Abstract
ERAP1 single nucleotide polymorphisms (SNP) are associated with ankylosing spondylitis. Data on ERAP1SNPs in juvenile idiopathic arthritis (JIA) is scarce. ERAP1 rs30187 SNP was shown to confer risk in the enthesitis-related arthritis (ERA) category of JIA. We examined the prevalence and association of this SNP in Indian children with ERA. SNPs in ERAP1 (rs30187) were genotyped in children with ERA (n = 271), ankylosing spondylitis (AS) (n = 213) and healthy controls (n = 101), using Taqman genotyping. Allele frequencies and genotype frequencies were calculated and compared using the Cochran Armitage test. Minor allele frequencies were 0.52 in ERA, 0.57 in AS, and 0.57 in healthy controls. Neither ERA nor AS patients showed significant association with this SNP. Segregating according to HLAB27 status did not alter the lack of association. rs30187 SNP in ERAP1 does not confer risk of developing ERA or AS in the Asian Indian population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Though HLAB27 is the major genetic risk factor in spondyloarthropathy, non-MHC genes have also been identified in genome-wide association studies [1]. These include Interleukin 23 receptor, endoplasmic reticulum aminopeptidase 1 (ERAP1; also called aminopeptidase regulator of TNFR1 shedding 1 or ARTS1), and TNFSF15. ERAP1 is a “molecular ruler,” and plays a role in trimming antigen peptides to length optimum for loading onto MHC1 molecules. Therefore, it influences the repertoire of peptides presented by class I molecules which in turn shape the immune response [2].
ERAP1 gene has several single nucleotide polymorphisms (SNPs) and some of them increase susceptibility to AS while others are protective. A recent meta-analysis has summarized the data available [3]. Though there are a large number of studies available in AS, data in juvenile idiopathic arthritis (JIA) is very limited. The ERAP1 rs30187 polymorphism was found to be significantly associated with the enthesitis-related arthritis (ERA) category of JIA, while showing no association with JIA overall [4].
The association of ERAP1 polymorphisms with spondyloarthropathy risk has not been elucidated in the South Asian population and allele frequencies differ substantially between different ethnicities. Further, since ERA is the most common category of JIA seen in our clinic (38%) and it shares many features with adult ankylosing spondylitis, we examined the prevalence and association of the rs30187 polymorphism in our cohort of patients.
Patients and methods
The study was conducted at the Sanjay Gandhi Postgraduate Institute of Medical Sciences, a tertiary referral hospital in North India. The study was approved by the Institutional Ethics committee and informed consent was taken from patients or legal guardians. Patients diagnosed with JIA-ERA according to the ILAR criteria [5] were included in the study. Age of onset and clinical features, including axial and peripheral involvement, were obtained from outpatient record files. To confirm findings in a second cohort, patients with ankylosing spondylitis were enrolled. Control samples were collected from unrelated healthy blood donors of the same ethnic group. One milliliter of blood was collected and stored in EDTA vials at −40c, and DNA was extracted using salting out method [6]. HLAB27 typing was done using amplification refractory mutation system PCR as previously described [7].
ERAP1 genotyping was done using Taqman genotyping assay for rs30187 polymorphism to detect C/T transition substitution according to manufacturer’s instructions (Thermo Fischer Scientific Inc., Waltham, MA, USA). The SNP was chosen based on previous reports of association with AS and ERA.
Statistical tests
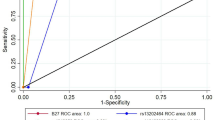
Allelic frequencies (number of copies of a specific allele divided by total number of alleles in the group) and carriage rates (number of individuals with at least one copy of a specific allele divided by the total number of individuals) were calculated in the patients and control group. Allele frequencies were compared using the Cochran Armitage test. Odds ratios with 95% confidence intervals were calculated to look for significance.
Results
Cohort characteristics
Two hundred and seventy-one children with ERA, and 213 patients with AS were included (Table 1). Median age of 101 healthy controls was 28 years (18–50) and 96 were male.
