Abstract
To evaluate quality of life (QoL) in patients with axial spondyloarthritis (axSpA) and its association with disease activity, functionality, structural damage, and spinal mobility, using patient-reported outcomes. This was an observational, cross-sectional, and single-center study in which 100 consecutive patients with axSpA were included. We obtained from all patients’ sociodemographic data and values related to disease activity, functionality, structural damage, mobility, and quality of life. The Ankylosing Spondylitis Quality of Life Questionnaire (ASQoL) was considered as the primary outcome. Pearson r statistic, Student’s T test, and univariate and multivariate linear regressions were performed to relate ASQoL with the studied covariates. Mean ASQoL score in all patients was 4.02 ± 2.81, with statistically significant differences between male and female (3.61 ± 2.80 vs. 4.83 ± 2.70). Patients with high disease activity (measured by the ASAS-endorsed Disease Activity Score, ASDAS > 2.1) showed higher mean score in ASQoL than those with low disease activity (ASDAS ≤ 2.1) (3.21 ± 0.74 vs. 1.43 ± 0.43, p < 0.001). ASQoL presented a significant linear correlation with BASDAI, BASFI, and ASDAS (r > 0.60). However, disease duration was not significantly correlated with ASQoL. Finally, the 68.9% of the ASQoL variability (R2 = 0.689) was determined by BASDAI, BASFI, and mSASSS, presenting mSASSS a negative regression coefficient (− 0.035). In our study, the impairment of QoL was mainly associated with disease activity (BASDAI) and worsening of functionality (BASFI). However, there is an inverse relationship between the worsening of QoL and structural damage. In addition, disease duration does not seem to influence the patient’s welfare.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Axial spondyloarthritis (axSpA) [1] is a chronic inflammatory disease characterized by inflammation and bone formation in the sacroiliac joints and spine [2, 3]. This entity includes two types of patients: those with radiographic changes defined on a simple sacroiliac X-ray (radiographic axSpA) [4, 5], whose hallmark is ankylosing spondylitis (AS) [6], and those who do not present changes in X-ray (non-radiographic axSpA).
The symptoms presented by these patients, such as inflammatory lumbar pain, morning stiffness, fatigue [7], and loss of spinal mobility [8], represent the clinical expression of lumbar spine inflammation, which leads to structural damage at that level. All of these symptoms have repercussions on different aspects of the patient’s life, such as their psychological state, occupational productivity [9], and quality of life (QoL) [10]. In addition, the diagnosis of SpA is usually performed between the second and third decades of life, thus impacting at the time of greater social and work performance [11].
It is becoming increasingly important to evaluate the overall impact of the disease and the general state of patients with rheumatic diseases, particularly in SpA. For these evaluations, physicians use the patient-reported outcomes (PROs): tools based on questionnaires that allow the patient to provide information to their rheumatologist about different subjective aspects related to their disease. One of the most commonly used PROs is the Ankylosing Spondylitis Quality of Life Questionnaire (ASQoL) [12], which refers to health-related quality of life. The Bath Ankylosing Spondylitis Patient Global Score (BAS-G) [13], another important PRO, provide information about the patient’s overall status with regard to his illness. Thus, these instruments (which are used in most clinical trials in patients with axSpA to assess therapeutic efficacy and response [14, 15]) have an important role in daily practice.
In recently published studies, Fernández-Carbadillo C et al. correlated disease activity with a worsening of the QoL [16]; however, this study has been performed in patients from the ESPERANZA program, who present a recent diagnosis of SpA (< 2 years of disease duration). In the same line, Almodóvar R et al. suggested an association between poor spinal mobility [17] and a deterioration of the QoL (evaluated through the use of ASQoL); however, in this study the QoL was not evaluated as the primary outcome but as a secondary variable.
Therefore, the main objective of this study was to evaluate the QoL (measured by ASQoL) in patients with axSpA and to determine its association with different indicators of disease activity, functionality, spinal mobility, and structural damage.
Materials and methods
This was an observational, cross-sectional, and single-center study which included 100 consecutive patients from a Spondyloarthritis consultation. All participants have a diagnosis of ax-SpA and met the Assessments in Ankylosing Spondylitis Working group (ASAS) criteria for ax-SpA [18]. Also, all of them presented definite changes in simple X-rays of their sacroiliac bones [4, 5].
