Abstract
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease in which pathogenesis oxidative stress has an important role. Single nucleotide polymorphisms (SNPs) in the genes that code enzymes involved in the antioxidative defense are possible factors that are responsible for their decreased activity of antioxidative defense enzymes. Thus, the aim of the study was to examine association of SNPs in these genes with SLE. A total of176 subjects were involved in this study. CAT A-21T (rs7943316), CAT C-262T (rs1001139) and manganese SOD (MnSOD) Ala16Val (rs4880) SNPs were determined using PCR-RFLP method, while GSTT1 and GSTM1 were determined using multiplex PCR. The obtained results showed significant differences in the distribution of genotypes (df = 2; p = 0.001) and alleles (p < 0.001; OR = 2.227; 95% CI = 1.429–3.741) of rs4880 between patients and controls. MnSODValVal genotype showed association with neurologic manifestations (p = 0.016; OR = 6.7; 95% CI = 1.18–37.89), while homozygous GSTT1 showed association with musculoskeletal manifestations of SLE (p = 0.008; OR = 4.168; 95% CI = 1.364–12.737). AlaVal/T+M+ genotype combination is a high-risk genotype for SLE. SNP–SNP interaction model showed positive correlation between CAT A-21T and CAT C-262T SNPs in SLE patients which was not influenced by the linkage disequilibrium (r 2 = 0.005; D′ = 0.071). MnSODVal allele is a risk factor for SLE, as well as for SLE with neurologic manifestations, while homozygous GSTT1 genotype is a risk factor for SLE with musculoskeletal manifestations. Catalase SNPs (C-262T and A-21T) show positive correlation in the model of SNP–SNP interaction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is a chronic multisystemic disease of the autoimmune origin, which predominantly occurs in women. The clinical presentation of the disease includes arthralgia and arthritis, skin rush, pleuritis or pericarditis, kidney or CNS disorders, and different types of cytopenia in blood [1]. Even though the precise etiologic and pathogenic mechanisms of the SLE are not clearly understood, it is assumed that SLE appears due to the complex interaction of different endogenic (genetic) [2] and exogenic (environmental) factors [3]. The dominant pathogenic mechanism in SLE is the dysfunction of immunoregulatory mechanisms due to the abnormal programmed cell death and oxidative stress, which results in loss of immune tolerance and increased autoantibody production [4].
Up to date studies showed an increased production of reactive oxygen (ROS) and nitrogen (RNS) species [5] and significantly decreased activity of antioxidative defense enzymes (catalase, superoxide dismutase, and glutathione peroxidase) in serum, plasma, and saliva of SLE patients [6, 7]. The possible factors that are responsible for decreased activity of antioxidative defense enzymes are the presence of single nucleotide polymorphisms (SNPs) in the genes that code enzymes involved in antioxidative defense.
Superoxide dismutase (SOD) is the first-line defense enzyme that protects cells from ROS by catalyzing the dismutation of superoxide anion radical to hydrogen peroxide (H2O2). Manganese SOD (MnSOD or SOD2; EC1.15.1.1) is the mitochondrial isoenzyme, coded by the gene located at the position 6q25 [8]. One of the most frequently studied SNPs in the MnSOD gene is rs4880, which is located at the 16th position within the mitochondrial target sequence (MTS). It is characterized by alanine (GCT) to valine (GTT) transition due to cytosine (C) to thymine (T) change at the position 2734. Valine disturbs enzyme translocation from cytosol to the mitochondrial matrix where the active enzyme is formed. It is considered that rs4880 SNP is associated with different diseases, such as diabetes mellitus [9], human neurodegenerative and aging disorders, Parkinson’s [10] or Alzheimer’s disease [11], schizophrenia [12], prostate cancer [13], and bronchial asthma [14].
