Abstract
Systemic sclerosis (SSc) is an autoimmune disease which may lead to malnutrition. Previous studies have defined it with different criteria. No thorough evaluations of sarcopenia in SSc are available. The aim of the present study was to assess the prevalence and the potential association of malnutrition and sarcopenia in a large cohort of SSc cases. A total of 141 SSc consecutive outpatients were enrolled. Body composition was analyzed by densitometry. Malnutrition was defined according to recently published ESPEN criteria, whereas sarcopenia was diagnosed in patients with reduced skeletal muscle index. Malnutrition was diagnosed in 9.2% of patients (95% CI, 4.4–14.0%). Malnourished patients had worse gastrointestinal symptoms according to UCLA SCTC GIT 2.0 questionnaire (p = 0.007), lower physical activity (p = 0.028), longer disease duration (p = 0.019), worse predicted DLCO/VA and FVC (p = 0.009, respectively), worse disease severity according to Medsger severity score (p < 0.001), lower hemoglobin (p = 0.023), and fat-free mass (p < 0.001) and were more often sarcopenic (p < 0.001). In multivariate analysis, only FVC (p = 0.006) and disease severity (p = 0.003), in particular for the lungs (p = 0.013), were confirmed to be worse in malnourished patients. Sarcopenia was diagnosed in 29\140 patients (20.7%; 95% CI, 14.0–27.4%); 11\29 were also malnourished. In multivariate analysis, sarcopenic patients had longer disease duration (p = 0.049), worse DLCO/VA (p = 0.002), and lung (p = 0.006) and skin (p = 0.014) involvement. In SSc, malnutrition defined with ESPEN criteria was found to be lower than previously reported. Sarcopenia was found to be somewhat common. Lung involvement was significantly associated with nutritional status and may not be explained only by muscle weakness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic sclerosis (SSc) is a connective tissue disease characterized by vasculopathy, immune activation, and progressive fibrosis of the skin and internal organs such as the gastrointestinal (GI) tract, lungs, and kidneys. GI tract is often involved (i.e., in up to 90% of patients) [1] with no differences between diffuse and limited subset. Although it may affect each section of the GI tract, from the mouth to anus, the esophagus and small bowel are more often involved, with gastroesophageal reflux symptoms and constipation and bacterial overgrowth [2, 3].
Malnutrition is defined as “a state resulting from lack of uptake or intake of nutrition leading to altered body composition (decreased fat free mass) and body cell mass leading to diminished physical and mental function and impaired clinical outcome from disease” [4].
Some studies [5,6,7,8,9,10,11] investigated the prevalence of malnutrition, in SSc, which was shown to range between 5.3% [9] and 55.6% [6]. The reason for such a wide difference is that previous studies used different criteria to define malnutrition, mainly due to the lack of a diagnostic gold standard until recent years.
SSc patients may develop malnutrition for different reasons such as reduced caloric intake due to gastroesophageal symptoms, reduced motility of GI tract which causes nausea, vomiting and early satiety, impaired digestion for pancreatic insufficiency, and malabsorption attributable to fibrosis of bowel wall and bacterial overgrowth [12]. Also, mouth and tooth involvement may further reduce food intake [13].
Very little information is available about sarcopenia and SSc. Sarcopenia is a condition characterized by “progressive loss of muscle mass and strength with a risk of adverse outcomes such as disability, poor quality of life and death” [14]. Many pathophysiologic mechanisms have been identified for sarcopenia especially in elderly subjects. These include genetics, immobility, nutritional status, and decreased synthetic capacity of muscle with age termed “anabolic resistance,” which is favored by endocrine factors such as reduced production of testosterone, insulin, and insulin-like growth factor 1 [15]. A long disease duration was associated with a higher risk of sarcopenia in SSc [16].
The aim of this study was to assess the prevalence of malnutrition in a cohort of SSc patients as defined according to the 2015 European Society of Clinical Nutrition and Metabolism (ESPEN) criteria for malnutrition [17], which are now considered the diagnostic gold standard. Possible determinants of the malnutrition were also explored among those characterizing the disease and GI tract involvement, as evaluated by Medsger severity score [18], University of California, Los Angeles Scleroderma Clinical Trial Consortium Gastrointestinal Tract Instrument 2.0 (UCLA SCTC GIT 2.0) [19] questionnaire, along with fecal calprotectin as a marker of GI wall inflammation and bacterial overgrowth. The prevalence of sarcopenia in our SSc cohort and its correlations with the main clinical characteristics were also investigated.
