinician who based his judgment on clinical and biological data according to Newman’s criteria [20], particularly synovial fluid direct examination and culture, blood culture, and the result of universal 16 s rDNA PCR and possibly a specific PCR.
Statistics
Statistical analysis was performed with the SPSS 20.0 software. The continuous quantitative variables were expressed as mean ± standard deviation or median ± IQR, after checking their Gaussian distribution or not by a Kolmogorov-Smirnof test. The comparison of these variables was performed by a Student’s t test (verified Gaussian distribution) or by a Mann-Whitney nonparametric U test (non-Gaussian distribution). The qualitative variables were expressed in absolute numbers and percentages and their comparison was carried out by a chi-2 (χ2) or exact Fischer test. To evaluate the diagnostic performance, ROC curves were performed with calculation of area under the curve (AUC), sensitivity (Se), specificity (Sp), positive likelihood ratio (LR+), negative likelihood ratio (LR−), and their 95% confidence intervals. A p value < 0.05 was considered significant.
Results
Study population characteristics (Table 1)
Ninety-five patients were included in this study, including 62 (65.3%) males, average age 57.7 ± 21.7 years. Patients most often had non-feverish (58.9%) monoarthritis (87.4%). Joints most often affected were the knee (n = 56, 58.9%), ankle (n = 15, 15.8%), shoulder (n = 8, 8.4%), wrist (n = 7, 7.4%), and hip (n = 6, 6.3%). Sixteen patients (16.8%) were already diagnosed with chronic inflammatory or crystal-related arthritis at the time of their acute arthritis episode. Nineteen (20.0%) patients had received probabilistic antibiotic therapy prior to the joint puncture. A diagnosis of septic arthritis was retained for 34 patients (35.8%). The non-bacteriological characteristics discriminating between septic arthritis and other non-infectious arthritis were a higher fever (p < 0.005), a more marked biological inflammatory syndrome. The diagnoses selected among non-infectious arthritis were 31 (32.6%) crystal arthritis (11 acute gouty arthritis and 20 acute calcium pyrophosphate deposits arthritis), 21 (22.1%) chronic inflammatory arthritis flares, 2 (2.1%) reactive arthritis with Chlamydia trachomatis, and 7 (7.3%) undifferentiatied or other non-septic arthritis.
Bacteriological characteristics of septic arthritis (Table 2)
Of the 34 septic arthritis cases, 16 (47.1%) were documented by blood culture and 30 (88.2%) by synovial fluid culture with direct positive examination in 13 (38.2%) cases. Note that two bacteriological cultures and one blood culture positive for coagulase-negative Staphylococcus were considered contaminations and not treated as septic arthritis by the clinician. In 79.4% (n = 27) of septic arthritis cases, the seed identified was from the Gram+ cocci family. Almost half of the cases (47.1%) were methicillin-sensitive Staphylococcus aureus (MSSA), and one third (32.1%) were Streptococcus sp. The remaining cases (14.7%) were Gram-negative bacterial infections.
Performance of DNAr16S PCR for the diagnosis of septic arthritis on native joints (Table 3)
Eight (23.5%) septic arthritis had positive 16S rDNA PCR in synovial fluid (1 MSSA, 2 S.agalactiae, 1 S.pneumoniae, 1 Capnocytophaga canimorsus, 1 S.marcescens, 1 P.aeruginosa, 1 Neisseria meningitidis). No arthritis classified as non-septic had a positive 16S rDNA PCR, i.e., a sensitivity calculated at 0.24 (CI 95% 0.12–0.40) for a specificity of 1.00 (CI 95% 0.94–1.00) with AUC at 0.618 (CI 95% 0.493–0.742). The diagnostic performance of this technique was lower than that of direct examination (AUC at 0.691 CI 95% 0.570–0.812), blood cultures (AUC at 0.727, CI 95% 0.610–0.844), and culture (0.925, CI 95% 0.856–0.994). No difference in 16S rDNA PCR positivity was observed based on previous antibiotic exposure (OR = 1.83 (CI 95% 0.27–12.5), p = 0.53), nor based on direct examination positivity (OR = 0.96 (CI 95% 0.19–4.92), p = 0.96). In three cases, 16S rDNA PCR was negative (patients 1, 16, and 24) due to the presence of Taq polymerase inhibitors. 16S rDNA PCR was significantly more frequently positive in Gram-negative infections (n = 4, 57.1%) than Gram-positive infections (n = 4, 14.8%) (OR = 7.69 (CI 95% 1.22–47.6), p = 0.02).