Catalase (CAT; EC1.11.1.6) is an intracellular, complex enzyme containing four identical subunits. It is present in the peroxisomes and catalyzes decomposition of H2O2 [15]. Human CAT gene is located in the 11th chromosome, position 11p13, and consists of 13 exons and 12 introns. Numbers of SNPs are identified in this gene: A-21T (rs793316), C-262T (rs1001179), and C-844T (rs769214). The most frequently studied SNP that leads to the substitution of cytosine (C) by thymine (T) at the position -262 is C-262T, located in the promoter region of the CAT gene. The presence of CAT-262T allele influences transcription process, and it is previously shown that it is associated with a catalasia [16]. Catalase A-21T (rs7943316) SNP is located in the promoter region of the gene, proximal from the transcription start site. It is characterized by adenine (A) to thymine (T) change in the position-21. Allele CAT-21T is associated with an increased risk for vitiligo and protective effect in osteonecrosis [16, 17], but it is not previously studied in SLE.
Glutathione S-transferase (GST) is also an enzyme that has very important role in the free radicals detoxification. Gene products of GSTM1 and GSTT1 are responsible for the detoxification of polycyclic aromatic hydrocarbons (PAHs) and smaller hydrocarbons, respectively, as well as for ROS scavenging [18], and thus have an important role in the protection of DNA from oxidative damage [19]. GSTM1 gene cluster is located at the 1p13.3 position, while GSTT1 gene is located at the position 22q11.2. Two common deletion SNPs are known in both genes. They result in the absence of enzyme activity, particularly in subjects with deletions of both GSTM1 and GSTT1 [20, 21].
In the last years, great numbers of SNPs are identified in order to explain the genetic background of the complex diseases. However, even if the particular SNPs are important indicators of the genetic background of complex diseases, they explain only a part of the genetic risk [22]. Thus, it is very important to examine possible SNP–SNP interactions in order to elucidate the real genetic risk for the certain disease. To the best of our knowledge, SNP–SNP interactions between the antioxidative enzymes are not previously studied in SLE.
Since the oxidative stress has very important role in disease pathogenesis and that SNPs located in the genes that code for antioxidative enzymes may change their activity, the aim of this study was to examine the association of SNPs in the CAT (rs1001179 and rs7943316), MnSOD (rs4880), GSTM1, and GSTT1 genes and to examine SNP–SNP interactions between these antioxidative enzymes in Serbian patients with SLE.
Patients and methods
Patients
A total of 176 subjects were involved in this study. All participants were divided into two groups:
-
Group I included 88 patients with SLE, 34 to 70 years old (median = 52). SLE was diagnosed according to the “Eleven Criteria of Lupus” guidelines of the American College of Rheumatology. Based on the clinical disease presentation, all patients were divided into 4 subgroups, as follows: patients with musculoskeletal manifestation (50), patients with hematologic changes (11), patients with lupus nephritis (17), and patients with neurologic lupus (6).
-
Group II included 88 healthy control subjects, matched by sex and age, without previous history of SLE or other acute and chronic disease.
All subjects signed an informed consent prior to inclusion in the study. The study was approved by the Ethical Committee of the Faculty of Medicine, University of Nis, Serbia. The research was conducted at the Laboratory for Functional Genomics and Proteomics, Faculty of Medicine, University of Nis, Serbia, according to the guidelines of the Declaration of Helsinki and the good laboratory practice.
Methods
Blood samples were obtained by the punction of the median cubital vein during the routine laboratory control. Two hundred microliters of blood was used for DNA isolation.
DNA isolation
DNA was isolated from the leucocytes of the whole blood using “QIAamp DNA Blood Mini Kit” (Quiagen GmbH, Hilden, Germany).
Genotyping methods
DNA samples were used for the determination of CAT A-21T (rs7943316), CAT C-262T (rs1001139), MnSOD Ala16Val (rs4880), GSTT1, and GSTM1 SNPs. The SNPs in the CAT and MnSOD genes were determined using the polymerase chain reaction–restriction fragment length polymorphism (PCR-RFLP), while GSTT1 and GSTM1 were determined using the multiplex PCR.
