Abstract
A consistent line of investigation proposes that fibromyalgia is a sympathetically maintained neuropathic pain syndrome. Dorsal root ganglia sodium channels may play a major role in fibromyalgia pain transmission. Ambroxol is a secretolytic agent used in the treatment of various airway disorders. Recently, it was discovered that this compound is also an efficient sodium channel blocker with potent anti-neuropathic pain properties. We evaluated the add-on effect of ambroxol to the treatment of fibromyalgia. We studied 25 patients with fibromyalgia. Ambroxol was prescribed at the usual clinical dose of 30 mg PO 3 times a day × 1 month. At the beginning and at the end of the study, all participants filled out the Revised Fibromyalgia Impact Questionnaire (FIQ-R) and the 2010 ACR diagnostic criteria including the widespread pain index (WPI). At the end of the study, FIQ-R decreased from a baseline value of 62 ± 15 to 51 ± 19 (p = 0.013). Pain visual analogue scale decreased from 77 ± 14 to 56 ± 30 (p = 0.018). WPI diminished from 14.6 ± 3.1 to 10.4 ± 5.3 (p = 0.001). Side effects were minor. In this pilot study, the use of ambroxol was associated to decreased fibromyalgia pain and improved fibromyalgia symptoms. The open nature of our study does not allow extracting the placebo effect from the positive results. The drug was well tolerated. Ambroxol newly recognized pharmacological properties could theoretically interfere with fibromyalgia pain pathways. Dose escalating-controlled studies seem warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction/objectives
A consistent course of investigations proposes that fibromyalgia is a sympathetically maintained neuropathic pain syndrome [1]. This proposal is reinforced by the recent description of small fiber neuropathy in a sizable proportion of fibromyalgia patients [2,3,4]. Small fiber neuropathy is a disorder of the thinly myelinated A-delta-fibers and unmyelinated C-fibers and is typically manifested by neuropathic pain and autonomic dysfunction.
Voltage-gated sodium channels play a major role in small fiber neuropathies. This type of sodium channels are responsible for the generation and conduction of action potentials in the dorsal root ganglia, in peripheral nociceptive neuronal pathway and in sympathetic fibers where NaV 1.7, NaV1.8, and NaV 1.9 channels (encoded by SCN9A, SCN10A, and SCN11A) are preferentially expressed [5]. Idiopathic small fiber neuropathy has been associated to Nav1.7 and Nav1.8 sodium channels gain of function mutations [6]. Severe fibromyalgia has been linked to a particular Nav1.7 genotype [7]. Nav1.8 polymorphisms have not been investigated in fibromyalgia patients. This emerging information makes dorsal root ganglia sodium channels an attractive fibromyalgia therapeutic target.
Ambroxol (2-amino-3,5-dibromo-N-[trans-4-hydroxycyclohexyl]benzylamine) is a secretolytic agent used in the treatment of various airway disorders since the late 1970s. Recently it was determined that this compound is a strong Nav1.8 sodium channel blocker with potent anti-neuropathic pain properties [8]. Ambroxol potency is 55, 39, and 13 times higher compared to others known sodium channel blocker such as benzocaine, lidocaine, and mexiletine, respectively [9]. Furthermore, this medication is effective in the neuropathic pain animal model [10]. Ambroxol has good safety profile. In many countries, this compound is freely dispensed as over-the-counter medication.
The objective of this pilot open label study was to evaluate the add-on effect of ambroxol to fibromyalgia pharmacological therapy.
Methods
In this one-group pretest-posttest open label pilot clinical observation, we recruited adult women with fibromyalgia that fulfilled the 2010 American College of Rheumatology (ACR) diagnostic criteria. The inclusion criteria demanded to have more than 5 points, in a 1 to 10 pain visual analogue scale, and to be in a stable pharmacological treatment in the previous 30 days. Exclusion criteria included comorbid autoimmune conditions, major anxiety/depression illness, or the presence of other concomitant illness. The institutional ethics and research committees approved the protocol (PT16-025). All participants signed a written consent form.
Ambroxol (Laboratorios Vitae S.A. de C.V., Lot: 601017) was added to the stable pharmacological therapy for 1 month period. Ambroxol was used at the amount usually recommended to clear excessive bronchial secretions of 30 mg PO 3 times a day. Acetaminophen 500 mg PO 3 times a day was allowed as pain rescue therapy. A log diary was given to each patient to supervise medication adherence. Patients were asked to mark date and time of each ambroxol or acetaminophen intake. Medication adherence less than 80% was considered as protocol violation.
Adverse events were graded according to the NIH Common Terminology Criteria for Adverse Events as follows: Mild: asymptomatic or mild symptoms, clinical or diagnostic observations only, intervention not indicated; Moderate: minimal, local, or noninvasive intervention indicated; and Severe: disabling, limiting self-care, hospitalization, or prolongation of hospitalization indicated.