Patients and methods
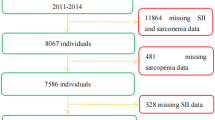
One-hundred and forty-one consecutive outpatients affected by SSc were enrolled between January and June 2016. We excluded patients who declined to provide a written informed consent, those with concomitant not-treated neoplastic disorders, and those receiving antibiotic treatment during the last month, as well as pregnant and breast feeding women.
All patients fulfilled the ACR criteria for the diagnosis of SSc [20]. The distinction between limited and diffuse cutaneous SSc was made according to LeRoy et al. criteria [21]. All patients underwent full clinical examination and laboratory testing including antinuclear and anti-ENA antibody detection by indirect immunofluorescence on HEp-2 cells and enzyme-linked immunosorbent assay (ELISA), respectively. Antibodies anti-RNA polymerase III (anti-RNAPIII) were also assessed with an immunoblot assay. Along with routine blood test, we also measured prealbumin and fecal calprotectin was measured using Quantum Blue® Calprotectin (BÜHLMANN Laboratories AG, Schönenbuch, Switzerland).
Skin involvement was assessed by modified Rodnan skin score (mRSS) [22]. Scleroderma disease was defined as active in agreement with Valentini et al. criteria [23]. Total Medsger severity scale [18] was applied with and without general item considering that the latter item also entails weight loss, so being a possible bias in the context of evaluating malnutrition. Medsger severity score was calculated for each item. Interstitial lung disease (ILD) was diagnosed by pulmonary high resolution computed tomography, whereas pulmonary artery hypertension (PAH) was defined by right hearth catheterization findings.
All patients underwent pulmonary function tests (PFT) with diffusing capacity for carbon monoxide adjusted for hemoglobin (DLCO) and evaluation of body composition by dual-energy X-ray absorptiometry (DXA) (GE Lunar iDXA) and dedicated software. Fat and free fat masses were recorded, and free fat mass index (FFMI), a height-adjusted assessment of fat-free mass, was finally calculated. Bone mineral density (BMD) was measured in all patients at the lumbar spine (L1–L4), at the total proximal femur, and at the femoral neck. The results were expressed as Z-score (SD below the age- and gender-matched mean reference value) so obtaining BMD adjustment for both sex and age.
Height at the time of evaluation was always measured using the same device. A weight history was collected and body mass index (BMI) was then calculated.
According to ESPEN criteria, patients were first screened using a validated tool. We used the Malnutrition Universal Screening Tool (MUST) [24] since it has been validated in outpatients and inpatients [25,26,27], displays high concordance with other screening tools [25], can be easily used [25], and was previously used in patients with SSc [5, 7, 10].
Malnutrition was then assessed according to ESPEN criteria [17]; malnutrition was defined when the BMI was < 18.5 kg/m2 (alternative 1) or in the presence of unintentional weight loss > 10% regardless of time or > 5% over the last 3 months combined with either BMI < 20 kg/m2 if < 70 years of age or < 22 kg/m m2 if > 70 years of age or FFMI < 15 and 17 kg/m2 in women and men, respectively (alternative 2).
Sarcopenia was evaluated using skeletal muscle mass index (SMI), i.e., appendicular skeletal muscle mass/height2 (kg\m2), with a cutoff of 7.26 kg\m2 for men and 5.50 kg\m2 for women as proposed by Baumgartner et al. [28].
To explore gastrointestinal symptoms, UCLA questionnaire [19] was administered.
Smoking history was recorded, ranking the patients in never, former, and active smokers. Alcohol intake was also calculated (unit\day) and physical activity was assessed with the Italian version of International Physical Activity Questionnaire (IPAQ) [29]. Drug treatment was also recorded; the dose of prednisone or equivalent was always < 10 mg/day and steroids were administered for arthralgias/arthritis in the majority of cases. All the investigations were performed within 3 months since enrollment.
The study was performed according to the Helsinki declaration and approved by Verona Medical School Institutional review board, with protocol number 18493. All patients provided written informed consent for participating the study.
Statistical analysis
Descriptive statistics were used to summarize patient characteristics. Continuous and normally distributed variables were expressed as mean (± standard deviation; SD), continuous and not normally distributed variables as median (and interquartile range; IQR), and categorical variable as absolute number (percentage).