PCR reaction was performed in the total volume of 25 μl containing 50 ng/μl of DNA and 10 μM of forward and reverse primers (CAT A-21T: F—5′-AATCAGAAGGCAGTCCTCCC-3′ and R–5′-TCGGGGAGCACAGAGTGTAC-3′; CAT C-262T: F—5′-GCC GCC TTT TTG CCT ATC CT-3′ and R–5′-TCCCGCCCATCTGCTCCAC-3′; MnSOD Ala16Val: F–5′-CCAGCAGGCAGCTGGCAC CG-3′ and R–5′-TCCAGGGCGCCGTAGTCGTAGG -3′; GSTM1: F—5′-CTGCCCTACTTGATTGATGGG-3′ and R—5′-CTGGATTGTAGCAGATCATGC-3′; GSTT1: F—5′-TTCCTTACTGGTCCTCACATCTC-3′ and R—5′-TCACGGGATCATGGCCAGCA-3′).
PCR products were verified on 2% agarose gel and afterwards digested using the specific restriction endonuclease (HinfI for CAT A-21T, SmaI for CAT C-262T, AgeI (BshTI) for SOD Ala16Val). Obtained results were visualized on 8% polyacrylamide gels and interpreted according to the obtained restriction fragments:
-
CAT A-21T: A allele 177 and 73 bp or T allele 250 bp
-
CAT C-262T: C allele 155 and 30 bp or T allele 185 bp
-
MnSOD Ala16Val: Ala allele 74 and 17 bp or Val allele 91 bp
Statistical analysis
The allele and the genotype frequencies determined in patients and healthy controls were compared with the values predicted by the Hardy–Weinberg equilibrium using the chi-squared (χ 2) test. The chi-squared and the two-tailed Fisher’s exact test (when the number of samples was less than 5) were used to compare allele and genotype frequencies between the groups. The risk was estimated by the odds ratio (OR) with 95% confidence interval (CI). Probability values less than 0.05 were considered statistically significant.
Linkage disequilibrium was calculated using PLINK version 1.07 [23]. The multifactor dimensionality reduction (MDR) method was used for the detection of SNP–SNP interactions between all genotyped SNPs. Statistical analysis and graphic presentation of the data were carried out using the MDR software package version 3.0.2 [24]. Evaluation of the obtained models was performed based on the testing accuracy (TA) as the measure of proportion of cases that are grouped correctly according to their case-control status and cross-validation consistency (CVC). CVC is the measure of the number of times the particular set of loci is identified in each of the subject in 10-fold cross-validation. The best selected model was the model with the highest TA and CVC. The statistical significance of the model was assessed by permutation testing using the MDR permutation testing software version 1.0 [24]. High- and low-risk genotype combinations were determined based on threshold value (1.0 in this study).
Results
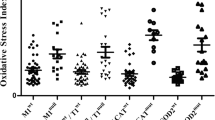
Analysis of genotypes and alleles of the SNPs in genes of antioxidative enzymes (MnSOD Ala16Va (rs4880), CAT A-21T (rs7943316), CAT C-262T (rs1001139), GSTT1, and GSTM1)
The genotype frequencies for all studied SNPs were in Hardy–Weinberg equilibrium (p > 0.05). Table 1 represents the distribution of genotypes for the studied SNPs.
The distribution of rs4880 genotypes showed statistically significant differences between SLE patients and healthy controls. Genotypes containing mutant MnSODVal allele (AlaVal + ValVal) are more frequent in SLE patients (75%) compared to controls (51.14%), while homozygous AlaAla genotype is more frequent in healthy controls compared to SLE patients (25 vs. 48.86%; χ 2 = 15.17; df = 2; p = 0.001; Table 1).
Distribution of genotypes for two studied SNPs in the catalase gene, A-21T and C-262T, did not show differences between patients and healthy controls (p = 0.283 and p = 0.157, respectively). Moreover, no differences in the distribution of GSTT1 (p = 0.34) and GSTM1 (p = 0.645) were observed between studied groups (Table 1).
Distributions of alleles for Ala16Val MnSOD, CAT A-21T, and CAT C-262T SNPs are presented in Table 2. The presence of MnSODAla allele was significantly higher in controls (72.77%) compared to SLE patients (54.54%), while MnSODVal allele was observed in 27.27% healthy subjects and 45.45% patients (p < 0.001; Table 2). However, distributions of CAT A-21T and CAT C-262T alleles did not show differences between SLE patients and controls (p < 0.05; Table 2).
