Abstract
The aim of this study was to investigate the utility of red blood cell distribution width (RDW) as a simple and readily available marker of occurrence of pulmonary arterial hypertension (PAH) in patients with systemic sclerosis (SSc). One hundred and forty-five consecutive patients with SSc were recruited to the single-center cross-sectional study. Demographic characteristics, hematological parameters, Modified Rodnan Skin Score, and World Health Organization functional classification were determined. Diagnosis of PAH was based on screening by echocardiography and was confirmed by right heart catheterization. Interstitial lung disease (ILD) was diagnosed based on chest high-resolution computed tomography findings. There were no significant differences in gender, age, or disease duration between limited and diffused SSc groups. PAH was detected in 28 of lcSSc (33.3%) and 14 of dcSSc (23.0%) subjects. Patients with higher RDW values were more likely to be men with high anti-u1RNP titers and PAH. A significant correlation was found between RDW and high-sensitivity C-reactive protein (p = 0.375, p < 0.01) and the diffusing capacity of the lungs for carbon monoxide (ρ = − 0.396, p < 0.01). The SSc-PAH group had significantly higher RDW values compared to the SSc group without pulmonary disease (15.7 ± 2.2 and 13.7 ± 1.0, p < 0.001). The mean RDW in the SSc-PAH-ILD group was significantly higher than that in the SSc-ILD group (16.3 ± 2.2% and 14.0 ± 1.5%, p < 0.001). Besides the recognized risk factors, high RDW was an independent predictor of PAH in patients with SSc (OR = 3.314 [95%CI 1.038–10.580], p < 0.05). RDW may be a related factor for identifying the pulmonary arterial hypertension in SSc patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pulmonary arterial hypertension (PAH) is a leading cause of death in patients with both limited and diffuse systemic sclerosis (SSc). Through screening echocardiography, approximately 15–30% of these patients will develop PAH during their lifetime [1, 2]. Despite advances in treatment options for PAH, long-term prognosis remains poor for SSc-associated PAH (SSc-PAH). Earlier detection and intervention may have a favorable effect on the management of patients with SSc-PAH; however, there are no pathognomonic features that easily identify SSc-PAH. Identification of risk factors or predictors of the development of PAH in individuals with SSc would allow earlier diagnosis and introduction of specific therapy for PAH at a time when it is most likely to be effective.
Red blood cell distribution width (RDW) is one of the RBC indices, which quantifies variation in circulating red blood cell size, pointing to the degree of anisocytosis in the complete blood count. It is an automated measure that is performed routinely as part of a complete blood cell count. Besides iron-deficiency anemia, thalassemia, and myelodysplastic syndrome, elevated RDW can be indicative of inflammation and nutritional deficiencies, pulmonary impairment [3], and renal failure [4]. Some previous studies have shown its usefulness as an adverse prognostic marker in patients with cardiovascular disease [5, 6], particularly those with left heart failure. Furthermore, increased RDW has been reported to be independently associated with death in patients with idiopathic PAH [7, 8]. A recent study demonstrated that higher RDW levels may be correlated with worsening of cardiopulmonary manifestations in patients with SSc [9]. No study to date has examined the association of RDW with PAH in SSc patients.
We hypothesized that elevated RDW levels may be associated with PAH in both diffuse and limited SSc patients and may serve as a potent predictor of this complication. The aim of this single-center, cross-sectional study was to investigate the utility of RDW as a simple and readily available associated factor of PAH in SSc patients.