ERAP1 rs30187 polymorphism
The genotypes were in Hardy Weinberg equilibrium in healthy controls. Minor allele frequencies were 0.52 in the ERA group, 0.57 in AS group, and 0.57 in healthy controls, with no significant difference between the groups (Table 2).
HLAB27 segregated results: Amongst the children with ERA, 233 were HLAB27 positive. Minor allele frequency was similar in HLAB27 positive and negative group (Table 3). There was no association between the polymorphism and disease susceptibility in either group.
Discussion
We found that rs30187 polymorphism in ERAP1 did not increase susceptibility for developing ERA or AS in the Asian Indian population. The presence or absence of HLAB27 did not alter the lack of association in ERA.
The ERAP1 gene encodes a multifunctional aminopeptidase with two major functions: one being trimming of peptides along with ERAP2 prior to loading into the class 1 HLA groove and the second being cleavage and shedding of membrane bound cytokine receptors [2]. ERAP1 generates extracellular soluble TNF-R1 by promoting cleavage of the extracellular domain of membrane bound TNF-R, thus regulating the pro-inflammatory effects of TNF [8]. Polymorphisms in ERAP1 may promote inflammation by altering both these functions. By altering the repertoire of peptides presented by MHC class I molecules, it may promote the presentation of an arthritogenic peptide, thus provoking a CD-8 T cell response. Cleavage of membrane bound inflammatory cytokine receptors and the subsequent downregulation of signaling may also be hampered by polymorphisms.
In the rs30187 polymorphism in ERAP1, arginine at position 528 is changed to lysine. Arg528 is located near the mouth of the substrate-binding pocket of ERAP1 [9]. Thus, it is plausible that a polymorphism here can alter binding affinity of the enzyme, supporting the arthritogenic peptide theory. In a recent meta-analysis including 11,137 patients with AS and 22,793 controls, association with rs30187 SNP and AS susceptibility risk was found in European (OR 1.28) but not in East Asian (OR 1.09) or Middle Eastern (OR 1.3, ) populations [3]. Minor allele frequencies and associations in ERA and AS from some studies are summarized in Table 4. The absence of the association in our population again supports the above observation that rs30187 SNP is not associated with susceptibility to AS in all ethnic groups. Further, the absence of association with both ERA and AS in our study and the presence of association in the European population suggest that genetics of ERA and AS are similar to each other.
The MAF was similar in our ERA patients as that previously described in a British cohort of JIA-ERA [4]. However, the MAF of 0.57 in our healthy controls was higher than most European populations studied and similar to those found in the Turkish study. The high prevalence in the population may explain the lack of association with disease, and perhaps the higher prevalence of ERA amongst JIA in the South Asian ethnic group [18].
The association of ERAP1 and HLAB27 has been well known, with studies showing ERAP1 polymorphisms influence AS risk only in HLAB27 positive patients [19]. Apart from presentation of arthritogenic peptide by HLAB27, a role in protein misfolding was postulated. However, ERAP1 polymorphisms conferring susceptibility to AS were not associated with increased ER stress [20]. Cell surface HLAB27 free heavy chains, which bring about increased T cell survival and prolonged Th17 response, are increasingly being implicated. The protective allele at rs30187 was found to be associated with reduced HLAB27 free heavy chain expression, which increased on silencing ERAP1 mRNA [21]. Our data, however, did not show any difference in the risk bestowed by rs30187 SNP between the HLAB27 positive or negative group.
Other polymorphisms have been associated with ankylosing spondylitis. These include rs27044, rs26653, rs2287987, rs17482078, and rs10050860 [3]. There is marked ethnic heterogeneity in these associations as well. Studies in East Asians have been done in the Chinese and South Korean populations [22–25]. Polymorphisms implicated in Asians include rs27037, rs27582, rs27434, rs27980, and rs10050860. It may be useful to study these polymorphisms in the South Asian population.