The study was approved by the Ethics Committee of the Hospital, and each of the participants signed an informed consent to be part of the study.
Variables studied
In each patient, sociodemographic and disease-related variables were collected, such as sex, age, HLA-B27 antigen positivity, and disease duration (expressed as years since first symptoms of the disease). All patients were submitted to a radiographic study, with the objective of assessing structural damage using the modified Stoke Ankylosing Spondylitis Spine Score (mSASSS) [19].
For the evaluation of spinal mobility, the UCOTrack ™ system [20] (based on the capture of kinematic measures by placing markers on the patient) was used. This method provides us an index of cervical and lumbar mobility with a range of 0 to 10, with the name of UCOASMI (University of Cordoba Ankylosing Spondylitis Metrology Index, 0–10 scale) [21, 22]. The Bath Ankylosing Spondylitis Metrology Index (BASMI, 0–10 scale) was also measured [23] to evaluate mobility. Anthropometric measures were performed by the same physician and at the same time of day in all participants to avoid variability in measurements, especially those related to morning stiffness.
Medians of disease duration, mSASSS, BASMI, and UCOASMI were used as cut-off when variables were considered as qualitative. Based on the mSASSS and disease duration medians, patients were classified as having aggressive clinical form (mSASSS ≥ 8 and disease duration ≤ 12 years) and non-aggressive clinical form (mSASSS < 8 and disease duration > 12 years). We considered that patients who are not included in these two groups, followed a normal disease course.
Regarding functionality, the Bath Ankylosing Spondylitis Functional Index (BASFI, 0–10 scale) questionnaire [24] was used. The BAS-G (0–10 scale) was considered to evaluate the general condition of patients.
The Bath Ankylosing Spondylitis Disease Activity Index (BASDAI, 0–10 scale) [25] and the ASAS-endorsed Disease Activity Score (ASDAS) [26] were used as variables related to disease activity. ASDAS includes four items in the form of a visual analogue scale which refer lumbar pain, morning stiffness, peripheral joint pain and overall disease status, and a fifth item that can refer to both C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR). In our study, we used ASDAS-CRP because it is the most commonly used. This index was considered in the study as a quantitative and qualitative variable, using a cut-off of ≤ 2.1 and > 2.1 (corresponding to moderate-low and high-very high disease activity, respectively) [27].
Finally, the ASQoL [12] questionnaire, which measures the QoL on a scale ranging from 0 to 18 (being 18 points the worst possible score in terms of QoL), was used as the main variable.
Statistical analysis
Statistical analysis was performed using SPSS software (v. 17). A p value < 0.05 was considered significant. Descriptive data are presented as the means ± standard deviation (SD) for quantitative variables and as frequencies and percentages for qualitative variables.
Firstly, several correlations were performed to evaluate the presence of a linear correlation between the different quantitative variables (related to mobility, functionality, disease activity, structural damage, and QoL). Therefore, we were able to determine the Pearson correlation coefficient r for each of the comparisons, classifying them as moderate, strong, or very strong correlations if the value of r was between 0.40 and 0.69, 0.70 and 0.89; and 0.90 and 0.99, respectively. Subsequently, considering ASQoL as the dependent variable, we calculated the coefficient of determination (R2) using a univariate linear regression for each of the variables. In addition, a multiple linear regression was performed to quantify the relationship of BASDAI, BASFI, BASMI, ASDAS, UCOASMI, mSASSS, disease duration, and sex with the ASQoL variability. Finally, Student’s T test was used to calculate the differences of means for the variables previously mentioned in different subgroups of patients (according to the presence of HLA-B27, disease duration, clinical form, ASDAS, UCOASMI, and BASMI).
Results
Among the 100 patients included in the study, 67 (67%) were men and 33 (33%) women, with a mean age of 48.38 ± 11.05 years and a mean disease duration of 14.37 ± 10.74 years. Table 1 presents the most important descriptive data of the studied population.
Table 2 shows the different correlations between the variables related to mobility (UCOASMI and BASMI), functionality (BASFI), disease activity (BASDAI and ASDAS), structural damage (mSASSS), and quality of life (ASQoL). The table also includes the disease duration to evaluate its influence on the other variables. A strong positive linear correlation was identified (p < 0.01) between ASQoL-BASDAI and between ASQoL-BASFI [r = 0.756 and r = 0.788, respectively]. Additionally, significant (p < 0.01) moderate correlation (r = 0.4–0.7) of the variables ASDAS, BASMI, and UCOASMI regarding ASQoL were obtained.