Materials and methods
Study population
Patients diagnosed with SSc (according to the ACR criteria) [10] who were admitted to the Rheumatology Division of Peking Union Medical College Hospital (PUMCH) from May 2008 to April 2012 were included. The limited (lcSSc) and diffuse (dcSSc) SSc subsets were based on the extent of skin involvement [11]. Patients with renal insufficiency, previous evidence of clinically relevant left heart disease, cerebrovascular diseases, pernicious anemia, malnutrition, blood transfusion, or systemic inflammatory response syndrome were excluded. Renal insufficiency is defined as serum creatinine greater than 1.5 mg/dL in men and greater than 1.2 mg/dL in women. Malnutrition is defined as body mass index lower than 18.5 kg/m2. The study was approved by the medical ethics committee of Peking Union Medical College Hospital and was conducted in accordance with the Declaration of Helsinki principles and followed the International Conference on Harmonisation Guideline for Good Clinical Practice. Written informed consent was obtained from all the patients.
Data collection
Demographic characteristics and comorbid conditions were recorded at baseline. Hematological parameters, including complete blood count, RDW, mean cell volume, hematocrit (HCT), creatinine (Cr), and blood urea nitrogen (BUN), were measured using an automatic hematology system. The normal reference range for RDW is 11–14.6% in our laboratory. In addition, erythrocyte sedimentation rate (ESR), high-sensitivity C-reactive protein (hsCRP), anti-nuclear antibody (ANA), anti-u1RNP, anti-DNA topoisomerase (anti-topo I), and anti-centromere antibody (ACA) were measured. Modified Rodnan Skin Score (MRSS), as well as the 6-min walk distance (6MWD) and World Health Organization (WHO) functional classification, was determined on the same day as blood sample collection.
Each SSc patient underwent high-resolution CT (HRCT) scan of the lungs and pulmonary function tests for the evaluation of ILD. Pulmonary function tests [forced vital capacity (FVC%) percent predicted, total lung capacity (TLC%) percent predicted, and diffusion capacity (DLCO%) percent predicted] were obtained according to standard procedures. ILD was diagnosed based on chest HRCT findings including ground-glass opacities, honeycombing, septal thickening, irregular linear opacities, traction bronchiectasis, and bronchiolectasis [12, 13]. FVC 50–70% of predicted and FEV1/FVC ≥ 0.7 on spirometry were defined as a moderate restrictive pattern, and FVC < 50% of predicted was defined as severe restriction.
Echocardiography was performed on all patients according to the standards of the American Society of Echocardiography by experienced cardiologists (who were blinded to the study protocol). If an estimated systolic pulmonary arterial pressure (sPAP) ≥ 36 mmHg was measured by echocardiography, patients would undergo right heart catheterization (RHC). Various hemodynamic parameters, including pulmonary arterial pressure (PAP), pulmonary arterial wedge pressure (PAWP), cardiac outputs (CO), and pulmonary vascular resistance (PVR), were measured according to the clinical guidelines [14]. According to the 2015 European Society of Cardiology/European Respiratory Society guidelines, PAH is defined as mean pulmonary artery pressure ≥ 25 mmHg at rest, pulmonary artery wedge pressure ≤ 15 mmHg, and pulmonary vascular resistance (PVR) > 3 Wood units, as assessed by RHC. Exclusion criteria were evidence of pulmonary venous hypertension (pulmonary capillary wedge pressure > 15 mmHg) and chronic thromboembolic disease.
Statistical analysis
Continuous variables were expressed as mean ± SD or medians (interquartile ranges), and categorical variables as numbers and percentages. The distribution of values was assessed using the Kolmogorov-Smirnov test. Continuous and categorical characteristics were compared using Student’s t test and Fischer’s exact test, respectively.
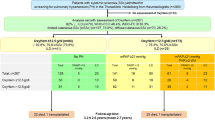
Patients were stratified according to the tertiles of RDW levels (< 13.6, 13.6–14.6, and > 14.6%) and clinically relevant differences were evaluated by the Kruskal-Wallis analysis of variance (ANOVA) test or the Fischer’s exact test, as appropriate. The receiver operating characteristic (ROC) curve analysis was used to assess the predictive value of the RDW. The ROC area under the curve (AUC) formed the criterion for assessing the discriminatory ability of the model.