Analysis of the association of SNPs in genes of antioxidative enzymes (MnSOD Ala16Va (rs4880), CAT A-21T (rs7943316), CAT C-262T (rs1001139), GSTT1 and GSTM1) with clinical manifestations of SLE
Distribution of genotypes of the studied SNPs according to the clinical manifestations of SLE (musculoskeletal, renal, neurologic, or hematologic) is presented in Table 3. Four patients were excluded from this analysis due to the overlap of SLE with other comorbidities. The genotypes of the studied SNPs in patients with the certain clinical presentation of the disease were compared to the presence of the genotypes in patients without certain clinical manifestation of SLE. Obtained results showed association of MnSODValVal genotype with neurologic manifestations of SLE (p = 0.016; OR = 6.7; 95% CI = 1.18–37.89), while homozygous GSTT1 showed association with musculoskeletal manifestations of SLE (p = 0.008; OR = 4.168; 95% CI = 1.364–12.737). No associations of clinical manifestations of disease were observed for catalase (CAT C-262T and CAT A-21T) and GSTM1 SNPs.
SNP–SNP interaction analysis
Among the predicted models, presented in the Table 4, two-locus (MnSOD, GST) and four-locus (MnSOD, CAT-21, CAT-262, GST) models were selected as the best models with CVC 10/10 and the highest TA of 0.665 and 0.668, respectively. Two- and four-locus models were statistically significant with p values of 0.005 and 0.004, respectively. Three-locus model (MnSOD, CAT-262, GST) reveals high TA of 0.631 and CVC 10/10, but the model was not statistically significant (p > 0.0125; Table 4).
High- and low-risk genotype combinations in the two-locus model of interaction between MnSOD and GST are presented in Fig. 1. The combination of genotypes was labeled as high risk if the ratio between the SLE patients, and the healthy controls were above threshold or as low risk if the ratio was below threshold. The carriers of AlaVal/T+M+ genotype combination, as well as AlaAla/T−M+ and combinations of homozygous MnSODValVal with GST genotypes, were selected as the high-risk combinations for SLE. Other genotype combinations in the two-locus model were labeled as low risk, while ValVal/T−M− genotype combination was not observed in the present study.
Distribution of high- and low-risk genotype combinations in two-locus model of interaction between MnSOD and GST SNPs. High-risk genotype combinations are represented with the dark gray cells, while those at low risk are represented with the light gray cells. White cell represents the combination of genotypes that was not detected in the study. Left bar in each cell corresponds to the number of SLE patients, and right bar corresponds to the number of control subjects
Interaction graph based on entropy measures between individual variables showed strong positive correlation (3.43%) between CAT A-21T and CAT C-262T SNPs (red colored line in Fig. 2) in patients with SLE which was not influenced by LD (r 2 = 0.005; D′ = 0.071). Additionally, mild interaction was present between MnSOD and GST SNPs (1.16%), while no interaction or redundancy was observed between MnSOD and catalase SNPs (Fig. 2).
Discussion
The association of CAT A-21T, CAT C-262T, Ala16ValMnSOD, GSTT1, and GSTM1 SNPs, as well as their interactions, with SLE was analyzed in this study. Since SLE is a chronic inflammatory autoimmune disease in which pathogenesis oxidative stress has very important role, we hypothesized that patients who are carriers of CAT-21T, CAT-262T, MnSODVal alleles, and deletions of GSTT1 and GSTM1 are prone to higher level of oxidative stress due to lower antioxidative defense compared to the patients who are carriers of wild type alleles (CAT-21A, CAT-262C, MnSODAla) or who do not carry GSTT1 and GSTM1 deletions.
Literature data showed significantly increased oxidative stress parameters in patients with SLE [5,6,7], as well as lower activity of antioxidative enzymes (catalase, SOD, and glutathione peroxidase) [7, 8]. Moreover, some authors suggested that synthesis of autoantibodies against antioxidative enzymes is responsible for lower activity of these enzymes [25, 26]. Furthermore, SNPs in genes that code the antioxidative enzymes may alter enzyme structure, substrate specificity, or enzyme’s activity and thus modify inter-individual variability in the defense capacity against oxidative stress [27].