Discussion
In this study, the 16 s rDNA PCR technique was the least effective microbiological technique compared to direct examination after Gram staining, blood cultures, and especially bacteriological culture of synovial fluid. The 16 s rDNA PCR technique did not provide any additional benefit for the diagnosis of septic arthritis treated with antibiotics prior to performing the synovial fluid puncture.
This technique seems to be defective for the diagnosis of Gram+ cocci infections and in particular Staphylococcus sp., the germ responsible for the majority of septic arthritis.
Fenollar et al. [15], in a large series of 525 bone and joint samples (255 joint fluids and 270 bone biopsies) found different results with sensitivity and specificity of rDNA PCR 16 s estimated at 92.5% and 98.7% respectively. However, unlike in our study, most punctures were performed on prosthetic joints (155 patients) and very few on native joints. Fihman et al. [16], in their study of 76 joint or bone samples, calculated a sensitivity of the 16 s rDNA PCR technique of 73.3% and a specificity of 95.2%. However, only 11 septic arthritis (4 Staphylococcus aureus, 4 Streptococcus sp., and 3 Neisseria gonorrhoeae) on native joints were included, with 7 synovial fluids available (and 4 synovial biopsies). Of the synovial fluids available, 16 s rDNA PCR was positive for only one in two Staphylococcus aureus infections and three in four Streptococcus sp.
Bonilla et al. [17] obtained a sensitivity of 62.5% and a specificity of 100% of r16S rDNA PCR in 16 cases of septic arthritis in peripheral joints (including 7 sepsis in joint replacements). Our team [21] recently obtained diagnostic performances lower than these results on 111 bone and joint samples (76 patients), including 26 synovial fluids on native joints, with a low sensitivity (29.6%) and excellent specificity (100%) of 16S rDNA PCR (AUC at 0.648), i.e., a diagnostic performance lower than the direct examination and culture, but higher than that of MALDI-TOF. Contrary to the situation of children in which 16S rDNA PCR is of major interest for the diagnosis of Kingela kingae septic arthritis [22, 23], the diagnostic performance of this technique therefore seems much less convincing in adults.
Several hypotheses could explain the low sensitivity of 16 s rDNA PCR in our study. In three cases, rDNA PCR 16 s was found to be defective due to the presence of Taq DNA polymerase inhibitors, a known cause of false negative results. This discrepancy is probably explained by a better sensitivity of the specific PCR technique, recognized for bone and joint infections due to Staphylococcus aureus and Mycobacterium tuberculosis [24]. However, none of the false 16S rDNA PCR negatives for Staphylococcus aureus infections were explained by the presence of a Taq DNA polymerase inhibitor in our study. This difficulty in identifying Gram-positive species by 16 s rDNA PCR was also reported in the literature [25, 26]. Rantakokko-Jalava et al. [26], in a study of 536 samples, reported 16 false negatives with PCR including 11 Gram-positive bacteria (3 Staphylococcus aureus, 5 Streptococcus sp., 2 Cutibacterium acnes and 1 Listeria monocytogenes), 4 mycobacteria and 1 Gram-negative bacteria (Pseudomonas aeruginosa). As in our study, the authors showed a significant difference between the detection of Gram-positive and Gram-negative bacteria. The nature of the bacterial wall would appear to play a role during the bacterial DNA extraction phase. Indeed, the lysis of bacteria requires the degradation of the bacterial wall which allows the bursting of cells and the release of intracellular constituents, including bacterial DNA. In addition, bacterial lysis is more difficult for Gram-positive bacteria because of their more resistant wall, composed mainly of peptidoglycan, which could explain the difficulty in extracting the bacterial DNA necessary for PCR amplification. Also, the bacterial lysis technique must be well adapted to the type of bacteria. If the lysis is insufficient, the bacterial DNA will not be released; if this bacterial lysis is too powerful, there