To explore which factors were most influential in SSc associated with PAH, logistical regression with stepwise selection was used. Correlations between RDW and the other laboratory and hemodynamic variables were determined using Spearman’s correlation coefficient. A p < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS statistics version 22.0 (IBM, Armonk, NY, USA).
Results
Demographics and clinical characteristics
One hundred and fifty consecutive patients with SSc were recruited to the study; five patients were excluded from the analysis because of incomplete clinical data. The remaining 145 patients were analyzed. Demographic data and general clinical manifestations are shown in Table 1. The mean age of patients with SSc was 43.6 ± 11.5 years. There were no significant differences in gender, age, disease duration, BMI, or antibody profiles between lcSSc and dcSSc groups. PAH was detected in 28 of lcSSc (33.3%) and 14 of dcSSc (23.0%) subjects.
Clinical characteristics of patients according to the tertile of RDW are presented in Table 2. Patients with higher RDW values were more likely to be men, have a significantly higher titer of anti-u1RNP and PAH, and a lower titer of anti-topoisomerase I antibodies.
RDW and inflammatory markers
Notably, there were strong, graded increases in ESR and hsCRP across RDW tertiles; both parameters were up to twofold higher in the highest tertile versus those in the lowest tertile of RDW (Table 2). A significant correlation was found between RDW and hsCRP (p = 0.375, p < 0.01).
RDW and respiratory markers
The patients in the highest RDW tertile (> 14.6%) had the lowest DLCO% compared to patients in the normal range (13.6–14.6%) and in the lowest tertile (< 13.6%) (Table 2). The DLCO showed a negative correlation with RDW at baseline (ρ = − 0.396; p = 0.000).
RDW in different lung impairment in SSc patients
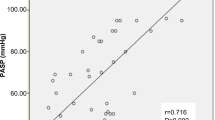
Comparison of RDW values between the four groups of SSc patients stratified according to the degree of lung impairment is shown in Fig. 1. SSc patients with PAH had significantly higher RDW values compared to SSc patients without pulmonary disease (15.7 ± 2.2% vs 13.7 ± 1.0%, p < 0.001). The mean RDW values were significantly higher in the SSc-PAH-ILD group, compared with the SSc-ILD group: 16.3 ± 2.2% and 14.0 ± 1.5%, respectively (p < 0.001). There was no significant difference between patients with SSc-ILD and SSc without pulmonary impairment (14.0 ± 1.5% vs 13.7 ± 1.0%, p = 0.570).
RDW percentage in various groups of SSc patients. Box plots of the percentage of RDW for 18 patients with SSc without pulmonary disease, 86 patients with SSc-ILD without PAH, 18 patients with SSc-PAH without ILD, and 23 patients with SSc with PAH and ILD. RDW, red blood cell distribution width. Circles indicate mild; the asterisk indicates extreme outlier values
Association of RDW and PAH in SSc patients
The ROC curve showed that RDW was a significant indicator of PAH in SSc patients (p < 0.001); the AUC of the RDW was 0.816 (95%CI 0.744, 0.889). The optimal RDW cutoff point was 14.3% with a sensitivity of 78.6% and specificity of 69.9% (Fig. 2).
Multivariable logistic regression analysis is shown in Table 3. Besides the well-known risk factors associated with PAH in SSc, such as anti-u1RNP and FVC%/DLCO%, the presence of high RDW was an independent risk factor that indicated PAH in patients with SSc (odds ratio, 3.314 [95%CI 1.038–10.580], p = 0.043).
There was a declining trend in DLCO% and 6MWD across the RDW tertile, with the highest tertile of RDW having significantly lower DLCO% and 6MWD (Table 2). None of the invasive hemodynamic variables were associated with RDW tertile; however, we did find a moderate negative correlation between RDW and cardiac output (CO) (ρ = − 0.318, p = 0.031). RDW was negatively correlated with the 6MWD (ρ = − 0.276, p = 0.001).