The prevalence of malnutrition and sarcopenia was expressed as percentage (and 95% CI). Comparisons between groups were performed using t test, Mann-Whitey, or chi-square tests, when appropriate. The determinants of malnutrition and sarcopenia were explored with multivariate regression analysis including variables exhibiting a p value < 0.05 in univariate analysis, both with and without logarithmic transformation of those not normally distributed. Statistical analysis was performed by SPSS 17.0 (SPSS Inc., Chicago, IL).
Results
One-hundred and forty-one consecutive patients were enrolled. Table 1 summarizes the demographical and clinical characteristics. Female sex was predominant (84.4% of the cases); mean age was 63 ± 13 years and mean disease duration was 13.3 ± 7.2 years.
Most patients had a limited disease pattern (68.8%). Interstitial lung disease was found in 27.7% of cases and a history of digital ulcers was reported in 31.9% of cases.
According to Valentini et al. score [23], disease was found to be active in 19.1% of cases and the median total Medsger severity score was 5 ± 3.
GI symptoms were assessed according to UCLA questionnaire; 11.3% of the study population had severe symptoms, in particular emotive well-being (14.9%) and reflux (14.9%).
Twenty-nine patients (20.6%) were at moderate or high risk of malnutrition according to MUST screening. The prevalence of malnutrition established according to ESPEN criteria [17] was 9.2% (95% CI, 4.4–14.0%).
Table 2 summarizes the differences between patients with malnutrition and those with normal nutritional status. As expected, the former group of patients had lower BMI (18.3 vs. 24.9 kg/m2, p < 0.001), free fat mass index (13.6 vs. 16.2 kg/m2, p < 0.001), and whole body fat percentage (27.1 vs. 33.8%, p = 0.003). Sarcopenia was found to be more frequent in malnourished subjects (84.6 vs. 14.1% of cases; p < 0.001).
Malnourished patients had also longer disease duration (16 vs. 13 years, p = 0.019) and were more often treated with steroids (38.5 vs. 14.1%, p = 0.039).
The values of forced vital capacity (FVC), DLCO, and DLCO/alveolar volume (DLCO/VA) were found to be worse in malnourished patients compared to those non-malnourished (p = 0.009, p = 0.006, and p = 0.022, respectively). The absolute values of FVC and DLCO were lower in malnourished patients than in those non-malnourished (p = 0.009 and p = 0.022, respectively). Nevertheless, no significant differences could be observed as for the prevalence of interstitial lung disease and/or pulmonary arterial hypertension.
Blood tests revealed lower values of hemoglobin and estimated glomerular filtration rate (eGFR) in malnourished patients (12.1 vs. 13.2 g/dl, p = 0.023 and 70 vs. 87 ml/min/1.73 m2, p = 0.016, respectively).
Malnutrition patients had an unexpectedly lower alcohol intake (p = 0.034).
Although no significant differences could be found in disease activity, patients with malnutrition displayed worse Medsger severity score, even when considering the total score without general item (9 ± 5 vs. 5 ± 2, p < 0.001). Table 3 summarizes the Medsger score according to each item. The largest difference between malnourished patients and patients with normal nutritional condition was found for lung involvement. The GI score was also worse in malnourished than in non-malnourished patients.
Total UCLA score was higher in malnourished patients (0.589 ± 0.831 vs. 0.260 ± 0.544, p = 0.007). When comparing each single item, only emotional well-being was found to be statistically different, (0.880 ± 1.110 in malnourished cases vs. 0.110 ± 0.550 in patients with normal nutrition condition, p = 0.025).
Physical activity was significantly lower in patients with malnutrition than in controls. High physical activity was reported by 39.8% of non-malnourished subjects compared to 7.7% of malnourished cases (p = 0.031). Sarcopenia was significantly more frequent in malnourished than in non-malnourished patients (84.6 vs. 14.1% respectively, p < 0.001).
Two different multivariate models were carried out (Table 4). Both included all variables displaying a p value lower than 0.05 in univariate analysis (i.e., alcohol intake, steroid treatment, glomerular filtrate, disease duration). Model 1 also incorporated Medsger score (without general item), whereas model 2 included FVC and DLCO/VA, so precluding redundant information on pulmonary involvement. In the first model, only Medsger score (without general item) was found to be higher in malnourished patients. When the total score was replaced by each item, only lung severity was confirmed as statistically different between the two subgroups. In model 2, FVC and alcohol consumption were lower in malnourished patients.