The strengths of this study include a large number of JIA patients belonging to a homogeneous sub-category, and the first exploration of ERAP1 polymorphisms in the South Asian population. Weaknesses include small numbers of healthy controls and HLAB27 negative patients. In conclusion, we demonstrated that the rs30187 polymorphism in ERAP1 did not confer susceptibility risk in a North Indian cohort of ERA.
References
Burton PR, Clayton DG, Cardon LR, Craddock N, Deloukas P, Duncanson A, Kwiatkowski DP, McCarthy MI, Ouwehand WH, Samani NJ (2007) Association scan of 14,500 nonsynonymous SNPs in four diseases identifies autoimmunity variants. Nat Genet 39(11):1329–1337
Haroon N, Inman RD (2010) Endoplasmic reticulum aminopeptidases: biology and pathogenic potential. Nat Rev Rheumatol 6(8):461–467
Lee YH, Song GG (2016) Associations between ERAP1 polymorphisms and susceptibility to ankylosing spondylitis: a meta-analysis. Clin Rheumatol 1–7
Hinks A, Martin P, Flynn E, Eyre S, Packham J, Barton A, Worthington J, Thomson W (2011) Subtype specific genetic associations for juvenile idiopathic arthritis: ERAP1 with the enthesitis related arthritis subtype and IL23R with juvenile psoriatic arthritis. Arthritis research & therapy 13(1):1
Petty RE, Southwood TR, Manners P, Baum J, Glass DN, Goldenberg J, He X, Maldonado-Cocco J, Orozco-Alcala J, Prieur A-M (2004) International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol 31(2):390
Miller S, Dykes D, Polesky H (1988) A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res 16(3):1215
Tonks S, Marsh S, Bunce M, Bodmer J (1999) Molecular typing for HLA class I using ARMS-PCR: further developments following the 12th international histocompatibility workshop. Tissue Antigens 53(2):175–183
Cui X, Hawari F, Alsaaty S, Lawrence M, Combs CA, Geng W, Rouhani FN, Miskinis D, Levine SJ (2002) Identification of ARTS-1 as a novel TNFR1-binding protein that promotes TNFR1 ectodomain shedding. J Clin Invest 110(4):515–526
Goto Y, Hattori A, Ishii Y, Tsujimoto M (2006) Reduced activity of the hypertension-associated Lys528Arg mutant of human adipocyte-derived leucine aminopeptidase (A-LAP)/ER-aminopeptidase-1. FEBS Lett 580(7):1833–1838
Maksymowych W, Inman R, Gladman D, Reeve J, Pope A, Rahman P (2009) Association of a specific ERAP1/ARTS1 haplotype with disease susceptibility in ankylosing spondylitis. Arthritis & Rheumatism 60(5):1317–1323
Choi C-B, Kim T-H, Jun J-B, Lee H-S, Shim SC, Lee B, Pope A, Uddin M, Rahman P, Inman RD (2009) ARTS1 polymorphisms are associated with ankylosing pondylitis in Koreans. Ann Rheum Dis
Zvyagin I, Dorodnykh VY, Mamedov I, Staroverov D, Bochkova A, Rebrikov D, Lebedev Y (2010) Association of ERAP1 allelic variants with risk of ankylosing spondylitis. Acta Naturae (англоязычная версия) 2(3):6
Pazár B, Safrany E, Gergely P, Szántó S, Szekanecz Z, Poór G (2010) Association of ARTS1 gene polymorphisms with ankylosing spondylitis in the Hungarian population: the rs27044 variant is associated with HLA-B* 2705 subtype in Hungarian patients with ankylosing spondylitis. J Rheumatol 37(2):379–384
Szczypiorska M, Sánchez A, Bartolomé N, Arteta D, Sanz J, Brito E, Fernández P, Collantes E, Martínez A, Tejedor D (2011) ERAP1 polymorphisms and haplotypes are associated with ankylosing spondylitis susceptibility and functional severity in a Spanish population. Rheumatology 50(11):1969–1975