Polymorphism MnSODAla16Val is characterized by the substitution of GCT to GTT sequence and thus substitution of alanine to valine at the 16th position of MTS. In newly diagnosed SLE patient, SOD activity is significantly lower compared to healthy subjects [28]. Distribution of MnSODAla allele differs between populations and counts from 11 to 30% in Japanese and Chinese to 41–62% in Caucasians [29]. In our population, MnSODAla allele was presented in 72.72% of healthy controls and 54.54% of SLE patients. MnSODVal allele was more frequent in patients compared to controls indicating 2.2-fold higher risk for disease in patients with SLE. Furthermore, genotypes with the mutant MnSODVal allele (AlaVal and ValVal) showed significantly higher frequency in SLE patients compared to healthy controls. Presence of the mutant MnSODVal allele changes the secondary structure of protein (β sheet is formed instead of α helix which is formed in the presence of MnSODAla allele) and thus disturbs enzyme translocation from cytosol to the mitochondrial matrix. Protein is kept in the inner mitochondrial membrane resulting in lower production of the active tetramer in mitochondrial matrix and thus inappropriate antioxidative defense due to lower enzyme activity [30]. It is previously shown that the presence of MnSODVal allele is associated with 30–40% lower enzyme activity. Moreover, mutant MnSODVal allele may also influence mRNA stability [30]. Homozygous ValVal genotype is significantly associated with neurologic manifestations of SLE in our study. Sobkowial et al. showed that ValVal genotype is associated with Raynaud’s phenomenon and immunologic manifestations of SLE [31].
Single-nucleotide polymorphisms in the CAT gene might alter the susceptibility to oxidative stress-mediated injury. It is suggested that CAT C-262T, located in the promoter region of catalase gene, may influence transcription by changing the binding of transcription factors and thus alter basal catalase expression in different cell types [15]. Our study showed that genotype and allele distributions of catalase SNPs were not significantly different between SLE patients and healthy controls. These results are in accordance with the literature data [25, 32,33,34]. Also, no association of CAT C-262T with the clinical manifestations of disease was found in our study. However, Warhol et al. showed significant correlation of C-262T SNP with thrombocytopenia, leukopenia, and increased autoantibody titer [32].
Distribution of CAT A-21T genotypes in healthy Caucasians showed that AT genotype is more frequent compared to TT and that AA has the lowest frequency, which is in accordance with our results [35]. Similar distribution is present in Russian and Tamil population of south India [16, 36], but in Chinese, AA is present in 56.3% and TT in only 8.1% [17]. According to Polonikov et al., CAT A-21T SNP is associated with the increased oxidative stress due to the decreased enzyme activity [37]. It is previously shown that CAT A-21T is associated with vitiligo [17], osteonecrosis [16], and bronchial asthma [29, 37], but it is not previously studied in SLE. However, our study failed to show any association of this SNP with SLE, as well as with clinical manifestations of disease.
Besides the catalase and SOD, GST superfamily of the genes has very important role in oxidative stress. It is shown that GSTM1 and GSTT1 genes are polymorphic and GSTM1 deletion is detected in 35–60%, whileGSTT1 deletion is detected in 10–65%of individuals depending on the studied population [38]. Detection of GSTM1 and GSTT1 null mutations could be of great importance, since the inadequate antioxidative defense is one of the risk factors for SLE development. Kang et al. suggested that GSTM1 and GSTT1 polymorphisms are not associated with SLE risk, but may affect the susceptibility to certain clinical manifestations and autoantibody profiles in Korean population [39]. Furthermore, few other studies demonstrated no association between SLE and presence of the homozygous null GSTM1 or GSTT1 genotype, which is in accordance with the results obtained in our study [40,41,42]. However, our results showed association of homozygous GSTT1 gene and musculoskeletal manifestations of SLE. The study of Kang et al. revealed association of GSTT1 null genotype with decreased discoid rash andnephritis [39], while the study of Tew et al. failed to find association of GST null alleles either with the development of SLE or with its clinical manifestations [41]. Association of GSTM1 null genotype with autoantibodies was previously showed in Caucasian and Afro-American patients with SLE [40]. However, GSTM1 null genotype had lower prevalence of hematologic disorders, suggesting the protective effect against hematologic manifestations in SLE [39].