At the beginning and at the end of the study, all participants filled out the following questionnaires: the Revised Fibromyalgia Impact Questionnaire (FIQ-R), the Hospital Anxiety and Depression Scale (HADS), the 2010 ACR diagnostic criteria including the following domains: Widespread Pain Index (WPI), Symptoms Severity Scale (SSS) and Polysymptomatic Distress Scale (PDS), Composite Autonomic Symptom Score 31 (COMPASS-31), Self-report Leeds Assessment of Neuropathic Symptoms and Signs pain scale (sLANSS), and Patient Global Impression of Change (PGIC). We did not test for cognitive impairment.
Statistical analysis
Quantitative variables are expressed as mean ± standard deviation. Qualitative variables are shown as percentages. Kolmogorov-Smirnov test was used for normality analysis. T test, Fisher’s exact test, Wilcoxon signed-rank test, and McNemar test were used for comparisons. Microsoft Excel 2010 was used to capture questionnaire answers and IBM SPSS Statistics 23 for calculations.
Results
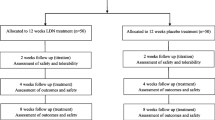
Participants were sourced from four hospital-based rheumatology clinics. We screened 37 patients, 7 had an exclusion criterion and did not enter the study. An additional 5 cases did not finish the study (Fig. 1). The per-protocol analysis was calculated for those patients who had more than 80% ambroxol adherence (25 patients). Safety information included the low medication adherence case (n = 26).
Patients mean age was 45 ± 10 years. All of them were female. As a group, they had severe fibromyalgia according to the revised Fibromyalgia Impact Questionnaire mean score of 62. At the end of the study, the group showed significant improvement in many fibromyalgia symptoms included in the questionnaires as shown in Table 1 and Fig. 2. HADS anxiety and depression scores had no significant change (Table 1).
PGIC scores showed improvement in 12 patients, no change in 9, and worsening in 4 cases. Concurrent medication use is shown in Table 2. Six subjects required acetaminophen pain rescue therapy, but only one of them took this medication in the final 36 h of the study. Side effects were minor and did not require drug withdrawal. Seventeen subjects had 27 non-serious adverse events (Table 3).
Discussion
We have proposed fibromyalgia as a neuropathic pain syndrome based on the following arguments: (a) fibromyalgia is a stimulus independent pain state, (b) the presence of allodynia as characteristic fibromyalgia feature, (c) the presence of paresthesias in the overwhelming majority of patients suffering from this condition [1].
Among neuropathic pain syndromes, fibromyalgia is suggested to be sympathetically maintained based on the following issues: (a) frequent physical and/or emotional trauma as inciting event, (b) diverse heart rate variability analyses showing that fibromyalgia patients have signs of ongoing sympathetic hyperactivity [11, 12], and (c) a double blind study demonstrating that fibromyalgia patients have norepinephrine-evoked pain [13]. Sympathetic dysfunction may also explain the multiple non-pain-related fibromyalgia symptoms [1]. The recent description of small fiber pathology in fibromyalgia patients reinforces the notion of fibromyalgia as a neuropathic pain syndrome [2,3,4].
In this pilot study, the use of a sodium channel blocker ambroxol was associated not only to decreased fibromyalgia pain but also to improvement in other bothersome fibromyalgia features such as sleep disturbances, stiffness, and dysautonomia symptoms. Hypothetically, ambroxol analgesic properties could lighten up sympathetic tone and thus alleviating insomnia and dysautonomia symptoms. Acetaminophen rescue therapy may had little or no effect on the final results, only 1 patient was taking this analgesic in the final 36 h of the study.
The open nature of our study does not allow extracting the placebo effect from the positive results. The drug was well tolerated.
Although animal models have shown that ambroxol is a potent anti-neuropathic analgesic compound [9, 10], human studies looking at the analgesic properties of the drug are scant. Controlled studies have shown that ambroxol lozenges are more effective than placebo in alleviating acute pharyngitis pain [14]. An uncontrolled observation suggests that topical ambroxol may be effective in relieving regional neuropathic pain [15].
Ambroxol is a well-tolerated drug. In many countries, it is dispensed as over-the-counter medication. Ambroxol has been recently used in much higher dose (up to 1300 mg per day) as a pharmacological chaperone therapy for Gaucher disease, without major side effects [16]. Ambroxol is a very cheap generic compound. The calculated monthly price at the dose used in our study would be around US$4.
Ambroxol newly recognized pharmacological properties could theoretically interfere with proposed fibromyalgia pain pathways. Preliminary evidence suggests that dorsal root ganglia sodium channels may play a key role in both small fiber neuropathy [6] and fibromyalgia [7]. As already stated, ambroxol is a potent sodium channel blocker with strong anti-neuropathic pain properties [8,9,10].
An obvious limitation of our pilot study is the lack of control group. So, placebo effect could be responsible for the favorable outcome.