Discussion
RDW is a quantitative measurement in the size of circulating red blood cells (anisocytosis) and is routinely reported by automated laboratory equipment in complete blood counts. In a prospective study of 145 patients, we found an independent, strong association between RDW level and the development of PAH in both diffuse and limited systemic sclerosis patients, even after adjusting for other potential confounder. In addition to reaching statistical significance, the magnitude of the increased risk associated with higher RDW levels was clinically relevant.
Hampole et al. were the first to report that increased RDW was a strong independent prognostic indicator for pulmonary hypertension (PH) [7]. In this prospective study of 162 PH patients, higher RDW was independently associated with mortality and was a better prognostic indicator than NT-pro-BNP. A recent study has found that an increase in RDW may indicate worsening of cardiopulmonary manifestations in patients with SSc [9]. A statistically significant inverse correlation was found between DLCO and RDW levels. The results of the present study confirmed and extended these findings in a population of SSc patients with pulmonary impairment. Furthermore, to the best of our knowledge, our study is the first to show that increased RDW indicates PAH in patients with SSc, independently of other risk factors, such as anti-centromere antibody and FVC%/DLCO% [15, 16] which were proved by the first multinational prospective evidence-based PAH screening study, the DETECT study.
The reason for the strong association of RDW and PAH in SSc is not well understood. Several potential mechanisms may account for the association of RDW with PAH, because RDW level may simply serve as an integrative measure of multiple pathological processes simultaneously occurring in SSc-PAH patients, including ineffective erythropoiesis, oxidative stress, thrombosis, inflammation, endothelial dysfunction [17, 18], and nutritional deficiencies. Similar to other previous studies [7, 19], an association between increasing RDW and elevated levels of acute phase reactants, including ESR and high-sensitivity C-reactive protein, was confirmed in this study, suggesting that elevated RDW may reflect an underlying inflammatory state that is associated with adverse outcomes. Furthermore, the increased RDW levels may also represent a procoagulant activity of red blood cells independent of inflammation; the elevated RDW may reflect an increased complement of immature reticulocytes. The reduction of red blood cell deformability may stimulate platelet aggregation, leading to vascular compromise and impaired blood viscosity. Variable red blood cell size, decreased deformability, and increased adhesion may lead to a thrombophilic state and develop thrombosis [20]. Those processes create disequilibrium between the vasoactive, proliferative mediators (e.g., thromboxane A2 and endothelin-1), and anti-proliferative vasodilators (e.g., nitric oxide and prostacyclin) within the endothelium. At the same time, hypoxemia occurs, and ischemia reperfusion injury in the pulmonary vasculature promotes vascular remodeling, fibroblast proliferation, and intraluminal microthrombosis. The end result is a progressive increase in pulmonary vascular resistance, PAP, and right ventricular pressure overload [21]. These data from the literature and the novel observations of this study help us to understand why RDW is a useful indicator of PAH in SSc patients.
Testing for RDW values is an affordable method for screening for PAH in SSc patients. Modern hemogram devices automatically measure the size of red blood cells and analyze their distribution volume. As part of the complete blood count, RDW is widely available to clinicians and incurs no additional costs; in contrast to the other novel markers of PAH, these findings are notable.
The strengths of our study include its relatively large size and the use of the gold standard diagnosis of PAH [14], right heart catheterization. However, some study limitations should be considered in the interpretation of the results. The present study was a single-center cross-sectional study; therefore, the present analysis was limited in its ability to establish causal or temporal relationships between RDW and the development of PAH. A prospective cohort study with a larger sample size and other influencing factors may prove to be more useful in evaluating the role of RDW in the early diagnosis of PAH among SSc patients. Although there is growing evidence that RDW is independently associated with PAH in SSc patients, additional studies should be performed to improve understanding of pathophysiology and to determine the underlying factors that affect RDW.