For 140 patients, SMI was calculated and used to define sarcopenia. For the single patient excluded from our cohort, complete information about body composition was unavailable. Twenty-nine patients (20.7%, 95% CI 14.0–27.4%) had low SMI and 11 of these were also malnourished. SMI did not correlate with age, although it was considerably higher in men than in women (8.0 ± 0.8 vs. 6.3 ± 0.9%, p < 0.001, respectively). Sarcopenic patients had lower BMI (20.3 ± 2.5 vs. 25.5 ± 4.1 kg/m2, p < 0.001) and longer disease duration (16.3 ± 7.8 vs. 12.5 ± 6.8 years, p = 0.012) (Table 5). Predicted values of DLCO (56 ± 20 vs. 70 ± 20%, p = 0.004) and DLCO/VA (62 ± 19 vs. 78 ± 21%, p < 0.001) were lower in sarcopenic patients; FVC neither in absolute nor in predicted values was found to be different between groups.
Sarcopenic patients had higher Medsger severity score for the lungs (p = 0.004) and skin (p < 0.001). The Medsger severity total score with and without the general item was also found to be higher (p = 0.001 for both comparisons). Sarcopenic patients reported lower alcohol intake (p = 0.020). There was a trend towards lower physical activity in sarcopenic patients (p = 0.073), but this difference did not reach statistical significance.
In multivariate analysis including each Medsger item, alcohol intake, and disease duration, only longer disease duration and higher Medsger severity score for the lungs and skin were confirmed as independent risk factors for sarcopenia (p = 0.049, p = 0.006, and p = 0.014 respectively). The link between lung involvement and sarcopenia was confirmed in multivariate analysis when Medsger lung severity score was replaced by predicted DLCO/VA (p = 0.002).
Z-scores of BMD were significantly lower in malnourished patients both at the femur and spine (Table 2). After adjustment for smoking habit, vitamin D serum values, use of steroids and bisphosphonates, the lumbar Z-score remained significantly lower (p = 0.033) whereas the femur Z-score did not reach statistical significance (0.054). In sarcopenic patients, only lumbar Z-score was lower compared to non-sarcopenic patients (− 0.9 ± 1.3 vs. 0.2 ± 2, p = 0.002), even after adjustment for possible confounders (p < 0.001) (Table 5).
Discussion
Malnutrition is a possible complication of SSc, which may significantly contribute to increased mortality [6]. In this study, we found a 9.2% (95% CI, 4.4–14.0%) prevalence of malnutrition, as defined according to 2015 ESPEN criteria. Moreover, cases displayed worse GI symptoms evaluated by UCLA questionnaire, longer disease duration, lower hemoglobin values, lower FVC and lumbar Z-scores, higher Medsger severity score (especially for lung and GI involvement), and lower physical activity and were more frequently treated with steroids. In multivariate analysis, lower FVC or higher Medsger severity score for the lung remained associated with poorer nutritional status. In addition, most of malnourished patients were also sarcopenic (11, 91.7%). Sarcopenic patients had longer disease duration and worse predicted DLCO/VA and Medsger severity score, especially for the lungs and skin. No differences were found for FVC.
This is the first study in which the 2015 ESPEN [17] criteria have been used in SSc patients to the best of our knowledge. Only Spanjer et al. [11] have recently defined malnutrition according to ESPEN criteria, but with no previous screening, in contrast with what suggested by these guidelines. Interestingly, they found a prevalence of malnutrition very similar to ours (8.3 vs. 9.2%), but no analysis on possible determinants was done. These criteria are widely accepted for diagnosing malnutrition. A large variability of criteria used to define malnutrition in SSc patients can be found in other current scientific literatures (Table 6), so that the prevalence of malnutrition was found to be rather different, ranging from 5.3 to 55.6% [5,6,7,8,9,10]. This variability may also be explained by different cohort characteristics. In most of previous studies [5,6,7, 9], the patients enrolled had very severe disease, especially in terms of disease subset or lung involvement, whereas in the studies of Pavia’s group [8, 10], the GI symptoms were found to be milder (Medsger severity score ≥ 1 in 51 and 75%, respectively) and disease duration was shorter (5 ± 6 vs. 13.3 ± 7.3 years, respectively) than in our investigation. Nevertheless, they showed a prevalence of risk for malnutrition comparable with ours when using MUST and higher when malnutrition was defined on the basis of a BMI < 20 kg\m2 or weight loss of at least 10% in 6 months, further confirming that different criteria identify different populations.