Even if it is shown that particular SNPs are associated with disease, it can only partially explain genetic risk for the certain disease. Thus, the examination of SNP–SNP interactions is important in order to explain the genetic risk in complex diseases. To the best of our knowledge, this is the first study that examined interactions of SNPs in antioxidative enzymes in SLE. Obtained results showed that AlaVal/T+M+ genotype combination, which had the highest frequency compared to other MnSOD/GST combination genotypes, is a high-risk genotype for SLE. Moreover, even though the particular catalase SNPs did not show association with SLE, interaction analysis showed positive correlation between CAT C-262T and CAT A-21T SNPs which is not influenced by linkage disequilibrium.
Conclusion
In conclusion, this is the first study that examined CAT A-21T SNP, as well as SNP–SNP interactions of antioxidative enzymes in SLE patients. Genotypes containing MnSODVal allele and MnSODVal allele are risk factors for SLE, as well as for SLE with neurologic manifestations, while homozygous GSTT1 genotype is the risk factor for SLE with musculoskeletal manifestations. Catalase SNPs (C-262T and A-21T) show positive correlation in the model of SNP–SNP interaction.
References
Tsokos GC (2011) Systemic lupus erythematosus. N Engl J Med 365:2110–2121
Nath SK, Kilpatrick J, Harley JB (2004) Genetics of human systemic lupus erythematosus: the emerging picture. Curr Opin Immunol 16:794–800
Miller FW, Alfredsson L, Costenbader KH, Kamen DL, Nelson LM, Norris JM, De Roos AJ (2012) Epidemiology of environmental exposures and human autoimmune diseases: findings from a National Institute of Environmental Health Sciences Expert Panel Workshop. J Autoimmun 39(4):259–271
Manson JJ, Isenberg DA (2003) The pathogenesis of systemic lupus erythematosus. Neth J Med 61:343–346
Oates JC, Farrelly LW, Hofbauer AF, Wang W, Gilkeson GS (2007) Association of reactive oxygen and nitrogen intermediate and complement levels with apoptosis of peripheral blood mononuclear cells in lupus patients. Arthritis Rheum 56(11):3738–3747
Bae SC, Kim SJ, Sung MK (2002) Impaired antioxidant status and decreased dietary intake of antioxidants in patients with systemic lupus erythematosus. Rheumatol Int 22(6):238–243
Zaieni SH, Derakhshan Z, Sariri R (2015) Alternations of salivary antioxidant enzymes in systemic lupus erythematosus. Lupus 24(13):1400–1405
Bastaki M, Huen K, Manzanillo P, Chande N, Chen C, Balmes JR, Tager IB, Holland N (2006) Genotype activity relationship for Mn-superoxide dismutase, glutathione peroxidase 1 and catalase in humans. Pharmacogenet Genomics 16(4):279–286
Pourvali K, Abbasi M, Mottaghi A (2016) Role of superoxide dismutase 2 gene Ala16Val polymorphism and total antioxidant capacity in diabetes and its complications. Avicenna J Med Biotechnol 8(2):48–56
Shimoda-Matsubayashi S, Matsumine H, Kobayashi T, Nakagawa-Hattori Y, Shimizu Y, Mizino Y (1996) Structural dimorphism in the mitochondrial targeting sequence in the human manganese superoxide dismutase gene. Biochem Biophys Res Commun 226:561–565
Ventriglia M, BocchioChiavetto L, Scassellati C, Squitti R, Binetti G, Ghidoni R, Rossini PM, Gennarelli M (2005) Lack of association between MnSOD gene polymorphism and sporadic Alzheimer’s disease. Aging Clin Exp Res 17(6):445–448
Akyol O, Yanik M, Elyas H, Namli M, Canatan H, Akin H, Yuce H, Yilmaz HR, Tutkun H, Sogut S, Herken H, Özyurt H, Savas HA, Zoruglu SS (2005) Association between Ala-9-Val polymorphism of Mn-SOD gene and schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 29:123–131