will be a risk of destroying it [26, 27]. Given the difference in results between our series and previous studies, we decided to test the MagNAPure technique used by Fenollar et al. [15] on methicillin-sensitive S.aureus arthritis samples. Despite the change in the extraction technique, our results of broad-range 16S rDNA PCR amplification remained negative (results not shown). The hypothesis of the presence of a weak bacterial inoculum in the joint fluid has been evoked [25]. However, we did not show any association between direct examination positivity (indicating a certain bacterial inoculum) and 16S rDNA PCR positivity, which does not provide an argument this hypothesis for native joint septic arthritis. It has also been suggested that there may be “persistent” forms of bacteria, which form microcolonies and are often found in chronic staphylococcal bone infections [28]. These dwarf colonies are reputed to be more difficult to extract and could also be at the origin of the failure of certain extractions. In addition, we chose to amplify only the single sequences detected at the electrophoreogram. In our study, the sequencing of the PCR products was not performed after amplification in several cases due to the appearance of several bands on the electrophoreogram. Fenollar et al. [15] used a cloning and sequencing technique when the electrophoreograms highlighted multiple bands. This technique allowed them to identify polymicrobial infections with the identification of six or seven different bacteria in several cases. However, these were patients suffering from osteitis following an open fracture or skin ulcers responsible for polymicrobial infections, a rare situation during acute hematogenic arthritis. These various bacteria identified include pathogens rarely or never described in bone and joint infections, germs not known to be pathogenic in humans, and new bacterial species whose pathological responsibility can be discussed. Finally, poor performance of 16S rDNA PCR for the diagnosis of infection has also been reported on other biological samples such as heart valves and cerebrospinal fluid, which does not make synovial fluid an exception [10,11,12].
Faced with these disappointing results of the 16 s rDNA for the microbiological diagnosis of septic arthritis, new bacteriological techniques for rapid diagnosis have been recently evaluated. The multiplex PCR technique with its combination of multiple genetic primers specific to the main bacteria involved in septic arthritis (Staphylococcus spp., Streptococcus (groups A, B, and C), Enterococcus sp, and main Enterobacteriaceae) appears attractive. However, the primers of some pathogenic bacteria such as Streptococcus pneumoniae are not included in the kit. The use of this technique does not seem to improve the diagnosis performance of bone and joint infections, as the results were found positive in only 27% [18] to 45% [29] in septic arthritis, mainly in prosthetic joints, with a concordance of 58% with bacterial identification in culture and 70% with PCR 16sDNAr [29]. Another approach is to assess resistance to probabilistic antibiotic therapy for acute febrile monoarthritis with probable diagnosis of septic arthritis without bacteriological documentation using resistance gene specific priming amplification. In a total of 184 specimens of bone and joint samples from a population of 125 children (septic arthritis/osteomyelitis in 61%), the completion of a novel musculoskeletal diagnostic panel (MDP) that incorporates three components: the Xpert MRSA/SA SSTI assay, a qPCR for the erm (erythromycin ribosomal methylase) A, B, and C genes that confer clindamycin resistance, and a qPCR for K. kingae, was evaluated, reporting an excellent negative predictive value of 99%, 98%, and 100% respectively [19].
In conclusion, our study suggests that broadband 16 s rDNA PCR in synovial fluid does not improve the diagnostic performance of septic arthritis in this cohort of acute arthritis in native adult joints, with numerous false negatives for Gram+ infection, the most common case observed in septic arthritis.