Conclusion
There are theoretical bases suggesting that ambroxol may be useful for fibromyalgia treatment. In this uncontrolled pilot clinical observation, the use of ambroxol was associated to fibromyalgia symptoms improvement. The drug was well tolerated. Randomized-controlled studies are warranted. In view of its good tolerability profile, higher ambroxol dosages may be explored.
References
Martinez-Lavin M (2007) Biology and therapy of fibromyalgia. Stress, the stress response system, and fibromyalgia. Arthritis Res Ther 9:216–219
Oaklander AL, Herzog ZD, Downs HM, Klein MM (2013) Objective evidence that small-fiber polyneuropathy underlies some illnesses currently labeled as fibromyalgia. Pain 154:2310–2316
Üçeyler N, Zeller D, Kahn AK, Kewenig S, Kittel-Schneider S, Schmid A, Casanova-Molla J, Reiners K, Sommer C (2013) Small fibre pathology in patients with fibromyalgia syndrome. Brain 136:1857–1867
Ramírez M, Martínez-Martínez LA, Hernández-Quintela E, Velazco-Casapía J, Vargas A, Martínez-Lavín M (2015) Small fiber neuropathy in women with fibromyalgia. An in vivo assessment using corneal confocal bio-microscopy. Semin Arthritis Rheum 45:214–219
Brouwer BA, Merkies IS, Gerrits MM, Waxman SG, Hoeijmakers JG, Faber CG. J Painful neuropathies: the emerging role of sodium channelopathies. J Peripher Nerv Syst 2014;19:53–65.
Faber CG, Hoeijmakers JG, Ahn HS, Cheng X, Han C, Choi JS et al (2012) Gain of function mutations in idiopathic small fiber neuropathy. Ann Neurol 71(1):26–39
Vargas-Alarcon G, Alvarez-Leon E, Fragoso JM, Vargas A, Martinez A, Vallejo M, Martinez-Lavin M (2012) A SCN9A gene-encoded dorsal root ganglia sodium channel polymorphism associated with severe fibromyalgia. BMC Musculoskelet Disord 2012
Paleari D, Rossi GA, Nicolini G, Olivieri D (2011) Ambroxol: a multifaceted molecule with additional therapeutic potentials in respiratory disorders of childhood. Expert Opin Drug Discov 6:1203–1214
Weiser T (2006) Comparison of the effects of four Na+ channel analgesics on TTX-resistant Na+ currents in rat sensory neurons and recombinant Nav1.2 channels. Neurosci Lett 395:179–184
Hama AT, Plum AW, Sagen J (2010) Antinociceptive effect of ambroxol in rats with neuropathic spinal cord injury pain. Pharmacol Biochem Behav 97:249–255
Lerma C, Martinez A, Ruiz N, Vargas A, Infante O, Martinez-Lavin M (2011) Nocturnal heart rate variability parameters as potential fibromyalgia biomarker. Correlation with symptoms severity Arthritis Res Ther 13:R185
Meeus M, Goubert D, De Backer F, Struyf F, Hermans L, Coppieters I, De Wandele I, Da Silva H, Calders P (2013) Heart rate variability in patients with fibromyalgia and patients with chronic fatigue syndrome: a systematic review. Semin Arthritis Rheum 43:279–287
Martínez-Lavín M, Vidal M, Barbosa RE, Pineda C, Casanova JM, Nava A (2002) Norepinephrine-evoked pain in fibromyalgia. A randomized pilot study ISCRTN 70707830. BMC Musculoskelet Disord 3:2
Chenot JF, Weber P, Friede T (2014) Efficacy of Ambroxol lozenges for pharyngitis: a meta-analysis. BMC Fam Pract 15:45. doi:10.1186/1471-2296-15-45
Kern KU, Weiser T (2015) Topical ambroxol for the treatment of neuropathic pain. An initial clinical observation. Schmerz (Suppl 3):S89–96
Narita A, Shirai K, Itamura S, Matsuda A, Ishihara A, Matsushita K, Fukuda C, Kubota N, Takayama R, Shigematsu H, Hayashi A, Kumada T, Yuge K, Watanabe Y, Kosugi S, Nishida H, Kimura Y, Endo Y, Higaki K, Nanba E, Nishimura Y, Tamasaki A, Togawa M, Saito Y, Maegaki Y, Ohno K, Suzuki Y (2016) Ambroxol chaperone therapy for neuronopathic Gaucher disease: a pilot study. Ann Clin Transl Neurol 3:200–215
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Rights and permissions
About this article
Cite this article
Martínez-Martínez, LA., Pérez, LF., Becerril-Mendoza, LT. et al. Ambroxol for fibromyalgia: one group pretest-posttest open-label pilot study. Clin Rheumatol 36, 1879–1884 (2017). https://doi.org/10.1007/s10067-017-3664-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-017-3664-z