We found that disease severity may impair nutritional status. This result was confirmed even when considering Medsger severity score without the general item, since this may be a bias in the final analysis because weight loss was found to be significantly different between groups. Only Baron et al. [5] and Caporali et al. [8] previously investigated the link between disease severity and malnutrition risk, reporting opposite findings. Baron et al. found that the global assessment of disease severity physicians was higher in malnourished patients, whereas Caporali et al. found no differences. Nevertheless, the population in the study of Caporali et al. had lower disease severity, which may hence be insufficient to influence nutrition. Lung involvement was probably the leading driver of such a correlation between disease severity and malnutrition in our patient cohort. Krause et al. [6] previously showed a reduced FVC in patients with malnutrition defined according to body composition at bioelectrical impedance analysis (BIA). In no other previous studies, PFT data were described. We hence underpin that only lung function defined by PFT and Medsger lung severity score (which is mainly based on PFT parameters) were found to be different between groups in our patient cohort, whereas no differences were found for ILD or PAH. Therefore, a link between malnutrition and muscle weakness can be hypothesized, so affecting the performance of PFT. Accordingly, we studied also sarcopenia in our SSc cohort, which was found to be more frequent in malnourished patients.
In a previous study by Marighela et al. [16], sarcopenia was defined by the same criterion used in our investigation. Although the overall prevalence was not described, the mean SMI value was similar to that obtained in our study (6.1 ± 1.1 kg\m2 vs. 6.3 ± 0.9 kg\m2 in our study). In accordance with our findings, the longer the disease duration, the higher was the risk of sarcopenia. An increased risk for sarcopenia in patients with higher Medsger score for the lungs and skin was also observed in our patients. Marighela et al. found that a higher mRSS was a risk factor for sarcopenia in univariate analysis. According to our data, and those earlier published by Marighela et al., disease duration and severity may be considered significant risk factors for low muscle mass. At EULAR 2017 meeting, March et al. [30] have reported a prevalence of sarcopenia in their 129-patient cohort somewhat higher than in ours (27.1 vs. 20.7%), but they used different diagnostic criteria. No other evidence on sarcopenia in SSc has ever been provided to the best of our knowledge.
Unlike findings in healthy subjects [31], the predicted FVC was not significantly different between sarcopenic and non-sarcopenic patients, and this is probably due to the fact that FVC was also influenced by the presence of lung disease. In our multivariate analysis, both ILD and malnutrition, but not sarcopenia, were found to be significant predictors of low FVC (data not shown).
Taken together, these data suggest that the reduced FVC in malnourished patients was not directly attributable to muscle weakness. The underlying association between reduced lung function and malnutrition may involve the catabolic state of malnourished patients, which may promote alveolar loss, so leading to a sort of emphysema with reduced gas exchange [32]. Another possible hypothesis is that lower FVC may be an index of more severe disease, so broadening its effects on body composition. Notably, none of the other possible markers of disease severity (e.g., skin and GI involvement) displayed a similar association.
In terms of survival, lung involvement is one of the leading causes of death in SSc [33]. Krause et al. [6] showed that abnormal body composition measured with BIA is associated with increased risk of death. It may hence be interesting to assess whether or not a thorough nutritional intervention may be effective to reduce mortality due to lung involvement.
Unlike some previous studies [5, 7, 9], multivariate analysis revealed that the GI involvement assessed with UCLA questionnaire and Medsger severity score was not found to be more severe in malnourished patients. A comparison with previous studies is challenging due to the different criteria used to define GI involvement. The results of the UCLA confirmed that our malnourished patients had a worse score for emotional well-being, suggesting a negative impact of malnutrition on quality of life.
Interestingly, although intestinal inflammation detected by the measurement of fecal calprotectin was not found to be a risk factor for malnutrition, this test is probably biased by the fact that malnutrition in SSc has a well-known multifactorial pathogenesis.
Rather unexpectedly, we also found that patients without malnutrition reported a higher alcohol intake. A possible explanation is that malnourished patients avoid alcoholic beverages, since these may contribute to worsen the GI symptoms.
The presence of osteoporosis in SSc is still a debated issue. We previously found that BMI is the leading cause of hip and whole body osteoporosis [34] and that the Z-score was lower in patients with lung involvement. In this more recent study, Z-scores at hip and spine were lower in malnourished patients, regardless of vitamin D status, that is well known to be often reduced in SSc patients [35, 36]. Besides mechanical stress (i.e., low BMI) and the degree of physical activity which may be strongly influenced by lung involvement, nutritional status is associated to BMD. This suggests that major attention should be focused on BMD and osteoporosis prevention/treatment in SSc patients with malnutrition.