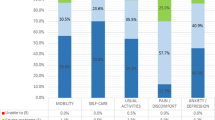
Figure 1 shows six graphics that represent the goodness of fit of the simple linear regressions between ASQoL and the different covariates. The 62.1% (R2 = 0.621) and 57.1% (R2 = 0.571) of ASQoL variability can be explained by BASFI and BASDAI values, respectively (p < 0.001).
Correlations between ASQoL and the rest of variables. ASDAS ASAS-endorsed disease activity score, ASQoL Ankylosing Spondylitis Quality of Life Questionnaire. BASDAI Bath Ankylosing Spondylitis Disease Activity Index, BASFI Bath Ankylosing Spondylitis Functional Index, BASMI Bath Ankylosing Spondylitis Metrology Index, BAS-G Bath Ankylosing Spondylitis Patient Global Score, mSASSS modified Stoke Ankylosing Spondylitis Spine Score, UCOASMI University of Cordoba Ankylosing Spondylitis Metrology Index
A multiple linear regression was performed to evaluate the ASQoL variability including in the model BASDAI, BASFI, BASMI, UCOAMI, ASDAS, mSASSS, disease duration, and gender. In the final model, shown in Table 3, 68.9% of the ASQoL variability (R2 = 0.689) was statistically explained by the BASDAI, BASFI, and mSASSS levels. However, mSASSS presented a negative regression coefficient (− 0.035).
Table 4 represents the differences in means of the quantitative variables between groups of patients stratified according to different characteristics (gender, presence of HLA-B27 antigen, disease duration > 12 years, aggressive clinical form, ASDAS > 2.1, UCOASMI > 4.2, and BASMI ≥ 2.4). Regarding the gender, we observed a lower average ASQoL score (better QoL) in male vs. female (3.61 ± 2.80 vs. 4.83 ± 2.70, p < 0.01). In addition, ASQoL levels were higher (p < 0.01) in patients with high disease activity (3.21 ± 0.74 vs. 1.43 ± 0.43, for ASDAS > 2.1 vs. ASDAS ≤ 2.1, respectively) and in those with poor spine mobility (5.07 ± 2.78 vs. 2.70 ± 2.41, p < 0.01, for patients with UCOASMI > 4.2 vs. UCOASMI ≤ 4.2, respectively).
Regarding other covariates, there were significant differences in mSASSS score between male and female (18.13 ± 18.75 vs. 6.91 ± 3.90, respectively) and between patients with disease duration > 12 years vs. patients with disease duration ≤ 12 years (19.50 ± 19.44 vs. 10.11 ± 11.71, respectively). Patients with high disease activity (ASDAS > 2.1) showed higher scores in ASQoL, BASFI, and BAS-G (p < 0.01) and in UCOASMI (p < 0.05). Patients with poor spinal mobility (UCOASMI > 4.2) showed statistically significant differences (p < 0.01) in ASQoL, ASDAS, BASFI, BAS-G, and mSASSS, against those with greater spinal mobility. Finally, no significant differences were found between patients with HLA-B27 antigen.
Discussion
QoL is a difficult concept to quantify in patients with SpA since it is composed of emotional, social, and health factors. The deterioration of the QoL in patients with SpA is a frequent and not negligible fact, due to its implication in a negative perception about their emotional, occupational, and social situations. To our knowledge, this is the first study which use QoL as the target variable measured by the ASQoL.
In our study, the mean ASQoL was somewhat lower than that of other studies reporting the QoL in Spanish patients [17]; although, the mean disease duration was similar. One possible explanation is that the Spanish cohort shows worse levels in disease activity and functionality, which can be associated to a poor QoL.
Our results suggest a direct relationship between loss of functionality (BASFI) and impairment of QoL as measured by the ASQoL. A previously published study argued that much of the health-related QoL (HR-QoL) is determined by physical capacity in patients with SpA [28]. Our study showed that there was a strong correlation between the ASQoL and patient functionality (BASFI) (r = 0.788), thus indicating that one of the symptoms that most negatively influences patients is loss of autonomy and difficulty in performing the basic activities of daily life.