References
Mathews CJ, Weston VC, Jones A, Field M, Coakley G (2010) Bacterial septic arthritis in adults. Lancet 375:846–855
Kennedy N, Chambers ST, Nolan I, Gallagher K, Werno A, Browne M, Stamp LK (2015) Native joint septic arthritis: epidemiology, clinical features, and microbiological causes in a New Zealand population. J Rheumatol 42:2392–2397
Gomez-Junyent J, Murillo O, Grau I, Benavent E, Ribera A, Cabo X, Tubau F, Ariza J, Pallares R (2018) Analysis of mortality in a cohort of 650 cases of bacteremic osteoarticular infections. Semin Arthritis Rheum 48:327–333
Rutherford AI, Subesinghe S, Bharucha T, Ibrahim F, Kleymann A, Galloway JB (2016) A population study of the reported incidence of native joint septic arthritis in the United Kingdom between 1998 and 2013. Rheumatology (Oxford) 55:2176–2180
Prior-Español Á, García-Mira Y, Mínguez S, Martínez-Morillo M, Gifre L, Mateo L (2018) Coexistence of septic and crystal-induced arthritis: a diagnostic challenge. A report of 25 cases. Reumatol Clín. https://doi.org/10.1016/j.reuma.2017.12.015
Ryan MJ, Kavanagh R, Wall PG, Hazleman BL (1997) Bacterial joint infections in England and Wales: analysis of bacterial isolates over a four year period. Br J Rheumatol 36:370–373
Weston VC, Jones AC, Bradbury N, Fawthrop F, Doherty M (1999) Clinical features and outcome of septic arthritis in a single UK Health District 1982-1991. Ann Rheum Dis 58:214–219
Eberst-Ledoux J, Tournadre A, Mathieu S, Mrozek N, Soubrier M, Dubost JJ (2012) Septic arthritis with negative bacteriological findings in adult native joints: a retrospective study of 74 cases. Joint Bone Spine 79:156–159
Dubost JJ (2006) Septic arthritis with no organism: a dilemma. Joint Bone Spine 73:341–343
Podglajen I, Bellery F, Poyart C, Coudol P, Buu-Hoï A, Bruneval P, Mainardi JL (2003) Comparative molecular and microbiologic diagnosis of bacterial endocarditis. Emerg Infect Dis 9:1543–1547
Goldenberger D, Künzli A, Vogt P, Zbinden R, Altwegg M (1997) Molecular diagnosis of bacterial endocarditis by broad-range PCR amplification and direct sequencing. J Clin Microbiol 35:2733–2739
Kotilainen P, Jalava J, Meurman O, Lehtonen OP, Rintala E, Seppälä OP, Eerola E, Nikkari S (1998) Diagnosis of meningococcal meningitis by broad-range bacterial PCR with cerebrospinal fluid. J Clin Microbiol 36:2205–2209
Ley BE, Linton CJ, Bennett DM, Jalal H, Foot AB, Millar MR (1998) Detection of bacteraemia in patients with fever and neutropenia using 16S rRNA gene amplification by polymerase chain reaction. Eur J Clin Microbiol Infect Dis 17:247–253
Jalava J, Skurnik M, Toivanen A, Toivanen P, Eerola E (2001) Bacterial PCR in the diagnosis of joint infection. Ann Rheum Dis 60:287–289
Fenollar F, Roux V, Stein A, Drancourt M, Raoult D (2006) Analysis of 525 samples to determine the usefulness of PCR amplification and sequencing of the 16S rRNA gene for diagnosis of bone and joint infections. J Clin Microbiol 44:1018–1028
Fihman V, Hannouche D, Bousson V, Bardin T, Lioté F, Raskine L et al (2007) Improved diagnosis specificity in bone and joint infections using molecular techniques. J Inf Secur 55:510–517
Bonilla H, Kepley R, Pawlak J, Belian B, Raynor A, Saravolatz LD et al (2011) Rapid diagnosis of septic arthritis using 16S rDNA PCR: a comparison of 3 methods. Diagn Microbiol Infect Dis 69:390–395