Our study has many strengths. The ESPEN criteria were used for the first time to define malnutrition in the setting of SSc. Moreover, the collection of many parameters on SSc characteristics, body composition, and lifestyle allowed clarifying the main determinants and confounders of nutritional status. This is also the largest cohort study which has evaluated prevalence and determinants of sarcopenia in SSc.
The main limitations of this study are the observational design, so that a cause-effect relationship could not be accurately defined. Although patients underwent a thorough evaluation, no data about food intake could be collected. Nevertheless, previous studies failed to find that nutrition plays a leading role neither in malnutrition [8] nor in sarcopenia [16] in SSc.
In conclusion, we found that malnutrition defined according to ESPEN criteria is lower than previously reported and that sarcopenia is quite common. We also found an intriguing association between the lungs, both body composition and nutritional status. Further studies are warranted to assess variations of lung function and body composition over time and explore whether or not a therapeutic approach in malnutrition may have a favorable impact on survival.
References
Butt S, Emmanuel A (2013) Systemic sclerosis and gut. Expert Rev Gastroenterol Hepatol 7(4):331–339. https://doi.org/10.1586/egh.13.22
Akesson A, Gustafson T, Wollheim F, Brismar J (1987) Esophageal dysfunction and radionuclide transit in progressive systemic sclerosis. Scand J Rheumatol 16(4):291–299. https://doi.org/10.3109/03009748709102931
Sallam H, McNearney TA, Chen JD (2006) Systematic review: phatophysiology and management of gastrointestinal dysmotility in systemic sclerosis (scleroderma). Aliment Pharmacol Ther 23(6):691–712. https://doi.org/10.1111/j.1365-2036.2006.02804.x
Sobotka L (2012) Basics in clinical nutrition, 4th edn. Galen, Prague
Baron M, Hudson M, Steele R, Canadian scleroderma research group (2009) Malnutrition is common in systemic sclerosis: results from the Canadian scleroderma research group database. J Rheumatol 36(12):2737–2743. https://doi.org/10.3899/jrheum.090694
Krause L, Becker MO, Brueckner CS, Bellinghausen CJ, Becker C, Schneider U, Haeupl T, Hanke K, Hensel-Wiegel K, Ebert H, Ziemer S, Ladner UM, Pirlich M, Burmester GR, Riemekasten G (2010) Nutritional status as marker for disease activity and severity predicting mortality in patients with systemic sclerosis. Ann Rheum Dis 69(11):1951–1957. https://doi.org/10.1136/ard.2009.123273
Murtaugh M, Frech T (2013) Nutritional status and gastrointestinal symptoms in systemic sclerosis patients. Clin Nutr 32(1):130–135. https://doi.org/10.1016/j.clnu.2012.06.005
Caporali R, Caccialanza R, Bonino C, Klersy C, Cereda E, Xoxi B, Crippa A, Rava ML, Orlandi M, Bonardi C, Cameletti B, Codullo V, Montecucco C (2012) Disease-related malnutrition in outpatients with systemic sclerosis. Clin Nutr 31(5):666–671. https://doi.org/10.1016/j.clnu.2012.02.010
Rosato E, Gigante A, Gasperini ML, Molinaro I, Di Lazzaro Giraldi G, Afeltra A, Amoroso D, Salsano F, Rossi Fanelli F, Laviano A (2014) Nutritional status measured by BMI is impaired and correlates with left ventricular mass in patients with systemic sclerosis. Nutrition 30(2):204–209. https://doi.org/10.1016/j.nut.2013.07.025
Cereda E, Codullo V, Klersy C, Breda S, Crippa A, Rava ML, Orlandi M, Bonardi C, Fiorentini ML, Caporali R, Caccialanza R (2014) Disease-related nutritional risk and mortality in systemic sclerosis. Clin Nutr 33(3):558–561. https://doi.org/10.1016/j.clnu.2013.08.010
Spanjer MJ, Bultink IEM, de van der Schueren MAE, Voskuyl AE (2017) Prevalence of malnutrition and validation of bioelectrical impedance analysis for the assessment of body composition in patients with systemic sclerosis. Rheumatology 56(6):1008–1012. https://doi.org/10.1093/rheumatology/kex014