Mahmoudi M, Jamshidi AR, Amirzargar AA, Farhadi E, Nourijelyani K, Fallahi S, Oraei M, Noori S, Nicknam MH (2012) Association between endoplasmic reticulum aminopeptidase-1 (ERAP-1) and susceptibility to ankylosing spondylitis in Iran. Iranian Journal of Allergy, Asthma and Immunology 11(4):294
Bettencourt BF, Rocha FL, Alves H, Amorim R, Caetano-Lopes J, Vieira-Sousa E, Pimentel-Santos F, Lima M, Porto G, Branco JC (2013) Protective effect of an ERAP1 haplotype in ankylosing spondylitis: investigating non-MHC genes in HLA-B27-positive individuals. Rheumatology 52(12):2168–2176
Cinar M, Akar H, Yilmaz S, Simsek I, Karkucak M, Sagkan RI, Pekel A, Erdem H, Avci IY, Acikel C (2013) A polymorphism in ERAP1 is associated with susceptibility to ankylosing spondylitis in a Turkish population. Rheumatol Int 33(11):2851–2858
Kunjir V, Venugopalan A, Chopra A (2010) Profile of Indian patients with juvenile onset chronic inflammatory joint disease using the ILAR classification criteria for JIA: a community-based cohort study. J Rheumatol 37(8):1756–1762. doi:10.3899/jrheum.090937
Evans DM, Spencer CC, Pointon JJ, Su Z, Harvey D, Kochan G, Oppermann U, Dilthey A, Pirinen M, Stone MA (2011) Interaction between ERAP1 and HLA-B27 in ankylosing spondylitis implicates peptide handling in the mechanism for HLA-B27 in disease susceptibility. Nat Genet 43(8):761–767
Kenna T, Lau M, Keith P, Ciccia F, Costello M, Bradbury L, Low P, Agrawal N, Triolo G, Alessandro R (2015) Disease-associated polymorphisms in ERAP1 do not alter endoplasmic reticulum stress in patients with ankylosing spondylitis. Genes and immunity 16(1):35–42
Chen L, Ridley A, Hammitzsch A, Al-Mossawi MH, Bunting H, Georgiadis D, Chan A, Kollnberger S, Bowness P (2015) Silencing or inhibition of endoplasmic reticulum aminopeptidase 1 (ERAP1) suppresses free heavy chain expression and Th17 responses in ankylosing spondylitis. Ann Rheum Dis 2014–206996
Zhang Z, Dai D, Yu K, Yuan F, Jin J, Ding L, Hao Y, Liang F, Liu N, Zhao X (2014) Association of HLA-B27 and ERAP1 with ankylosing spondylitis susceptibility in Beijing Han Chinese. Tissue Antigens 83(5):324–329
Wang C-M, Ho H-H, Chang S-W, Wu Y-JJ, Lin J-C, Chang P-Y, Wu J, Chen J-Y (2012) ERAP1 genetic variations associated with HLA-B27 interaction and disease severity of syndesmophytes formation in Taiwanese ankylosing spondylitis. Arthritis research & therapy 14(3):1
Bang S-Y, Kim T-H, Lee B, Kwon E, Choi SH, Lee KS, Shim SC, Pope A, Rahman P, Reveille JD (2011) Genetic studies of ankylosing spondylitis in Koreans confirm associations with ERAP1 and 2p15 reported in white patients. J Rheumatol 38(2):322–324
Davidson SI, Wu X, Liu Y, Wei M, Danoy PA, Thomas G, Cai Q, Sun L, Duncan E, Wang N (2009) Association of ERAP1, but not IL23R, with ankylosing spondylitis in a Han Chinese population. Arthritis & Rheumatism 60(11):3263–3268
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Institutional Ethics committee and informed consent was taken from patients or legal guardians.
Disclosures
None.
Funding
This study did not receive any external funding.
Rights and permissions
About this article
Cite this article
Srivastava, R., Phatak, S. & Aggarwal, A. ERAP1 rs30187 single nucleotide polymorphism does not confer disease susceptibility in North Indian children with enthesitis-related arthritis. Clin Rheumatol 36, 1161–1165 (2017). https://doi.org/10.1007/s10067-017-3560-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-017-3560-6