In conclusion, this study confirmed our hypothesis that RDW could be an associated factor of PAH in SSc patients. Because RDW is routinely reported as part of the complete blood count and no additional cost is involved, this measure is readily available for most patients in different clinics or hospitals. Finally, understanding its significance will be helpful in identifying the risk of PAH in SSc patients.
References
Steen VD, Medsger TA (2007) Changes in causes of death in systemic sclerosis, 1972–2002. Ann Rheum Dis 66(7):940–944. https://doi.org/10.1136/ard.2006.066068
Mukerjee D, St George D, Coleiro B, Knight C, Denton CP, Davar J, Black CM, Coghlan JG (2003) Prevalence and outcome in systemic sclerosis associated pulmonary arterial hypertension: application of a registry approach. Ann Rheum Dis 62(11):1088–1093. https://doi.org/10.1136/ard.62.11.1088
Subhashree AR, Shanthi B, Parameaswari PJ (2013) The red cell distribution width as a sensitive biomarker for assessing the pulmonary function in automobile welders—a cross sectional study. J Clin Diagn Res 7(1):89–92. https://doi.org/10.7860/JCDR/2012/5051.2678
Ujszaszi A, Molnar MZ, Czira ME, Novak M, Mucsi I (2013) Renal function is independently associated with red cell distribution width in kidney transplant recipients: a potential new auxiliary parameter for the clinical evaluation of patients with chronic kidney disease. Br J Haematol 161(5):715–725. https://doi.org/10.1111/bjh.12315
Felker GM, Allen LA, Pocock SJ, Shaw LK, McMurray JJ, Pfeffer MA, Swedberg K, Wang D, Yusuf S, Michelson EL, Granger CB, CHARM Investigators (2007) Red cell distribution width as a novel prognostic marker in heart failure: data from the CHARM Program and the Duke Databank. J Am Coll Cardiol 50(1):40–47. https://doi.org/10.1016/j.jacc.2007.02.067
Tonelli M, Sacks F, Arnold M, Moye L, Davis B, Pfeffer M, for the Cholesterol and Recurrent Events (CARE) Trial Investigators (2008) Relation between red blood cell distribution width and cardiovascular event rate in people with coronary disease. Circulation 117(2):163–168. https://doi.org/10.1161/CIRCULATIONAHA.107.727545
Hampole CV, Mehrotra AK, Thenappan T, Gomberg-Maitland M, Shah SJ (2009) Usefulness of red cell distribution width as a prognostic marker in pulmonary hypertension. Am J Cardiol 104(6):868–872. https://doi.org/10.1016/j.amjcard.2009.05.016
Rhodes CJ, Wharton J, Howard LS, Gibbs JS, Wilkins Red MR (2011) Cell distribution width outperforms other potential circulating biomarkers in predicting survival in idiopathic pulmonary arterial hypertension. Heart 97(13):1054–1060. https://doi.org/10.1136/hrt.2011.224857
Farkas N, Szabo A, Lorand V, Sarlos DP, Minier T, Prohaszka Z, Czirjak L, Varju C (2014) Clinical usefulness of measuring red blood cell distribution width in patients with systemic sclerosis. Rheumatology (Oxford) 53(8):1439–1445. https://doi.org/10.1093/rheumatology/keu022
Subcommittee for scleroderma criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee (1980) Preliminary criteria for the classification of systemic sclerosis (scleroderma). Arthritis Rheum 23:581–590
LeRoy EC, Black C, Fleischmajer R, Jablonska S, Krieg T, Jr Medsger TA et al (1988) Scleroderma (systemic sclerosis): classification, subsets and pathogenesis. J Rheumatol 15(2):202–205
Khanna D, Nagaraja V, Tseng CH et al (2015) Predictors of lung function decline in scleroderma-related interstitial lung disease based on high-resolution computed tomography: implications for cohort enrichment in systemic sclerosis-associated interstitial lung disease trials. Arthritis Res Ther 17(1):372. https://doi.org/10.1186/s13075-015-0872-2