In addition, the worsening of the ASQoL is significantly related to disease activity as measured by the BASDAI. Possible reason for the strong correlation between ASQoL-BASDAI and ASQOL-BASFI is that both include measures of similar things such as fatigue and pain, that can impact on daily living activities, household function, and social function. Thus, recently published studies confirming that disease activity is independently associated with a worsening of QoL in patients with early forms of SpA [16]. This relationship may be explained, as some studies show, by a worsening of inflammatory lumbar pain and, consequently, an increase in nocturnal awakenings, which in turn influence the perception of welfare [29]. Therefore, active SpA is associated with a worsening in physical capacity, which conditions a decrease of the patient’s QoL. Interestingly, high levels in ASDAS are not associated to QoL, maybe because this index is compounded by one item which is not crucial in axSpA (i.e., VAS peripheral arthritis) and by other which did not show statistically significative differences regarding QoL (i.e., global VAS).
However, there is a poor relationship between spinal mobility (measured by BASMI and UCOASMI) and ASQoL, which reflects that patients do not perceive mobility limitation as a problem in their daily lives.
Regarding structural damage, multivariate linear regression shows that mSASSS is paradoxically inversely associated with QoL, i.e., a higher rate of structural damage is associated with a better QoL. In addition, patients with more than 12 years of disease duration presented a worsening of anthropometric measures and greater structural damage compared with those with early forms of the disease; however, both groups show similar QoL values. Therefore, these results suggest that the disease duration does not influence the perception of welfare, that can be explained by the possible phenomenon of “habituation” to the functional deficits of these patients [30]. It is likely that in newly diagnosed young patients, the perception of quality of life is influenced by concerns about their future, work expectations, and the way they deal with the disease [31]. It seems that disease activity and pain may influence the conducting of normal tasks in patients with short disease duration. As the SpA progresses, in patients with a long disease duration and low functionality, activities are not the same as a young patient; therefore, they become accustomed to planning their life within their normal limitations. The decrement in pain perceived by axSpA patients as the mSASSS increases may be explained by the development of syndesmophytes, which can be less painful than erosions. It can also be explained by the “habituation” phenomenon (previously mentioned), with which patients become accustomed to latent chronic pain, so that it passes more unnoticed.
Regarding the women included in this study, their QoL was statistically significantly worse than that of men, despite having minor structural damage, as measured by mSASSS. Several international series of patients with SpA also support these data [32], in which male patients have a better subjective assessment of their QoL, even when presenting clinical forms with greater structural damage [33]. Fatigue, the emotional component [34] and fibromyalgia are likely present in a small percentage of patients with axSpA, influencing the outcome of this questionnaire [35]. Finally, patients with poor spinal mobility (UCOASMI > 4.2) showed worse levels ASQoL against those with greater spinal mobility, which confirms the influence of the axial mobility in the perception of QoL [17].
This analysis has some weaknesses but also some strengths. One weakness concerns to the evaluation of the radiographic study to obtain the mSASSS index, which was performed by a trained rheumatologist instead of a radiologist. This method was employed since it resembles typical clinical practice, where a simple X-ray is interpreted by the rheumatologist. Another important weakness is the subjectivity of questionnaires used in order to evaluate the patient’s condition. An advantage of this study is the use of a new objective parameter of the measurement of spinal mobility, i.e., the UCOASMI index, which has greater reliability and accuracy, thus avoiding subjectivity as well as intra- and interobserver variability.
Our results suggest that the impairment of QoL in patients with axSpA was mainly associated with disease activity (BASDAI) and worsening of functionality (BASFI). However, there is an inverse relationship between the worsening of QoL and structural damage. Finally, disease duration does not seem to influence the patient’s welfare.