Gyger G, Baron M (2012) Gastrointestinal manifestations of scleroderma: recent progress in evaluation, pathogenesis, and management. Curr Rheumatol Rep 14(1):22–29. https://doi.org/10.1007/s11926-011-0217-3
Isola G, Williams RC, Lo Gullo A, Ramaglia L, Matarese M, Iorio-Siciliano V, Cosio C, Matarese G (2017) Risk association between scleroderma disease characteristics, periodontitis, and tooth loss. Clin Rheumatol 36(12):2733–2741. https://doi.org/10.1007/s10067-017-3861-9
Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, Abellan van Kan G, Andrieu S, Bauer J, Breuille D, Cederholm T, Chandler J, de Meynard C, Donini L, Harris T, Kannt A, Keime Guibert F, Onder G, Papanicolaou D, Rolland Y, Rooks D, Sieber C, Souhami E, Verlaan S, Zamboni M (2011) Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc 12(4):249–256. https://doi.org/10.1016/j.jamda.2011.01.003
Ali S, Garcia JM (2014) Sarcopenia, cachexia and aging: diagnosis, mechanisms and therapeutic options—a mini-review. Gerontology 60(4):294–305. https://doi.org/10.1159/000356760
Marighela TF, Genaro Pde S, Pinheiro MM, Szejnfeld VL, Kayser C (2013) Risk factors for body composition abnormalities in systemic sclerosis. Clin Rheumatol 32(7):1037–1044. https://doi.org/10.1007/s10067-013-2235-1
Cederholm T, Bosaeus I, Barazzoni R, Bauer J, Van Gossum A, Klek S, Muscaritoli M, Nyulasi I, Ockenga J, Schneider SM, de van der Schueren MAE, Singer P (2015) Diagnostic criteria for malnutrition: an ESPEN consensus statement. Clin Nutr 34(3):335–340. https://doi.org/10.1016/j.clnu.2015.03.001
Medsger TA, Bombardieri S, Czirjak L, Scorza R, Della Rossa A, Bencivelli W (2003) Assessment of disease severity and prognosis. Clin Exp Rheumatol 21(3 suppl 29):S42–S46
Khanna D, Hays RD, Maranian P, Seibold JR, Impens A, Mayes MD, Clements PJ, Getzug T, Fathi N, Bechtel A, de Furst (2009) Reliability and validity of UCLA Scleroderma Clinical Trial Consortium Gastrointestinal Tract (UCLA SCTC GIT 2.0) instrument. Arthritis Rheum 61(9):1257–1263. https://doi.org/10.1002/art.24730
van den Hoogen F, Khanna D, Fransen J, Johnson SR, Baron M, Tyndall A, Matucci-Cerinic M, Naden RP, Medsger TA Jr, Carreira PE, Riemekasten G, Clements PJ, Denton CP, Distler O, Allanore Y, de Furst, Gabrielli A, Mayes MD, van Laar JM, Seibold JR, Czirjak L, Steen VD, Inanc M, Kowal-Bielecka O, Müller-Ladner U, Valentini G, Veale DJ, Vonk MC, Walker UA, Chung L, Collier DH, Ellen Csuka M, Fessler BJ, Guiducci S, Herrick A, Hsu VM, Jimenez S, Kahaleh B, Merkel PA, Sierakowski S, Silver RM, Simms RW, Varga J, Pope JE (2013) 2013 classification criteria for systemic sclerosis: an American college of rheumatology/European league against rheumatism collaborative initiative. Ann Rheum Dis 72(11):1747–1755. https://doi.org/10.1136/annrheumdis-2013-204424
LeRoy EC, Black CM, Fleischmajer R, Jablonska S, Krieg T, Medsger TA Jr et al (1988) Scleroderma (systemic sclerosis): classification, subsets and pathogenesis. J Rheumatol 15(2):202–205
Akesson A, Fiori G, Krieg T, van den Hoogen FHJ, Seibold JR (2002) Assessment of skin, joint, tendon and muscle involvement. Clin Exp Rheumatol 21(3 suppl 29):S5–S8
Valentini G, Della Rossa A, Bombardieri S, Bencivelli W, Silman AJ, D'Angelo S, Cerinic MM, Belch JF, Black CM, Bruhlmann P, Czirják L, de Luca A, Drosos AA, Ferri C, Gabrielli A, Giacomelli R, Hayem G, Inanc M, McHugh NJ, Nielsen H, Rosada M, Scorza R, Stork J, Sysa A, van den Hoogen FH, Vlachoyiannopoulos PJ (2001) European multicentre study to define disease activity criteria for systemic sclerosis. II. Identification of disease activity variables and development of preliminary activity indexes. Ann Rheum Dis 60(6):592–598. https://doi.org/10.1136/ard.60.6.592