Wells AU, Hansell DM, Corrin B, Harrison NK, Goldstraw P, Black CM, du Bois RM (1992) High resolution computed tomography as a predictor of lung histology in systemic sclerosis. Thorax 47(9):738–742. https://doi.org/10.1136/thx.47.9.738
Authors/Task Force, M, Galie N, Humbert M, Vachiery JL, Gibbs S, Lang I et al (2015) 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS) Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J 37(1):67–119. https://doi.org/10.1093/eurheartj/ehv317
Plastiras SC, Karadimitrakis SP, Kampolis C, Moutsopoulos HM, Tzelepis GE (2007) Determinants of pulmonary arterial hypertension in scleroderma. Semin Arthritis Rheum 36(6):392–396. https://doi.org/10.1016/j.semarthrit.2006.10.004
Coghlan JG, Denton CP, Grunig E, Bonderman D, Distler O, Khanna D et al (2014) Evidence-based detection of pulmonary arterial hypertension in systemic sclerosis: the DETECT study. Ann Rheum Dis 73(7):1340–1349. https://doi.org/10.1136/annrheumdis-2013-203301
Solak Y, Yilmaz MI, Saglam M, Caglar K, Verim S, Unal HU et al (2014) Red cell distribution width is independently related to endothelial dysfunction in patients with chronic kidney disease. Am J Med Sci 347(2):118–124. https://doi.org/10.1097/MAJ.0b013e3182996a96
Fatini C, Mannini L, Sticchi E, Rogai V, Guiducci S, Conforti ML, Cinelli M, Pignone AM, Bolli P, Abbate R, Cerinic MM (2006) Hemorheologic profile in systemic sclerosis: role of NOS3 -786T > C and 894G >T polymorphisms in modulating both the hemorheologic parameters and the susceptibility to the disease. Arthritis Rheum 54(7):2263–2270. https://doi.org/10.1002/art.21933
Lippi G, Targher G, Montagnana M, Salvagno GL, Zoppini G, Guidi GC (2009) Relation between red blood cell distribution width and inflammatory biomarkers in a large cohort of unselected outpatients. Arch Pathol Lab Med 133(4):628–632. https://doi.org/10.1043/1543-2165-133.4.628
Rezende SM, Lijfering WM, Rosendaal FR, Cannegieter SC (2014) Hematologic variables and venous thrombosis: red cell distribution width and blood monocyte count are associated with an increased risk. Haematologica 99(1):194–200. https://doi.org/10.3324/haematol.2013.083840
Lambova S, Muller-Ladner U (2010) Pulmonary arterial hypertension in systemic sclerosis. Autoimmun Rev 9(11):761–770. https://doi.org/10.1016/j.autrev.2010.06.006
Acknowledgements
This study was supported by EULAR Scleroderma Trial and Research (EUSTAR) Group, National Major Scientific and Technological Special Project (2012ZX09303006-002), Chinese National Key Technology R&D Program, Ministry of Science and Technology (2011BAI11B15), National Natural Science Foundation of China (81072485, 81071300, 81500306), Research Special Fund for Public Welfare Industry of Health (201202004), Fund of Capital Medical Development and Research (2009-2003), Clinical Research Project of Chinese Medical Association (12040740374) and Peking Union Medical College (PUMC) Youth Fund, and the Fundamental Research Funds for the Central Universities.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the medical ethics committee of Peking Union Medical College Hospital and was conducted in accordance with the Declaration of Helsinki principles and followed the International Conference on Harmonisation Guideline for Good Clinical Practice. Written informed consent was obtained from all the patients.
Disclosures
None.
Rights and permissions
About this article
Cite this article
Zhao, J., Mo, H., Guo, X. et al. Red blood cell distribution width as a related factor of pulmonary arterial hypertension in patients with systemic sclerosis. Clin Rheumatol 37, 979–985 (2018). https://doi.org/10.1007/s10067-017-3918-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-017-3918-9