Morgenstern C, Renz N, Cabric S, Perka C, Trampuz A (2018) Multiplex polymerase chain reaction and microcalorimetry in synovial fluid: can pathogen-based detection assays improve the diagnosis of septic arthritis? J Rheumatol 45:1588–1593
Searns JB, Robinson CC, Wei Q, Yuan J, Hamilton S, Pretty K et al (2018) Validation of a novel molecular diagnostic panel for pediatric musculoskeletal infections: integration of the Cepheid Xpert MRSA/SA SSTI and laboratory-developed real-time PCR assays for clindamycin resistance genes and Kingella kingae detection. J Microbiol Methods 156:60–67
Newman JH (1976) Review of septic arthritis throughout the antibiotic era. Ann Rheum Dis 35:198–205
Lallemand E, Coiffier G, Arvieux C, Brillet E, Guggenbuhl P, Jolivet-Gougeon A (2016) MALDI-TOF MS performance compared to direct examination, culture, and 16S rDNA PCR for the rapid diagnosis of bone and joint infections. Eur J Clin Microbiol Infect Dis 35:857–866
Rosey AL, Abachin E, Quesnes G, Cadilhac C, Pejin Z, Glorion C, Berche P, Ferroni A (2007) Development of a broad-range 16S rDNA real-time PCR for the diagnosis of septic arthritis in children. J Microbiol Methods 68:88–93
Hernández-Rupérez MB, Suárez-Arrabal MDC, Villa-García Á, Zarzoso-Fernández S, Navarro-Gómez M, Santos-Sebastián M et al (2018) Kingella kingae as the main cause of septic arthritis: importance of molecular diagnosis. Pediatr Infect Dis J 37:1211–1216
Fenollar F, Lévy PY, Raoult D (2008) Usefulness of broad-range PCR for the diagnosis of osteoarticular infections. Curr Opin Rheumatol 20:463–470
Harris KA, Hartley JC (2003) Development of broad-range 16S rDNA PCR for use in the routine diagnostic clinical microbiology service. J Med Microbiol 52:685–691
Rantakokko-Jalava K, Jalava J (2002) Optimal DNA isolation method for detection of bacteria in clinical specimens by broad-range PCR. J Clin Microbiol 40:4211–4217
Rantakokko-Jalava K, Nikkari S, Jalava J, Eerola E, Skurnik M, Meurman O, Ruuskanen O, Alanen A, Kotilainen E, Toivanen P, Kotilainen P (2000) Direct amplification of rRNA genes in diagnosis of bacterial infections. J Clin Microbiol 38:32–39
Marrie TJ, Costerton JW (1985) Mode of growth of bacterial pathogens in chronic polymicrobial human osteomyelitis. J Clin Microbiol 22:924–933
Malandain D, Bémer P, Leroy AG, Léger J, Plouzeau C, Valentin AS, Jolivet-Gougeon A, Tandé D, Héry-Arnaud G, Lemarié C, Kempf M, Bret L, Burucoa C, Corvec S, Cottin J, Ducellier F, Abgueguen P, Balan V, Stindel E, Ansart S, Greves A, Aubin G, Touchais S, Gouin F, Boutoille D, Asseray N, Happi L, Guinard J, Razanabola F, Mille C, Cognée AS, Gayet LE, le Moal G, Thomas C, Polard JL, Arvieux C, Meheut A, Bernard L, Rosset P, Gras G, Druon J, Fèvre K (2018) Assessment of the automated multiplex-PCR Unyvero i60 ITI® cartridge system to diagnose prosthetic joint infection: a multicentre study. Clin Microbiol Infect 24:83.e1–83.e6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 18 kb)
Rights and permissions
About this article
Cite this article
Coiffier, G., David, C., Gauthier, P. et al. Broad-range 16 s rDNA PCR in synovial fluid does not improve the diagnostic performance of septic arthritis in native joints in adults: cross-sectional single-center study in 95 patients. Clin Rheumatol 38, 1985–1992 (2019). https://doi.org/10.1007/s10067-019-04492-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-019-04492-7