Arsova-Sarafinovska Z, Matevska N, Petrovski D, Banev S, Dzikova S, Georgiev V, Sikole A, Sayal A, Aydin A, Suturkova L, Dimovski AJ (2008) Manganese superoxide dismutase (MnSOD) genetic polymorphism is associated with risk of early-onset prostate cancer. Cell Biochem Funct 26(7):771–777
Holla LI, Kankova K, Vasku A (2006) Functional polymorphism in the manganese superoxide dismutase (MnSOD) gene in patients with asthma. Clin Biochem 39(3):299–302
Kodydková J, Vávrová L, Kocík M, Žák A (2014) Human catalase, its polymorphisms, regulation and changes of its activity in different diseases. Folia Biol 60:153–167
Kim TH, Hong JM, Oh B, Cho YS, Lee JY, Kim HL et al (2008) Genetic association study of polymorphisms in the catalase gene with the risk of osteonecrosis of the femoral head in the Korean population. Osteoarthr Cartil 16(9):1060–1066
Liu L, Li C, Gao J, Li K, Zhang R, Wang G et al (2010) Promotor variant in the catalase gene is associated with vitiligo in Chinese people. J Investig Dermatol 130(11):2674–2653
Barnes PJ (1990) Reactive oxygen species and airway inflammation. Free Radic Biol Med 9:235–243
Ryberg D, Skaug V, Hewer A et al (1997) Genotypes of glutathione transferase M1 and P1 and their significance for lung DNA adduct levels and cancer risk. Carcinogenesis 18:1285–1289
Bruhn C, Brockmoller J, Kerb R, Roots I, Borchert HH (1998) Concordance between enzyme activity and genotype of glutathione S-transferase theta (GSTT1). Biochem Pharmacol 56:1189–1193
Nelson HH, Wiencke JK, Christiani DC et al (1995) Ethnic differences in the prevalence of the homozygous deleted genotype of glutathione S-transferase theta. Carcinogenesis 16:1243–1245
Curk T, Rot G, Zupan B (2011) SNPsyn: detection and exploration of SNP-SNP interactions. Nucleic Acids Res 39(Web Server issue):W444–W449
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D, Maller J, Sklar P, de Bakker PI, Daly MJ, Sham PC (2007) PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet 81(3):559–575
Hahn LW, Ritchie MD, Moore JH (2003) Multifactor dimensionality reduction software for detecting gene-gene and gene-environment interactions. Bioinformatics 19:376–382
Shah D, Kiran R, Wanchu A, Bhatnagar A (2010) Oxidative stress in systemic lupus erythematosus: relationship to Th1 cytokine and disease activity. Immunol Lett 129:7–12
Mansour RB, Lassoued S, Gargouri B, El Gaid A, Attia H, Fakhfakh F (2008) Increased levels of autoantibodies against catalase and superoxide dismutase associated with oxidative stress in patients with rheumatoid arthritis and systemic lupus erythematosus. Scand J Rheumatol 37:103–108
BohanecGrabar P, Logar D, Tomsic M, Rozman B, Dolzan V (2009) Genetic polymorphisms modifying oxidative stress are associated with disease activity in rheumatoid arthritis patients. Dis Markers 26:41–48
Yang LL, Huang MS, Huang CC, Wang TH, Lin MC, Wu CC et al (2011) The association between adult asthma and superoxide dismutase and catalase gene activity. Int Arch Allergy Immunol 156(4):373–380
Mak JC, Leung HC, Ho SP, Ko FW, Cheung AH, Ip MS et al (2006) Polymorphisms in manganese superoxide dismutase and catalase genes: functional study in Hong Kong Chinese asthma patients. Clin Exp Allergy 36(4):440–447
Sutton A, Khoury H, Prip-Buus C, Cepanec C, Pessayre D, Degoul F (2003) The Ala16Val genetic dimorphism modulates the import of human manganese superoxide dismutase into rat liver mitochondria. Pharmacogenetics 13:145–157