References
Rudwaleit M, Landewé R, van der Heidje D et al (2009) The development of assessment of spondyloarthritis international society classification criteria for axial spondyloarthritis (part I): classification of paper patients by expert opinion including uncertainty appraisal. Ann Rheum Dis 68:770–776 3
Dougados M, Baeten D (2011) Spondyloarthritis. Lancet 377:2127–2137
Khan M (1998) Ankylosing spondylitis: clinical aspects. In: Calin A, Taurog J (eds) The spondyloarthritides. Oxford University Press, Oxford
Wallis D, Haroon N, Ayearst R, Carty A, Inman RD (2013) Ankylosing spondylitis and nonradiographic axial spondyloarthritis: part of a common spectrum or distinct diseases? J Rheumatol 40:2038–2041
Robinson PC, Wordsworth BP, Reveille JD, Brown M (2013) Axial spondyloarthritis: a new disease entity, not necessarily early ankylosing spondylitis. Ann Rheum Dis 72:162–164
Van der Linden S, Valkenburg HA, Cats A (1984) Evaluation of diagnostic criteria for ankylosing spondylitis: a proposal for modification of the New York criteria. Arthritis Rheum 27:361–368
López-Medina C, Schiotis RE, Font-Ugalde P et al (2016) Assessment of fatigue in spondyloarthritis and its association with disease activity. J Rheumatol 43(4):751–757
Calvo-Gutiérrez J, Garrido-Castro JL, Gil-Cabezas J et al (2015) Is spinal mobility in patients with spondylitis determined by age, structural damage and inflammation? Arthritis Care Res 67(1):74–79
Martindale J, Shukla R, Goodacre J (2015) The impact of ankylosing spondylitis/axial spondyloarthritis on work productivity. Best Pract Res Clin Rheumatol 29(3):512–523
Dougados M, d’Agostino MA, Benessiano J, Berenbaum F, Breban M, Claudepierre P, Combe B, Dargent-Molina P, Daurès JP, Fautrel B, Feydy A, Goupille P, Leblanc V, Logeart I, Pham T, Richette P, Roux C, Rudwaleit M, Saraux A, Treluyer JM, van der Heijde D, Wendling D (2011) The DESIR cohort: a 10-year follow-up of early inflammatory back pain in France: study design and baseline characteristics of the 708 recruited patients. Joint Bone Spine 78(6):598–603
Braun J, Sieper J (2002) Therapy of ankylosing spondylitis and other spondyloarthritides: established medical treatment, antiTNF-alpha therapy and other novel approaches. Arthritis Res 4:307–321
Doward LC (2003) Development of the ASQoL: a quality of life instrument specific to ankylosing spondylitis. Ann Rheum Dis 62(1):20–26
Jones SD, Steiner A, Garrett SL, Calin A (1996) The Bath Ankylosing Spondylitis Patient Global Score (BAS-G). Br J Rheumatol 35(1):66–71
Baeten D, Sieper J, Braun J, Baraliakos X, Dougados M, Emery P, Deodhar A, Porter B, Martin R, Andersson M, Mpofu S, Richards HB, MEASURE 1 Study Group, MEASURE 2 Study Group (2015) Secukinumab, an interleukin-17A inhibitor, in ankylosing spondylitis. N Engl J Med 373:2534–2548
Martin-Mola E, Sieper J, Leirisalo-Repo M et al (2010) Sustained efficacy and safety, including patient-reported outcomes, with etanercept treatment over 5 years in patients with ankylosing spondylitis. Clin Exp Rheumatol 28:238–245
Fernández-Carbadillo C, Navarro-Compán V, Castillo-Gallego C, Castro-Villegas MC, Collantes-Estévez E, de Miguel E et al (2017) Disease activity as a major determinant of quality of life and physical function in patients with early axial spondyloarthritis. Arthritis Care Res (Hoboken) 69(1):150–155
Almodóvar R, Zarco P, Collantes E, González C, Mulero J, Fernández-Sueiro JL, Gratacós J, Torres-Alonso JC, Juanola X, Batlle E, Ariza R, Muñoz E (2009) Relationship between spinal mobility and disease activity, function, quality of life and radiology. A cross-sectional Spanish registry of spondyloarthropathies (REGISPONSER). Clin Exp Rheumatol 27:439–445
Rudwaleit M, van der Heijde D, Landewé R, Listing J, Akkoc N, Brandt J (2009) The development of assessment of spondyloarthritis international society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis 68:777–783
Creemers MCW, Franssen MJAM, van’t Hof MA, Gribnau FWJ, van de Putte LBA, van Riel PLCM (2005) Assessment of outcome in ankylosing spondylitis: an extended radiographic scoring system. Ann Rheum Dis 64:127–129