Elia M (2003) Screening for malnutrition: a multidisciplinary responsibility. Development and use of the ‘malnutrition universal screening tool’ (‘MUST’) for adults. Malnutrition Advisory Group (MAG), a standing committee of BAPEN Redditch, Worcs
Stratton RJ, Hackston A, Longmore D, Dixon R, Price S, Stroud M, King C, Elia M (2004) Malnutrition in hospital outpatients and inpatients: prevalence, concurrent validity and ease of use of the ‘malnutrition universal screening tool’ (‘MUST’) for adults. Br J Nutr 92(05):799–808. https://doi.org/10.1079/BJN20041258
Neelemaat F, Meijers J, Kruizenga H, van Ballegooijen H, van Bokhorst-de van der Schueren M (2011) Comparison of five malnutrition screening tools in one hospital inpatient sample. J Clin Nurs 20(15-16):2144–2152. https://doi.org/10.1111/j.1365-2702.2010.03667.x
Leistra E, Langius JA, Evers AM, van Bokhorst-de van der Schueren MA, Visser M, de Vet HC et al (2013) Validity of nutritional screening with MUST and SNAQ in hospital outpatients. Eur J Clin Nutr 67(7):738–742. https://doi.org/10.1038/ejcn.2013.85
Baumgartner R, Koehler K, Gallagher D, Romero L, Heymsfield SB, Ross RR et al (1998) Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 147(8):755–763. https://doi.org/10.1093/oxfordjournals.aje.a009520
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE et al (2003) International Physical Activity Questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35(8):1381–1395. https://doi.org/10.1249/01.MSS.0000078924.61453.FB
March C, Siegert E, Preis E, Makowka A, Buttgereit F, Riemekasten G et al (2017) Prevalence of sarcopenia in patients with systemic sclerosis according to the revised criteria of the european working group on sarcopenia in older people. Ann Rheum Dis 15:897–898
Schweitzer L, Geisler C, Johannsen M, Glüer CC, Müller MJ (2017) Associations between body composition, physical capabilities and pulmonary function in healthy older adults. Eur J Clin Nutr 71(3):389–394. https://doi.org/10.1038/ejcn.2016.146
Massaro D, Massaro GD (2004) Hunger disease and pulmonary alveoli. Am J Respir Crit Care Med 170(7):723–724. https://doi.org/10.1164/rccm.2408002
Tyndall AJ, Bannert B, Vonk M, Airò P, Cozzi F, Carreira PE et al (2010) Causes and risk factors for death in systemic sclerosis: a study from the EULAR Scleroderma Trials and Research (EUSTAR) database. Ann Rheum Dis 69(10):1809–1815. https://doi.org/10.1136/ard.2009.114264
Caimmi C, Caramaschi P, Barausse G, Orsolini G, Idolazzi L, Gatti D, Viapiana O, Adami S, Biasi D, Rossini M (2016) Bone metabolism in a large cohort of patients with systemic sclerosis. Calcif Tissue Int 99(1):23–29. https://doi.org/10.1007/s00223-016-0119-5
Caramaschi P, Dalla Gassa A, Ruzzenente O, Volpe A, Ravagnani V, Tinazzi I, Barausse G, Bambara LM, Biasi D (2010) Very low levels of vitamin D in systemic sclerosis patients. Clin Rheumatol 29(12):1419–1425. https://doi.org/10.1007/s10067-010-1478-3
Giuggioli D, Colaci M, Cassone G, Fallahi P, Lumetti F, Spinella A, Campomori F, Manfredi A, Manzini CU, Antonelli A, Ferri C (2017) Serum 25-OH vitamin D levels in systemic sclerosis: analysis of 140 patients and review of the literature. Clin Rheumatol 36(3):583–590. https://doi.org/10.1007/s10067-016-3535-z
Funding
This work had no funds.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was performed according to the Helsinki declaration and approved by Verona Medical School Institutional review board, with protocol number 18493. All patients provided written informed consent for participating the study.
Disclosures
None.
Rights and permissions
About this article
Cite this article
Caimmi, C., Caramaschi, P., Venturini, A. et al. Malnutrition and sarcopenia in a large cohort of patients with systemic sclerosis. Clin Rheumatol 37, 987–997 (2018). https://doi.org/10.1007/s10067-017-3932-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-017-3932-y