Sobkowiak A, Lianeri M, Wudarski M, Lacki JK, Jagodzinski PP (2008) Manganese superoxide dismutase Ala-9Val mitochondrial targeting sequence polymorphism in systemic lupus erythematosus in Poland. Clin Rheumatol 27:827–831
Warchoł T, Lianeri M, Wudarski M, Łacki JK, Jagodziński PP (2008) Catalase-262C/T polymorphism in systemic lupus erythematosus in Poland. Rheumatol Int 28(10):1035–1039
Ghaly MS, Ghattas MH, Labib SM (2012) Association of catalase gene polymorphisms with catalase activity and susceptibility to systemic lupus erythematosus in the Suez Canal area, Egypt. Lupus 21(11):1244–1249
Eny KM, El-Sohemy A, Cornelis MC, Sung YK, Bae SC (2005) Catalase and PPARgamma2 genotype and risk of systemic lupus erythematosus in Koreans. Lupus 14(5):351–355
Ukkola O, Erkkilä PH, Savolainen MJ, Kesän YA (2001) Lack of association between polymorphisms of catalase, copper-zinc superoxide dismutase (SOD), extracellular SOD and endothelial nitric oxide synthase genes and macroangiopathy in patients with type 2 diabetes mellitus. J Intern Med 249(5):451–459
Lourdhu Mary A, Nithya K, Isabel W, Angeline T (2014) Prevalence of catalase (-21 A/T) gene variant in south Indian (Tamil) population. Biomed Res Int 2014:894237
Polonikov AV, Ivanov VP, Solodilova MA, Kozhuhov MA, Panfilov VI (2009) Tobacco smoking, fruit and vegetable intake modify association between −21 a>T polymorphism of catalase gene and risk of bronchial asthma. J Asthma 46(3):217–224
Bell DA, Taylor JA, Paulson DF, Robertson CN, Mohler JL, Lucier GW (1993) Genetic risk and carcinogen exposure: a common inherited defect of the carcinogen-metabolism gene glutathione S-transferase M1 (GSTM1) that increases susceptibility to bladder cancer. J Natl Cancer Inst 85:1159–1164
Kang TY, El-Sohemy A, Comelis MC, Eny KM, Bae SC (2005) Glutathione S-transferase genotype and risk of systemic lupus erythematosus in Koreans. Lupus 14(5):381–384
Fraser PA, Ding WZ, Mohseni M et al (2003) Glutathione S-transferase M null homozygosity and risk of systemic lupus erythematosus associated with sun exposure: a possible gene-environment interaction for autoimmunity. J Rheumatol 30:276–282
Tew MB, Ahn CW, Friedman AW et al (2001) Systemic lupus erythematosus in three ethnic groups. VIII. Lack of association of glutathione S-transferase null alleles with disease manifestations. Arthritis Rheum 44:981–983
Horiuchi T, Washio M, Kiyohara C, Tsukamoto H, Tada Y, Asami T, Ide S, Kobashi G, Takahashi H, Kyushu Sapporo SLE Study Group (2009) Combination of TNF-RII, CYP1A1 and GSTM1 polymorphisms and the risk of Japanese SLE: findings from the KYSS study. Rheumatology (Oxford) 48(9):1045–1049
Acknowledgments
This work was supported by the Ministry of Education, Science, and Technological Development of the Republic of Serbia (grant number III41018, 2011–2016).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All subjects signed an informed consent prior to inclusion in the study. The study was approved by the Ethical Committee of the Faculty of Medicine, University of Nis, Serbia. The research was conducted at the Laboratory for Functional Genomics and Proteomics, Faculty of Medicine, University of Nis, Serbia, according to the guidelines of the Declaration of Helsinki and the good laboratory practice.
Disclosures
None.
Rights and permissions
About this article
Cite this article
Jevtovic Stoimenov, T., Despotovic, M., Stojanovic, S. et al. Polymorphic variants of antioxidative defense enzymes and their gene-gene epistatic interactions in systemic lupus erythematode patients. Clin Rheumatol 36, 2019–2026 (2017). https://doi.org/10.1007/s10067-017-3755-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-017-3755-x