Garrido-Castro JL, Medina Carnicer R, Schiottis R, Galisteo AM, Collantes-Estévez E, González-Navas C (2012) Assessment of spinal mobility in ankylosing spondylitis using a video-based motion capture system. Man Ther 17(5):422–426
Garrido-Castro JL, Escudero A, Medina-Carnicer R, Galisteo AM, Gonzalez-Navas C, Carmona L, Collantes-Estevez E (2014) Validation of a new objective index to measure spinal mobility: the University of Cordoba Ankylosing Spondylitis Metrology Index (UCOASMI). Rheumatol Int 34(3):401–406
Castro JL, Medina-Carnicer R, Galisteo AM (2006) Design and evaluation of a new three-dimensional motion capture system based on video. Gait Posture 24(1):126–129
Jenkinson TR, Mallorie PA, Whitelock HC, Kennedy LG, Garret SL, Calin A (1994) Defining spinal mobility in ankylosing spondylitis (AS). The Bath AS Metrology Index (BASMI). J Rheumatol 21:1694–1698
Calin A, Garrett S, Whitelock H, Kennedy LG, O’Hea J, Mallorie P et al (1994) A new approach to defining functional ability in ankylosing spondylitis: the development of the bath ankylosing spondylitis functional index. J Rheumatol 21:2281–2285
Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin (1994) A new approach to defining disease status in ankylosing spondylitis: the bath ankylosing spondylitis disease activity index. J Rheumatol 21:2286–2291
Lukas C, Landewé R, Sieper J, Dougados M, Davis J, Braun J, van der Linden S, van der Heijde D, Assessment of SpondyloArthritis international Society (2009) Development of an ASAS-endorsed disease activity score (ASDAS) in patients with ankylosing spondylitis. Ann Rheum Dis 68:18–24
Machado P, Landewé R, Lie E et al (2010) Ankylosing Spondylitis Disease Activity Score (ASDAS): defining cut-off values for disease activity states and improvement scores. Ann Rheum Dis (In Press)
Machado P, Landewé R, Braun J et al (2011) A stratified model for health outcomes in ankylosing spondylitis. Ann Rheum Dis 70:1758–1764
Jones SD, Koh WH, Steiner A, Garrett SL, Calin A (1996) Fatigue in ankylosing spondylitis: its prevalence and relationship to disease activity, sleep, and other factors. J Rheumatol 23:487–490
Ward MM, Learch TJ, Gensler LS, Davis JC, Reveille JD, Weisman MH (2013) Regional radiographic damage and functional limitations in patients with ankylosing spondylitis: differences in early and late disease. Arthritis Care Res 65(2):257–265
Ogzul A, Peker F, Taskaynatan MA, Tan AK, Dincer K, Kalyon TA (2006) Effect of ankylosing spondylitis on health-related quality of life and different aspects of social life in young patients. Clin Rheumatol 25(2):168–174
de Carvalho HM, Bortoluzzo AB, Gonçalves CR et al (2012) Gender characterization in a large series of Brazilian patients with spondyloarthritis. Clin Rheumatol 31:687–695
Webers C, Essers I, Ramiro S, Stolwijk C, Landewé R, van der Heijde D, van den Bosch F, Dougados M, van Tubergen A (2016) Gender-attributable differences in outcome of ankylosing spondylitis: long-term results from the outcome in ankylosing spondylitis international study. Rheumatology 55(3):419–428
Dagfinrud H, Vollestad NK, Loge JH, Kvien TK, Mengshoel AM (2005) Fatigue in patients with ankylosing spondylitis: a comparison with the general population and associations with clinical and self-reported measures. Arthritis Rheum 53:5–11
Salaffi F, De Angelis R, Carotti M, Gutierrez M, Sarzi-Puttini P, Atzeni F (2014 Aug) Fibromyalgia in patients with axial spondyloarthritis: epidemiological profile and effect on measures of disease activity. Rheumatol Int 34(8):1103–1110
Acknowledgments
The authors wish to thank all patients who participated in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Rights and permissions
About this article
Cite this article
López-Medina, C., Garrido-Castro, J.L., Castro-Jiménez, J. et al. Evaluation of quality of life in patients with axial spondyloarthritis and its association with disease activity, functionality, mobility, and structural damage. Clin Rheumatol 37, 1581–1588 (2018). https://doi.org/10.1007/s10067-018-4112-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-018-4112-4